Abstract
Rahima Bano, the world’s last endemic case of severe smallpox, Variola Major, developed rash on October 16, 1975 on Bhola Island, Bangladesh. Achieving eradication in a country destroyed by war challenged the achievement of smallpox eradication. Between January 1, 1972 and December 31, 1975, 225,000 smallpox cases and 45,000 smallpox deaths occurred. Adapting the global smallpox eradication strategies of surveillance, the detection of smallpox cases, and containment, the interruption of smallpox transmission, utilized progress toward three objectives to monitor performance: 1) Surveillance – the percent smallpox infected villages detected within 14 days of the first case of rash, 2) Knowledge of the Reward – public knowledge of the current amount of the reward for reporting smallpox, and 3) Containment – the percent of infected villages interrupting smallpox transmission within 14 days of detection. Failures to achieve these objectives led to identification and implementation of improved strategies that eventually achieved eradication. Essential to this success was a tripartite partnership of the citizens of Bangladesh, the Bangladesh Ministry of Health and its field staff, and personnel and resources mobilized by the World Health Organization.
Keywords: Bangladesh, Smallpox, Eradication, Surveillance, Containment
INTRODUCTION
On March 26, 1971, Bangladesh, then East Pakistan, declared independence when Pakistan refused to seat the Awami League majority elected in December of 1970. Civil repression by the Pakistani military led to an estimated 3 million deaths and the exodus of 10 million persons to refugee camps in India [1]. In November of 1971, smallpox broke out in Salt Lake Refugee Camp near Calcutta. Before smallpox control could be initiated, invasion of Indian troops ended the repression and liberation was achieved on December 16, 1972. Infected and susceptible refugees crowded aboard trains, buses, and boats for the trip home. The country, which had been smallpox free in 1971, was re-infected with smallpox.
Over a four year period (1972-75), an estimated 225,000 smallpox cases and 40,000 smallpox deaths occurred in Bangladesh. With an infrastructure destroyed by war, major floods and severe famine in 1974, and two coups d’état, Bangladesh was initially incapable of controlling its smallpox epidemic. As described in this paper, use of evidence at the field level led to the evolution of successful eradication strategies. Rahima Bano, the world’s last case of the severe form of smallpox, Variola Major, developed rash on October 16, 1975 [2:38-48].
PROGRAM INDICATORS TO MONITOR ERADICATION PROGRAM PERFORMANCE
As the Bangladesh Smallpox Eradication Program evolved, three indicators emerged, each measuring the effectiveness of field operations in a key area: 1) surveillance – the detection of smallpox infected villages, 2) public knowledge of the amount of the reward for reporting new smallpox infected villages, and 3) containment – the ability to interrupt smallpox transmission within 14 days of detection of an infected village. Perhaps the most important legacy of the Bangladesh Smallpox Program was the identification and use of failures to achieve objectives as drivers to improve program operations.
Surveillance
The surveillance indicator was defined as the percent of infected villages detected within 14 days of rash onset in the first smallpox case in that village. While only 11% of smallpox cases were reported in 1972, 53.8 % of 4,108 smallpox infected villages identified in 1975 were detected within one week of onset of smallpox rash in the first case; 74.1% were detected within 2 weeks [2: 87].
Public Knowledge of Amount of the Reward
In August of 1974, a monetary reward was introduced for the reporting of new smallpox infected villages; eight months later, only 30% of the public knew about the reward. Doubling and publicizing the reward through visits to 12 million houses increased knowledge to over 80%.
Containment
The containment indicator was defined as the percentage of infected villages with no new smallpox cases 15 or more days after identification. The percentage of containment failures decreased from 27% in November of 1974 to 1% in September of 1995.
SURVEILLANCE
Eradication of smallpox required effective surveillance including the identification and reporting of smallpox cases, the analysis of data, the preparation and distribution of reports, and most importantly, use of this data to strengthen surveillance and containment [3]. As the new government struggled to reestablish a functioning health system, 10,734 smallpox cases were reported in 1972. An estimated 81,000 smallpox cases were not reported. Reasons for the low 11% level of reporting related in part to traditional beliefs: for Moslems, smallpox was the will of Allah; for Hindus, smallpox was the visitation of the Goddess Shitala Mata; and for most Bangladeshis, reporting was never responded to and was therefore thought to be useless. Health officers were reluctant to report smallpox because cases were an admission of failure to follow orders to vaccinate everyone.
In 1972, the World Health Organization’s Global Smallpox Eradication Program assisted the Ministry of Health with five epidemiologists and the funding of five four-man, motorcycle-equipped surveillance teams. These teams visited markets and schools showing the picture of a person with smallpox and searching for individuals reported to have similar rash illnesses. Positive reports were investigated. Smallpox, when confirmed, was contained through focal vaccination of available residents and neighbors of the infected household. During 1973 and 1974, the number of surveillance teams increased from 5 in 1973 to 18 in 1974, 1 per district; the number of reported smallpox infections declined from a high of 32,711 in 1973 to 16,485 in 1974. Each year, smallpox incidence increased during the spring, February-May and decreased at the end of the rainy season, August-November, Figure 2.
Figure 2.
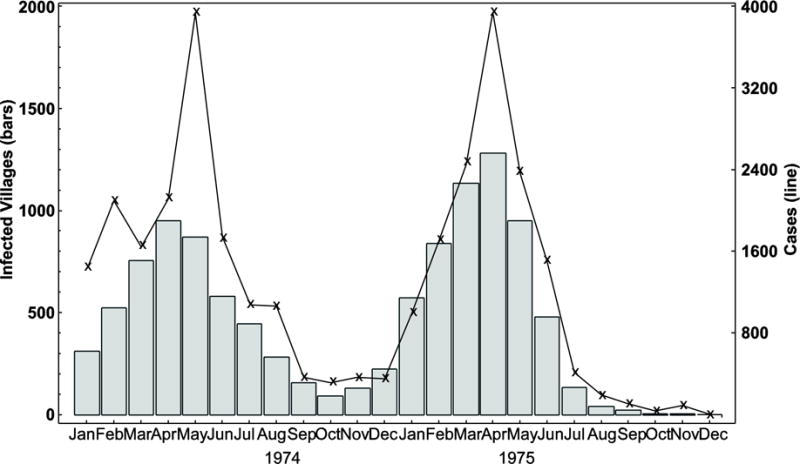
Smallpox infected villages and cases in Bangladesh, 1974-75. Smallpox incidence, as evidenced both by the number or infected villages and reported smallpox cases, increased from February to June in 1974 and September 1975.
Smallpox-Infected Villages
Although smallpox in Bangladesh occurred in both rural and urban locations, each infected area was designated as an infected village, a metric for surveillance. The number of smallpox cases per infected village ranged from one to hundreds. Each infected village was mapped, the houses numbered, and the population living within ½ mile enumerated. Investigations were carried out to trace the source of infection and to identify residents and contacts that had travelled away from the infected villages. Smallpox teams working in the destination villages were notified by radio of the possible arrival of an infected individual. Many cross notifications led to the identification of smallpox cases in the first few days of illness.
Recognizing that smallpox eradication was failing, an emergency plan was developed in April of 1974 [2: 257-260]. This plan decentralized authority for surveillance and containment to the Thana level (similar to a district with an average population of 200,000) and designated the most qualified health or malaria officer responsible for smallpox surveillance and containment. The number of smallpox-infected outbreaks fell from 949 in April of 1974 to 91 in October of 1974, Figure 1A. Eradication was predicted for December of 1974. Floods, the worst in 50 years, devastated the two most heavily infected areas in the northern part of the country. With houses and crops destroyed, the affected population migrated to the cities of Dhaka, Mymensingh, and Bogra in search of food and survival. Known smallpox infected villages increased from 91 in October of 1974 to 572 in January of 1975, Figure 1B.
Figure 1.

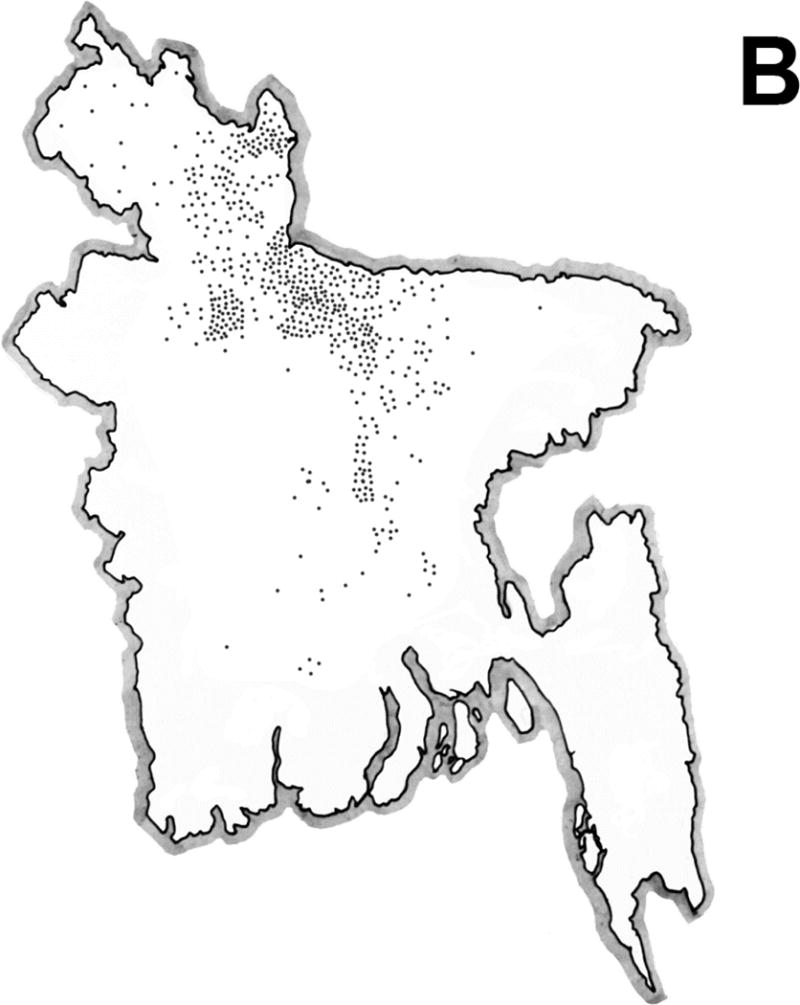
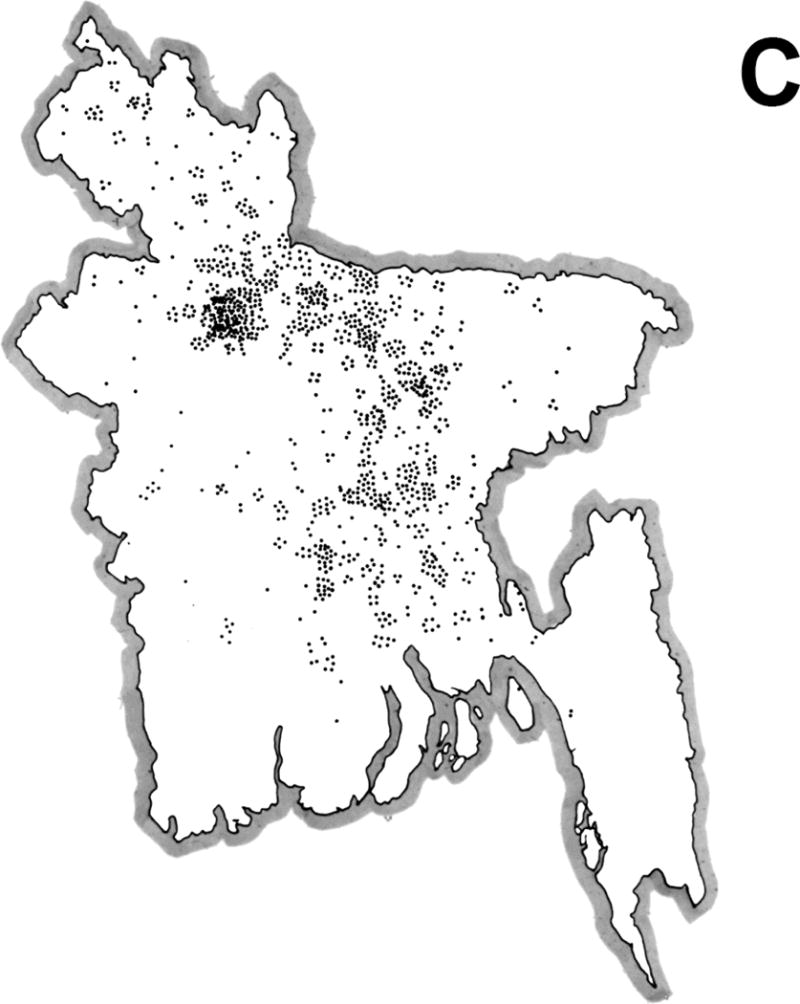

Geographic distribution of smallpox infected villages in Bangladesh. The distribution of infected villages during October 1974 (Figure 1A), January 1975 (Figure 1B), March 1975 (Figure 1C), and April1975 (Figure 1D) illustrates the spatial spread of smallpox throughout Bangladesh following reintroduction.
Concerned about the increasing numbers of homeless people in the cities, the Government ordered the destruction of slums in Dhaka, Chittagong, Rajshahi, and Khulna. Departing slum dwellers from Dhaka disseminated smallpox throughout the country. Smallpox infected villages increased to 1,132 in March of 1975 and 1,280 in April of 1975, Figures 1C and 1D. The number of reported smallpox infections increased from a low of 308 in October of 1994 to 3,948 in April of 1975.
Reward for Reporting Smallpox
To increase the completeness of reporting, a 50 Taka (US$6) reward was introduced for the reporting of a previously undetected smallpox infected village in August of 1974. Mass publicity included banners, radio messages, pamphlets and posters on rickshaws, buses, boats, and walls. By May of 1975, a field survey documented that only 30% of the public knew about the reward. Further studies documented that health workers were reluctant to inform the public about the reward for fear that the public reporter rather than the health worker would receive the money. Doubling the reward to pay both the public reporter and the health worker, who confirmed a new smallpox infected village, solved the problem.
As the number of smallpox infected villages fell, the amount of the reward increased from 50 to 100, then to 250, and finally to 500 Takas (about US$50). Public knowledge of the reward increased from 65% in September of 1975 to 87% in January of 1976, Table 1. Rewards were always presented at public ceremonies to further promote public reporting; $US 25,000 in reward money was expended during the program.
Table 1.
House to House Surveys for Rash Cases and Smallpox Post-Search Assessment for Houses Visited and Knowledge of Reward [2: 133]
| Search of 12 Million Houses for Rash and Smallpox | Post-Search Sample Assessment by Senior Ministry of Health Officials | |||||
|---|---|---|---|---|---|---|
| First Day of Search | Rash Cases | Smallpox Cases | Villages Checked | Houses Checked | Houses Visited (%) | Houses Knowing Amount of Reward (%) |
| 8/74 | No Reward | 0 | ||||
| 4/75 | Survey | 30 | ||||
| 5/75 | 101 | |||||
| 7/75 | 1,305 | 33 | 3,783 | 71,877 | 89 | 68 |
| 8/75 | 1,200 | 7 | 2,875 | 54,625 | 90 | 80 |
| 9/75 | 4,975 | 8 | 2,413 | 44,604 | 84 | 65 |
| 10/75 | 11,109 | 0 | 1,749 | 34,362 | 78 | 79 |
| 11/75 | 16,502 | 0 | 1,688 | 32,867 | 84 | 81 |
| 1/76 | 37,986 | 0 | 1,515 | 32,111 | 85 | 87 |
| 3/76 | 59,166 | 0 | 1,455 | 28,737 | 84 | 87 |
| 5/76 | 28,984 | 0 | 1,378 | 27,301 | 87 | 90 |
| 12-76 | 20,315 | 0 | 1,466 | 29,095 | 83 | 86 |
House-to-House Survey
In the spring of 1975, undetected chains of smallpox transmission continuing for weeks were uncovered. House-to-house surveys, as developed in India, were introduced. Building on a method applied earlier by the Malaria Eradication Program, each house was numbered and local area maps were drawn. Each of the 12,000 health workers was assigned 1,000 houses to search. At each house, residents were shown the smallpox picture-card, informed about the reward for reporting smallpox, and asked if they knew of any persons with a similar rash illness. In each of the five nation-wide surveys, 12 million houses were targeted for the house-to-house search. These searches were completed in 5-9 days and were effective in identifying unknown chains of transmission (Table 1, Columns 1-3). Each nation-wide survey required an estimated 100,000 person-days of labor.
Quality Assurance of House-to House Surveys
Following each search, a random sample of villages and houses was surveyed by senior Ministry of Health Officials to determine the percent of houses actually visited during the search and the percent of respondents who knew the amount of the reward. Results of these quality assurance visits are presented in Table 1, Column 4-7. The percent of houses visited increased from 78% to 90%. Given that the amount of the award increased at regular intervals, correct knowledge of the amount of the reward measured the timeliness of their knowledge; the percentage of correct knowledge of the amount of the reward peaked at 90% in May of 1976.
Smallpox Scar Survey to Assess Reporting Effectiveness
In November of 1975, Hughes and colleagues surveyed 465,892 individuals for smallpox facial scarring [4]. Each scarred individual was asked if their illness occurred prior to or after the end of the war. Using a calendar of local events, cases with smallpox after liberation (December 16, 1971) were further queried to determine the year of smallpox onset. Annual incidence rates were estimated by correcting for scarring loss and smallpox-specific and non-smallpox mortality. Figure 3 shows reported smallpox, estimated unreported smallpox, and surveillance effectiveness. Detection and reporting of smallpox increased from 11.8% in 1972 to 83% in 1975. The reporting rate exceeded 95% during the last 6 months of 1975.
Figure 3.

Results from the retrospective survey of smallpox facial scars conducted during 1976. Reported and unreported smallpox cases and percentages of the estimated annual totals that were reported each year in Bangladesh, 1972-75, the stacked bars and numbers, respectively.
MATHEMATICAL MODELING
Following the September 11, 2001 terrorist attack on the World Trade Center and subsequent intentional spread of anthrax in the United States, the possible use of smallpox as a biologic weapon emerged as a concern. Mathematical models were used as tools for developing potential response strategies. Before using the model to inform public policy [5], it was evaluated using existing smallpox data sets including Bangladesh. This evaluation provided a new understanding of the epidemiology of smallpox in Bangladesh.
Efficiency of Reporting
Because the efficiency of smallpox reporting in Bangladesh increased temporally, the logistic function, y(t) = 1/[1 + exp(a − bt)], where a and b are regression coefficients and t is time in years since 1 January 1971, was fitted to ratios of annual numbers of cases reported and estimated by Hughes [4]. Fitting involves choosing coefficients that minimize the sum of squared deviations (differences between the ratios and curve at mid-year). As mentioned above, reporting efficiency increased from about 10% in 1972 to over 80% in 1976, Figure 4.
Figure 4.
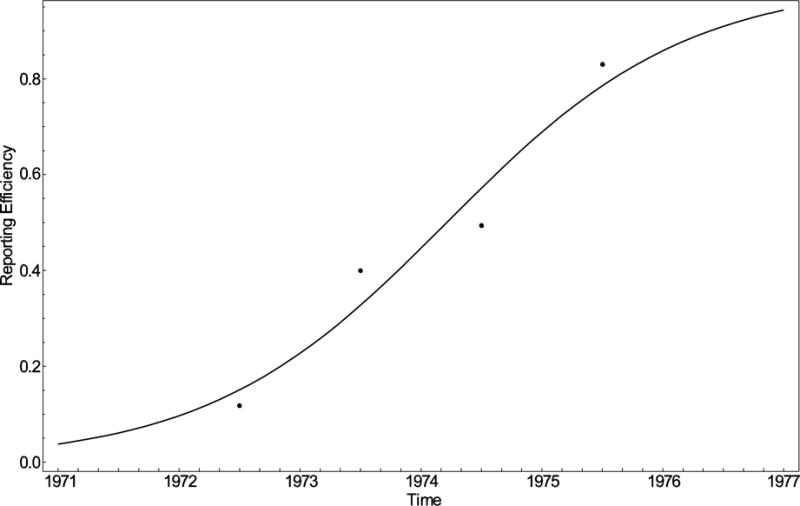
Secular improvement in smallpox reporting. The logistic equation, y(t) = 1/[1 + exp(3.24 - 1.01t)], where t = time in years since 1 January 1971, was fitted to ratios of cases reported and estimated via the 1976 pockmark survey [3], the curve and points, respectively.
Monthly smallpox cases were estimated by multiplying the numbers officially reported by the government of Bangladesh to the World Health Organization (and published in its Weekly Epidemiologic Record at http://whqlibdoc.who.int/wer/) by the reciprocal of y(t), the time-varying reporting efficiency derived from the facial scar survey, Figure 5. The decreasing gaps between reported and estimated cases over time provide evidence on the increasing effectiveness of smallpox surveillance.
Figure 5.
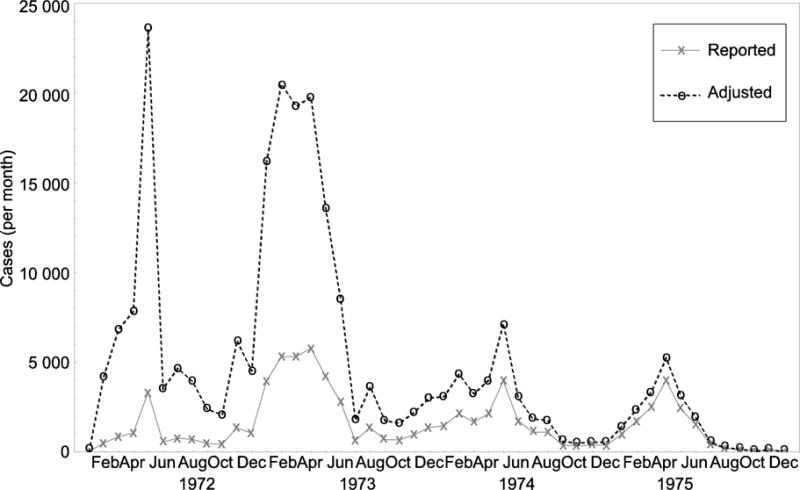
Cases reported and estimated by correcting for reporting inefficiency. To estimate the actual numbers of cases, reports were multiplied by reciprocals of efficiencies obtained from the function illustrated in Figure 4, the solid and dashed lines with ‘×’ and ‘o’ symbols, respectively.
Evaluation of the Model
These monthly “observations” were converted into weekly ones via the Expand Procedure (SAS Institute Inc., SAS Campus Drive, Cary, North Carolina 27513), a means of changing the interval between successive observations without changing their sum. The predicted cases were then compared to these weekly observations, adjusting initial conditions and coefficients of the harmonic function by which we modeled seasonal variation in the infection rate.
In the transmission model, the infection rate, β(t) = β0 + β1 cos (2πωt) + β2 sin (2πωt), where π is a mathematical constant (the ratio of any circle’s circumference to its diameter), t is time and ω is frequency (reciprocal of the period between successive observations). The mean, β0 and harmonic coefficients, β1 and β2 were estimated via the least squares procedure described above. Predicted and “observed” cases of smallpox in Bangladesh, 1972-75, are presented in Figure 6.
Figure 6.

Smallpox cases predicted by the transmission model [2] and “observed” in Bangladesh, 1972-75. The symbols represent daily estimates obtained from the corrected monthly observations illustrated in Figure 5, adjusted to match the annual totals of Hughes and co-workers [3].
Predictions resemble these adjusted observations in magnitude and timing, but not the year-to-year variation accompanying the resettlement of refugees from India. Delayed detection of cases in 1972 and early 1973 may have contributed to the apparent disparities. Alternatively, recall of onset dates may have become imprecise with time, possibly explaining why the model fits the reconstructed annual curves less well in 1972 and 1973 than it does in later years.
Seasonality of Smallpox
Smallpox is known in Bangla, the language of Bangladesh, as Guti Boshonto, the word for spring rash, the time of the maximum number of cases. Conventional wisdom was that maximum transmission occurred during these peak months, April-May, with minimum transmission occurring during October-November, the months of the lowest number of cases. Modeling clearly shows otherwise; maximum transmission occurred from November to March, Figure 7. Numerous explanations have been offered for this phenomenon: low temperature, low humidity, movement home at the end of the rice harvest season, and religious festivals. Transmission reaches its nadir in July, the start of the monsoon season.
Figure 7.
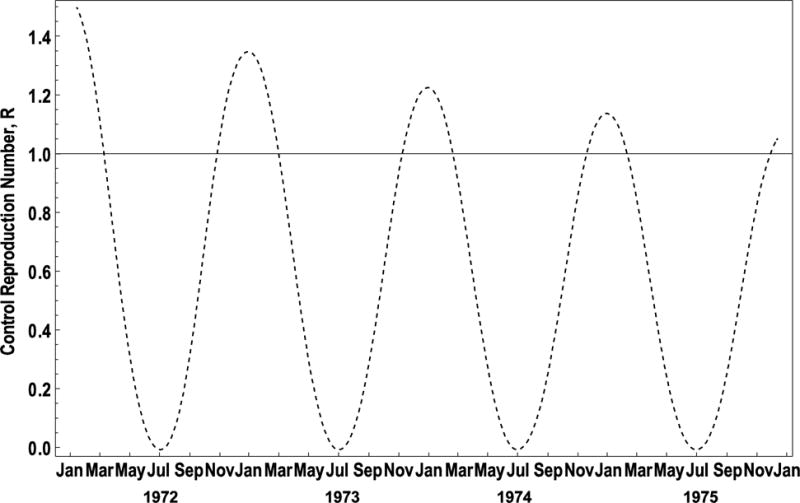
Impact of improved surveillance and containment on the reproduction number. Learning from failures reduced the average number of secondary infections per primary infection, the dotted line, which eventually converged on the threshold for elimination, the solid line.
Reproduction Number
The number of secondary infections per infectious person deduced from the smallpox transmission model resembles that reported by field epidemiologists, who estimated r from the exponential growth model, N(t) = N(0)exp(rt), early in outbreaks [2: 82-85]. In their model, N(0) and N(t) are the numbers of cases at times 0 and t, respectively, r is the growth rate, and t is time. They observed that the doubling time, td = ln(2)/r, approximated the serial interval, or period between successive generations of cases. As can be seen from this figure, ℜ ≈ 2 initially, but successive peaks approach ℜ = 1, the elimination threshold.
CONTAINMENT
Containment was designed to interrupt smallpox transmission in each identified infected village. The containment strategy, as it evolved over time, had multiple tasks:
Isolation of the smallpox case or cases in their home(s)
Posting of guards at all infected households 24 hours per day to ensure isolation of the smallpox cases and to vaccinate residents and visitors
Enumerating, vaccinating and following-up vaccinees to ensure successful vaccination of all residents and visitors of infected houses
Searching all houses situated within ½ mile of the infected houses including numbering of each house, enumeration and vaccination of all residents and visitors, and follow-up visits to document successful vaccination
Searching all markets, schools, and homes situated between ½ and five miles of the infected houses for individuals with fever or rash
Cross notification of travel of potential smallpox contacts to smallpox teams by radio
Containment 1972
In the post-conflict situation, surveillance and containment were the responsibility of the five regional surveillance-containment teams. Containment was initially limited to the vaccination of available household and neighborhood contacts on the day of investigation. Revisits to infected villages, however, identified continued transmission among residents and visitors absent at the time of vaccination.
Containment 1973
As health systems were reestablished, local health workers were ordered to remain in the infected villages to enforce isolation and to vaccinate contacts and neighbors until transmission was interupted. Follow-up of infected villages again identified continuing smallpox transmission. Health workers refused to spend nights in the infected villages during the times of maximum population density, and explained that there were no places to eat or sleep.
Containment 1974
In November of 1974, monthly assessment of the number and percent of infected villages with cases 15 days after detection was established as a critical indicator. In that month, 27% of outbreaks had new cases 15 or more days after the infected village had been identified and containment procedures initiated. As failures were identified and causes found, the containment protocol was modified to address the causes of the failures. Table 2 provides examples of causes of containment failures and corrective actions taken.
Table 2.
Examples of Containment Failures and Actions Taken
| Causes of Containment Failures | Corrective Actions Taken |
|---|---|
| Smallpox cases were thirsty and hungry and left their houses in search of water and food | Program provided water and food to infected households |
| Folk belief uncovered that if you entered a smallpox house at midnight through the back door you would not get smallpox | Guard-vaccinators were posted at all house entrances day and night |
| Health workers were unwilling to live in infected village to oversee containment | Neighbors of infected house were recruited and trained to serve as guards, vaccinators, and searchers. Once local residents were hired to carry out containment and were being paid by the health workers, health workers had a place to stay and a source of food |
| Smallpox among the homeless | Established isolation camps for cases where household isolation was not feasible |
| Smallpox cases among prostitutes | Vaccinator guards posted to brothel to vaccinate prostitutes and customers |
Many of these failures were identified by staff who worked 25 days a month in the field, many for four years. This process of identification of failures and initiation of remedial action is exemplified by Sabour, a surveillance team leader. Sabour became distressed when 11 of 17 infected villages had new cases after 14 days. On further investigation, he discovered that household members were not reporting relatives who had come to visit. because they did not consider relatives as visitors. Adding a list of relatives to the protocol solved the problem. As containment failures were identified and the protocol was strengthened, the rate of containment failures decreased from 27% in November of 1974 to 1% in September of 1975, Figure 8.
Figure 8.

Failures to stop transmission within 14 days, Bangladesh 1974-75. Monthly percentages of villages having new smallpox cases 15 or more days after identification of smallpox infected village. The decrease in containment failures documents the increased timeliness and effectiveness of containment tasks.
DRIVERS OF PROGRAM EFFECTIVENESS
In reflecting on smallpox eradication in Bangladesh 35 years after eradication, five drivers emerge as critical to the program’s success.
Leadership
As data identified the complexity of smallpox eradication, leadership and field operations were decentralized: initially to the five divisions, then to the 19 districts, then to the 56 subdivisions, and finally to 415 Thanas. At each level, individuals took on smallpox eradication as his/her personal challenge. Three individuals exemplify this commitment and leadership that kept the team together and ready to fight the next battle.
Kamrul Huda, the SubDivisional Medical Officering Chittagong, died en route to investigate a rumored infected village on Sandwip Island. After his death, Dr. Huda’s wife shared his commitment. “If young girls have facial scars from smallpox, they will have difficulty getting married and in life.” Dr. Nick Ward, the expert on smallpox in the densely populated Dhaka, left Bangladesh two times when smallpox was under control. Two times smallpox in Dhaka reappeared; two times the first author requested Nick’s return and two times Nick returned.
AG Rangaraj, India’s first physician parachutist and a survivor of General Stillwell’s fighting during World War II, was a constant source of optimism. As the number of smallpox infected villages increased from 91 in October of 1974 to 1,280 in April of 1975, Rangar cheered us on daily with “Hang in there; it’s going to be alright.” Three years later, the first author again crossed path with “Rangar” in Somalia. When asked about his optimism, he replied “I never thought you had a chance in hell of winning; I had, however, learned during World War II in Burma that optimism was essential to survival during the worst of times.” Thus, it was his military training, rather than objective assessment of the data, that kept us going during the difficult times of 1975. Optimism is essential for eradication programs to succeed.
Human and Financial Resources
The Bangladesh Smallpox Eradication Program started out as a joint partnership of the Ministry of Health and the World Health Organization. Neither partner initially recognized the complexity of eradication or the resources that would be required. Through dialogue informed by data between the Bangladesh Ministry of Health and WHO, operational procedures were modified. In 1972, program staffing was limited to 45 Bangladeshis and 5 internationals. As failures to achieve the three key objectives identified the need for additional resources, expansion of human and financial resources became an imperative. Over the 5 years of the Bangladesh program, 30,000 individuals including 225 internationals from 28 countries contributed to the program. During the 1975 final stages of household surveys and community-led containment, an estimated 152,000 person-days of labor were provided over a 3 month period [9]. The total cost of the program was US$15.6 million; the Bangladesh Government provided 50.7% of these costs, US$7.9 million [2: 213]; the remainder of the funds, US$ 7.7 million were provided by WHO, other UN Organizations, and bilateral partners.
Esprit de Corps
Three factors contributed to the building and maintenance of Esprit de Corps:
Each new team member was provided a short field mentored training as to his/her work responsibilities.
A Smallpox Zero radio system enabled rapid communications and provided a venue for a weekly Sunday smallpox conference call.
Monthly meetings were held at the national level.
The monthly meetings were held at the Smallpox Control Room known as Smallpox Zero. Sharing of information was critical to keeping all informed of the current status of eradication including:
Monitoring progress toward the three objectives
Identifying barriers to meeting the three objectives
Developing improved or innovative strategies to address barriers
Sharing successes, failures, and stories
Maintaining and encourage morale, especially during difficult times
Replenishing vaccine, money, and media supplies
Each meeting also included a social event to enable staff to let go, unwind, clean-up and renew friendships.
Civil Society Partnerships
Initially, reporting of smallpox was suppressed and containment was insensitive to local beliefs and values. As villagers saw that reports of smallpox were being responded to, they became active partners in reporting. Forty-four percent of the last 119 infected villages were reported by the public. The last case of Variola Major in the world was reported by 8 year old Bilkisunnessa, herself a victim of smallpox. Equally important was the involvement of communities in the containment of smallpox outbreaks. Additional information on the role of public partnerships is provided by Tarantola [6].
Not Accepting No as an Answer
An essential element of the program was not accepting no for an answer. As data identified the need for additional resources, an administrative response of no was occasionally received. With the data at hand, additional resources were almost always identified. When one operations officer went two months without an urgently needed boat, he hijacked a headquarters vehicle visiting his sight as ransom. The boat arrived two days later and the vehicle was returned. When an additional million dollars was needed, WHO Geneva found it in 7 days.
BANGLADESH SMALLPOX ERADICATION AND ITS RELEVANCE TO OTHER ERADICATION PROGRAMS
Each disease candidate for eradication has its own unique characteristics. For smallpox, they were the easy clinical diagnosis, severity of debilitation during the time of maximum infectivity, and the relatively low rate of person-to-person transmission. Its challenges were political, logistic, and natural disasters.
Global eradication of a disease requires full understanding of the epidemiology; a full and common recognition of what is required in terms of commitment, technology, and resources; a field staff empowered to make evidence-based decisions to identify and address unexpected barriers, and most importantly optimism.
CONCLUSION
While the surveillance-containment strategy to eradicate smallpox was developed by the USAID-CDC Smallpox Eradication Measles Control Program in West and Central Africa in 1970 [7], its effective implementation required adaptation to the realities of each country. Bangladesh was the most densely populated rural country in the world; the war had destroyed both the government and physical infrastructures. Almost all the bridges in the riverine country had been destroyed. Bangladesh lacked the health system and infrastructure to effectively implement an effective eradication strategy. In 1972, the program started out with a team of 50; only 11% of smallpox cases were reported. Using three indicators of progress – 1) detection of every new smallpox infected village within 14 days of the onset of rash in its first case, 2) public knowledge of the correct amount of the reward for reporting a previously undetected smallpox case, and 3) interruption of smallpox transmission within 14 days of the identification of newly infected villages – programmatic failures were identified, analyzed, and remedied. Each smallpox case was in fact a program failure. Rather than being satisfied with successes, e.g., the falling number of reported smallpox cases, the expanded and decentralized infrastructure focused on identifying barriers to achievement of its objectives and to developing more effective intervention strategies.
Achievement of smallpox eradication was threatened by three events: 1) two coups d’état; 2) the devastating flood of 1974 and subsequent famine and migration of people including smallpox cases to the cities; and 3) the government decision to destroy the smallpox infected urban slums and resulting dissemination of smallpox throughout the country. Five program drivers led to the eventual eradication of smallpox in Bangladesh: 1) leadership and its decentralization to 415 Thanas, 2) expanded staffing (an increase from 50 persons per day in 1972 to 1,300 persons per day at the time of maximum activity in 1975), and financial resources (US$ 1.12 million per year in 1972 to US$ 4.78 million per year in 1975); 3) esprit de corps through job-specific capacity strengthening, regular communications by radio, and monthly meetings; 4) civil society partnerships, where public volunteers took on major responsibilities for reporting smallpox cases and containing smallpox in infected villages; and 5) unwillingness to take no for an answer when evidence mandated affirmative responses.
Footnotes
This paper honors the many Bangladeshis that achieved Smallpox Eradication including Abdul Kashem Joarder, Assistant Director for Smallpox Eradication; Mahbubar Rahman, Director of Malaria and the 1974 Emergency Plan Coordinator; Farida Huq, Director of the Smallpox Diagnostic Laboratory; Bangladeshi Health Workers, and the Bangladeshi Public.
Contributor Information
Stanley O. Foster, Professor of Global Health, Rollins School of Public Health, Emory University, Atlanta, GA USA.
Kenneth Hughes, Associate Professor, National University of Singapore (Retired), Singapore.
Daniel Tarantola, Visiting Professor, The University of New South Wales, Faculty of Medicine, School of Public Health and Community Medicine, Sydney, Australia.
John W. Glasser, Mathematical Epidemiologist, National Center for Immunization and Respiratory Diseases, CDC, Atlanta, GA USA.
References
- 1.Heitzman J, Worden RL, editors. Bangladesh: a Country Study. 2nd. Federal Research Division, Library of Congress; Washington, DC: 1989. [Google Scholar]
- 2.Joarder AK, Tarantola D, Tulloch JL. The Eradication of Smallpox from Bangladesh. World Health Organization; Regional Publications; New Delhi: World Health Organization South-East Asia Regional Office; 1980. (South-East Asia Series No 8). [Google Scholar]
- 3.Foster SO, Ward NA, Joarder AK, Arnt N, Tarantola D, Rahman M, Hughes K. Smallpox surveillance in Bangladesh: I -Development of surveillance containment strategy. Int J Epidemiol. 1980;9:329–34. doi: 10.1093/ije/9.4.329. [DOI] [PubMed] [Google Scholar]
- 4.Hughes K, Foster SO, Tarantola D, Mehta H, Tulloch JL, Joarder AK. Smallpox surveillance in Bangladesh: II -Smallpox facial scar survey assessment of surveillance effectiveness. Int J Epidemiol. 1980;9:335–40. doi: 10.1093/ije/9.4.335. [DOI] [PubMed] [Google Scholar]
- 5.Glasser JW, Foster SO, Millar DJ, Lane JM. Evaluating public health responses to re-introduced smallpox via dynamic, socially structured, and spatially distributed meta-population models. Clin Infect Dis. 2008;46S:182–94. doi: 10.1086/524382. [DOI] [PubMed] [Google Scholar]
- 6.Tarantola D, Foster SO. Enhancing capacity towards a global public health goal: From Smallpox Eradication to Contemporary Global Health Initiatives Vaccine. 2011 doi: 10.1016/j.vaccine.2011.07.027. this issue. [DOI] [PubMed] [Google Scholar]
- 7.Foege WH, Millar JD, Henderson DA. Smallpox Eradication in West and Central Africa. Bull WHO. 1975;52:209–222. [PMC free article] [PubMed] [Google Scholar]


