Abstract
Introduction:
The aim of the study was to determine the most frequent early and late complications in different types of ileal urinary diversions.
Patients and methods:
The study was conducted in a five-year period, on 106 patients who were diagnosed with invasive urinary bladder cancer and who had indication for radical cystectomy with one of the investigated types of urine derivation. They were divided into 2 groups, based on the type of ileal urinary diversions.
Results:
The colonization of bacteria was more prominently present in the ileal conduit urinary diversion group (97%) compared to Ghoneim (25%) and Hautmann (10%) group, Ureteral stenosis was slightly less represented in the conduit group (9.1%). Wound infections were significantly more represented in the conduit (21.2%) than in the Ghoneim group (5%) Nighttime incontinence was present in 20% of patients in both groups or 4 patients in each group. Daytime incontinence in the Ghoneim group was present in 3 patients (15%) and in the Hautmann group 2 patients (10%). Late complications correlate significantly negative with the type of surgery and slightly negative with the grade, and significantly positively with the examined group and T stage, and slightly correlate positively to the N and R stages. Early complications correlate slightly negative with the type of surgery, slightly negative with the grade, and significantly positively with T stage, and slightly positively correlates with the N and R stage.
Conclusion:
The most commonly reported complications in ileal conduit are: prolonged ileus, stoma infection, wound dehiscence and bacterial colonization, followed by peristomal skin complications and complications related only to the stoma, such as stenosis and stoma retraction, and prolaps of ileostoma and ileointestinal stenosis. The ileus rate in orthotopic derivation was significantly lower than that of the ileal conduit group, which led to the conclusion that the neomybladder position does not disturb the anatomic abdominal structure.
Keywords: Ileal conduit, orthotopic neobladder, complications
1. INTRODUCTION
Radical cystectomy involves simultaneous surgery of the urinary tract, digestive tract and lymph nodes, and therefore complications often occur after such extensive surgery. According to the existing literature, the incidence of this secondary condition varies widely (19% -64%) (1). As with morbidity, there is a wide range of mortality incidence ranging from 0.8% to 8.3% (2.3). The rate of complications after radical cystectomy are also affected by follow-up period, because many complications are influenced by certain time period (4). Hollenbeck et al. (5) analyzed data from 2538 cases obtained from the National Quality Improvement Program in 123 US Medical Centers and the results of these studies showed that 30.5% of patients had at least one complication in 30 days of follow-up after radical cystectomy. Intestinal obstruction is the most common complication after radical cystectomy and occurs in 23% of cases (6). Infections are the other most common complication of radical cystectomy and make 25% of all early complications after radical cystectomy (6). Severe complication immediately after radical cystectomy is urinary extravasation on anastomosis of derivation as well as extravasation of intestinal content from intestinal anastomosis that occur in 3% of cases (3). Early wound complications include wound dehiscence which is present in 15% of cases.
2. AIM
The aim of the study was to determine the most frequent early and late complications in different types of ileal urinary diversions.
3. PATIENTS AND METHODS
The study was conducted in a five-year period at Urology clinic, Clinical Center University of Sarajevo in 106 patients aged from 40 to 80, who were diagnosed with invasive urinary bladder cancer and who had indication for radical cystectomy with one of the investigated types of urine derivation. All patients had transitional cell carcinoma (TCC) and no distant metastases were found or local recurrence. In this study, 106 patients were divided into 2 groups. Group A consisted of 40 patients who were diagnosed with invasive bladder cancer with radiologic, urological and pathohistological procedures and radical cystectomy was performed. In this group, patients were treated with Hautmann derivation and Chimney modification of the ureterointestinal anastomosis, i.e. the reflux mechanism of ureteral implantation in neobladder. In the other 20 patients a supravesical derivation by Ghoneim was performed, i.e. antirefluxing ureteric implantation in neobladder through the serous tunnel. Group B consisted of 66 patients who were diagnosed with invasive bladder cancer with radiologic, urological and pathohistological procedures and radical cystectomy was performed (ileal conduit, Brücker). These patients underwent ileal conduit urinary diversion.
Both early and late complications of intestinal derivations were observed in both groups. In the statistical analysis of results descriptive statistics, Spearman’s rank correlation coefficient, analysis of variance (ANOVA), Pearson’s chi-squared test, Fisher’s exact test and multivariate regression analysis were used.
4. RESULTS
The colonization of bacteria was more prominently present in the ileal conduit urinary diversion group (97%) compared to Ghoneim (25%) and Hautmann (10%) group, with statistically significant difference (p <0.001) demonstrated by Pearson’s chi-squared test.
Table 1. shows the number of cases of wound dehiscence in the examined groups and their representation in percentages. From this table, it is evident that wound dehiscence was significantly more represented in the B group (21.2%) than in the A group (5%),.
Table 1.
Percentage of wound dehiscence in the examined groups
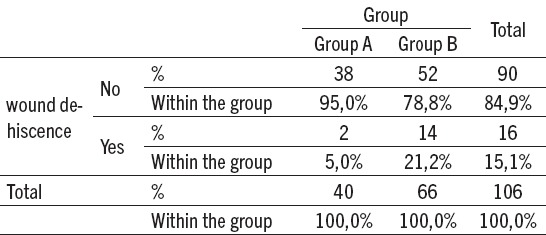
Figure 1. shows the symptomatic infection by type of operation and displays them in percentages. From this table it is apparent that the infection was more prominent in the conduit group (22.7%) compared to the Ghoneim group (15%) and was not present in the Hautmann group and that was not statistically significant difference proven with the Pearson’s chi-squared test.
Figure 1.
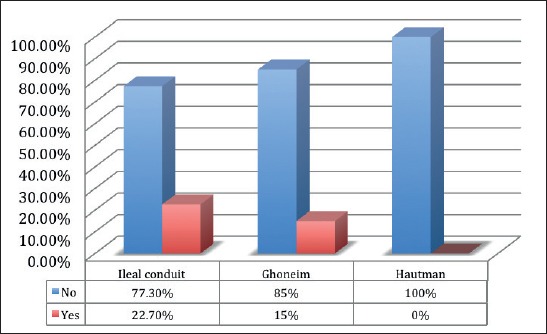
Symptomatic infection by type of surgery in %
Figure 2. shows the occurrence of right ureteral stenosis by type of surgery and its representation in percentages. From the figure it is apparent that the ureteral stenosis was slightly less represented in the conduit group (9.1%) than in the Ghoneim group (10%) and was not present in the Hautmann group which was not statistically significant difference proven with the Pearson’s chi-squared test. Ureteral stenosis was slightly less represented in the conduit gruop (6.1%) than in the Ghoneim group (15%) and in the Hautmann group it was present in 5% cases, which was not statistically significant difference proven with the Pearson’s chi-squared test. There was no bilateral ureteral stenosis in the conduit and Hautmann group while in the Ghoneim group was present only in one patient, which was not statistically significant difference proven with the Pearson’s chi-squared test. Ileus was slightly more represented in the conduit group (13.6%) compared to the Ghoneim group (5%) and was not present in the Hautmann group which was not statistically significant difference proven with the Pearson’s chi-squared test. Wound infections were significantly more represented in the conduit (21.2%) than in the Ghoneim group (5%) and were not present in the Hautmann group and that was statistically significant difference proven with the Pearson’s chi-squared test.
Figure 2.
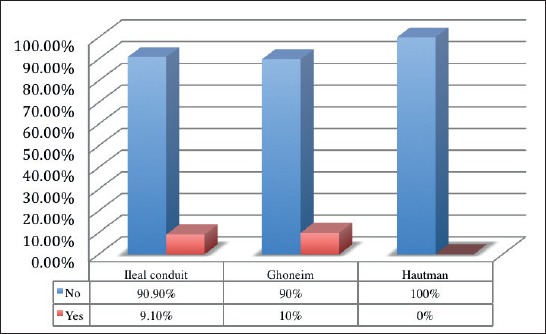
Percentage of right ureteral stenosis by type of surgery
Table 2. shows mean values of PVR in orthotopic derivation and is 62.5 ml in the Ghoneim group, and 45 ml in the Hautmann group. Although the range is very wide 0-400 ml for Ghoneim group and 0-300 ml for Hautmann group, the normal mean values result from the fact that both groups had only one patient with PVR 300 and 400 ml. The further range between the urination in hours for the Hautmann group is 4.25 hours in the interval 2-6 hours, and for the Ghoneim group is 4.85 in the interval 3-6 h. Nighttime incontinence was present in 20% of patients in both groups or 4 patients in each group. Daytime incontinence in the Ghoneim group was present in 3 patients (15%) and in the Hautmann group 2 patients (10%). By testing the data with the Fisher’s exact test, there are no statistical differences among the groups. All results are presented as late complications in orthotopic derivation.
Table 2.
Mean post-void residual (PVR) urine volume and hours between urination for orthotopic derivation
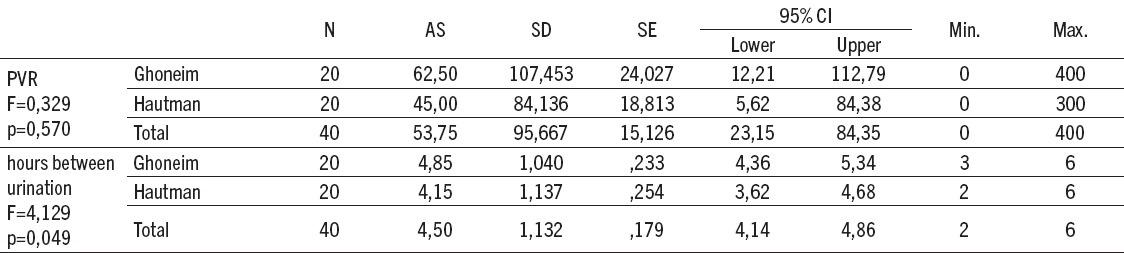
Table 3.
Correlation of late and early complications by type of surgery, group, T, N, R stage and grade.
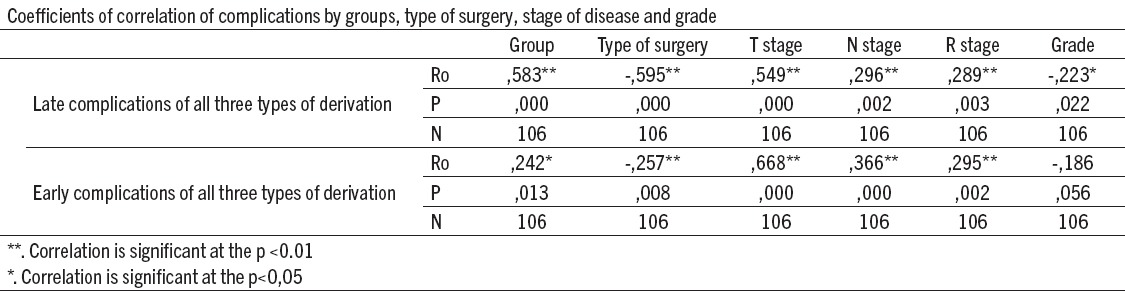
Late complications correlate significantly negative with the type of surgery and slightly negative with the grade, and significantly positively with the examined group and T stage, and slightly correlate positively to the N and R stages. Early complications correlate slightly negative with the type of surgery, slightly negative with the grade, and significantly positively with T stage, and slightly positively correlates with the N and R stage.
Bacterial colonization was more prominently represented in the conduit group (97%) compared to Ghoneim (25%) and Hautmann (10%) group, with statistically significant difference (p <0.001).
Ileus was more represented in the conduit group (13.6%) compared to the Ghoneim (5%) group and was not present in the Hautmann group. In this study, 66 of the total number of patients with ileal conduit derivation, 9.1% had stenosis, 3% of subjects had prolapse of the stoma, and 22.7% of patients had skin infection around the stoma.
5. DISCUSSION
Radical cystectomy is a treatment of choice for invasive urinary bladder cancer and that is also the case at Urology clinic, Clinical Center University of Sarajevo. Although surgical technique has been significantly improved over the past 10 to 15 years, this type of surgery remains an operation with significant morbidity and less significant mortality. During five-year period at the Urology clinic, a total of 139 cystectomies were performed, with a mortality rate of 2%. Similar results were published by Novotni et al. in 2007, Chahal et al. in 2003 (2, 3) and vary from 0.8 to 8.3% in range. The most common complications of ileal conduit can be linked to bowel function, ureteroileal anastomosis, complications related to cutaneous stoma itself and infections in general. They can also be divided on early and late complications. Despite the simplicity of the operation with ileal conduit in comparison to orthotopic derivation, the morbidity rate in the first 30 days is 20-56%, and after 30 days is 28-81% (8). The early intestinal complications are related to the intestinal anastomosis and resection. The most common complication is paralytic ileus. The incidence varies according to various authors from 18% (9), 20% (8) to 22% (10). In the conducted study, 26% of patients had prolonged ileus, which was treated conservatively, which approximately corresponds to previous results. In general, intestinal obstruction occurs in 5-10% of cases, depending on the author (11). Enterocutaneous fistula, extravasation of intestinal contents and ureteroileal extravasation of urine in this study were not recorded.
Although in the literature the rate of 3-7% (8) is recorded, this last complication was not present in this study because prosthesis (splint) was routinely used in all patients. The probable reason for the lack of enterocutaneous fistula and extravasation of the intestinal contents is a good surgical technique (in all patients anastomosis was performed with single Vicryl 3/0 seromuscular sutures which were not tightened, the mucus was always suppressed to the lumen and not caught in the suture, the distance between the sutures was on average 3 mm, mesentery on the mesenteric side of the intestine was never in the suture, the parts of the ileum on which anastomosis was performed were well vascularized and with no hematomas in the corresponding mesentery, which could endanger vascularization).
However, in the 21.2% of the cases in the ileal conduit group wound dehiscence and wound infections appeared, with identical percentage. The infection itself in other studies has a rate of 25%, and wound dehiscence appeared in 15% of cases. (6). The onset of dehiscence of the wound was associated with a high stage of disease, hypoproteinemia and prolonged ileus. Although the stage of disease, hypoproteinemia and prolonged ileus in the literature does not appear as a cause of dehiscence of the wound, but infection, according to this study, these factors must be considered in the future as one of the causes of wound dehiscence. This complication, after treatment of the wound infection, had to be surgically treated in all 14 patients. Complications related only to the stoma can be stenosis, retraction, infection, prolapse of the stoma, parastomal hernia. In most studies late complications related to stoma are mentioned in 15-65% of cases (12) and are the most common reason for reoperation in patients with ileal conduit diversion.
In the study of Cheung et al. in 1995, 322 stomas were analyzed. Stoma stenosis was present in 7.3% of cases, parastomal hernia in 27.6% of cases, prolapse in 4.1% of cases and excoriation in the 20.3% of the cases (13). In the examined sample, in the 9.1% of the stoma stenosis retraction occurred, 3% of patients a prolapse of the stoma occured, while skin infection and exacerbation around the stoma had 22.7% of the patients. Parastomal hernia was not recorded.
Also bacterial colonization was present in 97% of cases which was not treated. In 74% of patients after the formation of the conduit, colonization occured, which did not require any treatment. In our study, there is a very high percentage (93%), which can be explained by difficulty of obtaining the funds needed for stoma care. In 22.7% of patients who had manifested infection with skin changes, antibiotic therapy was applied according to the antibiogram.
The incidence of stenosis in ureterointestinal anastomosis, with ileal conduit, in this study was 9.1% for the left side and 6.1% for the right side. Although no statistical difference has been demonstrated, the hypothesis for this event is that the left ureter must be more liberalized and intersects below the inferior mesenteric artery. In the available literature, the incidence ranges from 7% (14) to 14% (15). Incidence of the stenosis of the ureteroileal anastomos in the orthotopic derivation is in the range from 2.4 to 9% (16,17,18).
In patients that are enrolled in this study, the urethra stenosis rate is 5%, and it is more likely that this is a consequence of surgical technique, and less likely to be the result of extravasation of urine from the ureteroileal joint. The reason for this statement lies in the fact that the standard procedure in these patients is to hold a permanent three-lane catheter in neobladder for an average of 15 days, with the intestinal mucus being flushed by the pressure of the water column every 2 hours, so extravasation of urine is recorded only in one patient or in 2.5% of cases (urine extravasation rate with ureteroileal anastomosis is 2.1-6.6% (19)).
The ureterointestinal stenosis incidence was 30% in the group of patients who had neobladder with serous tunnel (Abol-Enein and Ghoneim). Such high rate of ureterointestinal narrowing stenosis should be taken with the reserve as there were only 20 patients in this group. If the above results are taken into account, it is evident that the most optimal treatment for ureterointestinal anastomosis is chiminey modification of the urethra implantation on the tubularized short segment of the ileum on the orthotopic bladder by Hautmann. In the early postoperative period there was no extravasation of the urine at the site of the ureterointestinal anastomosis due to the fact that routine ureteral splints were used, although the rate of this complication is 3% (20).
The colonization of bacteria in the orthotopic bladder group was present in 17.5% of the cases, and the symptomatic bacteriuria was treated only in 7.5% of cases. In one patient, the infection progressed to sepsis. In this group of patients, the most dominant bacteria were Pseudomonas in 7.5% of cases, Klebsiella in 5% and Proteus in 2.5% of cases. Urine cultures where the amount of bacteria was 104 and more were taken in consideration. These results differ significantly from the results in published papers where bacterial colonization of the orthotopic bladder was present in 40-80% of cases (21, 22). In patients with impaired renal function, hyperchloremic metabolic acidosis developed with worsening of patient condition, dehydration, nausea, uremia and bone loss. Acidosis led to deterioration of vitamin D synthesis and osteoclastic activation in bone (19,23,24,25). Since the standard in this institution is taking 40 cm of intestine, no metabolic changes were noted except mild acidosis (-0.53). Also, in none of the patients a case of peristing diarrhea has been reported. Value of vitamin B12, which was the subject of evaluation, remained within the physiological limits, and most authors agree that there is a vitamin B12 reserve in the body of adults for a period of 5 years. It is important to note when comparing the values of urea, creatinine and erythrocyte in orthotopic derivations and ileal conduits, a statistically significant difference has been proven. It was demonstrated that the ileal conduit group had chronic renal insufficiency, which led to decreased production of erythropoietin.
The rate of prolonged ileus in the group of orthotopic derivation is also interesting. It was only present in 7.5% cases, while in the group of ileal conduit it was present in 26% of cases, proving that orthotopic derivation does not significantly reduce the anatomy and arrangement of the intestine after surgery. This claim is confirmed by the fact that the rate of dehiscence of the wound was only present in 5% cases, whereas the infection of the wound was present in 2.5% cases. In most studies it is mentioned that after 12 months of follow-up of daytime incontinence in patients with orthotopic derivation was present in 95% of cases and nighttime lower by 10-15% (15). Daytime incontinence was present in 87.5% of patients in this study, and nighttime was present in 80% of patients. These results are excellent considering the fact that 40 cm of the ileum was taken during surgery and that the evaluation of these patients was performed 6 months after surgery, and it is known that the establishment of continence is improved over time as the bladder capacity increases. In a study conducted by Steers et al. in 2000 (23, 24), on 2238 patients during 26 ± 18 months, the daytime incontinence rate was 13.3% ± 13.6%. The reason for such high deviation is that the author used data from different medical centers, which, given the multifactorial causes of incontinence had different definitions of continence. Nighttime incontinence develops in almost 28% of patients (ranging from 0-67%) with orthotopic bladder (23).
In this study, nighttime incontinence was present in 20% of cases, 6 months after surgery, which corresponds to the available data. It should be noted that all patients after discharge received instructions for urination in which was recommended, among other things, the use of alarm during the night.
6. CONCLUSION
The most commonly reported complications in ileal conduit are: prolonged ileus, stoma infection, wound dehiscence and bacterial colonization, followed by peristomal skin complications and complications related only to the stoma, such as stenosis and stoma retraction, and prolaps of ileostoma and ileointestinal stenosis. Colonization with bacteria was more frequently represented in relation to available literature, but that is explained by the fact that the patients being enrolled in the study were not able to provide stoma care products. The ileus rate in orthotopic derivation was significantly lower than that of the ileal conduit group, which led to the conclusion that the neomybladder position does not disturb the anatomic abdominal structure. The problem of the wound dehiscence can be repaired by laparoscopic surgery. Although all mentioned facts support the choice of orthotopic bladder as a method of choice, it should be taken into account that patients with ileal conduit are 10 years older with all of their comorbidities, and also that most of them prior to surgery had advanced disease (T3 and T4 and positive lymph nodes), or elevated creatinine levels and ureteral invasion were contraindications to the continental bladder.
Footnotes
• Conflict of interest: none declared.
• Authors contributiona: A.P. and E.B. made substantial contribution to conception and design (acquisition of data, analysis and interpretation of data). A.P. revised it critically and gave final approval of the version to be submitted.
REFERENCES
- 1.Meller AE, Nesrallah LJ, Dall'Oglio MF, et al. Complications in radical cystectomy performed at a teaching hospital. Int Braz J Urol. 2002;28:522–5. [PubMed] [Google Scholar]
- 2.Shabsigh A, Korets R, Vora KC, et al. Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol. 2009;55:164–76. doi: 10.1016/j.eururo.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 3.Novotny V, Hakenberg OW, Wiessner D. Perioperative complications of radical cystectomy in a contemporary series. Eur Urol. 2007;51:397–402. doi: 10.1016/j.eururo.2006.06.014. [DOI] [PubMed] [Google Scholar]
- 4.Chahal R, Sundaram SK, Iddenden R, et al. A study of the morbidity, mortality and long-term survival following radical cystectomy and radical radiotherapy in the treatment of invasive bladder cancer in Yorkshire. Eur Urol. 2003;43:246–57. doi: 10.1016/s0302-2838(02)00581-x. [DOI] [PubMed] [Google Scholar]
- 5.Meyer JP, Blick C, Arumainayagam N. A three-centre experience of orthotopic neobladder reconstruction after radical cystectomy: revisiting the initial experience, and results in 104 patients. BJU Int. 2009;103:680–3. doi: 10.1111/j.1464-410X.2008.08204.x. [DOI] [PubMed] [Google Scholar]
- 6.Hollenbeck BK, Miller DC, Taub D, et al. Identifying risk factors for potentially avoidable complications following radical cystectomy. J Urol. 2005;174:1231–7. doi: 10.1097/01.ju.0000173923.35338.99. [DOI] [PubMed] [Google Scholar]
- 7.Shabsigh A, Korets R, Vora KC, et al. Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol. 2009;55:164–76. doi: 10.1016/j.eururo.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Whitmore WF., Jr . Total cystectomy. In: Cooper EH, Williams RE, editors. The biology and clinical management of bladder cancer. Oxford, UK: Blackwell Scientific Publications; 1975. pp. 193–227. [Google Scholar]
- 9.Farnham SB, Cookson MS. Surgical complications of urinary diversion. World J Urol. 2004;22:157–67. doi: 10.1007/s00345-004-0429-5. [DOI] [PubMed] [Google Scholar]
- 10.Chang SS, Baumgartner RG, Wells N, et al. Causes of increased hospital stay after radical cystectomy in a clinical pathway setting. J Urol. 2002;167:208–11. [PubMed] [Google Scholar]
- 11.Lowrance WT, Rumohr JA, Chang SS, et al. Contemporary Open Radical Cystectomy: Analysis of Perioperative Outcomes. The Journal of Urology. 2008;179:1313–18. doi: 10.1016/j.juro.2007.11.084. [DOI] [PubMed] [Google Scholar]
- 12.Hollenbeck BK, Taub DA, Miller DC, et al. The regionalization of radical cystectomy to specific medical centers. J Urol. 2005;174:1385–9. doi: 10.1097/01.ju.0000173632.58991.a7. [DOI] [PubMed] [Google Scholar]
- 13.Herlufsen P, Olsen AG, Carlsen B, et al. Study of peristomal skin disorders in patients with permanent stomas. Br J Nurs. 2006;15:854–62. doi: 10.12968/bjon.2006.15.16.21848. [DOI] [PubMed] [Google Scholar]
- 14.Szymanski KM, St-Cyr D, Alam T, et al. External stoma and peristomal complications following radical cystectomy and ileal conduit diversion: a systematic review. Ostomy Wound Manage. 2010;56:28–35. [PubMed] [Google Scholar]
- 15.Cheung MT. Complications of an abdominal stoma: an analysis of 322 stomas. Aust N Z J Surg. 1995;65:808. doi: 10.1111/j.1445-2197.1995.tb00566.x. [DOI] [PubMed] [Google Scholar]
- 16.Lowrance WT, Rumohr JA, Clark PE, et al. Urinary diversion trends at a high volume, single American tertiary care center. J Urol. 2009;182:2369–74. doi: 10.1016/j.juro.2009.07.026. [DOI] [PubMed] [Google Scholar]
- 17.Madersbacher S, Schmidt J, Eberle JM, et al. Long-term outcome of ileal conduit diversion. The Journal of Urology. 2003;169:985–90. doi: 10.1097/01.ju.0000051462.45388.14. [DOI] [PubMed] [Google Scholar]
- 18.Kulkarni JN, Pramesh CS. Long-term results of orthotopic neobladder reconstruction after radical cystectomy. BJU International. 2003;91:485–8. doi: 10.1046/j.1464-410x.2003.04131.x. [DOI] [PubMed] [Google Scholar]
- 19.Simon J, Bartsch G, Jr, Kufer R, et al. Neobladder emptying failure in males: incidence, etiology and therapeutic options. J Urol. 2006;176:1468. doi: 10.1016/j.juro.2006.06.048. [DOI] [PubMed] [Google Scholar]
- 20.Hautmann RE, Volkmer BG, Schumacher MC, et al. Long-term results of standard procedures in urology: The ileal neobladder. World J Urol. 2006;24:305–14. doi: 10.1007/s00345-006-0105-z. [DOI] [PubMed] [Google Scholar]
- 21.Jensen JB, Lundbeck F, Jensen KME. Complications and neobladder function of the Hautmann orthotopic ileal neobladder. BJU Int. 2006;98:1289–94. doi: 10.1111/j.1464-410X.2006.06449.x. [DOI] [PubMed] [Google Scholar]
- 22.Akerlund S, Berglund B, Kock NG, et al. Voiding pattern, urinary volume, composition and bacterial contamination in patients with urinary diversion via a continent ileal reservoir. Br J Urol. 1989;63:619. doi: 10.1111/j.1464-410x.1989.tb05257.x. [DOI] [PubMed] [Google Scholar]
- 23.Wood DP, Jr, Bianco FJ, Jr, Pontes JE, et al. Incidence and significance of positive urine cultures in patients with an orthotopic neobladder. J Urol. 2003;169:2196. doi: 10.1097/01.ju.0000067909.98836.91. [DOI] [PubMed] [Google Scholar]
- 24.Steers WD. Voiding dysfunction in the orthotopic neobladder. World J Urol. 2000;18:330. doi: 10.1007/s003450000146. [DOI] [PubMed] [Google Scholar]
- 25.Temml C, Haidinger G, Schmidbauer J, et al. Urinary incontinence in both sexes: prevalence rates and impact on quality of life and sexual life. Neurourol Urodyn. 2000;19:259. doi: 10.1002/(sici)1520-6777(2000)19:3<259::aid-nau7>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]


