Highlights
-
•
An interparietal inguinal hernia with undescended testis & obstructed external ring is a rare presentation.
-
•
In Interperital hernia, the sac passes between the layers of the abdominal wall.
-
•
Pre-operative diagnosis even with the help of USG & CT is really a challenging issue.
-
•
Treatment is surgical exploration which also confirms the final diagnosis.
Keywords: Interparietal hernia, Spigelian hernia, Inguinal, Abdominal lump, Case report
Abstract
Introduction
An interparietal inguinal hernia is a rare form of hernia. In this type of hernia, the sac passes between the layers of the abdominal wall of the inguinal canal area. Although its treatment is very simple but pre-operative diagnosis is really a challenging issue.
Presentation of case
A 62 years old male patient presented with complaint of a large swelling over right lower abdomen with absence of right testes since birth. The lump was measured 26 × 22 cm in size. Ultrasonography (USG) and Contrast enhanced computed Tomography (CECT) failed to diagnose as interparietal inguinal hernia which was proved intra-operatively. Few cases have been reported in the medical literature like this.
Discussion
Exploration revealed the large abdominal lump presenting as an interparietal inguinal hernia. Hernia sac was lying in between external & internal oblique muscles. The right testis was intraabdominal & atrophied. The external inguinal ring was almost completely obstructed.
Conclusion
An interparietal hernia with undescended testis is a very rare presentation. Even with USG & CT scan diagnosis is very challenging and final diagnosis can be made only intraoperatively.
1. Introduction
The Interparietal hernia with undescended testis is an extremely rare presentation. The sac of the interparietal hernia enters the internal inguinal ring in a manner similar to an indirect inguinal hernia but Instead of passing downward to emerge through the external ring into the scrotum, a sac passes anteriorly between any two layers of the abdominal wall. The preoperative imaging techniques play a significant role in diagnosis of the condition. However, it is reported that both CT and USG are not successful in differentiating the different types of inguinal hernia [1], [2]. In our case also, both USG and CT could not diagnose it as an interparietal hernia, which was finally diagnosed intraoperatively. Our case report is in accordance with Consensus based Surgical Case Report (SCARE criteria) [14].
2. Case report
A 62 years old male patient presented with complaint of a large swelling over right lower abdomen for around 30 years. He also complained of absence of right testis since birth. His bowel habits were normal and there was no urinary complain.There was no history of trauma or any surgical procedure in past. He was chronic bidi smoker for around 40 years.On examination there was a huge lump of 26 × 20 cm, occupying right iliac fossa extending up to umbilicus, right hypochondrium (Fig. 1) right lumbar and inguinal area (Fig. 2). Lump was oval shaped, soft and partially reducible with gurgling sound. Cough impulse was present. Percussion notes were resonant and bowel sounds were present over the lump on auscultation. Testis and cord structure could not be felt on right side and scrotum was also underdeveloped on that side. Per rectal examination revealed mild prostatomegaly. A clinical impression of spigelian hernia was made and USG of abdomen advised. All investigations were within normal limit.USG report suggested the probability of spigelian hernia and advised CT scan for confirmation. CECT was done which showed a defect at lateral border of right rectus muscle with bowel loops inside sac (Fig. 3) and a final diagnosis of Spigelian hernia was made.After establishing the diagnosis of spigelian hernia operative intervention (laparoscopic/Open) planned. As patient was very poor and unable to purchase tacker so laparoscopic plan cancelled and prefer open exploration. Intraoperatively it was found to be interparietal inguinal hernia. Careful exploration revealed the hernia sac coming out of very widely dilated deep inguinal ring (DIR) of about 4 cm diameter and extending forward superiorly and laterally as well as medially and downward to some extent. Testis was intraabdominal and atrophic. External inguinal ring was almost completely obstructed. The external oblique muscle and aponeurosis was extremely thin (Fig. 4) and hernia sac was lying in between external & internal oblique muscles (Fig. 5). A long segment of small gut with their mesentery was the content of the sac. Inferior epigastric vessels were identified just medial to the neck of the sac. A formal herniotomy, right orchidectomy and strengthening of the floor done by preperitoneal placement of proline mesh. Post-operative period was uneventful and patient was discharged on second postoperative day, and he has now been on our follow-up for the last 8 months and is doing well. Informed consent was taken from patient for the publication of this case report and accompanying images.
Fig. 1.
Lump of 26 × 22 cm in right iliac fossa extending up to umbilicus & right hypochondrium.
Fig. 2.
Lateral View showing Lump extending up to right lumbar and inguinal area.
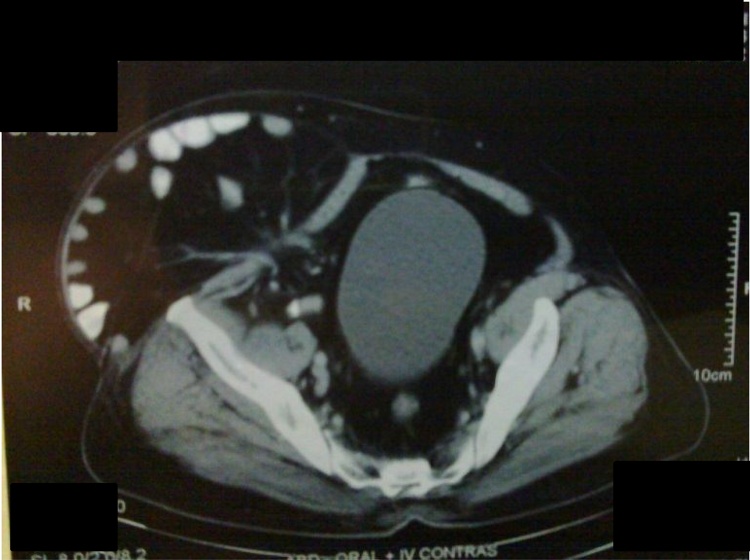
Fig. 3.
CECT showing defect at lateral border of right rectus muscle with bowel loops inside sac.
Fig. 4.
Thinned out External Oblique Aponeurosis.
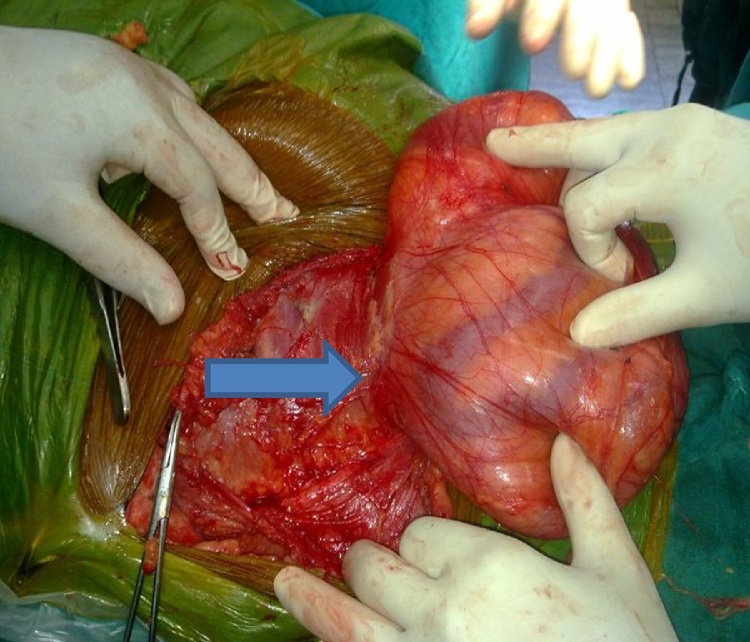
Fig. 5.
Interparietal hernia in the wall of abdominal wall near inguinal area & Arrow shows the external ring.
3. Discussion
Interparietal hernia was first described by Bartolin in 1661 [3]. Lower and Hicken [4] reported 0.01–1.6% incidence of interparietal hernias in his largest series.Recently three subtypes of interparietal hernia have been described. They are preperitoneal (between peritoneum and transversalis fascia), interstitial (between transversalis fascia and transverse, internal oblique or external oblique muscles), and superficial (between external oblique and skin or within aponeurosis of the inguinal region. In our case it was interstitial variety, which is most common of the three subtypes, as reported by Lower and Hicken [4] as comprising around 60 percent. The other two subtypes comprised about 20% each. Another study reported incidence of interstitial variant as 0.084–0.157% of all hernias, with male female ratio of around 5:1 [1]. Spigelian hernia is a protrusion of preperitoneal fat, peritoneal sac, or organs due to a congenital/acquired defect in the linea semilunaris [5], [6]. The line of transition between muscle fibres and the aponeurosis of the transversus abdominis muscle and the lateral border of the rectus sheath defines the semilunar, or Spigelian, zone. A lateral ventral hernia may occur anywhere through the semilunar zone from above the level of the umbilicus to the pubic symphysis [7]. In our case the extent of swelling was from umbilicus to right inguinal ligament. Interparietal like hernia may be the presentation of epigastric hernia [8]. On the other hand here interparietal hernia was presented as Spigelian hernia. The widest portion of the Spigelian fascia is the area where the semilunar line intersects the arcuate line of Douglas (the linea semicircularis). It is in this region, between the umbilicus and the arcuate line, where more than 90% of Spigelian hernias are found. The rearrangement of muscle and fascial fibres at the intersection of the arcuate and semilunar lines is thought to cause an area of functional weakness that is predisposed to hernia formation. CT and ultrasound have been used as a radiological adjunct for diagnosis in doubtful cases [9], [10], [11], [12], [13]. However CT scan is used as a gold standard diagnostic modality in the doubtful case [15]. Even if CT is doubtful, diagnostic laparoscopy is useful with 100% accuracy [16]. Although diagnosis may be challenging but treatment is simple surgical exploration. The approach of surgical exploration may be laparoscopic or open depends upon the surgeon’s choice and the facility available in hospital [17]. The final diagnosis was made only after exploration of the swelling with excision of large hernia sac and right sided orchiectomy. Undescended testis with obstructed external ring may be considered as an important etiological factor in our case. Though interparietal hernias have been reported by many authors but a combination of poorly developed hemiscrotum, completely obstructed external inguinal ring with undescended testis along with giant interparietal hernia is a very rare event as only few cases have been reported in medical literature.
4. Conclusion
A combination of large lower abdominal lump with undescended testis and poorly developed hemiscrotum is a very rare event. Although clinical diagnosis may be challenging but treatment is always surgical exploration. Hence great caution needs to be exercised towards management of patients with such kind of presentation.
Conflict of interests
The authors have no conflicts of interests to disclose.
Funding
No Source to be stated.
Ethical approval
For case report our Institute exempted to take ethical approval.
Consent
Informed consent for the publication of this work has been taken by the patient.
Author contribution
Anil Kumar: Wrote the Manuscript
Shiv Shankar Paswan: Operated the patient.
Anita Paswan: Surgeon responsible for the in-patient optimization
Rekha Kumari: Follow up and Post-operative Pain management.
Vimal Bhandari: Review the manuscript
Guarantor
Dr Anil Kumar.
Contributor Information
Anil Kumar, Email: dranil4@gmail.com.
Shiv Shankar Paswan, Email: drshivanita@gmail.com.
Anita Paswan, Email: anitapaswan@gmail.com.
Rekha Kumari, Email: dr.rekha911@gmail.com.
Vimal Bhandari, Email: vbhandari_24@yahoo.co.in.
References
- 1.Eddy K., Piercy G.B., Eddy Vasitis R. clinical and ultrasound confusion with inguinal hernia clarified by computed tomography. Can. Urol. Assoc. J. 2011;5(August (4)):E74–E76. doi: 10.5489/cuaj.10116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berg J.C.V.D. vol 23. 2002. Inguinal Hernias; pp. 156–173. (RI and Ultrasound. Seminars in Ultrasound, CT and MRI). (2), April. [DOI] [PubMed] [Google Scholar]
- 3.Reddy K.M., Stellakis M.L.C., Khaliq T., AGTW Fiennes. Interparietal hernia mimicking malignant small bowel obstruction. Hernia. 1999;3(1):37–38. PubMed. [Google Scholar]
- 4.Lower W.E., Hicken N.F. Interparietal hernias. Ann. Surg. 1931;94(6):1070–1087. doi: 10.1097/00000658-193112000-00010. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skandalakis P.N., Zoras O., Skandalakis J.E., Mirilas P. Spigelian hernia: surgical anatomy, embryology, and technique of repair. Am. Surg. 2006;72(1):42–48. PubMed. [PubMed] [Google Scholar]
- 6.Rogers F.B., Camp P.C. A strangulated Spigelian hernia mimicking diverticulitis. Hernia. 2001;5(1):51–52. doi: 10.1007/BF01576167. PubMed. [DOI] [PubMed] [Google Scholar]
- 7.Mederos R., Lamas J.R., Alvarado J., Matos M., Padron I., Ramos A. Laparoscopic diagnosis and repair of Spigelian hernia: a case report and literature review. Int. J. Surg. Case Rep. 2017;31:184–187. doi: 10.1016/j.ijscr.2017.01.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Asuquo M.E., Nwagbara V.I.C., Ifere O. Epigatric hernia presenting as giant abdominal interparietal hernia. Int. J. Surg. Case Rep. 2011;2(8):243–245. doi: 10.1016/j.ijscr.2011.07.008. PubMed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Larson D.W., Farley D.R. Spigelian hernias: repair and outcome for 81 patients. World J. Surg. 2002;26:1277–1281. doi: 10.1007/s00268-002-6605-0. PubMed. [DOI] [PubMed] [Google Scholar]
- 10.Zacharakis E., Papadopoulos V., Ganidou M. Incarcerated spigelian hernia: a case report. Med. Sci. Monit. 2006;12:CS64–CS66. PubMed. [PubMed] [Google Scholar]
- 11.Campanelli G., Pettinari D., Nicolosi F.M. Spigelian hernia. Hernia. 2005;9:3–5. doi: 10.1007/s10029-004-0280-z. PubMed. [DOI] [PubMed] [Google Scholar]
- 12.Onal A., Sokmen S., Atila K. Spigelian hernia associated with strangulation of the small bowel and appendix. Hernia. 2003;7:156–157. doi: 10.1007/s10029-003-0118-0. PubMed. [DOI] [PubMed] [Google Scholar]
- 13.Mittal T., Kumar V., Khullar R., Sharma A., Soni V., Baijal M. Diagnosis and management of Spigelian hernia: a review of literature and our experience. J. Minim. Acc. Surg. 2008;4:95–98. doi: 10.4103/0972-9941.45204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Agha Riaz A., Fowler Alexander J., Saeta Alexander, Barai Ishani, Rajmohan Shivanchan, Orgill Dennis P. The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 15.Foster D., Nagarajan S., Panait L. Richter-type Spigelian hernia: a case report and review of the literature. Int. J. Surg. Case Rep. 2015;6:160–162. doi: 10.1016/j.ijscr.2014.10.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bell R.L., Longo W.E. Images for surgeons/spigelian hernia. J. Am. Coll. Surg. 2004;199(1):16. doi: 10.1016/j.jamcollsurg.2003.12.028. [DOI] [PubMed] [Google Scholar]
- 17.Siosaki M.D., Costa M.M.H.C., Figueiredo H.F., Junior M.F.S., Junior R.A.S. A differential diagnosis in chronic lower abdominal pain. Int. J. Surg. Case Rep. 2012;3:504–506. doi: 10.1016/j.ijscr.2012.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]