Abstract
OBJECTIVES
To assess the incidence of chronic illness and its effect on veteran centenarians.
DESIGN
Retrospective longitudinal cohort study.
SETTING
United States Veterans Affairs Corporate Data Warehouse (CDW).
PARTICIPANTS
Community-dwelling veterans born between 1910 and 1915 who survived to at least age 80 (N = 86,892; 31,121 octogenarians, 52,420 nonagenarians, 3,351 centenarians).
MEASUREMENTS
The Kaplan–Meier method was used to estimate cumulative incidence of chronic conditions according to age group. Incidence rates were compared using the log-rank test. Cox proportional hazards models were used to estimate unadjusted hazard ratios.
RESULTS
Ninety-seven percent of Centenarians were male, 88.0% were white, 31.8% were widowed, 87.5% served in World War II, and 63.9% did not have a service-related disability. The incidence rates of chronic illnesses were higher in octogenarians than centenarians (atrial fibrillation, 15.0% vs 0.6%, P < .001; heart failure, 19.3% vs 0.4%, P < .001; chronic obstructive pulmonary disease, 17.9% vs 0.6%, P < .001; hypertension, 29.6% vs 3.0%, P < .001; end-stage renal disease, 7.2% vs 0.1%, P < .001; malignancy, 14.1% vs 0.6%, P < .001; diabetes mellitus, 11.1% vs 0.4%, P < .001; stroke, 4.6% vs 0.4%, P < .001) and in nonagenarians than centenarians (atrial fibrillation, 13.2% vs 3.5%, P < .001; heart failure, 15.8% vs 3.3%, P < .001; chronic obstructive pulmonary disease, 11.8% vs 3.5%, P < .001; hypertension, 27.2% vs 12.8%, P < .001; end-stage renal disease, 11.9% vs 4.5%, P < .001; malignancy, 8.6% vs 2.3%, P < .001; diabetes mellitus, 7.5% vs 2.2%, P < .001; and stroke, 3.5% vs 1.3%, P < .001).
CONCLUSION
In a large cohort of predominantly male community-dwelling elderly veterans, centenarians had a lower incidence of chronic illness than those in their 80s and 90s, demonstrating similar compression of morbidity and extension of health span observed in other studies.
Keywords: centenarians, nonagenarians, octogenarians, chronic illness, incidence, veterans
Longevity beyond 80 years of age is no longer uncommon1–4 Despite accounting for only 0.02% of the United States population, the number of centenarians in the U.S. is growing rapidly. The U.S. Social Security Administration predicts that the number of centenarians in the United States will exceed 1 million before the end of this century.5 This group of survivors is composed of individuals who may serve as a model for successful aging.6,7 Significant improvements in public health have contributed to this success—specifically, lower early childhood mortality, the introduction of antibiotics early in the 20th century, and adoption of healthy habits and disease preventive strategies at younger ages.1,8 These factors have added almost 30 years to life expectancy, resulting in delayed mortality.7
The Framingham Heart Study and Honolulu Heart program have improved our understanding of life span and health span through inclusion of aging-related factors to their existing studies of older adults with several decades of follow-up. In addition, given the prognostically heterogeneous group, elderly patients are poorly represented in clinical trials, however, interest in this group has increased steadily in recent decades. Globally and in the United States, several teams have been studying centenarians and their habits, support systems, personalities, coping styles, cognition, and genetics.8–15
No study to date has examined U.S. military or Veteran centenarians. Veterans centenarians are predominantly male, and most have outlived their spouses. This group also served in World War II and experienced combat, a unique occupational exposure that may provide an opportunity to examine resilience in this particular group of survivors. Furthermore, the Veteran Health Administration (VHA), with its longstanding adoption of an electronic health record (EHR) system, provides an unparalleled opportunity to access centenarian data for hypothesis testing, adding to current knowledge regarding this unique group of survivors.
This study was designed to determine characteristics of community-dwelling male veteran centenarians cared for in the VHA system and assess the incidence of chronic illness and its effect on survival.
METHODS
Study Design
This was a retrospective longitudinal cohort study of elderly U.S. veterans. Incidence rates of chronic illnesses including atrial fibrillation, congestive heart failure, chronic obstructive pulmonary disease (COPD), hypertension, renal failure, cancer, diabetes mellitus, and stroke in centenarians were compared with those in octogenarians and nonagenarians. Data from the Department of Veterans Affairs (VA) Informatics and Computing Infrastructure were used. The Corporate Data Warehouse is a national repository of data from several VHA data sources, including clinical and health utilization data.
Study Population
The cohort included 86,892 veterans born between 1910 and 1915 who had records in the VA Informatics and Computing Infrastructure system. To confirm VA care, veterans who had had fewer than two outpatient visits since age 80 were excluded. Institutionalized veterans admitted to a nursing home or hospice were also excluded. To construct the three arms of the cohort, mortality data were obtained from the VHA Vital Status File, which includes dates of death for veterans who had received care from the VHA since 1992, were enrolled in the VHA, or had received compensation or pension benefits from the Veterans Benefit Administration since 2002. Multiple VHA and non-VHA data sources contribute to the VHA Vital Status File, including the Beneficiary Identification Records Locator Subsystem Death File, VHA Medicare Vital Status File, and the Social Security Administration Death Master File.16
In this study of veterans, octogenarians were defined as those who lived to at least age 80, nonagenarians as those who lived to at least age 90, and centenarians as those who lived to at least age 100. All participants were community-dwelling veterans who had not been admitted to a VA nursing home, including a skilled nursing facility or hospice, irrespective of length of stay.
Outcome Variables
The primary endpoint for this study was incidence of chronic diseases occurring on or after age 80. International Classification of Diseases, Ninth Revision (ICD-9) diagnostic codes were used to capture all diagnoses. Incidence of comorbidity was defined using the Elixhauser Agency for Healthcare Research and Quality-WebICD-9, Clinical Modification, coding algorithm (Appendix S1).17 For comorbidities, participants with a diagnosis before the age of 80 were excluded. Two outpatient ICD-9 codes or one inpatient ICD-9 code was required to count as an incident case of comorbidity.
Age at time of incidence of the condition was calculated using the time difference between date of diagnosis and date of birth. Data for participants who did not reach an endpoint by age 100 were censored at date of death for octogenarians and nonagenarians.
Statistical Analysis
The Kaplan–Meier method was used to estimate the probability of each endpoint according to the ages of the participants. Differences between octogenarians, nonagenarians, and centenarians were tested using log-rank tests. At ages 89 and 99, a two-sided P-value was computed on the basis of the difference between the Kaplan–Meier estimates at that time point, with standard errors obtained using the Greenwood formula. A Cox proportional hazards model was used to estimate hazard ratios and confidence intervals for the study outcomes comparing the three age groups.
RESULTS
Of the 86,892 veterans born between 1910 and 1915, 31,121 were octogenarians, 52,420 were nonagenarians, and 3,351 were centenarians. Overall baseline demographic characteristics were similar in the three groups (Table 1). The cohort was more than 97.0% male, 88.0% Caucasian, and 31% widowed; more than 63.9% had no service connection disability, and more than 87.5% had served in World War II.
Table 1.
Baseline Demographic Characteristics
| Characteristic | Octogenarians, n = 31,121 |
Nonagenarians, n = 52,420 |
Centenarians, n = 3,351 |
|---|---|---|---|
| Age, median (interquartile range) | 87 (86–88) | 92 (91–94) | 101 (100–102) |
| Male | 34,017 (97.5) | 47,775 (96.8) | 2,520 (94.1) |
| Marital status | |||
| Married | 18,761 (53.8) | 24,418 (49.5) | 1,052 (39.3) |
| Single | 1,991 (5.7) | 2,532 (5.1) | 123 (4.6) |
| Widowed | 9,617 (27.6) | 16,756 (34.0) | 1,299 (48.5) |
| Other or missing | 4,501 (12.9) | 5,637 (11.4) | 205 (7.6) |
| Race | |||
| African American | 2,457 (7.0) | 2,501 (5.1) | 138 (5.1) |
| American Indian or Alaskan Native | 5 (0.0)1 | 7 (0.0)1 | 0 (0.0) |
| Asian or Pacific Islander | 139 (0.4) | 170 (0.3) | 10 (0.4) |
| Caucasian | 30,499 (87.5) | 43,773 (88.7) | 2,205 (82.3) |
| Other or missing | 1,770 (5.1) | 2,892 (5.9) | 564 (21.0) |
| Service-connected disability, % | |||
| <70 | 10,857 (31.1) | 14,256 (28.9) | 768 (28.7) |
| ≥70 | 2,204 (6.3) | 3,067 (6.2) | 221 (8.2) |
| None | 21,809 (62.5) | 32,020 (64.9) | 1,690 (63.1) |
| Rural location | 11,710 (33.6) | 15,957 (32.3) | 702 (26.2) |
| Period of service | |||
| Korean War | 1,141 (3.3) | 1,531 (3.1) | 72 (2.7) |
| Vietnam War | 935 (2.7) | 1,136 (2.3) | 77 (2.9) |
| World War II | 31,592 (90.6) | 41,985 (85.1) | 2,479 (92.5) |
| Other | 1,202 (3.4) | 4,691 (9.5) | 51 (1.9) |
Atrial Fibrillation
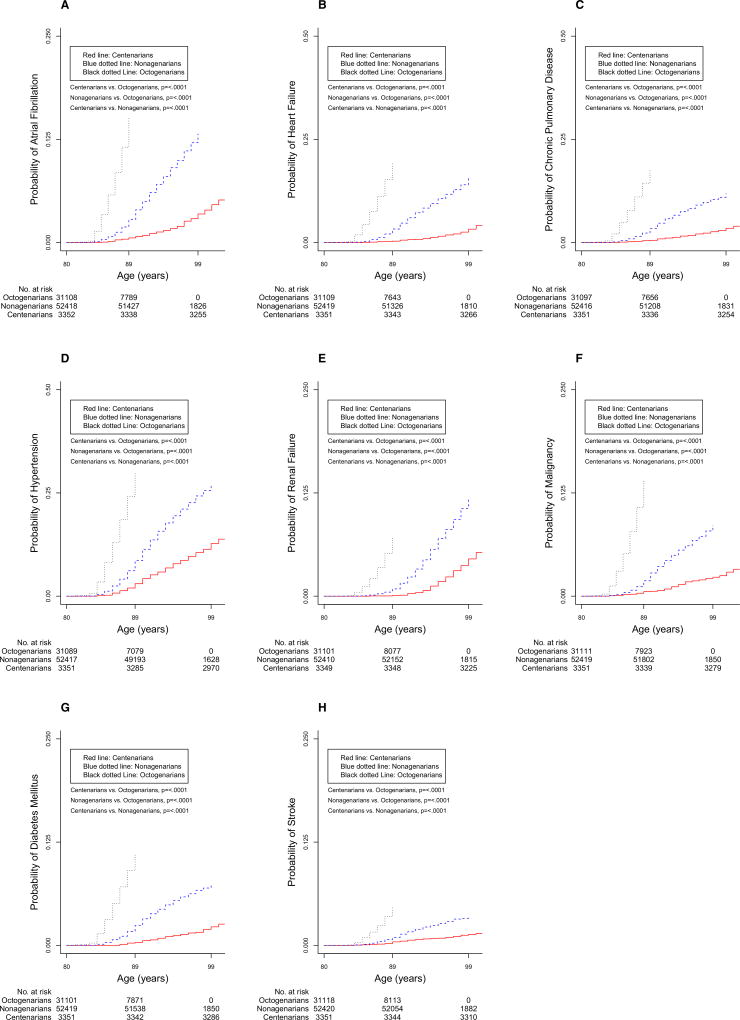
By age 89, the estimated incidence of atrial fibrillation was 0.6% in centenarians (reference group), 15.0% in octogenarians, and 2.8% in nonagenarians. Fourteen veterans with a recorded diagnosis of atrial fibrillation before the age of 80 were excluded. A significant difference was found in the Kaplan–Meier estimates of atrial fibrillation incidence at age 89 between centenarians and octogenarians (P < .001), by age 99, the incidence of atrial fibrillation was 3.5% for centenarians and 13.2% for nonagenarianss. The difference between centenarians and nonagenarians was also significant (P < .001) (Figure 1A). Centenarians had a lower incidence of atrial fibrillation after age 80 than did octogenarians and nonagenarians (Table 2).
Figure 1.
Kaplan–Meier survival curves for incidence of comorbidity of octogenarian, nonagenarian, and centenarian veterans. Red line: centenarians. Blue dotted line: nonagenarians. Black dotted line: octogenarians. [Color figure can be viewed at wileyonlinelibrary.com]
Table 2.
Chronic Disease Incidence of Octogenarians and Nonagenarians Compared with Centenarians (Reference Group)
| Disease | End Point, n |
Hazard Ratio (95% Confidence Interval) |
|---|---|---|
| Atrial fibrillation | ||
| Octogenarians | 3,121 | 24.70 (20.29–30.07) |
| Nonagenarians | 3,879 | 4.13 (3.42–4.99) |
| Centenarians | 116 | 1 |
| Heart failure | ||
| Octogenarians | 4,092 | 36.54 (29.90–44.65) |
| Nonagenarians | 4,602 | 5.37 (4.42–6.52) |
| Centenarians | 109 | 1 |
| Chronic obstructive pulmonary disease | ||
| Octogenarians | 3,912 | 22.53 (18.55–27.36) |
| Nonagenarians | 4,002 | 3.72 (3.08–4.49) |
| Centenarians | 116 | 1 |
| Hypertension | ||
| Octogenarians | 6,605 | 9.80 (8.83–10.88) |
| Nonagenarians | 9,480 | 2.39 (2.16–2.64) |
| Centenarians | 428 | 1 |
| Renal failure | ||
| Octogenarians | 1,366 | 25.94 (21.27–31.63) |
| Nonagenarians | 2,641 | 2.87 (2.42–3.41) |
| Centenarians | 151 | 1 |
| Cancer | ||
| Octogenarians | 2,900 | 32.09 (25.263–40.752) |
| Nonagenarians | 2,654 | 3.841 (3.05–4.84) |
| Centenarians | 77 | 1 |
| Diabetes mellitus | ||
| Octogenarians | 2,437 | 18.63 (14.64–23.70) |
| Nonagenarians | 2,597 | 3.59 (2.84–4.54) |
| Centenarians | 75 | 1 |
| Stroke | ||
| Octogenarians | 908 | 13.60 (9.87–18.74) |
| Nonagenarians | 1,162 | 2.75 (2.02–3.74) |
| Centenarians | 44 | 1 |
Proportion of participants with the end points was estimated using the Kaplan–Meier method.
Heart Failure
By age 89, the estimated incidence of HF was 0.4% in centenarians, 19.3% in octogenarians, and 3.3% in nonagenarians. The study excluded 13 veterans with a recorded diagnosis of HF before the age of 80. Kaplan–Meier estimates of HF incidence showed a significant difference at age 89 between centenarians and octogenarians (P < .001), by age 99, the incidence of HF increased to 3.3% for centenarians and 15.8% for nonagenarians. The difference between centenarians and nonagenarians was significant (P < .001) (Figure 1B). Centenarians had a lower incidence of HF after age 80 than did octogenarians and nonagenarians (Table 2).
Chronic Obstructive Pulmonary Disease
By age 89, the estimated incidence of COPD was 0.6% in centenarians, 17.9% in octogenarians, and 3.4% in nonagenarians. The study excluded 28 veterans with a recorded diagnosis of COPD before the age of 80. Kaplan–Meier estimates of COPD at age 89 showed a significant difference between centenarians and octogenarians (P < .001), by age 99, the incidence of COPD increased to 3.5% for centenarians and 11.8% for nonagenarians. The difference between centenarians and nonagenarians was significant (P < .001) (Figure 1C). Centenarians had a lower incidence of COPD after age 80 than did octogenarians and nonagenarians (Table 2).
Hypertension
By age 89, the estimated incidence of hypertension was 3.0% in centenarians, 29.6% in octogenarians, and 8.6% in nonagenarians. The study excluded 35 veterans with a recorded diagnosis of hypertension before the age of 80. The Kaplan–Meier estimates of hypertension showed a significant difference between centenarians and octogenarians at age 89 (P < .001), by age 99, the incidence of hypertension increased to 12.8% for centenarians and 27.2% for nonagenarians. The difference between centenarians and nonagenarians was significant (P < .001) (Figure 1D). Centenarians had a lower incidence of hypertension after age 80 than did octogenarians and nonagenarians (Table 2).
End-Stage Renal Disease
By age 89, the estimated incidence of ESRD was 0.1% in centenarians, 7.2% in octogenarians, and 0.9% in nonagenarians. The study excluded 32 veterans with a recorded diagnosis of ESRD before the age of 80. A significant difference was found in the Kaplan–Meier estimates of ESRD incidence at age 89 between centenarians and octogenarians (P < .001), by age 99, the incidence of ESRD increased to 4.5% for centenarians and 11.9% for nonagenarians. The difference between centenarians and nonagenarians was statistically significant (P < .001) (Figure 1E). Centenarians had a lower incidence of ESRD after age 80 than did octogenarians and nonagenarians (Table 2).
Cancer
By age 89, the estimated incidence of malignancy was 0.6% in centenarians, 14.1% in octogenarians, and 1.9% in nonagenarians. The study excluded 11 veterans with a recorded diagnosis of cancer before the age of 80. Kaplan–Meier estimates of cancer incidence at age 89 showed a significant difference between centenarians and octogenarians (P < .001), by age 99, the incidence of cancer increased to 2.3% for centenarians and 8.6% for nonagenarians. The difference between centenarians and nonagenarians was statistically significant (P < .001) (Figure 1F). Centenarians had a significantly lower incidence of cancer than octogenarians and nonagenarians (Table 2).
Diabetes Mellitus
By age 89, the estimated incidence of diabetes mellitus was 0.4% in centenarians, 11.1% in octogenarians, and 2.4% in nonagenarians. The study excluded 21 veterans with a recorded diagnosis of diabetes mellitus before the age of 80. A significant difference was seen in the Kaplan–Meier estimates of diabetes mellitus incidence at age 89 between centenarians and octogenarians (P < .001), by age 99, the incidence of diabetes mellitus increased to 2.2% for centenarians and 7.5% for nonagenarians. The difference between centenarians and nonagenarians was statistically significant (P < .001) (Figure 1G). Centenarians had a lower incidence of diabetes mellitus after age 80 than did octogenarians and nonagenarians (Table 2).
Stroke
By age 89, the estimated incidence of stroke was 0.4% in centenarians, 4.6% in octogenarians, and 1.0% in nonagenarians. The study excluded three veterans with a diagnosis of stroke before the age of 80. A significant difference was seen in the Kaplan–Meier estimates of stroke incidence at age 89 between centenarians and octogenarians (P < .001), by age 99, the incidence of stroke increased to 1.3% for centenarians and 3.5% for nonagenarians. The difference between centenarians and nonagenarians was statistically significant (P < .001) (Figure 1H). Centenarians had a lower incidence of stroke after age 80 than did octogenarians and nonagenarians (Table 2).
DISCUSSION
This study demonstrates that, in a large VA cohort of community-dwelling predominately male veterans, centenarians had a lower incidence of chronic illnesses after age 80 than did octogenarians and nonagenarians. The survival curves demonstrated similar consequential patterns of disease incidence in the three study groups, with octogenarians having the highest incidence rates, followed by nonagenarians and centenarians. To the best of the authors’ knowledge, this is the largest sample to date of these age groups, with the additional advantage of being matched for birth year cohort. Furthermore, population-based centenarian studies have included overwhelmingly female participants except in rare areas of the world.18 This cohort of predominantly men, in contrast to centenarian cohorts outside the VA system of care, is well positioned to stimulate much-needed research that may make important contributions to current knowledge about this group of survivors.
One or more of several hypotheses might explain these findings. One that is widely deliberated states that centenarians markedly delay onset or even escape diseases that would otherwise be lethal at younger ages because of what is known as compression of morbidity.4,19 This hypothesis might explain the sequential trend in the survival curves; the study found that 85% of all centenarians had had no incidence of major chronic conditions between the ages of 80 and 99. In a population-based study of the New England Centenarian Study, 32% of male and 15% of female subjects fit the escaper profile, but when only the most-lethal diseases of the elderly population were examined (heart disease, nonskin cancer, stroke), 87% of male and 83% of female subjects delayed or escaped these diseases.20 Poorer quality of life in advanced age because of increases in disability and degenerative diseases counterbalances the survival advantage of women.21 Male veteran centenarians tend to have a better health profile than female centenarians, and their incidence of having one or more chronic illness ranges from 0.1% to 12.8%, which is lower than that in the general population.
The progress being made in lengthening lifespans is largely from medical and public health efforts, improved nutrition and healthier lifestyles. The VA healthcare system provides open access to healthcare for all enrolled veterans. Financial barriers to receiving care are minimized, and the differences in socioeconomic factors are less significant than in the general population, but it is unclear whether greater access to care, including prevention and treatment for all veterans, as well as programs that offer social support against hardship, resulted in markedly longer life expectancy in this cohort than in similar non-VA cohorts.
Low incidences of cardiovascular disease, stroke, diabetes mellitus and cancer were observed in all three study groups (Table S1). The veteran centenarian population has a pattern of compression of morbidities similar to that observed in other cohorts with exceptional longevity.4 The lower incidence of cardiovascular disease has been observed in veteran and nonveteran populations, as reported in a small prospective study that included 93 veterans; centenarians had lower incidences of hypertension, diabetes mellitus, and myocardial infarction than did younger individuals.22 In addition, in a study of death certificates, centenarians had evidence of lower rates of diabetes mellitus and myocardial infarction,23 in contrast to the widely accepted concept of heart failure as a disease of elderly adults. It appears that this elderly population may somehow skip the usual cardiac risk factors. The lower incidence of chronic illness in centenarians is intriguing; it is plausible that centenarians have fewer cardiovascular risk factors, genetic variants that effectively counteract those risk factors, or possibly both. Further studies are needed to explore these hypotheses.
Studies have shown that hypertension is common in older persons and is the most common risk factor for cardiovascular and cerebrovascular morbidity and mortality.24 Current study data show that octogenarians and nonagenarians were much more likely to have hypertension than were centenarians. Although this association was not as strong as for other comorbidities such as heart failure, it is plausible that it may not have been possible to capture data for participants who developed hypertension in middle age, before the inception of EHRs.
As individuals age, cardiovascular events and hypertension are among the most-frequent illnesses experienced. The Framingham Study found that the lifetime incidence of persons aged 55–65 developing hypertension was 90%,25 although it is intriguing to see the much lower rate of other associated cardiovascular illnesses in this age group, which supports the delayer theory.20
Several limitations of this study need to be acknowledged. The cohort was predominantly community-dwelling men with no history of admission to VA nursing homes, skilled nursing facilities, or hospice; therefore, results may not be applicable to all veteran centenarians, and it is plausible that findings could be different for women. Study of veteran male centenarians may provide an opportunity for further hypothesis testing and fill the knowledge gap in many areas, because the vast majority of centenarians are female in the general population, although it appears that veteran women outlived men in this cohort, reflecting the general population experience. Another limitation is that diagnoses made before the early 1990s were not reliably captured in the database. The risk of having certain comorbidities may have been underestimated for all three cohorts.
Data were not available for veterans who received care in the private sector using their Medicare coverage; it is plausible that a number of veterans in the cohort are dual-care beneficiaries.26 Data were not available on mobility. An analysis of U.S. data concluded that overall prevalence of loss of mobility increased between 1998 and 2008.27 Another limitation was the lack of genetic information on participants, although data indicate that the role of genetic factors is modest in determining how long individuals live,28–30 and environmental factors can strongly affect this. Data were not available on socioeconomic status, education, diet, and function, all of which may have influenced the findings. Finally, the EHR became the major data repository in the early years of this study. To mitigate look-back errors related to EHR data entry, multiple sources of data were assimilated from within the VA system.
In conclusion, in a large cohort of community-dwelling veterans, centenarians had a lower incidence of disease beyond age 80 than did octogenarians and nonagenarians. The VA centenarians demonstrated similar compression of morbidity and extension of health span observed in other cohorts, underscoring the importance of further studying factors contributing to health and longevity in this group of survivors.
Supplementary Material
Appendix S1. Elixhauser Agency for Healthcare Research and Quality-Web International Classification of Diseases, Ninth Revision, Clinical Modification, Coding Algorithm
Table S1. Estimates of the Cumulative Incidence of Conditions in Elderly Veterans
Acknowledgments
We are grateful to the veteran centenarian study team, including Helen Sheriff, Shervin AhmadBeygi, Chris Hastings, and Paula Gorman. The study was approved by the the Washington DC VA Institutional Review Board (IRB). The opinions are the authors’ and do not reflect those of the VA.
Financial Disclosure: Dr. Kheirbek received funds from the Veterans Affairs Capitol Health Care Network to establish the Center for Health and Aging at the Washington DC VA Medical Center.
Footnotes
Conflict of interest: None.
Please note: Wiley-Blackwell is not responsible for the content, accuracy, errors, or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
References
- 1.Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–135. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- 2.Sebastiani P, Sun FX, Andersen SL, et al. Families enriched for exceptional longevity also have increased health-span: Findings from the long life family study. Front Public Health. 2013;1:38. doi: 10.3389/fpubh.2013.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andersen SL, Sun JX, Sebastiani P, et al. Personality factors in the Long Life Family Study. J Gerontol B Psychol Sci Soc Sci. 2013;68B:739–749. doi: 10.1093/geronb/gbs117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ismail K, Nussbaum L, Sebastiani P, et al. Compression of morbidity is observed across cohorts with exceptional longevity. J Am Geriatr Soc. 2016;64:1583–1591. doi: 10.1111/jgs.14222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kincel B. The Centenarian Population: 2007–2011. [Accessed June 21, 2016];American Community Survey Briefs 2014 [on-line] Available at https://www.census.gov/prod/2014pubs/acsbr12–18.pdf.
- 6.Willcox BJ, Willcox DC, Ferrucci L. Secrets of healthy aging and longevity from exceptional survivors around the globe: Lessons from octogenarians to supercentenarians. J Gerontol A Biol Sci Med Sci. 2008;63A:1181–1185. doi: 10.1093/gerona/63.11.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Terry DF, Sebastiani P, Andersen SL, et al. Disentangling the roles of disability and morbidity in survival to exceptional old age. Arch Intern Med. 2008;168:277–283. doi: 10.1001/archinternmed.2007.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fries JF. Measuring and monitoring success in compressing morbidity. Ann Intern Med. 2003;139(5 Pt 2):455–459. doi: 10.7326/0003-4819-139-5_part_2-200309021-00015. [DOI] [PubMed] [Google Scholar]
- 9.Willcox DC, Willcox BJ, Poon LW. Centenarian studies: Important contributors to our understanding of the aging process and longevity. Curr Gerontol Geriatr Res. 2010;2010:484529. doi: 10.1155/2010/484529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Franceschi C, Bonafe M. Centenarians as a model for healthy aging. Biochem Soc Trans. 2003;31:457–461. doi: 10.1042/bst0310457. [DOI] [PubMed] [Google Scholar]
- 11.Barzilai N, Atzmon G, Derby CA, et al. A genotype of exceptional longevity is associated with preservation of cognitive function. Neurology. 2006;67:2170–2175. doi: 10.1212/01.wnl.0000249116.50854.65. [DOI] [PubMed] [Google Scholar]
- 12.Puca AA, Daly MJ, Brewster SJ, et al. A genome-wide scan for linkage to human exceptional longevity identifies a locus on chromosome 4. Proc Natl Acad Sci USA. 2001;98:10505–10508. doi: 10.1073/pnas.181337598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poon LW, Jazwinski M, Green RC, et al. Methodological considerations in studying centenarians: Lessons learned from the Georgia Centenarian Studies. Annu Rev Gerontol Geriatr. 2007;27:231–264. [PMC free article] [PubMed] [Google Scholar]
- 14.Serna E, Gambini J, Borras C, et al. Centenarians, but not octogenarians, up-regulate the expression of microRNAs. Sci Rep. 2012;2:961. doi: 10.1038/srep00961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sebastiani P, Perls TT. The genetics of extreme longevity: Lessons from the New England Centenarian Study. Front Genet. 2012;3:277. doi: 10.3389/fgene.2012.00277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sohn MW, Arnold N, Maynard C, et al. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metr. 2006;4:2. doi: 10.1186/1478-7954-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 18.Poulain M, Pes GM, Grasland C, et al. Identification of a geographic area characterized by extreme longevity in the Sardinia island: The AKEA study. Exp Gerontol. 2004;39:1423–1429. doi: 10.1016/j.exger.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 19.Andersen SL, Sebastiani P, Dworkis DA, et al. Health span approximates life span among many supercentenarians: Compression of morbidity at the approximate limit of life span. J Gerontol A Biol Sci Med Sci. 2012;67A:395–405. doi: 10.1093/gerona/glr223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Evert J, Lawler E, Bogan H, et al. Morbidity profiles of centenarians: Survivors, delayers, and escapers. J Gerontol A Biol Sci Med Sci. 2003;58A:232–237. doi: 10.1093/gerona/58.3.m232. [DOI] [PubMed] [Google Scholar]
- 21.Ostan R, Monti D, Gueresi P, et al. Gender, aging and longevity in humans: An update of an intriguing/neglected scenario paving the way to a gender-specific medicine. Clin Sci (Lond) 2016;130:1711–1725. doi: 10.1042/CS20160004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Selim AJ, Fincke G, Berlowitz DR, et al. Comprehensive health status assessment of centenarians: Results from the 1999 large health survey of veteran enrollees. J Gerontol A Biol Sci Med Sci. 2005;60A:515–519. doi: 10.1093/gerona/60.4.515. [DOI] [PubMed] [Google Scholar]
- 23.Gessert CE, Elliott BA, Haller IV. Dying of old age: An examination of death certificates of Minnesota centenarians. J Am Geriatr Soc. 2002;50:1561–1565. doi: 10.1046/j.1532-5415.2002.50413.x. [DOI] [PubMed] [Google Scholar]
- 24.Chobanian AV. Time to reassess blood-pressure goals. N Engl J Med. 2015;373:2093–2095. doi: 10.1056/NEJMp1513290. [DOI] [PubMed] [Google Scholar]
- 25.Vasan RS, Beiser A, Seshadri S, et al. Residual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart Study. JAMA. 2002;287:1003–1010. doi: 10.1001/jama.287.8.1003. [DOI] [PubMed] [Google Scholar]
- 26.Halanych JH, Wang F, Miller DR, et al. Racial/ethnic differences in diabetes care for older veterans: Accounting for dual health system use changes conclusions. Med Care. 2006;44:439–445. doi: 10.1097/01.mlr.0000207433.70159.23. [DOI] [PubMed] [Google Scholar]
- 27.Crimmins EM, Beltran-Sanchez H. Mortality and morbidity trends: Is there compression of morbidity? J Gerontol B Psychol Sci Soc Sci. 2011;66B:75–86. doi: 10.1093/geronb/gbq088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perls TT, Wilmoth J, Levenson R, et al. Life-long sustained mortality advantage of siblings of centenarians. Proc Natl Acad Sci USA. 2002;99:8442–8447. doi: 10.1073/pnas.122587599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.vB Hjelmborg J, Iachine I, Skytthe A, et al. Genetic influence on human lifespan and longevity. Hum Genet. 2006;119:312–321. doi: 10.1007/s00439-006-0144-y. [DOI] [PubMed] [Google Scholar]
- 30.Hirose N, Arai Y, Yamamura K, et al. Suggestions from a centenarian study—aging and inflammation. Nihon Ronen Igakkai Zasshi. 2001;38:121–124. doi: 10.3143/geriatrics.38.121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Elixhauser Agency for Healthcare Research and Quality-Web International Classification of Diseases, Ninth Revision, Clinical Modification, Coding Algorithm
Table S1. Estimates of the Cumulative Incidence of Conditions in Elderly Veterans