Abstract
Background
Although, the variable pattern of asthmatic symptoms is well recognized, little is known about the respiratory symptoms variability in patients of chronic obstructive pulmonary disease (COPD). The present study evaluated the variability of the respiratory symptoms in a day and their influence on the daily activities in a cohort of Chinese COPD patients.
Methods
An observational cross-sectional study was conducted in 11 medical centers of China. Participants were outpatient ≥40 years old with stable COPD, post-bronchodilator forced expiratory volume in 1 second (FEV1) <80% predicted. Overall, data of 1,032 eligible patients were valid for final analysis.
Results
Mean post bronchodilator FEV1 (predicted %) was 46.5%. Cough, expectoration and dyspnea were the most commonly observed symptoms (73.6%, 68.8% and 61.4%, respectively). Daily symptom variability was experienced by 50.2% of symptomatic patients. The wake up time in the morning was the worst and the most troublesome time during the day (39.3%), followed by the nighttime (21.3%). The morning activities were most affected by COPD symptoms. Multivariate analyses revealed that COPD assessment test (CAT) scores was the only factor correlated with patients’ symptom variability [odds ratio (OR) =0.463, P<0.0001].
Conclusions
Patient-perceived symptoms vary during the day in Chinese COPD patients. They experience the greatest increase in respiratory symptoms early in the morning. This variation should be considered as a potential new target in the long-term COPD management.
Keywords: Chinese, chronic obstructive pulmonary disease (COPD), COPD assessment test (CAT), quality of life, symptom variability
Introduction
Chronic obstructive pulmonary disease (COPD) is mainly characterized by persistent airflow limitation that is usually not fully reversible. The commonest symptoms are chronic cough, sputum production and breathlessness that are generally described as slowly progressive (1). Although, the disease has also been recognized as having a high level of heterogeneity with different rates of progression, they usually keep clinical stability between exacerbations (2). However, this traditional paradigm has been contested in recent decades. Several studies have reported that COPD-related symptoms are not uniformly perceived by patients in a similar manner, showing not just seasonal variation, but also changes in symptom perception over a week or even during a single day (3-9). This time-dependent variation is of substantial importance, since it has an impact on everyday life activities and health-related quality of life (HRQoL) (5). In studies that investigated day-to-day variation, up to 40% of patients reported diurnal variations that impacted their daily activities and QoL. These variations were shown to be associated with episodes of severe breathlessness and frequent exacerbations (5). European studies have reported significant differences in the characteristics and the variability of the COPD symptoms amid geographical areas and this justifies an in-depth analysis of the data from various regions (5-7), However, the symptom variability of COPD has not been well studied in Chinese patients to date.
The prevalence of COPD in adults was 8.2% in China that has made it the fourth leading cause of death (10). Therefore, in order to understand more details; the present study aimed to evaluate a global perception of the symptoms and their variability in COPD patients through a multicenter survey in China. Moreover, we also aimed to ascertain the determinants of the variability.
Methods
Subjects and study design
This was a multicenter, observational, and cross-sectional study conducted between December 2012 and November 2013, in 11 medical hospitals of China. The study protocol was approved by the institutional review board at each participating center. All the participating patients signed the informed consent.
For inclusion in the study, the patients needed to fulfill all the following criteria: (I) outpatients aged ≥40 years; (II) clinical diagnosis of COPD for ≥6 months; (III) forced expiratory volume in 1 second (FEV1) <80% predicted and FEV1/forced vital capacity (FVC) <0.7 (post-bronchodilator).
The exclusion criteria were: (I) patients who had an ongoing or had experienced an exacerbation in the previous 3 months; (II) history of asthma or rhinitis; (III) patients who had been diagnosed with left ventricular dysfunction, lung cancer or any other major respiratory diseases such as bronchiectasis, interstitial lung disease, pulmonary fibrosis, tuberculosis or sarcoidosis; (IV) currently enrolled in a clinical trial; (V) not able to understand the study procedure.
For each patient at the inclusion visit and after the informed consent was signed, the physicians recorded the demographic information, time since COPD diagnosis, smoking status, other comorbidities, lung function measurements, Medical Research Council (MRC) dyspnea scores, the COPD assessment test (CAT) scores, exacerbations and previous hospitalizations as well as current COPD medication.
In addition, the patient was queried regarding his/her COPD symptoms, especially dyspnea, cough, expectoration, chest distress and wheezing. Patients were also asked about the variability of the symptoms during the day and the time when the symptoms were most likely to occur such as on waking up, later in the morning, during the afternoon, in the evening and at night. Furthermore, patients were also questioned about the impact of the symptoms on morning activities, including getting up, dressing, washing up, having breakfast and performing post-breakfast indoor and outdoor activities.
Statistical analysis
Statistical analyses were performed using SAS 9.2 software. The significance level was established at 5%. Quantitative variables were expressed as mean and standard deviation. Qualitative variables were described by the absolute frequencies and relevant percentage of each variable. Factors significantly associated with symptom variability were identified using a univariate analysis of individual dependent variables. All factors with a P<0.05 in the univariate analysis were then included into a logistic regression model.
Results
Patient characteristics
Of 1,058 patients, 1,032 eligible patients were included for the final analysis. Table 1 demonstrates their baseline characteristics. All the patients were of Asian origin. About 28.5% reported having cardiovascular disease, including hypertension and ischemic heart disease, and 5.5% reported having diabetes. A total of 986 patients had available information on COPD medication; 54.9% were on regular treatment, whereas the others received medications only during exacerbations. The exact medication time prescribed by physicians was unknown to 27.9% of the patients. Morning medication was prescribed to 377 patients (38.0%), with 48.5% taking medications within 30 minutes after getting up, 31.6% after 1 hour of getting up, while only 3.2% before getting up.
Table 1. Baseline characteristics of the study population.
| Variables | N=1,032 [mean ± SD] [n (%)] |
|---|---|
| Age (years) | 64.9±9.2 |
| Male/female | 835/197 (81/19) |
| BMI (kg/m-2) | 23.3±3.7 |
| Smoking status | |
| Nonsmoker | 185 (17.9) |
| Current smoker | 252 (24.4) |
| Ex-smoker | 595 (57.7) |
| Residence | |
| Urban | 651 (63.1) |
| Rural | 381 (36.9) |
| Lung function (post-bronchodilator values) | |
| FEV1 (L) | 1.23±0.47 |
| FVC (L) | 2.56±0.80 |
| FEV1 (% predicted) | 46.5±15.4 |
| GOLD airflow limitation grading | |
| Moderate | 414 (40.1) |
| Severe | 442 (42.8) |
| Very severe | 176 (17.1) |
| History of exacerbations | |
| Last 3 years | 385 (37.3) |
BMI, body mass index; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
Frequency of symptoms and variability
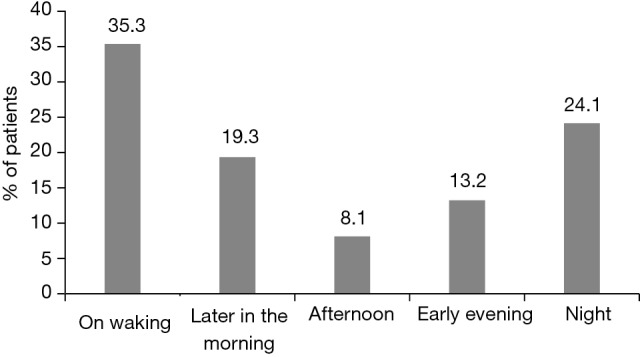
Among 1,032 patients, 1,025 (99.3%) reported having ≥ one symptom, and the other seven patients had none of the typical symptoms of COPD, including cough, breathlessness, wheezing, chest distress, and sputum production. Of the 1,025 symptomatic patients, cough occurred most frequently (73.6%), followed by expectoration (68.8%) and breathlessness (61.4%) (Figure 1). It is observed that dyspnea, chest tightness, and wheezing are the symptoms that become prominent as lung function worsen. However, cough and expectoration are often perceived as constant (Figure 2). As shown in Figure 3, 50.2% of the patients reported variation in their symptoms over the course of the day, and symptoms variability was associated with the degree of airflow limitation. The perception of changes in COPD symptoms was found to be higher in the very severe group (59.7%), followed by severe (52.4%) and moderate (44%) groups. Furthermore, patients perceiving symptom variability reported that “on waking in the morning” (39.3%) and “at night” (21.3%) was the most probable occurring time and the most problematic time (Figures 4,5).
Figure 1.
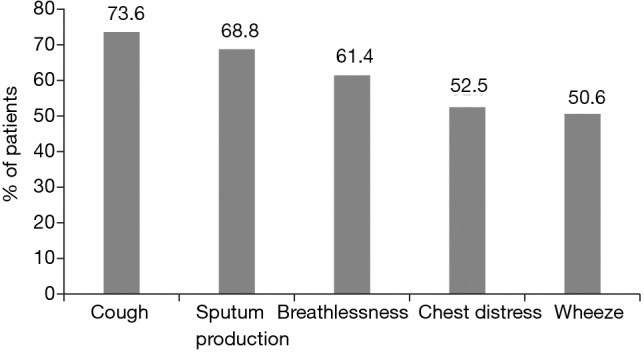
Frequency of respiratory symptoms in the population analyzed.
Figure 2.
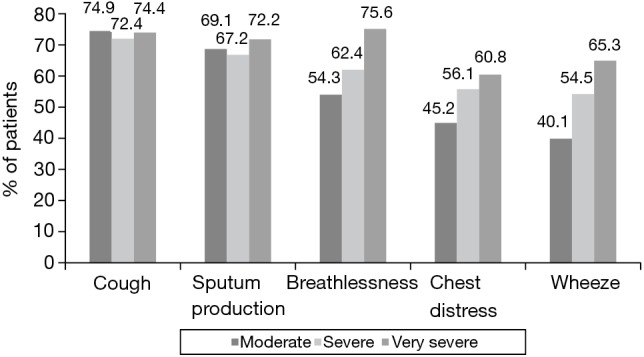
Frequency of respiratory symptoms according to GOLD classification. GOLD, Global Initiative for Chronic Obstructive Lung Disease.
Figure 3.
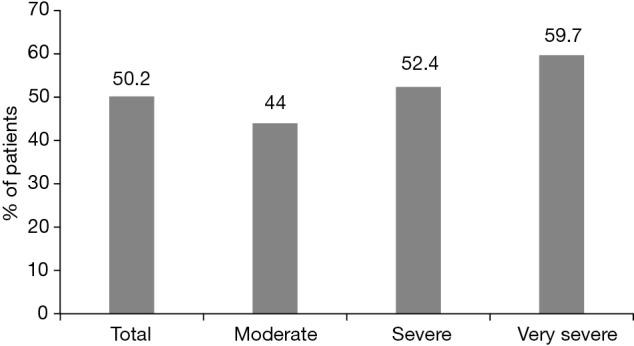
Perception of COPD symptoms variability according to GOLD classification. COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease.
Figure 4.
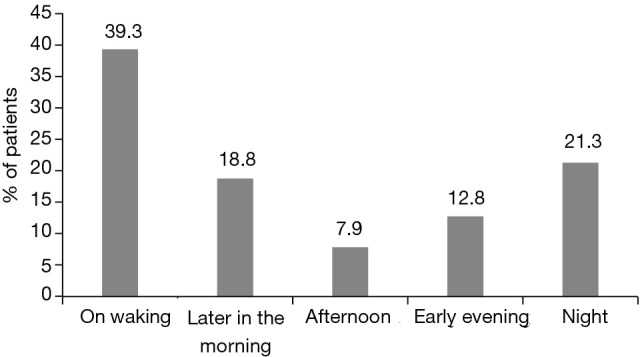
Distribution of patients according to the time slice of the day during which respiratory symptoms are most likely to occur.
Figure 5.
Distribution of patients according to the time slice of the day during which respiratory symptoms are most troublesome.
Impact of the COPD symptoms
When inquired about the impact of the symptoms on daily living activities and sleep, 86.5% had impaired exercise tolerance, 78.6% had difficulty in stair climbing, and 29.8% declared that they were experiencing poor sleep (Table 2).
Table 2. Impact of COPD symptoms on daily living activities.
| Variable | Number of patients (%) |
|---|---|
| Impact on daily living activities | |
| No impact | 34 (3.3) |
| Going up and down the stairs | 811 (78.6) |
| Going out for shopping | 435 (42.2) |
| Exercising | 893 (86.5) |
| Doing housework | 325 (31.5) |
| Impact on quality of sleep at night | |
| Sleep quality—good | 724 (70.2) |
| Sleep quality—poor | 308 (29.8) |
| Difficulty in falling asleep | 134 (43.5) |
| Frequent awakening at night | 171 (55.5) |
| Early wakening | 76 (24.7) |
| Reason for poor quality of sleep | |
| COPD symptoms interfering with the quality of sleep | 224 (72.7) |
| Others | 84 (27.3) |
COPD, chronic obstructive pulmonary disease.
Factors associated with symptom variability
A logistic regression analysis was also performed to identify factors associated with symptom variability. Univariate analysis showed that patients with very severe airflow limitation, CAT scores ≥10, mMRC scores ≥2, and a history of ≥2 exacerbations in the previous 12 months were more likely to experience symptom variability than patients with moderate airflow limitation, CAT scores of <10, mMRC scores of ≤1, and no history of exacerbations in the preceding 12 months. However, sex, body mass index, smoking index, comorbidity (including cardiovascular disease, diabetes mellitus, osteoporosis, depression) were not associated with variability during a day. Statistically significant variables during the univariate analysis were singled out and subjected to multivariate analysis, and these are presented in Table 3. CAT score ≥10 was the lone factor associated with symptom variability [odds ratio (OR) =0.463, P<0.001].
Table 3. Determination of factors that may influence symptoms variability during the day.
| Factor | OR (95% CI) | P value |
|---|---|---|
| Severity of airflow limitation (very severe vs. moderate) | 0.712 (0.487–1.042) | 0.08 |
| Severity of airflow limitation (very severe vs. severe) | 0.872 (0.605–1.257) | 0.46 |
| BMI (BMI <18 vs. >25) | 1.333 (0.794–2.238) | 0.28 |
| BMI (18≤ BMI ≤25 vs. BMI >25) | 1.151 (0.873–1.519) | 0.32 |
| CAT score (CAT <10 vs. CAT ≥10) | 0.463 (0.352–0.609) | <0.0001 |
| Frequency of COPD exacerbations (number of exacerbations ≤1 vs. none) | 1.279 (0.962–1.701) | 0.09 |
| Frequency of COPD exacerbations (number of exacerbations ≥2 vs. none) | 1.562 (0.969–2.517) | 0.07 |
BMI, body mass index; CAT, chronic obstructive pulmonary disease assessment test; CI, confidence interval; OR, odds ratio.
Discussion
COPD has been shown to be a highly heterogeneous disease with a wide range of symptoms such as breathlessness, chronic cough, and sputum production. Diurnal variation of these symptoms was shown to be associated with circadian variation of airway smooth musculature and inflammation, is a well-recognized event in other respiratory diseases such as asthma (11).
However, despite having similar clinical manifestations and lower pulmonary function, the circadian variability of COPD symptoms has been largely ignored. To our knowledge, this is the first study that assessed diurnal variations of COPD symptoms in Chinese patients.
Prevalence, variation and severity of COPD symptoms
In our study, cough and sputum production were the most commonly reported symptoms in patients with COPD. The present study results concur with the findings in Spanish, Turkish, and the US populations in whom sputum production and cough that peaked during the morning hours were reported to have the highest circadian variability (7). At least over half of all patients (50.2%) with symptomatic COPD perceived variability in one or more symptoms during the day, which is higher than those in Spanish (39.6%) (6) and different European populations (44.7%) (5). All those participants recruited were outpatients with more severe COPD (FEV1 <50% predicted) (5,6) . However, the inclusion was FEV1 <80% predicted in our study, 44% with moderate COPD (50%< FEV1 <80% predicted) reported that ≥ one symptom varied during the entire day, which indicated that symptom variability wasn’t perceived only in severe COPD patients. If only severe COPD patients enter the statistics in our study, the percent of symptom variability would be 54.5%, which is higher than those in Spanish and European populations (5,6). This difference may attribute to the insufficient treatment because of lower economic level in China. Almost all the patients were regularly prescribed ≥ one COPD medication, and most of them were treated with long-acting bronchodilators in European populations (5). Yet about half of our patients received medications only during exacerbations. We didn’t detail the variation of each symptom in our study. However, Spanish study reported that sputum production and cough had the highest circadian variability (6), whereas breathlessness was reported as the most common and troublesome symptom among European populations (5). All these fluctuations could be attributed to geographic variations, genetic background, exposure to risk factors and management strategies around the world (12-14).
The daily activities of the patients were most disturbed by COPD symptoms (5). The activities were affected markedly in patients reporting variability of breathlessness throughout the day, and the impact on activities was also pronounced in patients who experienced the greatest variability of symptoms compared with those with minimal variation (5). So, increased variability of symptoms during the day may reflect: (I) the severity of the respiratory impairment and its effect on exercise limitation; (II) inadequate treatment; (III) more adverse healthcare events. However, it is unknown whether the symptom variability during the times of the same day may predict a new COPD exacerbation.
COPD symptoms and health status
There is an old Chinese saying: make your whole year’s plans in spring and your day’s plan early in the morning. In our study, we found that the symptoms were perceived to be more intense during the early morning, which is similar to the literature reports in European populations (5). About 10% of the patient population reported that they needed support in performing their routine morning activities that they were concerned about becoming a burden to their relatives (5). In addition, most people may prefer to exercise in the morning; the troublesome symptoms in morning hours will certainly influence their mood and QoL during the whole day. There is growing evidence that COPD shows diurnal variability in physiological parameters of lung function, such as inspiratory capacity, FEV1, FVC and peak expiratory flow (3,5,15). Early morning hours presented least FEV1 values for COPD patients (16). So, the correlation between variability in morning symptoms and the impact on morning activities corresponds to the observations of circadian variations in lung function. Another justification could be that morning is the most active time of the day for severely impaired patients.
The clarification of factors that either increase or decrease the variability of breathlessness is important for the effective management of patients. Multivariate analysis demonstrated that CAT score was the only independent predictor in our study, whereas the European study showed that the factors associated with higher variability were younger age and increased severity of breathlessness in the preceding 7 days (5). Both the studies showed that sex, BMI, smoking status, time elapsed since COPD diagnosis, MRC dyspnea score, and predicted FEV1 were not related with the variability. As is well known, CAT is an 8-item unidimensional measure of health status impairment in COPD, including the degree of respiratory symptom, impaired activities and night sleep quality, which correlates more closely with the SGRQ. These may reflect a complex mechanism of symptom variability in COPD. Although the CAT provides a broader view on COPD, none of all the present questionnaires, including CAT and Clinical COPD Questionnaire (CCQ), could assess the variability of the measured symptoms during different times in the day. In this regard, to supplement the data from this study, it is necessary to design a new CAT questionnaire that specifically include the circadian variability and the impact of symptoms on morning activities for better coverage of clinical assessment and management, such as the Capacity of Daily Living during the Morning (CDLM) questionnaire, the first tool developed by Partridge et al. (17).
COPD symptoms and medication
The daytime variability in perceived symptoms is hardly ever considered in the actual treatment plans, despite the compelling evidence. In our study, only 38% were prescribed morning medication for alleviation of symptoms. Similarly, in the study by Kessler et al. (5), 51.3% of patients reported that they did not modify the use of their COPD medications during times of symptom variability. Partridge et al. compared the impact of different treatment on symptoms, lung function and activities early in the morning (18). Although budesonide/formoterol or salmeterol/fluticasone was effective in treating patients with COPD, the onset of action was rapid with budesonide/formoterol than salmeterol/fluticasone, which resulted in bigger improvements in the patient’s ability to perform routine morning activities. This difference was mainly due to the faster onset of action of formoterol compared with salmeterol. Additionally, formoterol, taken twice daily (8 am and 8 pm) with tiotropium once-daily (8 pm), can also control night symptom (19), as our study described that “at night” was another worst time during the day. Therefore, health care professionals must be provided with modified treatment strategies to minimize the impact of this variation.
Someone may doubt that the early morning was the worst moment for COPD patients which may be related to medications received. In other words, some individuals receiving medications, such as tiotropium QD or formoterol BID, remained uncovered for the last part of the period (i.e., the early morning of the next day) because of insufficient duration of action of the drug received. We agree with the presence of such possibility in patients receiving medications. However, 54.9% of the enrolled patients were on regular treatment, whereas the other 45.1% of patients received medications only during exacerbations in our study. We have performed an analysis (not list in the part of results) and also found the presence of circadian variation of symptoms in the latter subgroup. In addition, except morning waking time, night was also the worse time in the whole day when the medications could cover effectively. All these findings indicate the circadian variation of symptoms was incompletely relevant with drugs of insufficient duration.
This study has few limitations. Firstly, the perception of the symptoms variability is very subjective; many factors may produce some deviation such as different educational background and lifestyle. Secondly, the observational and cross-sectional design of the study itself could be the primary limitation in studies of this nature, which carries the risk of including patients with other comorbidities and confounding factors. The possibility that few subjects with asthma COPD overlap syndrome (ACOS), obstructive sleep apnea (OSA), left heart insufficiency or other diseases were enrolled could not be eliminated. Asthma symptoms are more variable than COPD, OSA and left heart insufficiency may manifest paroxysmal nocturnal dyspnea, which may influence the assessment of the worst moment throughout the day. However, the patients with asthma or ACOS were identified based on their medical histories and excluded as much as possible. Hence, their proportion was likely to be small among the population of COPD patients. Furthermore, the incidence of OSA is not clear as our study did not monitor the sleep for all COPD patients. It is well known that OSA is common in obese population and FEV1 was reported to increase overnight in OSA patients with obesity (20). However, the mean BMI of COPD patients enrolled in this study was only 23. Thereby, we speculate that the proportion of COPD overlap with OSA would not be high in this study. In addition, multi-regression analysis in this study revealed that BMI did not impact the circadian variation of symptoms of patients with COPD.
Conclusions
The symptoms perceived by COPD patients varied during the day that had major impact on daily living activities. Moreover, poor adherence to their treatment was observed in patients in response to deterioration of symptoms. The impact of circadian variation in symptoms provides an important insight for developing an individualized plan modeled on patient characteristics for COPD management. This has vital implications in a country such as China, where primary care physicians have a tenuous grasp on Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommendations for COPD therapy, and the most frequently prescribed medications like expectorants and short-acting bronchodilators are not able to meet patient expectations and improve their long-term clinical outcomes. The variation in the perception of symptoms should be considered in the long-term COPD management in China. The findings of our study not only provide additional knowledge on diurnal variability of symptoms in Chinese patients but also pave way to establish a potential novel target in the long-term treatment plan to alleviate the impact of symptoms variability on HRQoL.
Acknowledgements
We thank the patients, their families, and the investigators for their participation in this study. The authors acknowledge Dr. Ramu Periyasamy, Indegene Pvt. Ltd., for providing the medical writing assistance and editorial support towards the development of the manuscript. The co-author of this study, Dr. Yongchang Sun current affiliation is Department of Respiratory Medicine, Peking University Third Hospital, Beijing, China. This research was funded by AstraZeneca.
Ethical Statement: The study protocol was approved by the institutional review board at each participating centre: (I) Peking University Third Hospital (Approval ID: 20121128); (II) Peking Union Medical College Hospital (Approval ID: 20130124); (III) Beijing Chao-Yang Hospital (Approval ID: 20141222); (IV) Tianjin Medical University General Hospital (Approval ID: 20130123); (V) The First Affiliated Hospital of Guangzhou Medical University (Approval ID: 20130116); (VI) Beijing Tongren Hospital, Capital Medical University (Approval ID: 20130131); (VII) West China Hospital, Sichuan University (Approval ID: 20130201); (VIII) Huadong Hospital Affiliated to Fudan University (Approval ID: 20130128); (IX) Shanghai First People’s Hospital (Approval ID: 20130128); (X) Tongji Hospital, Tongji Medical College, Huang Zhong University of Science and Technology (Approval ID: 20130105); (XI) Beijing Hospital (Approval ID: 20121115) and written informed consent was obtained from the patient for publication of this manuscript.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Global Strategy for the Diagnosis, Management and Prevention of COPD. Available online: http://www.goldcopd.org [DOI] [PubMed]
- 2.Soriano JB, Calle M, Montemayor T, et al. The general public's knowledge of chronic obstructive pulmonary disease and its determinants: current situation and recent changes. Arch Bronconeumol 2012;48:308-15. [DOI] [PubMed] [Google Scholar]
- 3.McCarley C, Hanneman SK, Padhye N, et al. A pilot home study of temporal variations of symptoms in chronic obstructive lung disease. Biol Res Nurs 2007;9:8-20. 10.1177/1099800407303501 [DOI] [PubMed] [Google Scholar]
- 4.Partridge MR, Karlsson N, Small IR. Patient insight into the impact of chronic obstructive pulmonary disease in the morning: an internet survey. Curr Med Res Opin 2009;25:2043-8. 10.1185/03007990903103006 [DOI] [PubMed] [Google Scholar]
- 5.Kessler R, Partridge MR, Miravitlles M, et al. Symptom variability in patients with severe COPD: a pan-European cross-sectional study. Eur Respir J 2011;37:264-72. 10.1183/09031936.00051110 [DOI] [PubMed] [Google Scholar]
- 6.Espinosa de los Monteros MJ, Peña C, Soto Hurtado EJ, et al. Variability of respiratory symptoms in severe COPD. Arch Bronconeumol 2012;48:3-7. [DOI] [PubMed] [Google Scholar]
- 7.Kuyucu T, Güçlü SZ, Saylan B, et al. A cross-sectional observational study to investigate daily symptom variability, effects of symptom on morning activities and therapeutic expectations of patients and physicians in COPD-SUNRISE study. Tuberk Toraks 2011;59:328-39. 10.5578/tt.3268 [DOI] [PubMed] [Google Scholar]
- 8.Lopez-Campos JL, Calero C, Quintana-Gallego E. Symptom variability in COPD: a narrative review. Int J Chron Obstruct Pulmon Dis 2013;8:231-8. 10.2147/COPD.S42866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casanova C, Aguirre-Jaíme A, de Torres JP, et al. Longitudinal assessment in COPD patients: multidimensional variability and outcomes. Eur Respir J 2014;43:745-53. 10.1183/09031936.00096913 [DOI] [PubMed] [Google Scholar]
- 10.Zhong N, Wang C, Yao W, et al. Prevalence of chronic obstructive pulmonary disease in China: a large, population-based survey. Am J Respir Crit Care Med 2007;176:753-60. 10.1164/rccm.200612-1749OC [DOI] [PubMed] [Google Scholar]
- 11.Hetzel MR, Clark TJ. Comparison of normal and asthmatic circadian rhythms in peak expiratory flow rate. Thorax 1980;35:732-8. 10.1136/thx.35.10.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miravitlles M, Murio C, Tirado-Conde G, et al. Geographic differences in clinical characteristics and management of COPD: the EPOCA study. Int J Chron Obstruct Pulmon Dis 2008;3:803-14. 10.2147/COPD.S4257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peña VS, Miravitlles M, Gabriel R, et al. Geographic variations in prevalence and underdiagnosis of COPD: results of the IBERPOC multicentre epidemiological study. Chest 2000;118:981-9. 10.1378/chest.118.4.981 [DOI] [PubMed] [Google Scholar]
- 14.Fang X, Wang X, Bai C. COPD in China: the burden and importance of proper management. Chest 2011;139:920-929. 10.1378/chest.10-1393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van Noord JA, Aumann JL, Janssens E, et al. Effects of tiotropium with and without formoterol on airflow obstruction and resting hyperinflation in patients with COPD. Chest 2006;129:509-17. 10.1378/chest.129.3.509 [DOI] [PubMed] [Google Scholar]
- 16.Calverley PM, Lee A, Towse L, et al. Effect of tiotropium bromide on circadian variation in airflow limitation in chronic obstructive pulmonary disease. Thorax 2003;58:855-60. 10.1136/thorax.58.10.855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Partridge MR, Miravitlles M, Ståhl E, et al. Development and validation of the Capacity of Daily Living during the Morning questionnaire and the Global Chest Symptoms Questionnaire in COPD. Eur Respir J 2010;36:96-104. 10.1183/09031936.00123709 [DOI] [PubMed] [Google Scholar]
- 18.Partridge MR, Schuermann W, Beckman O, et al. Effect on lung function and morning activities of budesonide/formoterol versus salmeterol/fluticasone in patients with COPD. Ther Adv Respir Dis 2009;3:1-11. 10.1177/1753465809344870 [DOI] [PubMed] [Google Scholar]
- 19.Terzano C, Petroianni A, Conti V, et al. Rational timing of combination therapy with tiotropium and formoterol in moderate and severe COPD. Respir Med 2008;102:1701-7. 10.1016/j.rmed.2008.07.012 [DOI] [PubMed] [Google Scholar]
- 20.Kunos L, Lazar Z, Martinovszky F, et al. Overnight Changes in Lung Function of Obese Patients with Obstructive Sleep Apnoea. Lung 2017;195:127-33. 10.1007/s00408-016-9957-1 [DOI] [PubMed] [Google Scholar]


