Abstract
Purpose
At end of life, spiritual well-being is a central aspect of quality of life for many patients and their family caregivers. A prevalent spiritual value in advanced cancer patients is the need to actively give. To address this need, the current randomized trial examined whether adding a peer helping component to a coping skills intervention leads to improved meaning in life and peace for advanced gastrointestinal cancer patients and their caregivers. Feasibility and acceptability outcomes were also assessed.
Methods
Advanced gastrointestinal cancer patients and caregivers (n=50 dyads) were randomly assigned to a 5-session, telephone-based coping skills intervention or a peer helping + coping skills intervention. One or both dyad members had moderate-severe distress. Peer helping involved contributing to handouts on coping skills for other families coping with cancer. Patients and caregivers completed measures of meaning in life/peace, fatigue, psychological symptoms, coping self-efficacy, and emotional support. Patient pain and caregiver burden were also assessed.
Results
Small effects in favor of the coping skills group were found regarding meaning in life/peace at 1 and 5 weeks post-intervention. Other outcomes did not vary as a function of group assignment, with both groups showing small decreases in patient and caregiver fatigue and caregiver distress and burden. High recruitment and retention rates supported feasibility, and high participant satisfaction ratings supported acceptability.
Conclusions
Although telephone-based intervention is feasible and acceptable for this population, peer helping in the context of a coping skills intervention does not enhance spiritual well-being relative to coping skills alone.
Keywords: gastrointestinal cancer, family caregivers, psychosocial interventions, spiritual well-being, peer helping, distress
Introduction
A growing literature has demonstrated the importance of spiritual well-being, including a sense of meaning in life and peace, for advanced cancer patients and their family caregivers [1–4]. Indeed, meta-analytic evidence suggests that spiritual well-being is associated with better physical and mental quality-of-life (QoL) outcomes in cancer patients across disease stages [5,6]. In a recent meta-analysis, meaning in life in particular showed a moderate, negative association with distress in cancer patients, which supports its clinical relevance [7].
Aspects of spiritual well-being have received less research attention in cancer caregivers; however, growing evidence suggests that higher levels of spiritual well-being (i.e., meaning in life/peace and faith) are correlated with better mental health outcomes in this population [1,2,8]. Some research supports a stress buffering effect of spiritual well-being in cancer caregivers, such that the association between caregiving stress and poorer mental health is attenuated for those with higher levels of spiritual well-being [8,2].
A limited number of interventions have aimed to promote meaning in life in advanced cancer patients [9–14], and this work has yet to be adapted for cancer caregivers [15]. Examples of these interventions include meaning-centered psychotherapy [10] and dignity therapy [13]. Meaning-centered psychotherapy involves didactics, discussion, and experiential exercises regarding sources of meaning in life (e.g., creativity, love), whereas dignity therapy involves reflecting on one’s legacy, which is recorded and transcribed into a document to share with loved ones. In multiple randomized trials, both meaning-centered psychotherapy and dignity therapy have shown positive short-term effects on spiritual well-being and other QoL outcomes [13,12,9–11].
A novel approach to improving meaning in life in advanced cancer patients and caregivers is helping others in similar circumstances. Indeed, the need to actively give was among the most prevalent spiritual needs reported by advanced cancer patients [3]. According to the helper therapy principle [16], helping others can increase psychological and physical well-being in the helper. Consistent with this principle, results of correlational research in the general population suggest that volunteering is associated with reduced physical symptoms, improved emotional well-being and purpose in life, and better social functioning [17–20]. However, this principle has rarely been experimentally tested. For example, one study randomly assigned hematopoietic stem cell transplant survivors to one of four conditions: peer helping (writing about transplant experiences to help others prepare for the procedure), expressive writing (writing expressively about their transplant experience), expressive helping (combination of peer helping and expressive writing), or neutral writing (writing a factual narrative of transplantation) [21]. Although there were no main effects of condition on distress, subgroup analyses showed that among survivors with greater survivorship problems, expressive helping reduced distress compared to peer helping and neutral writing. Another trial with patients with multiple sclerosis found that a coping skills group involving didactics and the provision of telephone support to a peer resulted in better psychosocial role performance and well-being than controls (i.e., receiving telephone peer support) [22].
To our knowledge, peer helping interventions have yet to be tested with cancer caregivers, although correlational evidence suggests that volunteering to help others outside of one’s family is associated with mental health benefits in various caregiving populations [23,24]. Researchers have theorized that volunteering offsets the burden of family caregiving through increasing external resources (e.g., informational and social resources) and internal resources (e.g., feelings of status or emotional gratification) [25].
In this study, we examined the potential spiritual benefits of adding a peer helping component to a coping skills intervention for advanced gastrointestinal (GI) cancer patients and their family caregivers. We chose to focus on this population due to the high prevalence of this cancer [26] and its significant symptom burden [27–29]. Patient-caregiver dyads were randomly assigned to one of two telephone-based interventions: coping skills or peer helping (PH) + coping skills. Dyads assigned to the coping skills condition learned evidence-based coping skills for managing fatigue, pain, depressive symptoms, and anxiety as well as improving social functioning [30–33]. Framed by Social Cognitive Theory [34,35], the intervention was designed to enhance coping self-efficacy through goal setting and skill practice. In the PH + coping skills condition, the same content was discussed and practiced, but the dyad also assisted the therapist in creating an informational resource for other families coping with cancer. This resource consisted of handouts with coping skills for addressing common QoL concerns (e.g., stress, fatigue). As participants aimed to reduce others’ suffering through sharing personal wisdom on handouts, their sense of meaning or purpose in life was expected to increase.
This study tested the feasibility, acceptability, and preliminary efficacy of the interventions. We hypothesized that the interventions would be feasible as indicated by adequate recruitment, retention, and session completion. We also hypothesized that the interventions would be acceptable as indicated by participant satisfaction ratings. Consistent with theories of volunteerism [18,36], we expected that the PH + coping skills group would experience increased meaning in life and peace relative to the coping skills group. We also compared the interventions with respect to their impact on secondary outcomes (i.e., patient and caregiver fatigue, depressive symptoms, anxiety, general distress, coping self-efficacy, and emotional support; patient pain; and caregiver burden).
Methods
Participants
Eligible patients had been diagnosed with stage IV GI cancer at least 8 weeks prior to enrollment and had a consenting primary family caregiver. Patients were excluded from study participation if they 1) had severe cognitive impairment defined as 3 or more errors on a six-item cognitive screener [37], 2) had a self-reported Eastern Cooperative Oncology Group (ECOG) score > 2 [38,39], or 3) were receiving hospice care at the time of enrollment. Eligible caregivers lived with the patient or had visited the patient at least twice a week for the past month. In addition, both patients and caregivers had to be adults (≥18 years of age) who were fluent in English, and one or both dyad members had to report moderate to severe distress, defined as a score of 3 or higher on the Distress Thermometer [40,41].
Procedures
Participants were recruited from the Indiana University Simon Cancer Center and the Roudebush VA Medical Center in Indianapolis, IN between August 2015 and August 2016. All study procedures received institutional review board approval. Following confirmation of initial patient eligibility via chart review and consultation with the oncologist, a research assistant approached the patient during an oncology clinic visit to describe the study. Interested patients identified their primary family caregiver and were screened for eligibility. With the patient’s written consent, caregivers were approached in clinic or through telephone for eligibility screening and consent.
Consenting dyads completed baseline telephone assessments and were randomly assigned to either the coping skills or PH + coping skills group. Randomization was performed by a person who was not a study interviewer or therapist using a SAS procedure and was stratified by study therapist (KC or DT) and patient performance status (self-reported ECOG scores 0 or 1 vs. 2). Participants in both groups completed follow-up telephone assessments at 1 and 5 weeks post-intervention and received $25 gift cards for each assessment. Trained research assistants administering the assessments were blind to study condition.
Measures
Primary and secondary outcomes were assessed with valid self-report measures that have been used with cancer patients and caregivers.
Primary Outcome
The 8-item meaning/peace subscale of the Functional Assessment of Chronic Illness Therapy-Spiritual Well-Being Scale (FACIT-Sp) [42] was used to assess a sense of meaning in life and peace in patients and caregivers.
Secondary Outcomes
Regarding physical symptoms, the 6-item Patient Reported Outcomes Measurement Information System (PROMIS) short-form fatigue measure assessed patient and caregiver fatigue, and the 3-item PROMIS pain intensity measure assessed patient pain [43,44]. Regarding psychological symptoms, the 6-item PROMIS short-form depression measure and 6-item PROMIS short-form anxiety measure were used to assess patient and caregiver depressive and anxiety symptoms, respectively [45]. For all PROMIS measures, responses are summed to form a raw score that can be converted to a T-score with a mean of 50 and a standard deviation of 10. Additionally, the Distress Thermometer [41,40] was used to assess patient and caregiver distress on a scale from 0 (no distress) to 10 (extreme distress). Finally, the coping confidence subscale of the Measure of Current Status (MOCS) [46] was used to assess patient and caregiver self-efficacy for coping with challenging situations.
Regarding social functioning, the 4-item PROMIS short-form emotional support measure assessed the perceived availability of emotional support [47]. Finally, the 12-item short form of the Zarit Burden Interview assessed personal and role strain associated with caregiving [48].
Sociodemographics, Medical Variables, and Volunteer Activity
Patients and caregivers reported their demographic information and mental health service use at baseline. Patient medical information was obtained through medical record review. In addition, at baseline, patients and caregivers rated their frequency of volunteer work during the past month on a 5-point scale from 0 (never or almost never–0 times per month) to 5 (daily–30 times per month) [49].
Feasibility, Acceptability, and Treatment Fidelity
Feasibility was assessed through study accrual and retention rates. Acceptability was examined through posttreatment ratings of the helpfulness of the number and length of the sessions, topics, therapist, and telephone format on a scale from 1 (did not help at all) to 5 (extremely helpful). Participants also reported whether the sessions met their expectations and their confidence in recommending the treatment to families coping with cancer on a scale from 1 (not at all) to 5 (extremely).
Fidelity checklists were developed for both study conditions, and a study psychologist used them to evaluate coverage of session topics, in-session exercises, and home practice assignments. Fidelity scores were the number of correctly delivered topics divided by the total number of fidelity criteria.
Study Groups
Participants in both study groups (PH + coping skills and coping skills) were asked to complete five weekly 50 to 60-minute telephone sessions. Both dyad members participated simultaneously via speakerphone, and all sessions were audiorecorded. Both study conditions were delivered by Ph.D. students in clinical psychology who were trained and supervised by two psychologists. Training involved didactics and role-plays of treatment sessions detailed in manuals. Following the initial training, students received weekly supervision from the psychologists who listened to audiorecordings of sessions and provided feedback on treatment quality and adherence to the manual.
Peer Helping + Coping Skills Group
Dyads in this condition helped create an informational resource on various QoL issues for other patients and caregivers coping with cancer. The dyad was told that this resource would be available to others in print and on-line at the conclusion of the study. Each person was mailed identical handouts that were drafts of the informational resource and a CD with instructions for relaxation exercises. A summary of the intervention components is found in Table 1.
Table 1.
Summary of Topics Covered in Both Study Conditions
| Topic | Selected Session Content |
|---|---|
| Session 1: Managing Physical Symptoms–Part 1 |
|
| Session 2: Managing Physical Symptoms–Part 2 |
|
| Session 3: Managing Stress |
|
| Session 4: Maintaining Relationships |
|
| Session 5: Review |
|
The first four sessions had a similar format. The therapist introduced the session topic (e.g., physical symptoms, stress, social changes) and asked about the dyad’s experiences related to the topic. Then the therapist asked the dyad for their advice (e.g., “What advice would you give to other cancer patients [family members] for dealing with stress?”). Next, the dyad reviewed handouts listing evidence-based coping skills related to the session topic and indicated which skills may be most helpful to others. This was followed by in-session practice of one or more coping skills and/or self-evaluation of their use of coping skills. Following in-session practice of a coping skill, the dyad indicated whether the skill should be included in the informational resource for others. Finally, each dyad member set a goal for the upcoming week related to the session focus, and goal progress was assessed during the subsequent session.
Following the fourth session, the dyad received the handouts with their edits and additions that would be an informational resource for others. During the fifth session, the dyad was asked to critique the handouts further and discuss their use of the skills on the handouts during the past 2 weeks. Then the dyad was asked to provide final advice for others on coping with cancer. Finally, each dyad member was asked to set a goal for the coming week related to one of the session topics.
Coping Skills Group
Dyads in the coping skills condition discussed the same topics as the PH + coping skills condition, but did not help create an informational resource for other patients and caregivers. The same therapists administered both study conditions. Coping skills participants received the same initial handouts and CD with relaxation exercises and completed the same in-session practice of skills and weekly goal setting. Instead of providing advice to others or critiquing the helpfulness of the skills for others, dyads focused on the helpfulness of the skills for themselves. To equalize the time across study conditions, coping skills participants spoke at greater length about their use of coping skills.
Statistical Analyses
Descriptive statistics were computed to examine feasibility and acceptability indicators. Using t-tests (or, where appropriate, Mann-Whitney U tests), study conditions were compared with respect to intervention satisfaction. Baseline comparisons of study conditions (Fisher’s exact tests and t-tests) were also conducted for patients and caregivers separately. Potential gender differences were assessed. Linear mixed-model repeated-measures analyses in SPSS were used to evaluate the preliminary efficacy of PH + coping skills. As these analyses use all available data, an intent-to-treat framework was employed. Multi-level modeling for dyadic data, an approach that addresses the non-independence of data from members of the same dyad, was used for outcomes reported by patients and caregivers [50,51]. Models included the main effect of time, study group, and role (patient or caregiver) and time × group and time × group × role interaction effects. Both time and study group were categorical variables in these models, which focuses the analysis on mean differences across groups and time. Treatment effects are evidenced either by a significant study group main effect or a significant interaction between time and study group. A significant time × study group × role interaction indicates that the treatment effects are different for patients and caregivers. For outcomes that only patients or caregivers reported, models included the main effects of time and study group and the time × group interaction. Gender was not included in the models because only two outcomes varied by gender (data not shown).
Results
Feasibility and Acceptability
Study Enrollment and Participation
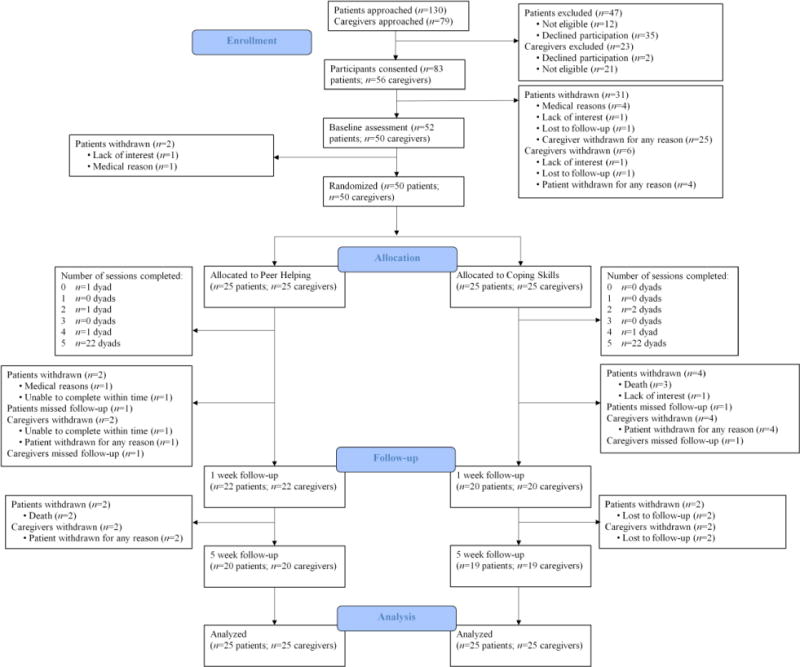
As shown in Figure 1, of 130 GI cancer patients who were approached regarding this study, 35 declined participation, 12 were ineligible, and 83 consented. Patients agreeing to the eligibility screening did not differ from refusers with respect to age, gender, or race (all ps>.10). Of the 79 caregivers who were approached, 2 declined participation and 21 were ineligible. Thus, 56 dyads were eligible and consented to participate. Primary reasons for study refusal were that the patient or caregiver had time constraints, did not like talking on the phone, or were not interested in the study. Six dyads withdrew prior to randomization because of medical reasons, lack of interest, or loss to follow-up. Twenty-five of the remaining 50 dyads were randomized to the PH + coping skills intervention, and 25 were randomized to the coping skills intervention. Retention was high, with 22 dyads in each intervention condition completing all 5 sessions and the 1-week follow-up. Most dyads (39/50, 78%) also completed the 5-week follow-up.
Fig. 1.
Study flow chart
Treatment Fidelity and Participant Satisfaction
All sessions were digitally recorded. Fidelity to the intervention manual was rated for 20% of the sessions, and the average fidelity rating was 99%. Participants rated both telephone interventions favorably with respect to helpfulness and confidence in recommending the intervention to other families coping with cancer (see Table 2). Therapists’ helpfulness was also highly rated. Small, statistically significant differences in favor of the PH + coping skills intervention were found for most aspects of intervention satisfaction (see Table 2).
Table 2.
Patient and Caregiver Intervention Satisfaction
| Peer Helping + Coping Skills | Coping Skills | ||||
|---|---|---|---|---|---|
|
|
|||||
| Intervention Satisfactiona | Mean (SD) | Mean (SD) | df | t/U | P |
| Telephone sessions met expectationsb | 4.40 (0.70) | 3.93 (0.80) | 81 | 2.87 | 0.01 |
| Number of sessions was helpfulc | 3.95 (0.73) | 3.50 (0.85) | 80 | −2.59 | 0.01 |
| Length of sessions was helpfulc | 3.98 (0.90) | 3.33 (1.00) | 80 | −3.11 | 0.00 |
| Topics of the sessions were helpfulc,d | 4.09 (0.75) | 3.90 (1.06) | 70 | −0.95 | 0.34 |
| Therapist was helpfulc,d | 4.74 (0.49) | 4.53 (0.68) | 71 | −1.67 | 0.10 |
| Use of the telephone was helpfulc,d | 4.58 (0.63) | 4.08 (1.10) | 61 | −2.56 | 0.01 |
| Confidence in recommending this treatment to families coping with cancerb,e | 4.70 (0.51) | 4.33 (1.00) | – | 691.00 | 0.07 |
df = degrees of freedom. SD = standard deviation. Ns = 82–83 participants.
Intervention satisfaction was assessed at 1-week post-intervention.
Rated on a 5-point Likert scale (1 = Not at all, 5 = Extremely).
Rated on a 5-point Likert scale (1 = Did not help at all, 5 = Extremely helpful).
Statistics for the t-test not assuming homogeneity of variance are presented.
Statistics for the Mann-Whitney U test are presented.
Participant Characteristics
Table 3 presents demographic and medical data by study group and group comparisons at baseline. Most patients had been diagnosed with colorectal (38%) or pancreatic cancer (26%). The majority of caregivers (76%) were spouses or partners of the patient. Demographics, medical factors, volunteer activity, and outcome variables at baseline did not vary by study condition.
Table 3.
Patient and Caregiver Characteristics and Group Comparisons at Baseline
| Patients (n = 50)
|
Caregivers (n = 50)
|
|||||
|---|---|---|---|---|---|---|
| Characteristics | Peer Helping + Coping Skills (n = 25) | Coping Skills (n = 25) | t-test/Fisher’s Exact Test p | Peer Helping + Coping Skills (n = 25) | Coping Skills (n = 25) | t-test/Fisher’s Exact Test p |
| Sex, n (%) | 1.00 | 1.00 | ||||
| Male | 16 (64.00) | 15 (60.00) | 9 (36.00) | 8 (32.00) | ||
| Female | 9 (36.00) | 10 (40.00) | 16 (64.00) | 17 (68.00) | ||
| Age | 0.67 | 0.46 | ||||
| Mean | 58.88 | 57.48 | 55.32 | 52.40 | ||
| SD | 11.50 | 11.65 | 12.23 | 15.11 | ||
| Range | 41–82 | 33–81 | 35–83 | 21–73 | ||
| Race, n (%) | ||||||
| Non-Hispanic white | 21 (84.00) | 22 (88.00) | 1.00 | 22 (88.00) | 22 (88.00) | 1.00 |
| Missing | 1 (4.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | ||
| Employment status, n (%) | 0.38 | 0.86 | ||||
| Employed full or part-time | 9 (36.00) | 5 (20.00) | 15 (60.00) | 14 (56.00) | ||
| Retired | 9 (36.00) | 9 (36.00) | 6 (24.00) | 5 (20.00) | ||
| Unemployed | 7 (28.00) | 11 (44.00) | 4 (16.00) | 6 (24.00) | ||
| Household income, n (%) | 0.75 | 0.45 | ||||
| $0 – $50,999 | 7 (28.00) | 10 (40.00) | 6 (24.00) | 9 (36.00) | ||
| $51,000 – $99,999 | 10 (40.00) | 9 (36.00) | 8 (32.00) | 12 (48.00) | ||
| $100,000 or more | 6 (24.00) | 5 (20.00) | 7 (28.00) | 4 (16.00) | ||
| Missing | 2 (8.00) | 1 (4.00) | 4 (16.00) | 0 (0.00) | ||
| Years of education | 0.38 | 0.07 | ||||
| Mean | 14.96 | 14.28 | 15.16 | 14.04 | ||
| SD | 2.54 | 2.84 | 2.06 | 2.13 | ||
| Range | 11–20 | 9–21 | 12–19 | 11–19 | ||
| Caregiver relationship to the patient, n (%) | 0.32 | |||||
| Spouse/partner | — | — | 21 (84.00) | 17 (68.00) | ||
| Other family member | — | — | 4 (16.00) | 8 (32.00) | ||
| Caregiver lives with the patient, n (%) | 22 (88.00) | 20 (80.00) | 0.70 | |||
| Married/living with a partner, n (%) | 21 (84.00) | 17 (68.00) | 0.32 | 25 (100.00) | 21 (84.00) | 0.11 |
| Psychiatric medication, n (%)a | 13 (52.00) | 7 (28.00) | 0.15 | 7 (28.00) | 6 (24.00) | 1.00 |
| Psychotherapy/counseling, n (%)a | 2 (8.00) | 1 (4.00) | 1.00 | 0 (0.00) | 1 (4.00) | 1.00 |
| Study site, n (%) | 1.00 | |||||
| Indiana University Simon Cancer Center | 25 (100.00) | 24 (96.00) | ||||
| Roudebush VA Medical Center | 0 (0.00) | 1 (4.00) | ||||
| Type of gastrointestinal cancer, n (%) | 0.36 | |||||
| Colorectal | 10 (40.00) | 9 (36.00) | — | — | ||
| Pancreatic | 8 (32.00) | 5 (20.00) | — | — | ||
| Esophageal | 1 (4.00) | 5 (20.00) | — | — | ||
| Other | 6 (24.00) | 6 (24.00) | — | — | ||
| Time since diagnosis in years | 0.69 | |||||
| Mean | 1.63 | 1.43 | — | — | ||
| SD | 2.14 | 1.24 | — | — | ||
| Range | 0.18–10.27 | 0.18–4.79 | — | — | ||
| Treatments received, n (%) | ||||||
| Chemotherapy | 23 (92.00) | 24 (96.00) | 1.00 | — | — | |
| Radiation | 1 (4.00) | 5 (20.00) | 0.19 | — | — | |
| Surgery to remove primary tumor | 15 (60.00) | 13 (52.00) | 0.78 | — | — | |
| Surgery to remove metastases | 5 (20.00) | 7 (28.00) | 0.74 | — | — | |
| Targeted therapy | 8 (32.00) | 9 (36.00) | 1.00 | — | — | |
| Patient ECOG score | 0.26 | |||||
| Mean | 0.76 | 1.00 | — | — | ||
| SD | 0.78 | 0.71 | — | — | ||
| Range | 0–2 | 0–2 | — | — | ||
| Distress Thermometer score at screening | 0.61 | 0.53 | ||||
| Mean | 3.20 | 3.56 | 5.32 | 4.88 | ||
| SD | 2.75 | 2.10 | 2.51 | 2.46 | ||
| Range | 0–9 | 0–9 | 0–9 | 1–10 | ||
| Volunteer activity | 1.00 | 0.50 | ||||
| Mean | 0.92 | 0.92 | 0.72 | 0.92 | ||
| SD | 1.04 | 1.38 | 0.89 | 1.19 | ||
SD = standard deviation; ECOG = Eastern Cooperative Oncology Group.
Treatment received in the past month at baseline.
At baseline, 12% of patients and 30% of caregivers had PROMIS anxiety T-scores ≥ 60 (+1 SD), indicating high levels of anxiety. Also at baseline, 8% of patients and 12% of caregivers had PROMIS depression T-scores ≥ 60, indicating high levels of depressive symptoms. Regarding physical symptoms, at baseline, 48% of patients and 32% of caregivers had PROMIS fatigue T-scores ≥ 60, suggesting high levels of fatigue. In addition, at baseline, 4% of patients had PROMIS pain T-scores ≥ 60, suggesting high levels of pain.
Preliminary Efficacy
Table 4 presents means for the primary and secondary outcomes and results from the mixed-model analyses.
Table 4.
Intent-to-Treat Results for Multilevel Linear Models Predicting Outcomes (n = 50 Dyads)
| Peer Helping + Coping Skills | Coping Skills | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| Baseline | 1 Week Post-intervention | 5 Weeks Post-intervention | Baseline | 1 Week Post-intervention | 5 Weeks Post-intervention | ||||
|
|
|||||||||
| Outcome Fixed Effect | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | df | F | P |
| Primary Outcome:
|
|||||||||
| Patient meaning in life/peace | 25.40 (6.16) | 24.95 (7.63) | 24.65 (8.00) | 23.36 (6.18) | 25.20 (5.27) | 24.80 (4.37) | |||
| Caregiver meaning in life/ | 23.88 (4.48) | 25.18 (4.73) | 23.75 (4.73) | 21.52 (4.92) | 23.90 (4.61) | 24.63 (5.20) | |||
| peace | |||||||||
| Group | 49 | 0.38 | 0.54 | ||||||
| Time | 76 | 3.37 | 0.04 | ||||||
| Role | 45 | 0.75 | 0.39 | ||||||
| Time × role | 72 | 2.34 | 0.10 | ||||||
| Group × time | 76 | 5.26 | 0.01 | ||||||
| Group × role | 45 | 0.21 | 0.65 | ||||||
| Group × time × role | 72 | 0.28 | 0.76 | ||||||
| Secondary Outcomes:
|
|||||||||
| Patient fatigue | 17.44 (5.64) | 17.43 (6.24) | 16.00 (6.74) | 19.28 (5.44) | 18.80 (5.53) | 17.35 (6.71) | |||
| Caregiver fatigue | 16.32 (4.80) | 14.23 (3.77) | 15.50 (5.46) | 17.88 (5.39) | 15.65 (5.40) | 14.84 (5.04) | |||
| Group | 49 | 1.07 | 0.31 | ||||||
| Time | 79 | 7.08 | 0.00 | ||||||
| Role | 43 | 4.94 | 0.03 | ||||||
| Time × role | 73 | 1.43 | 0.25 | ||||||
| Group × time | 79 | 0.94 | 0.40 | ||||||
| Group × role | 43 | 0.12 | 0.73 | ||||||
| Group × time × role | 73 | 0.12 | 0.89 | ||||||
| Patient pain | 6.24 (2.79) | 6.05 (3.02) | 5.75 (2.45) | 6.16 (2.37) | 6.45 (2.67) | 6.35 (3.07) | |||
| Group | 48 | 0.09 | 0.77 | ||||||
| Time | 79 | 0.15 | 0.86 | ||||||
| Group × time | 79 | 0.39 | 0.68 | ||||||
| Patient depressive symptoms | 9.52 (4.14) | 9.76 (5.58) | 9.00 (4.38) | 9.96 (3.81) | 9.90 (3.48) | 10.35 (4.85) | |||
| Caregiver depressive | 10.44 (3.42) | 8.86 (3.03) | 9.85 (3.39) | 11.92 (4.73) | 10.50 (4.68) | 10.80 (4.63) | |||
| symptoms | |||||||||
| Group | 49 | 0.45 | 0.51 | ||||||
| Time | 80 | 2.55 | 0.09 | ||||||
| Role | 43 | 1.57 | 0.22 | ||||||
| Time × role | 78 | 2.29 | 0.11 | ||||||
| Group × time | 80 | 0.32 | 0.73 | ||||||
| Group × role | 43 | 0.60 | 0.44 | ||||||
| Group × time × role | 78 | 0.53 | 0.59 | ||||||
| Patient anxiety symptoms | 9.88 (3.83) | 10.19 (5.22) | 9.50 (3.41) | 10.64 (3.94) | 10.70 (4.61) | 11.25 (5.96) | |||
| Caregiver anxiety symptoms | 11.72 (3.47) | 10.91 (4.72) | 11.25 (4.45) | 14.16 (5.34) | 11.40 (4.76) | 11.80 (4.54) | |||
| Group | 49 | 0.83 | 0.37 | ||||||
| Time | 81 | 1.88 | 0.16 | ||||||
| Role | 46 | 6.23 | 0.02 | ||||||
| Time × role | 81 | 2.93 | 0.06 | ||||||
| Group × time | 81 | 0.96 | 0.39 | ||||||
| Group × role | 46 | 0.06 | 0.81 | ||||||
| Group × time × role | 81 | 1.14 | 0.33 | ||||||
| Patient general distress | 2.76 (2.39) | 3.10 (2.49) | 2.65 (2.46) | 4.00 (2.55) | 3.60 (2.14) | 4.25 (2.85) | |||
| Caregiver general distress | 4.96 (1.84) | 3.73 (2.19) | 3.65 (2.21) | 4.72 (2.32) | 3.70 (2.39) | 4.00 (2.65) | |||
| Group | 48 | 0.54 | 0.47 | ||||||
| Time | 77 | 2.57 | 0.08 | ||||||
| Role | 41 | 6.49 | 0.02 | ||||||
| Time × role | 75 | 3.69 | 0.03 | ||||||
| Group × time | 77 | 0.55 | 0.58 | ||||||
| Group × role | 41 | 2.86 | 0.10 | ||||||
| Group × time × role | 75 | 0.61 | 0.55 | ||||||
| Patient coping self-efficacy | 2.96 (0.67) | 2.84 (0.89) | 2.85 (0.89) | 2.98 (0.64) | 2.99 (0.59) | 2.89 (0.68) | |||
| Caregiver coping self-efficacy | 2.86 (0.62) | 3.01 (0.56) | 2.78 (0.62) | 2.68 (0.61) | 2.68 (0.59) | 2.67 (0.69) | |||
| Group | 49 | 0.25 | 0.62 | ||||||
| Time | 77 | 1.31 | 0.28 | ||||||
| Role | 47 | 1.36 | 0.25 | ||||||
| Time × role | 75 | 1.03 | 0.36 | ||||||
| Group × time | 77 | 0.06 | 0.94 | ||||||
| Group × role | 47 | 2.91 | 0.10 | ||||||
| Group × time × role | 75 | 1.27 | 0.29 | ||||||
| Patient emotional support | 18.52 (2.00) | 18.43 (2.54) | 17.75 (2.99) | 18.52 (1.96) | 18.55 (2.11) | 17.70 (2.87) | |||
| Caregiver emotional support | 16.20 (4.27) | 17.86 (2.93) | 17.20 (3.22) | 17.84 (2.44) | 17.45 (2.61) | 17.37 (2.73) | |||
| Group | 47 | 0.37 | 0.55 | ||||||
| Time | 80 | 1.64 | 0.20 | ||||||
| Role | 44 | 4.58 | 0.04 | ||||||
| Time × role | 77 | 2.84 | 0.07 | ||||||
| Group × time | 80 | 1.64 | 0.20 | ||||||
| Group × role | 44 | 0.35 | 0.56 | ||||||
| Group × time × role | 77 | 2.81 | 0.07 | ||||||
| Caregiver caregiving burden | 14.36 (7.44) | 12.32 (7.91) | 13.00 (9.57) | 14.64 (8.40) | 10.85 (7.01) | 11.63 (8.70) | |||
| Group | 47 | 0.09 | 0.76 | ||||||
| Time | 78 | 4.74 | 0.01 | ||||||
| Group × time | 78 | 0.66 | 0.52 | ||||||
df = degrees of freedom; SD = standard deviation.
Primary Outcome
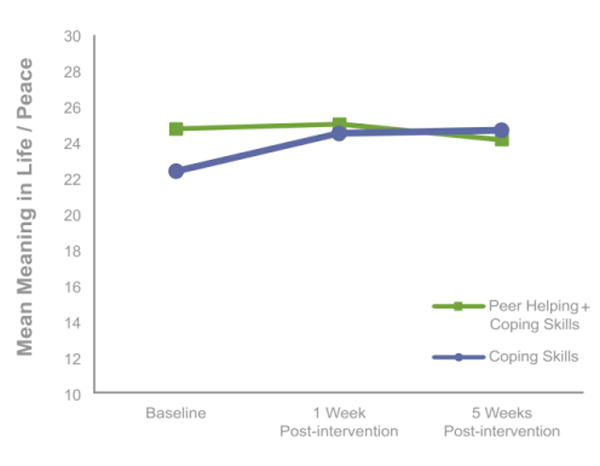
Mixed-model dyadic analyses revealed a significant time × group effect on meaning in life/peace (d=.53, p=.01; see Table 4). As shown in Figure 2, means were relatively stable over time for the PH + coping skills group, whereas means for the coping skills group showed a small increase at 1 week post-intervention, which was maintained at the 5-week follow-up.
Fig. 2.
Changes in meaning in life/peace by study group
Secondary Outcomes
Results from the mixed-model dyadic analyses revealed no main effects of study group or time × group effects on fatigue, anxiety, depressive symptoms, general distress, coping self-efficacy, or emotional support (ds=.06-.30). However, there were significant main effects of role and time on fatigue, indicating that patients, on average, had higher levels of fatigue than caregivers, and both patients and caregivers experienced small decreases in fatigue over time. In addition, there was a main effect of role on anxiety symptoms, such that caregivers, on average, had higher levels of anxiety than patients. Furthermore, there was a time × role effect on general distress. Means found in Table 4 show relatively stable distress for patients over time, whereas caregivers had small decreases in distress at both followups relative to baseline. Finally, there was a main effect of role on emotional support, such that patients, on average, reported higher levels of emotional support than caregivers.
Regarding individual outcomes, mixed-model analyses showed no main effects of study group or time × group effects on patient pain or caregiver burden (ds=.08-.18). However, there was a main effect of time on caregiver burden, with both groups showing small decreases in burden at both follow-ups relative to baseline.
Discussion
This study supports the feasibility and acceptability of 5-session, telephone-based dyadic coping skills interventions for advanced GI cancer patients and their caregivers. The majority (73%) of patients agreed to the eligibility screening and all eligible patients consented to participate, which exceeds recruitment rates of other telephone-based dyadic interventions in cancer [52]. Although participants rated both interventions as helpful, the ratings were slightly higher for the PH + coping skills intervention. Retention was high, with most attrition being due to death or medical factors.
Although the interventions were acceptable to participants, results did not support our hypothesis that the PH + coping skills group would experience higher levels of meaning in life and peace than the coping skills group. Instead, this outcome was stable over time for the PH + coping skills group and showed a small increase in the coping skills group. Furthermore, compared to coping skills alone, the PH + coping skills intervention did not have an impact on patient pain, caregiver burden, or patient and caregiver fatigue, mental health outcomes, or social outcomes. These outcomes did not change over time, with the exception of small decreases in patient and caregiver fatigue and caregiver general distress and burden. Taken together, results do not support the efficacy of our brief, telephone-based dyadic interventions for advanced GI cancer patients and caregivers.
To date, limited research has examined dyadic psychosocial interventions in advanced cancer [53–55] or peer helping interventions in cancer [21,56]; thus, few comparisons of this trial to prior research can be made. For example, one study tested a six-session telephone dyadic intervention in which advanced lung cancer patients and caregivers learned various coping skills and found large effects on patient and caregiver mental health outcomes relative to usual care [54]. Another trial testing a four-session telephone intervention to enhance the coping skills of primarily advanced lung cancer patient-caregiver dyads did not find effects on patient physical symptoms or patient and caregiver mental health outcomes relative to an education/support condition [57]. Regarding peer helping interventions, the two published intervention trials with cancer patients, examining Internet support groups [56] and expressive writing [21], have yielded mixed findings. Given the scarce literature and methodological differences across studies, few conclusions may be drawn at this time.
Several potential explanations for the current findings warrant mention. First, a brief intervention involving the creation of educational materials for peers may not be sufficient to increase a sense of meaning in life and peace in advanced GI cancer patients and caregivers. Although the need to actively give is a prevalent spiritual value for advanced cancer patients [3], other resources (e.g., social support) and challenges (e.g., physical decline) may have a greater impact on their meaning in life and peace. Further research is needed to identify culture-specific factors that may be targeted to bolster patient and caregiver meaning in life and peace towards the end of life.
Another possible explanation for our results is that the brevity of the intervention and telephone delivery lessened its impact. Meta-analytic findings regarding the effect of intervention dose on cancer patient and caregiver outcomes have been mixed [52,58]. Additionally, the cancer literature has not yielded evidence that telephone delivery of psychosocial interventions is inferior to in-person delivery; however, intervention modalities have rarely been compared [58]. Further work is needed to determine the optimal intervention dose and modality for advanced cancer patients and caregivers.
Sample characteristics may have also influenced the current results. Despite the inclusion requirement that one or both dyad members endorse moderate distress, rates of clinically meaningful distress were relatively low, with the exception of caregiver anxiety. Additionally, both patients and caregivers, on average, endorsed moderately high levels of meaning in life/peace and coping self-efficacy; thus, there was little room for positive change during the intervention period. Furthermore, null findings may be related to the perception of participants in both groups that they were helping others through research participation.
Finally, a usual care group was not included in this study. This group may have shown worsening outcomes over time relative to the intervention conditions. Three-arm trials are needed to examine intervention components relative to usual care.
Several research directions may build upon the current findings. First, examining different types of helping (e.g., direct vs. indirect helping) and formats (e.g., dyadic vs. individual) might elucidate conditions in which helping confers spiritual or health benefits for helpers. In addition, if peer helping is found to benefit helpers, then determining the mechanisms underlying this effect would advance theory. For example, theory suggests that enhanced coping self-efficacy or meaning in life may help explain positive effects of peer helping or volunteerism on mental health [18,36]. Finally, having a clinically meaningful distress criterion for study entry would ensure generalizability of study findings to those who warrant psychosocial care.
Limitations of this study should be noted. Participants were primarily Caucasian, middle class, and residing in the Midwestern United States. Thus, results may not generalize to ethnic minorities, people with low incomes, or those from other geographic regions. Additionally, the low prevalence of clinically elevated depressive symptoms in patients and caregivers and anxiety in patients may have reduced intervention impact. Finally, this trial was underpowered for detecting moderators of intervention effects. Further work is needed to determine for whom the interventions are most efficacious.
In conclusion, this study is one of the first to show that dyadic telephone interventions are feasible and acceptable to advanced GI cancer patients and caregivers. Although the addition of peer helping to a coping skills intervention did not produce spiritual benefits, it warrants further experimental study due to the ubiquity of peer support and its associations with positive health outcomes for helpers in the general population [59]. Identifying ways to promote the spiritual well-being of advanced cancer patients and caregivers is central to improving their QoL.
Acknowledgments
Catherine Mosher’s work was supported by the National Cancer Institute under Grants K05CA175048 and K07CA168883. Victoria Champion’s work was supported by Grant K05CA175048 from the National Cancer Institute. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute. This material is the result of work supported with resources and the use of facilities at the Roudebush VA Medical Center in Indianapolis, IN. The content does not represent the views of the U.S. Department of Veterans Affairs or the United States Government. The authors would like to thank the study participants, the study therapists, Kelly Chinh and Danielle B. Tometich, and Susan Daily for her assistance.
Footnotes
Compliance with Ethical Standards
Conflict of Interest: The authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
Contributor Information
Catherine E. Mosher, Department of Psychology, Indiana University-Purdue University Indianapolis, 402 North Blackford Street, LD 124, Indianapolis, IN 46202, USA, Phone: 1-317-274-6769
Ekin Secinti, Department of Psychology, Indiana University-Purdue University Indianapolis, 402 North Blackford Street, LD 124, Indianapolis, IN 46202, USA
Shelley A. Johns, Indiana University School of Medicine, Center for Health Services Research, Regenstrief Institute, 1101 W. 10th Street, RF-226, Indianapolis, IN 46202, USA.
Bert H. O’Neil, Department of Medicine, Indiana University School of Medicine, Indiana Cancer Pavilion, 535 Barnhill Drive, Room 473, Indianapolis, IN 46202, USA
Paul R. Helft, Department of Medicine, Indiana University School of Medicine, Indiana Cancer Pavilion, 535 Barnhill Drive, Room 473, Indianapolis, IN 46202, USA
Safi Shahda, Department of Medicine, Indiana University School of Medicine, Indiana Cancer Pavilion, 535 Barnhill Drive, Room 473, Indianapolis, IN 46202, USA
Shadia I. Jalal, Department of Medicine, Indiana University School of Medicine, Indiana Cancer Pavilion, 535 Barnhill Drive, Room 473, Indianapolis, IN 46202, USA
Victoria L. Champion, Indiana University School of Nursing, 1111 Middle Drive, NU 340G, Indianapolis, IN 46202, USA
References
- 1.Kim Y, Carver CS, Spillers RL, Crammer C, Zhou ES. Individual and dyadic relations between spiritual well-being and quality of life among cancer survivors and their spousal caregivers. Psycho-Oncology. 2011;20(7):762–770. doi: 10.1002/pon.1778. [DOI] [PubMed] [Google Scholar]
- 2.Colgrove LA, Kim Y, Thompson N. The effect of spirituality and gender on the quality of life of spousal caregivers of cancer survivors. Annals of Behavioral Medicine. 2007;33(1):90–98. doi: 10.1207/s15324796abm3301_10. [DOI] [PubMed] [Google Scholar]
- 3.Hocker A, Krull A, Koch U, Mehnert A. Exploring spiritual needs and their associated factors in an urban sample of early and advanced cancer patients. European Journal of Cancer Care. 2014;23(6):786–794. doi: 10.1111/ecc.12200. [DOI] [PubMed] [Google Scholar]
- 4.Lo C, Zimmermann C, Gagliese L, Li M, Rodin G. Sources of spiritual well-being in advanced cancer. BMJ Supportive and Palliative Care. 2011;1(2):149–153. doi: 10.1136/bmjspcare-2011-000005. [DOI] [PubMed] [Google Scholar]
- 5.Jim HS, Pustejovsky JE, Park CL, Danhauer SC, Sherman AC, Fitchett G, et al. Religion, spirituality, and physical health in cancer patients: A meta-analysis. Cancer. 2015;121(21):3760–3768. doi: 10.1002/cncr.29353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salsman JM, Pustejovsky JE, Jim HS, Munoz AR, Merluzzi TV, George L, et al. A meta-analytic approach to examining the correlation between religion/spirituality and mental health in cancer. Cancer. 2015;121(21):3769–3778. doi: 10.1002/cncr.29350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Winger JG, Adams RN, Mosher CE. Relations of meaning in life and sense of coherence to distress in cancer patients: a meta-analysis. Psycho-Oncology. 2016;25(1):2–10. doi: 10.1002/pon.3798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim Y, Wellisch D, Spillers R, Crammer C. Psychological distress of female cancer caregivers: effects of type of cancer and caregivers’ spirituality. Supportive Care in Cancer. 2007;15(12):1367–1374. doi: 10.1007/s00520-007-0265-4. [DOI] [PubMed] [Google Scholar]
- 9.Breitbart W, Poppito S, Rosenfeld B, Vickers AJ, Li Y, Abbey J, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. Journal of Clinical Oncology. 2012;30(12):1304–1309. doi: 10.1200/JCO.2011.36.2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Breitbart W, Rosenfeld B, Gibson C, Pessin H, Poppito S, Nelson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psycho-Oncology. 2010;19(1):21–28. doi: 10.1002/pon.1556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Breitbart W, Rosenfeld B, Pessin H, Applebaum A, Kulikowski J, Lichtenthal WG. Meaning-centered group psychotherapy: an effective intervention for improving psychological well-being in patients with advanced cancer. Journal of Clinical Oncology. 2015;33(7):749–754. doi: 10.1200/JCO.2014.57.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chochinov HM, Kristjanson LJ, Breitbart W, McClement S, Hack TF, Hassard T, et al. Effect of dignity therapy on distress and end-of-life experience in terminally ill patients: a randomised controlled trial. Lancet Oncology. 2011;12(8):753–762. doi: 10.1016/S1470-2045(11)70153-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chochinov HM, Hack T, Hassard T, Kristjanson LJ, McClement S, Harlos M. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. Journal of Clinical Oncology. 2005;23(24):5520–5525. doi: 10.1200/JCO.2005.08.391. [DOI] [PubMed] [Google Scholar]
- 14.Piderman KM, Johnson ME, Frost MH, Atherton PJ, Satele DV, Clark MM, et al. Spiritual quality of life in advanced cancer patients receiving radiation therapy. Psycho-Oncology. 2014;23(2):216–221. doi: 10.1002/pon.3390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Applebaum AJ, Kulikowski JR, Breitbart W. Meaning-Centered Psychotherapy for Cancer Caregivers (MCP-C): Rationale and overview. Palliative and Supportive Care. 2015;13(6):1631–1641. doi: 10.1017/S1478951515000450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reissman F. The helper therapy principle. Social Work. 1965;10(2):27–32. [Google Scholar]
- 17.Greenfield EA, Marks NF. Formal volunteering as a protective factor for older adults’ psychological well-being. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2004;59(5):S258–264. doi: 10.1093/geronb/59.5.s258. [DOI] [PubMed] [Google Scholar]
- 18.Piliavin JA, Siegl E. Health benefits of volunteering in the Wisconsin longitudinal study. Journal of Health and Social Behavior. 2007;48(4):450–464. doi: 10.1177/002214650704800408. [DOI] [PubMed] [Google Scholar]
- 19.Thoits PA, Hewitt LN. Volunteer work and well-being. Journal of Health and Social Behavior. 2001;42(2):115–131. [PubMed] [Google Scholar]
- 20.Musick MA, Wilson J. Volunteering and depression: the role of psychological and social resources in different age groups. Social Science and Medicine. 2003;56(2):259–269. doi: 10.1016/s0277-9536(02)00025-4. [DOI] [PubMed] [Google Scholar]
- 21.Rini C, Austin J, Wu LM, Winkel G, Valdimarsdottir H, Stanton AL, et al. Harnessing benefits of helping others: a randomized controlled trial testing expressive helping to address survivorship problems after hematopoietic stem cell transplant. Health Psychology. 2014;33(12):1541–1551. doi: 10.1037/hea0000024. [DOI] [PubMed] [Google Scholar]
- 22.Schwartz CE. Teaching coping skills enhances quality of life more than peer support: Results of a randomized trial with multiple sclerosis patients. Health Psychology. 1999;18(3):211–220. doi: 10.1037//0278-6133.18.3.211. [DOI] [PubMed] [Google Scholar]
- 23.van Campen C, de Boer AH, Iedema J. Are informal caregivers less happy than noncaregivers? Happiness and the intensity of caregiving in combination with paid and voluntary work. Scandinavian Journal of Caring Sciences. 2013;27(1):44–50. doi: 10.1111/j.1471-6712.2012.00998.x. [DOI] [PubMed] [Google Scholar]
- 24.Shen HW, Pickard JG, Johnson SD. Self-esteem mediates the relationship between volunteering and depression for African American caregivers. Journal of Gerontological Social Work. 2013;56(5):438–451. doi: 10.1080/01634372.2013.791907. [DOI] [PubMed] [Google Scholar]
- 25.Moen P, Robison J, Dempster-McClain D. Caregiving and women’s well-being: a life course approach. Journal of Health and Social Behavior. 1995;36(3):259–273. [PubMed] [Google Scholar]
- 26.American Cancer Society. Cancer facts and figures 2017. Atlanta, GA: American Cancer Society; 2017. [Google Scholar]
- 27.Krouse RS. Gastrointestinal cancer. In: Holland JC, Breitbart WS, Jacobsen PB, Lederberg MS, Loscalzo MJ, McCorkle R, editors. Psycho-Oncology. 2nd. New York: Oxford University Press; 2010. pp. 140–145. [Google Scholar]
- 28.Pettersson G, Bertero C, Unosson M, Borjeson S. Symptom prevalence, frequency, severity, and distress during chemotherapy for patients with colorectal cancer. Supportive Care in Cancer. 2014;22(5):1171–1179. doi: 10.1007/s00520-013-2069-z. [DOI] [PubMed] [Google Scholar]
- 29.Clark KL, Loscalzo M, Trask PC, Zabora J, Philip EJ. Psychological distress in patients with pancreatic cancer–an understudied group. Psycho-Oncology. 2010;19(12):1313–1320. doi: 10.1002/pon.1697. [DOI] [PubMed] [Google Scholar]
- 30.Porter LS, Keefe FJ, Garst J, Baucom DH, McBride CM, McKee DC, et al. Caregiver-assisted coping skills training for lung cancer: Results of a randomized clinical trial. Journal of Pain and Symptom Management. 2011;41(1):1–13. doi: 10.1016/j.jpainsymman.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moorey S, Greer S. Cognitive-behavioral therapy for people with cancer. New York: Oxford University Press; 2002. [Google Scholar]
- 32.Barlow J, Wright C, Sheasby J, Turner A, Hainsworth J. Self-management approaches for people with chronic conditions: a review. Patient Education and Counseling. 2002;48(2):177–187. doi: 10.1016/s0738-3991(02)00032-0. [DOI] [PubMed] [Google Scholar]
- 33.Keefe FJ, Abernethy AP, Campbell LC. Psychological approaches to understanding and treating disease-related pain. Annual Review of Psychology. 2005;56:601–630. doi: 10.1146/annurev.psych.56.091103.070302. [DOI] [PubMed] [Google Scholar]
- 34.Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice-Hall; 1977. [Google Scholar]
- 35.Bandura A. Health promotion by social cognitive means. Health Education and Behavior. 2004;31(2):143–164. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 36.Morrow-Howell N. Volunteering in later life: Research frontiers. The Journals of Gerontology: Series B. 2010;65B(4):461–469. doi: 10.1093/geronb/gbq024. [DOI] [PubMed] [Google Scholar]
- 37.Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Medical Care. 2002;40(9):771–781. doi: 10.1097/00005650-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Bauer J, Capra S, Ferguson M. Use of the scored Patient-Generated Subjective Global Assessment (PG-SGA) as a nutrition assessment tool in patients with cancer. European Journal of Clinical Nutrition. 2002;56(8):779–785. doi: 10.1038/sj.ejcn.1601412. [DOI] [PubMed] [Google Scholar]
- 39.Dajczman E, Kasymjanova G, Kreisman H, Swinton N, Pepe C, Small D. Should patient-rated performance status affect treatment decisions in advanced lung cancer? Journal of Thoracic Oncology. 2008;3(10):1133–1136. doi: 10.1097/JTO.0b013e318186a272. [DOI] [PubMed] [Google Scholar]
- 40.Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, Holland JC. Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer. 1998;82(10):1904–1908. doi: 10.1002/(sici)1097-0142(19980515)82:10<1904::aid-cncr13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 41.National Comprehensive Cancer Network. Distress management. Clinical practice guidelines. Journal of the National Comprehensive Cancer Network. 2003;1(3):344–374. doi: 10.6004/jnccn.2003.0031. [DOI] [PubMed] [Google Scholar]
- 42.Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: the functional assessment of chronic illness therapy–Spiritual Well-being Scale (FACIT-Sp) Annals of Behavioral Medicine. 2002;24(1):49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- 43.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. Journal of Clinical Epidemiology. 2010;63(11):1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cella D, Yount S, Rothrock N, Gershon R, Cook K, Reeve B, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS): progress of an NIH Roadmap cooperative group during its first two years. Medical Care. 2007;45(5 Suppl 1):S3–S11. doi: 10.1097/01.mlr.0000258615.42478.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS(R)): depression, anxiety, and anger. Assessment. 2011;18(3):263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carver CS. Measure of Current Status. 2006 http://www.psy.miami.edu/faculty/ccarver/sclMOCS.html.
- 47.Hahn EA, DeWalt DA, Bode RK, Garcia SF, DeVellis RF, Correia H, et al. New English and Spanish social health measures will facilitate evaluating health determinants. Health Psychology. 2014;33(5):490–499. doi: 10.1037/hea0000055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bedard M, Molloy DW, Squire L, Dubois S, Lever JA, O’Donnell M. The Zarit Burden Interview: a new short version and screening version. Gerontologist. 2001;41(5):652–657. doi: 10.1093/geront/41.5.652. [DOI] [PubMed] [Google Scholar]
- 49.Okun MA, August KJ, Rook KS, Newsom JT. Does volunteering moderate the relation between functional limitations and mortality? Social Science and Medicine. 2010;71(9):1662–1668. doi: 10.1016/j.socscimed.2010.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kenny D, Kashy D, Cook W. Dyadic data analysis. New York: Guilford Press; 2006. [Google Scholar]
- 51.Atkins DC. Using multilevel models to analyze couple and family treatment data: basic and advanced issues. Journal of Family Psychology. 2005;19(1):98–110. doi: 10.1037/0893-3200.19.1.98. [DOI] [PubMed] [Google Scholar]
- 52.Badr H, Krebs P. A systematic review and meta-analysis of psychosocial interventions for couples coping with cancer. Psycho-Oncology. 2013;22(8):1688–1704. doi: 10.1002/pon.3200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Keefe FJ, Ahles TA, Sutton L, Dalton J, Baucom D, Pope MS, et al. Partner-guided cancer pain management at the end of life: A preliminary study. Journal of Pain and Symptom Management. 2005;29(3):263–272. doi: 10.1016/j.jpainsymman.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 54.Badr H, Smith CB, Goldstein NE, Gomez JE, Redd WH. Dyadic psychosocial intervention for advanced lung cancer patients and their family caregivers: Results of a randomized pilot trial. Cancer. 2015;121(1):150–158. doi: 10.1002/cncr.29009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McLean LM, Walton T, Rodin G, Esplen MJ, Jones JM. A couple-based intervention for patients and caregivers facing end-stage cancer: outcomes of a randomized controlled trial. Psycho-Oncology. 2013;22(1):28–38. doi: 10.1002/pon.2046. [DOI] [PubMed] [Google Scholar]
- 56.Lepore SJ, Buzaglo JS, Lieberman MA, Golant M, Greener JR, Davey A. Comparing standard versus prosocial Internet support groups for patients with breast cancer: A randomized controlled trial of the Helper Therapy Principle. Journal of Clinical Oncology. 2014;32(36):4081–4086. doi: 10.1200/JCO.2014.57.0093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mosher CE, Winger JG, Hanna N, Jalal SI, Einhorn LH, Birdas TJ, et al. Randomized pilot trial of a telephone symptom management intervention for symptomatic lung cancer patients and their family caregivers. Journal of Pain and Symptom Management. 2016;52(4):469–482. doi: 10.1016/j.jpainsymman.2016.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Northouse LL, Katapodi MC, Song L, Zhang L, Mood DW. Interventions with family caregivers of cancer patients: meta-analysis of randomized trials. CA: A Cancer Journal for Clinicians. 2010;60(5):317–339. doi: 10.3322/caac.20081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Konrath S, Brown S. The effects of giving on givers. In: Newman ML, Roberts NA, editors. Health and social relationships: The good, the bad, and the complicated. Washington, DC: American Psychological Association; 2013. pp. 39–64. [Google Scholar]


