Abstract
Introduction:
Inflammation plays an important role in atherosclerosis which is the primary cause of acute coronary syndrome (ACS) that encompasses acute myocardial infarction (AMI) and unstable angina (UA).
Objective:
To investigate and characterize white blood cells (WBC) count, differential blood count in peripheral blood and neutrophil to lymphocyte ratio (NLR) in patients by the type of ACS.
Patients and methods:
The cross-sectional study included 100 patients with ACS (50 males, 50 females), aged 41 to 91 years, classified into two groups: AMI group (n=50) and UA group (n=50). Patients were hospitalized at the Clinic for Heart Diseases, University Clinical Center of Sarajevo. From patients’ medical histories the following data were obtained: WBC, neutrophil, eosinophil and basophil granulocytes count, monocyte and lymphocyte count, levels of high sensitive troponin I (hsTnI), creatine kinase MB (CK-MB) and C-reactive protein (CRP). The results were analyzed using software package SPSS, version 19.0.
Results:
Average WBC count, neutrophil granulocytes, and monocytes were significantly higher in AMI group than in UA group (p = 0.001, p < 0.0005, p = 0.03, respectively). Eosinophil count was significantly lower in patients with AMI (p = 0.022). NLR was significantly higher in AMI group in relation to patients with UA (p = 0.001). Significantly higher values of hsTnI and CK-MB were established in patients with AMI. NLR correlated significantly positive with the values of hsTnI, CK-MB, CRP, WBC and neutrophil count, and significantly negative with lymphocyte count.
Conclusion:
Average values of NLR were significantly higher in patients with AMI in relation to patients with UA, indicating the importance of this inflammatory marker in discrimination of clinical forms of ACS. A positive correlation was established between NLR and markers of myocardial necrosis, and between NLR and CRP, indicating the importance of NLR in the assessment of the extent of the myocardial lesion and in inflammation intensity assessment in ACS.
Keywords: acute coronary syndrome, neutrophil-to-lymphocyte ratio, inflammation
1. INTRODUCTION
Acute coronary syndrome (ACS) is a manifestation of coronary artery disease (CAD) and includes acute myocardial infarction (AMI) and unstable angina pectoris (UA) (1). It is known that coronary artery disease results from a complex process known as atherosclerosis. Today, it is known that atherosclerotic plaque formation is built up not only from cholesterol but also inflammatory response may be present in plaques (2). As the process of atherosclerosis begins, proinflammatory markers are beginning to emerge; the inflammation process could be followed by monitoring of these proinflammatory markers. These proinflammatory markers are oxidized LDL, proinflammatory cytokines (IL-1, TNF-α), adhesion molecules (intracellular adhesion molecule-1, selectins), inflammatory stimulants with hepatic effect (IL-6) or hepatic stimulation products such as serum amyloid A (SAA), C-reactive protein (CRP), and many others (3). Since understanding of the role of inflammation in the atherosclerosis process is increasing, so a large number of studies have focused on the research of inflammatory markers to assess the risk of acute coronary syndrome (4). More recently, the importance of neutrophil-to-lymphocyte ratio (NLR) has been increasingly investigated. The NLR represents a balance between the two important immune response paths, an inflammation that is reflected by neutrophilia and the body’s stress response, reflected by lower lymphocyte count (5). In countries with a lack of resources, this relatively inexpensive and very available parameter can be of great importance and contribute to establishing the correct diagnosis in patients with chest pain (6), since the diagnosis of acute coronary syndrome can pose a difficult challenge. Symptoms that patients complain about can be numerous and atypical, and even a classic ischemic chest pain can be caused by pulmonary thromboembolism, aortic dissection, or some other life-threatening condition (7). The electrocardiogram (ECG) finding is important in the diagnosis of myocardial ischemia. However, it is estimated that only 1/3 of patients with acute myocardial infarction have ECG classical elevation of the ST segment indicating myocardial ischemia (8). Since a large number of patients with chest pain have not specific ischemic changes on the ECG, the diagnosis in these cases largely depends on the increase in the concentration of the serum markers of myocardial injury.
2. OBJECTIVE
The objective of this study was to investigate the existence of difference in NLR between patients with acute myocardial infarction and patients with unstable angina pectoris, as well as the correlation of this ratio with markers of myocardial injury (high sensitivity troponin and creatine kinase MB) and inflammatory markers (C-reactive protein, total leukocyte count and differential blood count), with particular attention to NLR as a potential myocardial lesion intensity indicator in acute coronary syndrome.
3. PATIENTS AND METHODS
The cross-sectional study included 100 patients of both sexes, 50 male, and 50 female, aged 41-91. Patients included in this study were hospitalized at the Clinical Center for Heart Diseases at the University Clinical Center in Sarajevo, in the period from 09 August 2014 to 05 February 2015. The data were obtained from patients’ medical histories. According to the form of acute coronary syndrome patients were classified into two groups: AMI group and UA group. AMI group consisted of 50 patients of both sexes, 25 male and 25 female, aged 43 to 91, with a confirmed diagnosis of acute myocardial infarction based on clinical picture, ECG findings, elevation of biochemical markers of myocardial damage and echocardiogram findings. UA group consisted of 50 patients of both sexes, 25 male and 25 female, aged 41 to 83, with a confirmed diagnosis of unstable angina pectoris based on clinical picture, ECG findings, elevation of biochemical markers of myocardial damage and echocardiogram findings. This study did not include patients diagnosed with acute myocardial infarction or unstable angina pectoris with comorbidities, some other acute or chronic systemic inflammatory diseases, infectious or septic conditions, and patients with incomplete anamnesis.
Biochemical analyses for patients were completed at the Organizing Unit for Clinical Chemistry and Biochemistry at the University Clinical Center in Sarajevo. Peripheral blood samples were collected and tested obtaining the following results: total leukocytes and differential blood count–neutrophil, eosinophil and basophilic granulocytes, lymphocytes and monocytes, as well as levels of C-reactive protein (CRP) and high sensitivity troponin (hsTnI) and catalytic activity of creatine kinase MB (CK - MB).
Statistical analysis of the obtained data was performed using the SPSS, Statistical Package for Social Sciences version 19.0. A Shapiro-Wilk’s test of normality was used to determine the significant difference in deviation from a normal distribution. Results of descriptive statistics for numerical variables are presented as median with interquartile range (25-75 percentile). Mann-Whitney U test was used to analyze the significant difference in variables with incorrect distribution between the two observed groups. Spearman’s rank correlation was performed to test the association between two observed numerical variables. Statistically significant value of p < 0.05 was considered.
4. RESULTS
The average age of patients in the AMI group was 68.6 ± 10.0 years and in the UA group 64.8 ± 10.6 years. Patients in the AMI group were older than patients in the UA group, but without significant differences (p = 0.072).
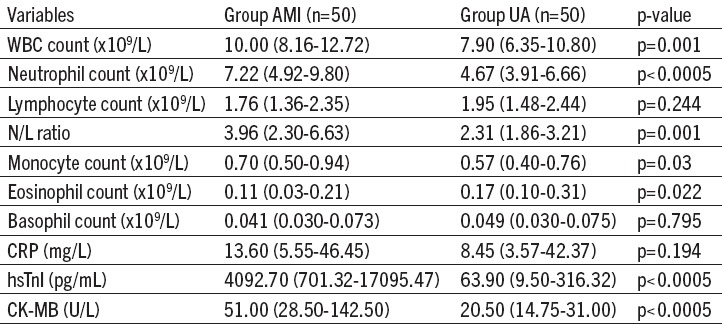
The obtained results showed that the mean values of the peripheral blood NLR in the AMI group were significantly higher than those observed in patients in the UA group (p = 0.001). Also, mean leukocyte count (p = 0.001), neutrophils (p < 0.0005) and monocytes (p = 0.03) in the peripheral blood were significantly higher in the AMI group compared to the values recorded in the UA group. Table 1 shows the values of inflammatory parameters and markers of myocardial injury in the both groups.
Table 1.
Values of inflammatory parameters and markers of myocardial injury in patients with acute myocardial infarction (AMI) and patients with unstable angina pectoris (UA). Results are presented as median with interquartile range (25-75 percentile); p<0.05 statistically significant value
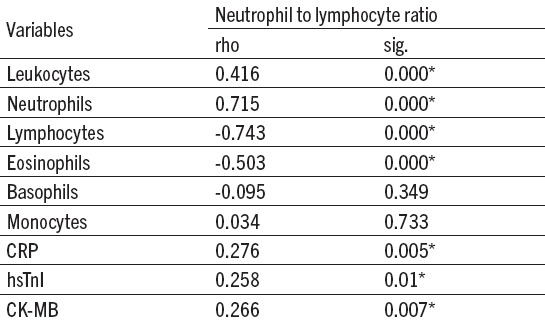
Positive correlations between NLR and total leukocytes and absolute neutrophil count (ANC) in the peripheral blood of patients with ACS and between NLR and CRP level, hsTnI level and CK-MB activity in the serum of patients with ACS were observed. Table 2 shows Spearman’s correlation coefficient between NLR and inflammatory parameters, as well as markers of myocardial damage in patients with the acute coronary syndrome.
Table 2.
Spearman’s correlation coefficient between neutrophil to lymphocyte ratio and inflammatory parameters and markers of myocardial injury in patients with acute myocardial infarction (AMI) and patients with unstable angina pectoris (UA). *p < 0.05 statistically significant value
5. DISCUSSION
This study showed that the total leukocytes and absolute neutrophil count were significantly higher in patients with AMI compared to patients with UA, which is consistent with the results of studies conducted by Zazula et al (6) and Meissner et al (9). In acute coronary syndrome, neutrophil granulocytes could be associated with the formation of platelet aggregates in the intravascular lumen, leading to an increase of the extent of myocardial infarction. Also, neutrophil granulocytes release proteolytic enzymes, making atherosclerotic plaque prone to rupture (vulnerable plaque). Therefore, an increased ANC in patients with atherosclerosis is not only the mirror of inflammation but also has an effect on the instability of the atherosclerotic plaque (10). The mean lymphocyte counts in both groups of patients in this study were within the reference range but were closer to the lower limit of reference values. However, there were no significant differences in lymphocyte count between patients in the AMI and UA group. The same results were obtained in the study conducted by Yilmaz and associates (11). Haeusler et al (12) have not found lymphopenia in patients with acute myocardial infarction, explaining that finding with the fact that their patients had the lower extent of myocardial damage. In the study conducted by Suliman et al (10) it was found that patients with ST-elevation myocardial infarction (STEMI) had lower lymphocytes compared to patients with non-ST elevation myocardial infarction (NSTEMI) and UA. The difference between this study and the above-mentioned research is the fact that patients with myocardial infarction (STEMI and NSTEMI) are all classified into one group, and it is therefore not possible to establish a significant difference in lymphocyte counts between the group of patients with AIM and the group of patients with UA.
The neutrophil-to-lymphocyte ratio demonstrated by this study is consistent with the results of the study conducted by Zazula and associates (6), who also observed a statistically significant difference in the NLR between the following four groups of patients: a group of patients with chest pain that was not the result of a heart disease, in whom the mean NLR was the lowest; a group of patients with unstable angina pectoris; a group of patients with NSTEMI; and a group of patients with STEMI in whom the mean NLR was the highest. Zazula and colleagues have proven that the calculation of NLR could be relevant in evaluating and distinguishing the origin of chest pain, while it is a cheap and widely available predictive marker. In relation to the study conducted by Zazula and associates, the disadvantage of this study was that all patients with an acute myocardial infarction, STEMI, and NSTEMI, were classified into one group. However, in a study conducted by Meissner et al (9), it was found that the NLR was higher in patients with acute myocardial infarction (STEMI, NSTEMI) and unstable angina pectoris compared to patients diagnosed with other chest pain, but no statistically significant difference in NLR values in patients with STEMI and NSTEMI was not detected.
The study showed that monocytes were significantly higher in patients with AMI than patients with UA. However, the mean values of monocytes in both groups were below the lower limit of the reference range. The results of this study are consistent with the study conducted by Hamaad and associates (13). Given that data on the medications taken by patients before admission were not taken into account in this study, it was possible that patients were treated previously with some antibiotics or immunosuppressants, which could lead to reduced number of monocytes.
This study showed, as well as the study conducted by Avramakis et al (14), that eosinophils were significantly lower in patients with AMI compared to patients with UA. Avramakis and associates attributed lower eosinophils in AMI patients to fact that eosinophils were attracted to the myocardial lesion immediately after the acute event, and that is precisely the reason for lower eosinophils in peripheral blood. Also, one of the reasons for a lower number of eosinophils in circulation may be an increase in plasma cortisol, which occurs immediately after an acute myocardial infarction (15). Although the role of eosinophil remains unexplained, there is evidence that they may have proinflammatory and/or procoagulant properties (16).
CRP values in serum samples were elevated in both groups of patients relative to the reference values. However, a statistically significant difference in the CRP levels between these two groups was not observed. This study did not include data on the medications taken by patients before admission to the hospital, and whether some of the anti-inflammatory drugs have been administered to the patients prior to blood drawing, such as, for example, aspirin, which may have an effect on the serum CRP level. According to the study conducted by Roy and associates (17), aspirin could affect CRP level, leading to lower CRP level. Also, the use of statins can have a strong anti-inflammatory effect, and according to recent studies, it has been demonstrated that the use of statins leads to lower CRP level (18).
By analyzing the correlation of the investigated parameters in patients with AMI and UA, significant negative correlations between NLR and lymphocyte count were observed, which supports the fact that lymphopenia is present in patients with the acute coronary syndrome. Significant positive correlations between the NLR and hsTnI level, and between NLR and CK-MB activity were observed, which is consistent with the results of a study conducted by Altun and associates (19). Also, a significant positive correlation between the NLR and CRP was observed, which is in line with the study conducted by Akpek and associates (20).
6. CONCLUSION
The study found that the total leukocytes, ANC, and monocytes were significantly higher in patients with AMI compared to patients with UA. Eosinophilic granulocytes were significantly lower in patients with AMI compared to patients with UA. These results suggest that these parameters can be used in the differentiation of clinical forms of acute coronary syndrome. The NLR was significantly higher in patients with AMI compared to UA patients, indicating the importance of this inflammatory indicator in the discrimination of clinical forms of acute coronary syndrome. A positive correlation between NLR and markers of myocardial damage was observed, suggesting the importance of NLR in assessing of myocardial lesion intensity in ACS, while its positive correlation with CRP indicates its significance in assessing the intensity of the inflammatory response in ACS.
Footnotes
• This article is part of the author’s (Ema Tahto) graduate thesis, done at the Faculty of Medicine, University of Sarajevo.
• Conflict of interest: All authors declare no conflict of interest.
• Authors contributions: Study conception and design: ET, RJ, LP. Acqusition of data: ET, RJ, LP, EK. Statistical analysis and interpretation of data: ET, RJ, EK. Drafting of the manuscript: ET, RJ, LP, EK. Critical revision of the manuscript for important intellecctual content: ET, RJ.
REFERENCES
- 1.Thom T, Haase N, Rasamond W, Howard VJ, Rumsfeld J, Manolio T, et al. Heart disease and stroke statistics - 2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Criculation. 2006;113:85–151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 2.Kleinschmidt KC. Epidemiology and Pathophysiology of acute coronary syndrome. Adv Stud Med. 2006;6:477–82. [Google Scholar]
- 3.Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, Criqui M, et al. Markers of inflammation and cardiovascular disease. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 4.Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 2002;105:1135–43. doi: 10.1161/hc0902.104353. [DOI] [PubMed] [Google Scholar]
- 5.Afari ME, Bhat T. Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: an update. Expert Review of Cardiovascular Therapy. 2016 doi: 10.1586/14779072.2016.1154788. doi:10.1586/14779072.2016.1154788. [DOI] [PubMed] [Google Scholar]
- 6.Zazula AD, Precoma-Neto D, Gomes AM, Kruklis H, Barbieri GF, Forte RY. An assessment of neutrophils/lymphocytes ratio in patients suspected of acute coronary syndrome. Arq Bras Cardiol. 2008;90(1):30–5. doi: 10.1590/s0066-782x2008000100006. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton B, Kwakyi E, Koyfman A, Foran M. Diagnosis and management of acute coronary syndrome. Afr J Emerg Med. 2013;3:124–33. [Google Scholar]
- 8.Welch RD, Zalenski RJ, Frederik PD, Malmgren JA, Compton S, Grzybowaki M, et al. Prognostic value of a normal or nonspecific initial electrocardiogram in acute myocardial infarction. JAMA. 2001;286:1977–84. doi: 10.1001/jama.286.16.1977. [DOI] [PubMed] [Google Scholar]
- 9.Meissner J, Irfan A, Twerenbold R, Mueller S, Reiter M, Haaf P, et al. Use of neutrophil count in early diagnosis and risk stratification of AMI. Am J Med. 2011;124(6):534–42. doi: 10.1016/j.amjmed.2010.10.023. [DOI] [PubMed] [Google Scholar]
- 10.Suliman MA, Juma AA, Almadhani AA, Pathare AV, Alkindi SS, Werner FU. Predictive value of neutrophil to lymphocyte ratio in outcomes of patients with acute coronary syndrome. Arch Med Res. 2010;41:618–22. doi: 10.1016/j.arcmed.2010.11.006. [DOI] [PubMed] [Google Scholar]
- 11.Yilmaz M, Tenekecioglu E, Arslan B, Bekler A, Ozlem AO, Karaagac K, et al. White blood cell subtypes and neutrophil-lymphocyte ratio in prediction of coronary thrombus formation in non-ST-segment elevated acute coronary syndrome. Clin Appl Thromb Hemost. 2015;21(5):446–52. doi: 10.1177/1076029613507337. [DOI] [PubMed] [Google Scholar]
- 12.Haeusler KG, Schmidt WUH, Foehring F, Meisel C, Guenther C, Brunecker P, et al. Immune responses after acute ischemic stroke or myocardial infarction. Int J Cardiol. 2010;155:372–77. doi: 10.1016/j.ijcard.2010.10.053. [DOI] [PubMed] [Google Scholar]
- 13.Hamaad A, Sosin M, Blann AD, Patel J, Gregory YH, Mac-Fadyen RJ. Markers of inflammation in acute coronary syndromes: association with increased heart rate and reductions in heart rate variability. Clin Cardiol. 2005;28:570–6. doi: 10.1002/clc.4960281207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Avramakis G, Papadimitraki E, Papakonstandinou D, Liakou K, Zidianakis M, Dermitzakis A. Platelets and white blood cell subpopulations among patients with myocardial infarction and unstable angina. Platelets. 2007;18(1):16–23. doi: 10.1080/09537100600800412. [DOI] [PubMed] [Google Scholar]
- 15.Bain BJ, Philips D, Thomson K, Richardson D, Gabriel I. Investigation of the effect of marathon running on leukocyte counts of subjects of different ethnic origins: Relevance to the aetiology of ethnic neutropenia. Br J Haematol. 2000;108:483–7. doi: 10.1046/j.1365-2141.2000.01922.x. [DOI] [PubMed] [Google Scholar]
- 16.Samoszuk M, Corwin M, Hazen SL. Effects of human mast cell tryptase and eosinophil granule proteins on the kinetics of blood clotting. Am J Hematol. 2003;73:18–25. doi: 10.1002/ajh.10323. [DOI] [PubMed] [Google Scholar]
- 17.Roy D, Quiles J, Avanzas P, Arroyo-Espliguero R, Sinha M, Kaski JC. A comparative study of markers of inflammation for the assessment of cardiovascular risk in patients presenting to the emergency department with acute chest pain suggestive of acute coronary syndrome. Int J Cardiol. 2006;109:317–21. doi: 10.1016/j.ijcard.2005.06.030. [DOI] [PubMed] [Google Scholar]
- 18.Albert M, Danielson E, Rifai N, Ridker PM. Effect of statin therapy on C-reactive protein levels. The Pravastatin inflammation/CRP evaluation (PRINCE): a randomized trial and cohort study. JAMA. 2001;286:64–70. doi: 10.1001/jama.286.1.64. [DOI] [PubMed] [Google Scholar]
- 19.Altun B, Turkon H, Tasolar H, Beggi H, Altun M, Temiz A, et al. The relationship between high-sensitive troponin T, neutrophil-lymphocyte ratio and SYNTAX score. Scand J Clin Lab Invest. 2014;74:108–15. doi: 10.3109/00365513.2013.860619. [DOI] [PubMed] [Google Scholar]
- 20.Akpek M, Sahin O, Elcik D, Kaya MG. The association of neutrophil/lymphocyte ratio with coronary flow and in-hospital mace in patients with STEMI undergoing primary PCI. Eur Heart J. 2013;27:534–9. [Google Scholar]


