Abstract
Fewer adults meet guidelines for aerobic physical activity, and many report a lack of enjoyment as a barrier. This survey was designed to determine the interest of primary care patients in participating in program designed to maximize enjoyment. Primary care patients (n = 540) in Central Pennsylvania reported their interest in participating in a “a regular fitness program where people your own age played games, such as softball, floor hockey and soccer, that were made to be easier to play and less competitive.” Mean age was 58.4 years (SD = 16.5, range = 18–98). More than one-third (37.0%), including 59.6% of those under age 50, were interested in the modified sports fitness program. After adjusting for confounders, patients under age 40 were 5.9 (95% CI: 2.6–13.9) times as interested (v. age > 70) and non-white patients were 3.4 (95% CI: 1.3–8.5) times interested. Female patients and those with hypertension, high cholesterol or obesity were equally interested. A fitness program that consists of modified sports may be of interest to most primary care patients under age 50. Patients' initial interest appears high enough to warrant further development and testing.
Keywords: Physical activity, Exercise, Primary care
Highlights
-
•
Most patients under age 50 were interested in a modified sports fitness program.
-
•
Interest was much higher among younger patients and non-white patients.
-
•
Interest was similar among patients of different gender or body mass index.
1. Introduction
“We in America live rather a tense life, under high pressure. Our diversified interests, our many social duties, our multitudinous responsibilities, our insistent worries, even our stimulating climate combine to make our modern life very strenuous, taxing our minds and bodies to the limit. …Hence, the need of relaxation, recreation and play. Psychologists, social workers, religious workers and employers of labor have all awakened in recent years to the importance of play.”
G. Patrick, Science October 1921 (Patrick, 1921).
Although written in 1921, the need for active play remains a public health priority. Greater active and recreational play may help combat high rates of physical inactivity, one of the most common risk factors for premature mortality worldwide, killing an estimated 5.3 million people each year (Wen and Wu, 2012, Mokdad et al., 2004). Large-scale accelerometry studies observe that fewer than 10% of US adults get the recommended amount of aerobic physical activity (Hagstromer et al., 2010). These low rates of activity are consistent with the observation that, though there are > 50 million fitness center memberships in the US, the average membership is used only 4.3 times per month (Dellavigna and Malmendier, 2006).
Although many potential barriers to physical activity (PA) active have been described (Salmon et al., 2003, Reichert et al., 2007), evidence suggests that a key modifiable, and underappreciated, barrier is that most adults simply do not enjoy PA enough to do it regularly. Studies consistently observe that people who enjoy PA are more likely to become active (Conroy et al., 2010, Lee et al., 2016). Recently, Lee and colleagues described an “Exercise-Affect-Adherence” pathway, in which adherence to PA is directly dependent upon the affective response (e.g., enjoyment), as most adults have past experience with physical activity (Lee et al., 2016). Despite this evidence, there are few PA interventions for adults that focus on maximizing enjoyment as a means of increasing adherence.
Gamification of physical activity, such as with sports, provides an opportunity to enhance enjoyment. The Social Networks For Activity Promotion (SNAP) model, developed by one of the authors (LR) (Rovniak et al., 2013), suggests that physical activity enjoyment and participation are influenced by the characteristics of: (a) the built/natural environments in which activity takes place (“where”); (b) the participants who provide companionship before/during/after activity (“with whom”); and (c) the social interactions that take place among participants (“what we do”) (Rovniak et al., 2013, Rovniak et al., 2016a). For example, Pickleball is a version of tennis modified to reduce effort, with a smaller court and plastic ball and, by some estimates, is one of the fastest growing sports in the US (Kilborn, 2014). After observing the joyful social interactions of Pickleball, our team recognized that many other sports could be similarly modified to reduce effort, competitiveness and injuries and thereby overcome many of the key barriers to adult sports participation (Robert Wood Johnson Foundation, 2015).
Encouraging PA in primary care settings is increasingly important as the Affordable Care Act has outlined a change in reimbursement away from visits and procedures (“fee for service”) and toward improving health outcomes (“population health”) (Shaw et al., 2014). Unfortunately, primary care providers (PCPs) often do not counsel their patients about physical activity (Kraschnewski et al., 2013, Carroll et al., 2011) due, in part, to a belief that patients will not follow the advice (Hebert et al., 2012). If programs existed with higher rates of adherence, PCPs may recommend PA more often and use it as a means to control a number of chronic illnesses that PA is proven to reduce, such as hypertension, diabetes, heart disease, osteoporosis, osteoarthritis and others. We set out first to examine whether primary care patients would be interested in such a program.
2. Methods
We created an anonymous questionnaire to understand whether primary care patients would be interested in participating in sports program in which a number of commonly played sports were modified and rotated. We began with the assumption that any sport was modifiable, by making changes to the materials (e.g., lighter lower-pressure balls to reduce injuries), the playing area (e.g., smaller playing area reduces running), and rules (e.g., ultimate Frisbee has specific rules to reduce physical contact), all of which can enhance the enjoyment while minimizing competition and injuries, known barriers to adults sports participation (Robert Wood Johnson Foundation, 2015).
We created a single “yes/no” question to measure interest in a modified sports fitness program. The header read “Would you consider participating in any of the following:” and the modified sports fitness program was described as “a regular fitness program where people your own age played games, such as softball, floor hockey and soccer, that were made to be easier to play and less competitive.” The sports chosen in the question were selected to include a number of commonly-played sports in the US, but were not designed to be comprehensive as the program was in evolution and the list could change.
The survey was performed at two general internal medicine practices in Central Pennsylvania in 2015. Consecutive patients were handed the questionnaire during the clinic check-in process. The following script was created for front desk staff to use: “For the next several weeks, we're asking all patients to fill out this short survey before seeing your doctor. When you're done, please drop it in this box. Thank you very much.” No financial incentive was provided for participation and staff did not review the surveys for completeness before they were placed into the locked box. These methods have been used by our team previously to identify interest in a range of wellness programs offered to our patients as part of a practice-based quality improvement process (Rovniak et al., 2016b, Sciamanna et al., 2014).
In addition to the PA program item, several items were included to understand the health and demographics of the patient population. Mental and physical quality of life were assessed using questions from the CDC's Healthy Days measure (Moriarty et al., 2005). Physical activity was assessed using a single item measure developed by Greenwood and colleagues (Greenwood et al., 2010). Resistance training activities were assessed by a question adapted from the National Health Interview Survey. Quality of life and physical activity responses were categorized into groups approximating tertiles. Weight and height were converted into body mass index (BMI) using standard formulas and cut-points for overweight and obesity according to the 2001 Clinical Guidelines on the Identification, Evaluation and Treatment of Overweight and Obesity in Adults from the National Institutes of Health (Anon., 2000). Demographics, educational level, smoking status and past medical history were assessed using standard self-report measures from the Behavioral Risk Factor Surveillance System.
Separate logistic regressions were used to describe associations between program interest and covariates, including patient demographics and medical history. Adjusted odds ratios and 95% confidence intervals from the logistic regression models were used to control for potential confounders. Variance inflation factor statistics were included in all regression analyses to examine the potential for multicollinearity (Shieh, 2011). Any variable with an acceptably low variance inflation factor was included in the analysis as a covariate. All analyses were performed in SPSS statistical software, version 22.0 (IBM, Inc.). This study was determined to be exempt from review by the Penn State College of Medicine Institutional Review Board as it was intended to improve quality of care by identifying programs that could be developed and offered to our patients.
3. Results
Between June and October 2015, 600 patients were given a survey after checking-in for a PCP visit and 540 surveys were returned, for a response rate of 90.0%. Missing data varied for individual items, ranging from < 1% for smoking status to 9.5% for weight. Demographics, smoking status, and medical history are shown in Table 1. Overall, half of the patients were 60 years or older (50.0%) and most were female (65.8%) and non-smoking (91.6%). In terms of chronic diseases, approximately half (53.1%) reported high blood pressure and one-quarter (25.9%) reported diabetes. Greater than one-third of the sample (37.3%) reported zero days of aerobic physical activity and 36.5% had a BMI > 30, categorized as obese.
Table 1.
Characteristics of primary care patients (N = 540) in Central Pennsylvania, 2015.
| Variable | % |
|---|---|
| Age, y | |
| 18–40 | 16.5 |
| 41–50 | 12.6 |
| 51–60 | 20.9 |
| 61–70 | 26.8 |
| > 70 | 23.2 |
| Sex | |
| Male | 34.2 |
| Female | 65.8 |
| Race | |
| White | 90.3 |
| Non-white | 9.7 |
| Ethnicity | |
| Hispanic | 4.0 |
| Non-Hispanic | 96.0 |
| Education | |
| Some high school, high school graduate, GED | 28.0 |
| Some college (1–3 years) | 26.0 |
| College graduate (4 or more years) | 46.0 |
| Smoking status | |
| Smoker | 8.4 |
| Nonsmoker | 91.6 |
| Have hypertension | 53.1 |
| Have diabetes | 25.9 |
| Have high cholesterol | 49.2 |
| Body mass index, kg/m2 (based on self-reported height and weight) | |
| 18.5–25.0 | 38.5 |
| > 25.0–30.0 | 25.0 |
| > 30.0 | 36.5 |
| Days of aerobic physical activity per week | |
| 0 | 37.3 |
| 1–3 | 37.1 |
| 4–7 | 25.6 |
| Days of strength training per week | |
| 0 | 55.7 |
| 1–3 | 27.5 |
| 4–7 | 16.8 |
| Self-reported health | |
| Excellent, very good, or good | 79.4 |
| Fair or poor | 20.6 |
| Days of poor physical health in the past month | |
| 0 | 34.5 |
| 1–9 | 34.3 |
| ≥ 10 | 31.2 |
| Days of poor mental health in the past month | |
| 0 | 55.4 |
| 1–9 | 21.4 |
| ≥ 10 | 23.2 |
| Interested in a group program to increase muscle strength. | 55.0 |
| Interested in a regular fitness program that includes games. | 37.0 |
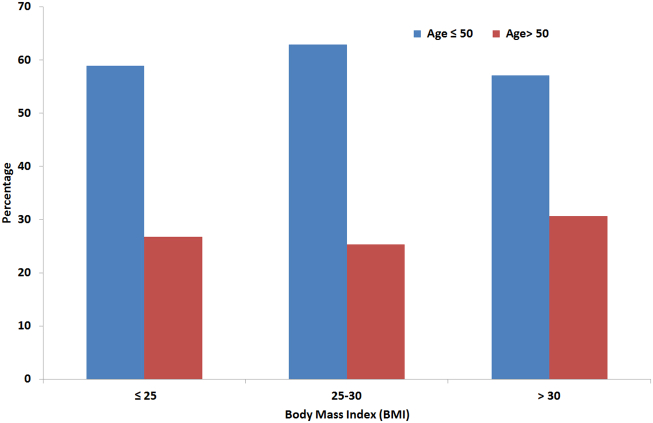
Overall, interest in a modified sports program was modest; slightly more than one-third (37.0%) were interested in the modified sports fitness program. The bivariate relationships between interest in a modified sports fitness program and patient characteristics are shown in Table 2. Younger patients, those with more education and those without chronic conditions and those with better perceived health were more interested in a modified sports fitness program, though the differences were not significant for all comparisons. Further, as seen in Fig. 1, those under 50 years of age were consistently more interested in the modified sports fitness program than those over 50, across all BMI categories.
Table 2.
Association between patient characteristics (N = 540) and interest in a modified sports fitness program.
| Variable | % Interested |
|---|---|
| Age, y | |
| 18–40 | 68.7⁎⁎⁎ |
| 41–50 | 46.8 |
| 51–60 | 34.7 |
| 61–70 | 28.8 |
| > 70 | 12.6 |
| Sex | |
| Male | 34.9 |
| Female | 38.3 |
| Race | |
| White | 35.1⁎⁎⁎ |
| Non-white | 61.4 |
| Ethnicity | |
| Hispanic | 36.8 |
| Non-Hispanic | 37.3 |
| Education | |
| Some high school, high school graduate, GED | 24.8⁎⁎⁎ |
| Some college (1–3 years) | 36.4 |
| College graduate (4 or more years) | 44.7 |
| Smoking status | |
| Smoker | 31.7 |
| Nonsmoker | 37.5 |
| Hypertension | |
| Yes | 30.0⁎⁎⁎ |
| No | 45.3 |
| Diabetes | |
| Yes | 24.2⁎⁎⁎ |
| No | 42.2 |
| High cholesterol | |
| Yes | 29.6⁎⁎⁎ |
| No | 45.8 |
| Body mass index, kg/m2 (based on self-reported height and weight) | |
| 18.5–25.0 | 36.8 |
| > 25.0–30.0 | 35.4 |
| > 30.0 | 38.2 |
| Days of aerobic activity per week | |
| 0 | 28.8⁎ |
| 1–3 | 42.0 |
| 4–7 | 41.6 |
| Days of strength training per week | |
| 0 | 34.1 |
| 1–3 | 42.5 |
| 4–7 | 40.5 |
| Self-reported health | |
| Excellent, very good, or good | 39.0 |
| Fair or poor | 29.0 |
| Days of poor physical health in the past month | |
| 0 | 36.9 |
| 1–9 | 39.8 |
| ≥ 10 | 28.5 |
| Days of poor mental health in the past month | |
| 0 | 37.7 |
| 1–9 | 35.3 |
| ≥ 10 | 38.5 |
Calculated using logistic regression.
p < 0.05.
p < 0.001.
Fig. 1.
Percentage of primary care adult patients interested in a modified sports fitness program, based on age and body mass index; Central Pennsylvania, 2015.
The results of the multivariate regression model, with interest in the modified sports fitness program as the dependent variable, adjusting for all demographic, medical history, self-reported health and behavior variables, can be seen in Table 3. No variance inflation factor was > 5, so all variables were left in the final regression model (Shieh, 2011). After adjusting for covariates, age remained strongly associated with interest in a modified sports fitness program, though the associations between hypertension and high cholesterol were no longer significant. Adults aged 18–40 and adults aged 41–50 were 5.9 (95% CI; 2.6–13.9) times and 3.0 (95% CI; 1.3–7.1) times, respectively, more likely to be interested in a modified sports fitness program than adults over 70, composing 12.6% of our sample. College graduates were 2.1 (95% CI; 1.1–3.6) times as likely to be interested as those who did not complete any years of college. Patients with diabetes were less interested [OR = 0.5 (95% CI; 0.3–0.9)] than those without diabetes. Those reporting 4–7 days of aerobic physical activity were 1.8 (95% CI; 1.2–2.9) times as likely to be interested as those reporting no days of aerobic physical activity. In addition, those reporting excellent, very good or good health were 1.6 (95% CI; 0.7–3.3) times as likely to be interested as those reporting fair or poor health. Non-whites, 9.7% of the sample, were 3.4 (95% CI; 1.3–8.5) times as likely to be interested as whites. Of note, gender and body mass index category were not associated with interest, after adjusting for covariates. In addition, days of poor physical health, days of poor mental health, smoking status and Hispanic ethnicity were not associated with interest in a modified sports program.
Table 3.
Association between interest in modified play and self-reported primary care patient characteristics, adjusted for patient characteristics (N = 540), Central Pennsylvania, 2015.
| Variable | Odds ratio (95% confidence interval) |
|---|---|
| Age, y | |
| 18–40 | 5.9 (2.6–13.9) |
| 41–50 | 3.0 (1.3–7.1) |
| 51–60 | 1.9 (0.9–4.3) |
| 61–70 | 1.5 (0.7–3.0) |
| > 70 | 1 [Reference] |
| Sex | |
| Male | 1.0 (0.6–1.7) |
| Female | 1 [Reference] |
| Race | |
| White | 1 [Reference] |
| Non-white | 3.4 (1.3–8.5) |
| Ethnicity | |
| Hispanic | 0.9 (0.2–3.7) |
| Non-Hispanic | 1 [Reference] |
| Education | |
| Some high school, high school graduate, GED | 1 [Reference] |
| Some college (1–3 years) | 1.8 (0.9–3.5) |
| College graduate (4 or more years) | 2.1 (1.1–3.6) |
| Smoking status | |
| Smoker | 0.7 (0.3–1.9) |
| Nonsmoker | 1 [Reference] |
| Hypertension | |
| Yes | 1.0 (0.6–1.8) |
| No | 1 [Reference] |
| Diabetes | |
| Yes | 0.5 (0.3–0.9) |
| No | 1 [Reference] |
| High cholesterol | |
| Yes | 0.7 (0.4–1.2) |
| No | 1 [Reference] |
| Body mass index, kg/m2 (based on self-reported height and weight) | |
| 18.5–25.0 | 1 [Reference] |
| > 25.0–30.0 | 1.1 (0.6–2.1) |
| > 30.0 | 1.6 (0.9–2.8) |
| Days of aerobic activity per week | |
| 0 | 1 [Reference] |
| 1–3 | 1.8 (1.2–2.8) |
| 4–7 | 1.8 (1.1–2.9) |
| Days of strength training per week | |
| 0 | 1 [Reference] |
| 1–3 | 1.7 (0.9–3.0) |
| 4–7 | 1.3 (0.7–2.7) |
| Self-reported health | |
| Excellent, very good, or good | 1.6 (0.7–3.3) |
| Fair or poor | 1 [Reference] |
| Days of poor physical health in the past month | |
| 0 | 1 [Reference] |
| 1–9 | 1.1 (0.6–1.9) |
| ≥ 10 | 1.0 (0.5–1.9) |
| Days of poor mental health in the past month | |
| 0 | 1 [Reference] |
| 1–9 | 0.7 (0.4–1.4) |
| ≥ 10 | 0.9 (0.5–1.8) |
4. Discussion
In this survey of primary care patients, most adults under age 50 were interested in participating in a modified sports fitness program. This strong inverse relationship between age and interest was not surprising, given the strong relationship with physical limitations and age. Schoenborn and colleagues, for example, observed that only 17.5% of adults aged 55–64 reported difficulty walking 1/4 mile, which increased sharply to over one-half (56.1%) of those over 84 (Schoenborn and Heyman, 2004). We were surprised, however, by the similar levels of interest in men and women and among those with varying levels of BMI. While a recent national survey observed that adult men are more than twice as likely to currently participate in sports as adult women (35% v. 16%) (Robert Wood Johnson Foundation, 2015), these results suggest that participation rates may be more similar if the sports were modified to be easier to play and less competitive.
We also observed that the modified sports fitness program was of greater interest to patients from racial minority groups (OR = 3.4; 95% CI: 1.3–8.5), suggesting that such a program has the potential to address health disparities, given that minorities suffer disproportionately from a number of physical inactivity-related illnesses such as diabetes and hypertension. The observations that interest was higher among patients of higher education level and those who were already more active suggests that some degree of outreach may be needed to maximize the population health gains from such a program. For example, patients reporting 4–7 days of physical activity were 1.8 (95% CI: 1.1–2.9) times as likely to be interested as those reporting zero days of PA. This suggests that if programs are simply offered, many who could benefit (e.g., lower education, lower levels of activity, diabetes) may be less likely to self-refer. Of particular concern was the lower level of interest among patients with diabetes, who were half as interested (OR = 0.5; 95% CI: 0.3–0.9) compared to those without diabetes. Polonsky and colleagues note that fear of low blood sugar while exercising (Polonsky et al., 2015) is a commonly held belief, suggesting that patients with diabetes are in general more concerned about exercising than other patient groups and may need targeted approaches to encourage their participation.
These rates of interest are higher than other reports of actual participation in similar activities, though the other reports generally were not performed in primary care settings, where people are older and suffer from much higher rates of chronic illness than in the general adult population. Ford and colleagues, using data from the 2000 Behavioral Risk Factor Surveillance Study (BRFSS) observed that no sport had an adult participation rate > 5% (Ford et al., 2003), led by golf (4.5%), basketball (3.1%), tennis (1.1%) and softball (1.0%). The level of interest that we observed is similar to findings by Ostbye and colleagues who observed, among women in the military, higher levels of interest in programs that were more social. For example, interest ranged between 8 and 9 (out of a maximum of 10) for a group exercise class versus 4–6 for exercise counseling via e-mail (Ostbye et al., 2003).
These results suggest that a great number of primary care patients under age 50 may be interested in participating in a modified sports fitness program. While our research team continues our work on developing a modified sports fitness program, the high levels of interest observed in this study suggest several actions now. First, providers may consider recommending modified sports activities, such as Pickleball, to their patients. Second, these high levels of interest also suggest that fitness facilities and municipalities that do not offer modified sports, such as Pickleball, may want to consider offering them. A recent article in the Chicago Tribune noted that the number of Pickleball courts in the US doubled from 2000 to 4000 in the previous 7 years and that, in some cases, tennis courts are being replaced with Pickleball courts (Arvia, 2017). This trend creates new opportunities and our results suggest that a large number of patients would be interested. Though the study was not designed to identify the reasons for interest, the interest could have been due to two aspects of the described modified sports fitness program; the play-based nature of the activities (“what we do”) and the social nature of the activity (“with whom”), as described in the SNAP Model (Rovniak et al., 2013, Rovniak et al., 2016a). Perceived enjoyment consistently predicts future physical activity (Conroy et al., 2010, Lee et al., 2016), which suggests that more enjoyable activities may be of greater interest. Interest in social activities may be due to both greater enjoyment from social activities and recent trends toward social isolation. Using daily diaries, Kahneman and colleagues observed that time spent socializing is one of the most enjoyable activities that humans report (Kahneman et al., 2004).
Although the study question is novel and response rate to the survey was high, this study has a number of limitations. First, as it was performed only in Central Pennsylvania, results may not be generalizable to other settings. However, we identified similar rates of obesity to national rates within primary care (68.0%, comparable to the 68.3% in the current study) (Ma et al., 2009). The rates of diabetes and hypertension, however, are higher than reported in other studies. Also conclusions about the increased interest in minority patients is tempered by the low percentage of our patients who were a minority (9.6%), versus the state of Pennsylvania or the US (19.1% and 27.6%, respectively), based on the 2010 US Census. Second, as the survey asked about “interest”, it is not clear whether the individuals who expressed an interest would actually participate if the program was offered. Future studies will be needed to understand whether these high rates of interest translate into high rates of participation. Third, we measured few covariates, increasing the potential for confounding from unmeasured variables (e.g., marital status). For example, the rate of uninsured patients at our medical center is < 5%, below the national level of at least 10% in 2015 (Li et al., 2012). We also measured few medical conditions and no symptoms. The brief and anonymous nature of the survey, designed to maximize the response rate, limited our ability to gather these variables either from patients or from the electronic health record. While this may mean that some of the respondents would have required medical clearance before participating, the conclusions are mainly focused on individuals under age 50 and, after clearance, it is rare for patients that young to be deemed ineligible for physical activity according to standard screening guidelines (Riebe et al., 2015). Fourth, the question used to describe the program was designed only for face validity and may not have been correctly interpreted. Formal testing of the item was not performed, so it is not clear whether slight changes in wording or in the activities listed may have influenced interest. We focused primarily on communicating the physically easier and less competitive nature of the activities (“… made to be easier to play and less competitive”) to differentiate the program from competitive sports leagues which are felt to be intimidating to many lower-skilled players (Baruth et al., 2014).
Despite the above limitations, it appears that if a modified sports fitness program would be of great interest to most primary care patients under age 50, including many with chronic illnesses such as hypertension and high cholesterol. One of the most powerful trends in healthcare today is the movement away from fee-for-service care toward value-based care, where payments will be based on delivering improved health outcomes to populations (Shaw et al., 2014). Given the clear health benefits of physical activity and low rates of participation, a major opportunity exists to develop physical activity programming that maximizes long-term adherence by increasing the perceived enjoyment of the activities. These results suggest that a modified sports fitness program has the potential to be of interest to a large percentage of adults under age 50, creating an opportunity to support healthy habits and prevent or delay the onset of chronic health conditions associated with aging.
5. Conclusion
A fitness program that consists of modified sports may be of interest to most primary care patients under age 50. Patients' initial interest appears high enough to warrant further development and testing.
Conflict of interest statement
No authors have financial or other conflicts of interest pertaining to the work presented.
Acknowledgments
No internal or external grant funding was used to complete this study.
Contributor Information
Christopher N. Sciamanna, Email: cns10@psu.edu.
Andrew J. Mowen, Email: ajm194@psu.edu.
Jennifer L. Kraschnewski, Email: jkraschnewski@pennstatehealth.psu.edu.
Joshua M. Smyth, Email: jms1187@psu.edu.
Liza S. Rovniak, Email: lur12@psu.edu.
David E. Conroy, Email: dec9@psu.edu.
Kalen Kearcher, Email: kkearcher@pennstatehealth.psu.edu.
Courtney Redman, Email: credman@pennstatehealth.psu.edu.
Matthew Silvis, Email: msilvis@pennstatehealth.psu.edu.
Brandon J. Auer, Email: bauer@pennstatehealth.psu.edu.
Ming Wang, Email: mwang@pennstatehealth.psu.edu.
Erik Lehman, Email: elehman@psu.edu.
Dino Messina, Email: dino_messina@brown.edu.
References
- Anon. National Heart, Lung, and Blood Institute; Bethesda, MD: 2000. Clinical Guidelines on the Identification, Evaluation and Treatment of Overweight and Obesity in Adults. [Google Scholar]
- Arvia P. Chicago Tribune; 2017 January 25. The Growth of Pickleball Is on Fire. (Sect. Daily Southtown) [Google Scholar]
- Baruth M., Sharpe P.A., Parra-Medina D., Wilcox S. Perceived barriers to exercise and healthy eating among women from disadvantaged neighborhoods: results from a focus groups assessment. Women Health. 2014;54(4):336–353. doi: 10.1080/03630242.2014.896443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll J.K., Antognoli E., Flocke S.A. Evaluation of physical activity counseling in primary care using direct observation of the 5As. Ann. Fam. Med. 2011;9(5):416–422. doi: 10.1370/afm.1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conroy D.E., Hyde A.L., Doerksen S.E., Ribeiro N.F. Implicit attitudes and explicit motivation prospectively predict physical activity. Ann. Behav. Med. 2010;39(2):112–118. doi: 10.1007/s12160-010-9161-0. [DOI] [PubMed] [Google Scholar]
- Dellavigna S., Malmendier U. Paying not to go to the gym. Am. Econ. Rev. 2006;96(3):694–719. [Google Scholar]
- Ford E.S., Heath G.W., Mannino D.M., Redd S.C. Leisure-time physical activity patterns among US adults with asthma. Chest. 2003;124(2):432–437. doi: 10.1378/chest.124.2.432. [DOI] [PubMed] [Google Scholar]
- Greenwood J.L., Joy E.A., Stanford J.B. The physical activity vital sign: a primary care tool to guide counseling for obesity. J. Phys. Act. Health. 2010;7(5):571–576. doi: 10.1123/jpah.7.5.571. [DOI] [PubMed] [Google Scholar]
- Hagstromer M., Troiano R.P., Sjostrom M., Berrigan D. Levels and patterns of objectively assessed physical activity–a comparison between Sweden and the United States. Am. J. Epidemiol. 2010;171(10):1055–1064. doi: 10.1093/aje/kwq069. [DOI] [PubMed] [Google Scholar]
- Hebert E.T., Caughy M.O., Shuval K. Primary care providers' perceptions of physical activity counselling in a clinical setting: a systematic review. Br. J. Sports Med. 2012;46(9):625–631. doi: 10.1136/bjsports-2011-090734. [DOI] [PubMed] [Google Scholar]
- Kahneman D., Krueger A.B., Schkade D.A., Schwarz N., Stone A.A. A survey method for characterizing daily life experience: the day reconstruction method. Science. 2004;306(5702):1776–1780. doi: 10.1126/science.1103572. [DOI] [PubMed] [Google Scholar]
- Kilborn P.T.A. New York Times; 2014 May 14. Funny Name, a Serious Sport. Pickleball, Anyone? [Google Scholar]
- Kraschnewski J.L., Sciamanna C.N., Stuckey H.L. A silent response to the obesity epidemic: decline in US physician weight counseling. Med. Care. 2013;51(2):186–192. doi: 10.1097/MLR.0b013e3182726c33. [DOI] [PubMed] [Google Scholar]
- Lee H.H., Emerson J.A., Williams D.M. The exercise-affect-adherence pathway: an evolutionary perspective. Front. Psychol. 2016;7:1285. doi: 10.3389/fpsyg.2016.01285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C., Balluz L.S., Ford E.S., Okoro C.A., Zhao G., Pierannunzi C. A comparison of prevalence estimates for selected health indicators and chronic diseases or conditions from the Behavioral Risk Factor Surveillance System, the National Health Interview Survey, and the National Health and Nutrition Examination Survey, 2007–2008. Prev. Med. 2012;54(6):381–387. doi: 10.1016/j.ypmed.2012.04.003. [DOI] [PubMed] [Google Scholar]
- Ma J., Xiao L., Stafford R.S. Adult obesity and office-based quality of care in the United States. Obesity (Silver Spring) 2009;17(5):1077–1085. doi: 10.1038/oby.2008.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokdad A.H., Marks J.S., Stroup D.F., Gerberding J.L. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Moriarty D.G., Kobau R., Zack M.M., Zahran H.S. Tracking healthy days -- a window on the health of older adults. Prev. Chronic Dis. 2005;2(3):A16. [PMC free article] [PubMed] [Google Scholar]
- Ostbye T., McBride C., Demark-Wahnefried W. Interest in healthy diet and physical activity interventions peripartum among female partners of active duty military. Mil. Med. 2003;168(4):320–325. [PubMed] [Google Scholar]
- Patrick G.T.W. The play of a nation. Sci. Mon. 1921;13(4):350–362. [Google Scholar]
- Polonsky W.H., Fisher L., Hessler D., Edelman S.V. Identifying the worries and concerns about hypoglycemia in adults with type 2 diabetes. J. Diabetes Complicat. 2015;29(8):1171–1176. doi: 10.1016/j.jdiacomp.2015.08.002. [DOI] [PubMed] [Google Scholar]
- Reichert F.F., Barros A.J., Domingues M.R., Hallal P.C. The role of perceived personal barriers to engagement in leisure-time physical activity. Am. J. Public Health. 2007;97(3):515–519. doi: 10.2105/AJPH.2005.070144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riebe D., Franklin B.A., Thompson P.D. Updating ACSM's recommendations for exercise preparticipation health screening. Med. Sci. Sports Exerc. 2015;47(11):2473–2479. doi: 10.1249/MSS.0000000000000664. [DOI] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation . 2015 June. Sports and Health in America. Report No. [Google Scholar]
- Rovniak L.S., Sallis J.F., Kraschnewski J.L. Engineering online and in-person social networks to sustain physical activity: application of a conceptual model. BMC Public Health. 2013;13:753. doi: 10.1186/1471-2458-13-753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovniak L.S., Kong L., Hovell M.F. Engineering online and in-person social networks for physical activity: a randomized trial. Ann. Behav. Med. 2016;50(6):885–897. doi: 10.1007/s12160-016-9814-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovniak L.S., Sciamanna C.N., George D.R., Bopp M., Kong L., Ding D. Interest in using workplace energy expenditure devices among primary care patients. J. Prim. Care Community Health. 2016;7(2):96–101. doi: 10.1177/2150131915624892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmon J., Owen N., Crawford D., Bauman A., Sallis J.F. Physical activity and sedentary behavior: a population-based study of barriers, enjoyment, and preference. Health Psychol. 2003;22(2):178–188. doi: 10.1037//0278-6133.22.2.178. [DOI] [PubMed] [Google Scholar]
- Schoenborn C.A., Heyman K.M. Health characteristics of adults aged 55 years and over: United States, 2004–2007. Natl. Health Stat. Rep. 2009;(16):1–31. [PubMed] [Google Scholar]
- Sciamanna C.N., Patel V.A., Kraschnewski J.L. A strength training program for primary care patients, central Pennsylvania, 2012. Prev. Chronic Dis. 2014;11:E107. doi: 10.5888/pcd11.130403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw F.E., Asomugha C.N., Conway P.H., Rein A.S. The patient protection and affordable care act: opportunities for prevention and public health. Lancet. 2014;384(9937):75–82. doi: 10.1016/S0140-6736(14)60259-2. [DOI] [PubMed] [Google Scholar]
- Shieh G. Clarifying the role of mean centring in multicollinearity of interaction effects. Br. J. Math. Stat. Psychol. 2011;64(3):462–477. doi: 10.1111/j.2044-8317.2010.02002.x. [DOI] [PubMed] [Google Scholar]
- Wen C.P., Wu X. Stressing harms of physical inactivity to promote exercise. Lancet. 2012;380(9838):192–193. doi: 10.1016/S0140-6736(12)60954-4. [DOI] [PubMed] [Google Scholar]