Abstract
Introduction
There is fragmented information about the different needs following a spinal cord injury (SCI). Expressed SCI needs can be met or unmet, they change along the rehabilitation continuum (eg, acute, rehabilitation and reintegration into the community) and can be different for traumatic and non traumatic SCI. The general objective of this scoping study is to evaluate and integrate the needs of individuals with traumatic and non-traumatic SCI, their family caregivers and those reported by rehabilitation professionals from the time of rehabilitation admission to community reintegration. The specific objectives are to: (A) synthesise the needs of individuals with SCI as perceived by themselves, their family caregivers and rehabilitation professionals using two theoretical models, (B) classify needs as met and unmet, (C) explore the evolution of met/unmet needs from the time of rehabilitation admission to community reintegration and (D) provide recommendations to improve SCI care.
Methods and analysis
(A) identifying the most frequent met and unmet needs reported by adults with traumatic and non-traumatic SCI, their family caregivers and their rehabilitation professionals from the time of rehabilitation admission to community reintegration; (B) identifying relevant studies with a search in electronic databases; (C) charting the data based on categories refined and adjusted with a stakeholder group; (D) collating, summarising and reporting the results using two analytical frameworks (Maslow’s hierarchical model of human needs and the Ferrans et al’s model of health-related quality of life) and (E) a stakeholder consultation phase.
Ethics and dissemination
The results of this scoping study will allow understanding SCI needs from the time of rehabilitation admission to community reintegration from the perspective of different stakeholders. An integrated master report combining the needs of individuals with SCI from the perspectives of different stakeholders from the time of rehabilitation admission to community reintegration will follow the consultation meetings.
Keywords: Spinal Cord Injury, needs, caregiver, healthcare, scoping study
Strengths and limitations of this study.
Description of spinal cord injury (SCI) met and unmet needs in different moments of the rehabilitation process.
Comprehensive definition of needs in the context of SCI.
Multiperspective approach including family caregivers, healthcare professionals and individuals with SCI.
Synthesis of SCI needs using two theoretical frameworks to capture both personal and environmental variables.
Knowledge translation plan to inform stakeholders about the conclusions.
Scoping studies do not appraise the quality of the evidence.
Generalisation is limited to the SCI population.
Studies in languages other than English are excluded.
Introduction
Spinal cord injury (SCI) corresponds to a neurological condition affecting 330–400 per 100 000 Canadians living in the community.1 According to provincial data, traumatic SCI affects mainly young and middle-aged adults, with men showing the highest prevalence regardless of age group (men-to-women ratio of 4.4:1).2 Traumatic SCI is concentrated in younger populations, while non-traumatic SCI is condensed in older age groups.3 In addition, Canadian estimates indicate that compared with non-traumatic SCI (49%), the prevalence is higher for traumatic SCI (51%).3 Furthermore, SCI is a high-cost chronic disability4 involving changes in roles, self-image, body function, social interactions and family relationships.5
For individuals with SCI, the injury permanently transforms their lives. Indeed, SCI can result in diverse motor, sensory and autonomic problems.6 Mobility impairment (eg, paraplegia and tetraplegia), bowel and bladder incontinence, loss of sensation and sexual dysfunction are common following SCI.7 As a result, individuals with SCI have complex health needs as their condition includes chronic multimorbidity, mainly associated with the development of several secondary health conditions (eg, pain and pressure ulcers).7 In addition, compared with community estimates, higher rates of psychological disorders can be present in 17%–25% of individuals with SCI.8 Particularly, between 18% and 37% of individuals with SCI experience depression.9 10
Also, studies regarding long-term outcomes indicate that individuals with SCI have low employment rates 20 years postinjury.11 A review shows that employment rates following SCI range from 11% to 69% depending on the definition of employment and differences in the study methodology.12 Thus, SCI has an important functional, psychological and social impact on individuals that requires an integrated care approach across the continuum from acute care to community living. For instance, Craven et al (2012) stressed the need for lifetime access to rehabilitation healthcare for individuals with SCI.13 Individuals with SCI require follow-up to address their evolving health needs, including the challenges that represent ageing with a disability and the development of SCI-related secondary health conditions.
For families, the unforeseen nature of the injury leads some of the members into an ‘unexpected career’ as family caregivers.14 As family caregivers normally do not have training for the caregiving tasks (eg, bathing, dressing and feeding), they can experience role transitions,15 strain,16 isolation,7 burden,17 poor leisure satisfaction,18 reduced ability to become and remain employed19 and marital disruption.20
Different perspectives in SCI needs
Individuals with SCI and their families, as well as healthcare professionals must work together to effectively meet the diverse post-SCI needs.21 For rehabilitation professionals, understanding the interplay of different factors influencing support mechanisms to assist the transition to home and community after discharge can facilitate social reintegration of the individual with SCI.22 In fact, rehabilitation professionals have an understanding of the needs and barriers that individuals with SCI can encounter. Their observations are valuable as experts due to their professional roles with good knowledge about the problems that individuals with SCI face.23 Also, they can directly contribute to the understanding of the rehabilitation process and the predischarge and postdischarge challenges during service delivery. For instance, shorter lengths of stay during inpatient rehabilitation can diminish the opportunities to provide information and efficiently train dyads of individuals with SCI and their family caregivers when they return to the community.22 Thus, the healthcare professional’s perspective is necessary when depicting a thorough picture of the barriers to meet the needs of individuals with SCI. For instance, a study showed that compared with physiotherapists, some individuals with SCI have unrealistically high expectations about walking 1-year postinjury.24 Another study showed that when the perspectives of individuals with SCI are acknowledged during rehabilitation, they become more committed to therapy, they express more confidence in their treating clinicians and they have better satisfaction and outcomes.25
Compared with family caregivers of different neurological conditions, family caregivers of individuals with SCI have experienced more frequent physical distress and present increased odds of coronary heart disease and obesity.26 Thus, their experience as family caregivers is crucial to understand the needs of individuals with SCI, as they progressively become experts by experience while providing care, supporting and addressing the needs of the care recipient with SCI. Family caregivers are an important resource in the treatment of individuals with SCI considering that the quality of the care they provide matches or exceeds the quality of professional care.27 However, unmet caregiver needs may prevent optimal care and negatively affect the health of both the care recipients and their own. From a clinical perspective, understanding the needs of individuals with SCI, knowing the person and working with the family can be beneficial to guide their healthcare and improve outcomes.28 As unmet needs have a direct relationship with diminished quality of life,29 it is mandatory to understand them and to find ways to meet them. In consequence, obtaining a comprehensive picture of needs by integrating the different perspectives of professionals, family caregivers and individuals with SCI is paramount.
Changing needs in the rehabilitation continuum
The challenge is in understanding the evolution of these needs as they change over time. The literature on SCI needs indicates that in the first year postdischarge, the fulfilment of critical needs (eg, housing and transportation) is below 60%,30 while the long-term care needed is higher than the care received for information and psychosocial care needs.31 Furthermore, there are differences in needs between individuals with traumatic and non-traumatic SCI. Compared with individuals with non-traumatic SCI (>70%), individuals with traumatic SCI (>85%) report more expressed needs on equipment and technical aids, short-distance transportation, accessible housing, general healthcare and SCI-specialised healthcare.29 In addition, individuals with non-traumatic SCI report more unmet needs in accessible housing, job training and peer support.32 Finally, fully addressing the needs of individuals’ with SCI must include evaluating and targeting the needs of family caregivers. Family caregivers of individuals with SCI report health information needs as the most important and emotional support needs as those most often unmet.33 Among the health and social consequences of unmet needs, individuals with SCI can present higher rates of multimordidity,7 34 dissatisfaction with their lives, high rates of psychological problems,9 poor quality of life29 and poor long-term integration into the community.30 Also, unmet needs lead their family caregivers to invest more hours in their care.27
Gaps in understanding met and unmet needs
Previous studies have evaluated SCI needs separately at different points of the rehabilitation continuum (eg, inpatient, outpatient and community) and with different types of SCI (eg, traumatic vs non-traumatic SCI and complete vs incomplete), from the perspective of individuals with SCI, family caregivers and healthcare professionals. Furthermore, studies have mainly considered SCI needs from a health services perspective rather than from a patient-centred perspective that accounts for areas that influence needs outside of the health system. To our knowledge, there are no previous studies that have evaluated the variations in factors and synthesising these needs together from a patient-centred perspective. With fragmented information, it remains difficult for patients, family caregivers, health professionals and researchers to understand the current gaps in SCI care and the most efficient ways to deliver care that are most likely to address unmet needs.
The objective of this study is to review the literature on SCI needs using a scoping study approach given the diffuse literature on SCI needs. Scoping studies allow for an appraisal of the literature and have four objectives35: (A) to examine the extent, range and nature of the research activity, (B) to determine the value of conducting a systematic review, (C) to summarise and disseminate research findings and (D) to identify gaps in the literature. This methodological strategy was chosen because compared with systematic reviews, scoping studies address broader topics and questions where different study designs are used, they intend to rapidly map the key concepts of a research area and they encompass a comprehensive coverage of the literature (breadth more than in-depth). This scoping study will provide broad understanding and synthesis of SCI needs as reported by different stakeholders, for traumatic and non-traumatic SCI, from the time of rehabilitation admission to community reintegration. This scoping study will help us to identify unexplored areas of SCI needs and to provide recommendations to improve the quality of health services, to inform the development of new interventions to address unmet needs.
Theoretical frameworks to guide the evaluation of unmet needs
SCI needs will be synthesised based on two guiding theoretical frameworks: (A) the conceptual framework of Maslow’s hierarchy model of needs coming from humanistic psychology36 and the Ferrans et al’s model of health-related quality of life (HRQoL), which is a modified version of the Wilson and Cleary model of HRQoL.37 Both the Maslow’s model and the Ferrans et al’s model are informative and appropriate to frame SCI needs taking into account the perspectives of different stakeholders.
The definition of needs has been variable across published studies. Some of them define needs as the discrepancies between what is desired or optimal based on a guideline and what is actually occurring,38 a circumstance requiring a course of action39 or services that are necessary to support individual’s community living.29 For the current scoping study, a broader definition of needs corresponds to a lack of something that is essential to a person’s existence or well-being, according to Maslow’s hierarchical model.40 In his groundbreaking theory of motivation, Maslow describes human needs as being hierarchical. Figure 1 depicts the pyramidal representation of human needs. As described in his theory, human needs can be classified in five levels: (A) physiological needs, (B) safety and security needs, (C) belonging and love needs, (D) esteem needs and (E) self-actualization needs. In healthcare, the hierarchical model of needs has been applied to nursing,41 geriatric care,42 intensive care,43 palliative care,44 disability and rehabilitation45 as well as to specific conditions such as dementia,46 type 1 diabetes,47 addiction,48 homeless adults with serious mental illness49 and dissociative and conversion disorders.50 Although some of these needs cannot be provided by the health system, the use of this framework has been useful to prioritise, conceptualise and understand needs to develop a more humanistic approach to successful healthcare, to support person-centred care planning and to redefine, change and improve the culture of care.
Figure 1.
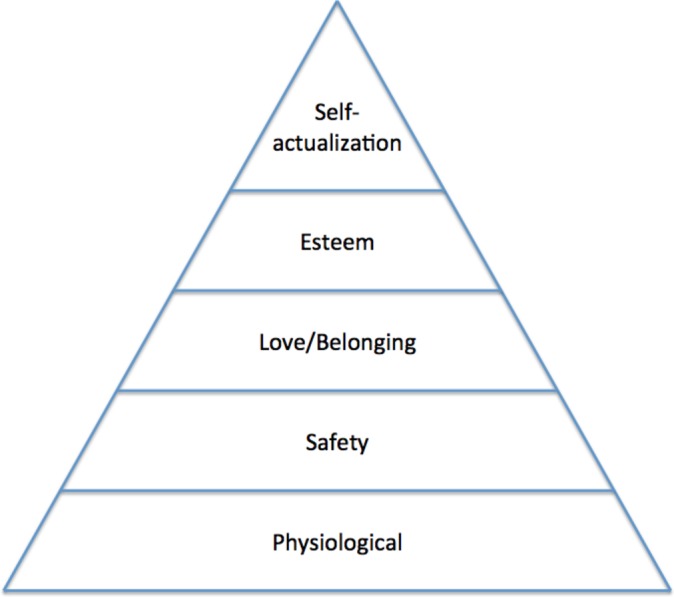
Maslow’s hierarchy model of human needs.
Given that a SCI impacts all domains of the person’s life (physical, social and psychological), needs are related to the characteristics of the individual and the environment the person lives in. Therefore, the Ferrans et al’s model of HRQoL complements Maslow’s model as it provides a guide for understanding characteristics of the individual (that are mainly encompassed in the hierarchy model of needs) and also the environmental component (eg, physical and social environment), as well as health-related domains that influence general health perceptions and quality of life (eg, symptoms, function and participation) that need to be addressed when making evidence-based recommendations regarding unmet SCI needs.51 Thus, both theoretical models will provide an understanding of the dynamics between the motivational aspects associated with SCI needs (Maslow) and the environmental influences on the HRQoL of individuals with SCI (Ferrans et al), given that unmet needs have a direct relationship with diminished quality of life.29
In summary, as studies about SCI needs are conducted in different points of the rehabilitation continuum (eg, inpatient, outpatient and community) and with different types of injuries (eg, traumatic vs non-traumatic SCI and complete vs incomplete), a scoping study approach integrating the different perspectives of healthcare professionals, family caregivers and individuals with SCI, guided by the Maslow and the Ferrans et al’s models, can help to depict a comprehensive picture of their needs. SCI needs are ongoing, and they change in the rehabilitation continuum over the years.52 In the very stressful period of the acute phase, SCI needs are not the same because both the families and individuals with SCI need time to adjust to their new reality following the injury, whereas outside the rehabilitation centre, SCI needs change depending on the path that individuals follow.53 This scoping study will help to identify research gaps regarding SCI needs from the time of rehabilitation admission to community reintegration and to holistically understand the met and unmet needs to improve healthcare with an integrative approach including different perspectives (see figure 2).
Figure 2.

Integrative approach towards SCI needs.
Methods
The current scoping study will use the methodology described by Arksey and O’Malley.35
Step 1: Identifying the research question
The research question guiding the current scoping study is ‘Which are the most frequent met and unmet needs (eg, information needs, home support needs, personal care needs, respite needs, psychological support needs, educational needs, employment needs, sexuality needs, technological needs, telerehabilitation needs, spiritual needs, among others) reported by adults with traumatic and non traumatic SCI, their family caregivers, and their rehabilitation professionals from the time of rehabilitation admission to community reintegration?’
Specifically, the current scoping study has four objectives:
To synthesise the needs of individuals with SCI as perceived by themselves, their family caregivers and their rehabilitation professionals according to the categories of the hierarchy of human needs and the Ferrans et al’s model of HRQoL.
To classify needs as met and unmet.
To explore the evolution of met/unmet needs from the time of rehabilitation admission to community reintegration.
To provide recommendations to improve SCI care.
Step 2: Identifying eligible studies
We will search published articles with the following inclusion criteria: (A) publications from all health professions, (B) describing different needs in both traumatic and non-traumatic SCI, (C) participants with 18 years of age and older, (D) from acute to chronic injuries, (E) the timeframe of publication will be limited to the last 20 years (1997–2017), (F) qualitative, quantitative studies and case reports, (G) available in English language and (H) grey literature defined as any documentary material that is non-commercially published such as technical reports, thesis’ repositories, materials produced by associations and the industry, government documents and working papers.54 We will exclude: (A) conference abstracts, (B) articles published in other languages and (C) studies addressing paediatric populations.
Search strategy and information sources
A health science librarian (JB) developed the search strategy for Ovid Medline (table 1) and had it peer reviewed by another librarian per the PRESS standard.55 As health system issues often change with models of care delivery, the economic climate, and the environment, we have decided to narrow the scope to the past 20 years (1997 to present). This search strategy will be adapted for subsequent databases. The following databases will be searched with no language limits applied: Ovid Medline, CINAHL, EMBASE, PsycINFO, Cochrane Library, Web of Science, ProQuest Dissertations and Theses. We will do hand searches of the reference lists of the selected articles to ensure that we have not missed any relevant information.
Table 1.
Search strategy for Ovid Medline in-process and other non-indexed citations, Ovid Medline daily and Ovid Medline 1997 to present
| 1 | exp Spinal Cord Injuries/ |
| 2 | spinal cord injur*.tw,kf. |
| 3 | exp Paraplegia/ |
| 4 | Quadriplegia/ |
| 5 | tetraplegia.tw,kf. |
| 6 | paraplegia.tw,kf. |
| 7 | Quadriplegia.tw,kf. |
| 8 | spinal column injur*.tw,kf. |
| 9 | central cord injur*.tw,kf. |
| 10 | 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 |
| 11 | ((met or unmet or expressed) adj3 (need or needs)).tw,kf. |
| 12 | Needs Assessment/ |
| 13 | ‘Health Services Needs and Demand’/ |
| 14 | Patient Preference/ |
| 15 | Patient Satisfaction/ |
| 16 | (sexual* adj2 (concern* or satisfaction or need or needs)).tw,kf. |
| 17 | ((caregiver* or famil* or spouse* or person* or patient* or client* or individual* or user* or research) adj3 (priorities or expectation* or preference* or perspective*)).tw,kf. |
| 18 | ((self-actualization or self-esteem or esteem or spiritual or belonging or love or physiological or security or caregiver* or famil* or spouse* or transportation or support or social or economic or health or life or telerehabilitation or rehabilitation or rehabilitative or information or economic or emotional or community or home or personal care or respite or psychological or instrumental or safety or health care or healthcare or educational or employment or leisure or housing or technological) adj3 (need or needs)).tw,kf. |
| 19 | 11 or 12 or 13 or 14 or 15 or 16 or 17 or 18 |
| 20 | self concept/ or self efficacy/ |
| 21 | (satisfaction or needs).tw,kf. |
| 22 | 20 and 21 |
| 23 | 19 or 22 |
| 24 | 10 and 23 |
| 25 | limit 24 to yr=‘1997 -Current’ |
Grey literature will be searched on SCI websites, scientific and professional associations and also using search engines on the Internet (eg, Google and Yahoo). When using search engines, we will retain the first 50 results for the analysis given the amount of information available.
Step 3: Study selection
In the first step, a reference management software (EndNote X7) will be used to merge the results and remove the duplicates before screening the abstracts. Later, a data extraction form will be developed by the research team to screen the abstracts based on the eligibility criteria described in step 2. Two independent reviewers will conduct the selection of abstracts starting with a pilot phase involving the examination of the first 20 titles and abstracts to screen and decide the retention of the abstract based on the inclusion criteria. The results of the independent ratings will be recorded separately using the data extraction form. Inter-rater agreement will be assessed using the kappa statistic.56 Inter-rater agreement below 75% will lead to a revision and clarification of the eligibility criteria. The process will be repeated until an agreement of 75% is reached, which is evidence of excellent agreement. This is important as it is recommended that discussions are being held regarding the challenges and uncertainties related to study selection and to refine the search strategy as needed.57 Finally, all eligible studies and those classified as unclear (ie, requiring further information to make a final decision regarding their retention) will be independently reviewed as full-text articles. Inter-rater agreement will be reassessed using the kappa statistic56 on a random sample of 10 publications. Disagreements at this stage will be resolved by consensus. In case of persistent disagreement, a third reviewer will be consulted to determine the final inclusion.
Step 4: Data extraction process
The data extracted in the previous step will include the information corresponding to author(s), year of publication, country of origin and context (where the study was conducted), status of publication (eg, published or grey literature), journal, aims/purpose, study population (individuals with SCI, family caregivers, rehabilitation professionals) and sample size (if applicable), SCI type (traumatic and non-traumatic), level(s) of care (acute, primary care and community), time since SCI, methodology/methods (study design and measures) and key findings that relate to the scoping study question/s (in terms of met and unmet specific categories of needs). When available, the time for community reintegration will be included and reported in years. At this stage, two independent reviewers will extract the information based on the first 10 publications. Also, during the charting of the information, the reviewers will meet following the extraction of the first 10 studies to make sure that the data extraction follows consistently the purpose of the study. A meeting to evaluate the consistency of the information extracted will allow the reviewers to identify inconsistencies and make decisions regarding the best way to deal with ambiguity.
An iterative process consisting of inter-reviewer discussions held at the beginning, in the middle and at the end of the extraction will lead to a consensus regarding the best way to extract the data. When disagreements persist, a third independent reviewer will be consulted.
Step 5: Data synthesis
This phase involves collating, summarising and reporting the results. Compared with systematic reviews, scoping studies present a narrative account of a potentially large body of material.35 Thus, guided by the previous theoretical frameworks, we intend to identify a descriptive numerical summary (eg, characteristics of included studies, types of study design, characteristics of the study population and geographical location) and emerging themes (deductive thematic analysis).57 Using as an analytical framework, the Maslow’s hierarchical model of human needs, we will extract the main themes corresponding to the five categories of human needs and classify them as described by professionals, family caregivers and individuals with SCI. Similarly, met and unmet SCI needs will be classified based on the Ferrans et al’s model of HRQoL as characteristics of the individual and characteristics of the environment and their relationship with other components (eg, biological function, symptoms, functional status, general health perceptions and overall quality of life). We will create a matrix that integrates the themes identified for the Maslow’s and Ferrans et al’s model that will allow us to explore the relationship between personal and environmental factors (Ferrans et al’s model) that influence needs (Maslow model). The matrix will allow the identification and intergroup comparison of the met/unmet needs for each one of the groups (eg, adults with traumatic and non-traumatic SCI, their family caregivers and their rehabilitation professionals). Following the thematic analysis, special considerations regarding the implications for research, policy and practice will be presented. Thus, the analysis will include both individual and environmental influences of quality of life because SCI needs can be unmet at different points of the continuum of care as a consequence of subjective (eg, motivation, believes and attitudes) and environmental barriers (eg, administrative issues, financial limitations, limitations of health policies, among others).
Step 6: Stakeholder consultation
The objective of this stage is to start translating knowledge into practice by disseminating results among potential knowledge users. Given the extensive information that will be synthesised and the diverse perspectives involved, we will request input from stakeholders at each step and for each document/process that is developed for data extraction and synthesis. Therefore, stakeholder consultations will be held at the beginning of the process (requesting feedback to refine the research question, further refine the Ferrans et al’s model relative to Maslow’s model to focus data extraction and synthesis), during the study (validate the data extraction and decide the best way to align the information with stakeholders’ needs), two to three times during data synthesis and when preliminary or final results are available (knowledge mobilisation). Having information about SCI met and unmet needs will help stakeholders to prioritise different needs, based on the conclusions of the scoping review. Thus, stakeholders will benefit from the results and will be able to focus their efforts based on informed decisions about the different SCI needs. The current scoping review will permit to write an integrated master report combining the needs of individuals with SCI from the perspectives of different stakeholders from the time of rehabilitation admission to community reintegration. However, our knowledge translation plan will include extracting end-user specific information from the master report for each targeted group (ie, adults with traumatic and non-traumatic SCI, their family caregivers and their rehabilitation professionals). For the current scoping study, relevant stakeholders include support groups of individuals with SCI and their family caregivers, clinicians and decision makers. The meetings will be organised either in a face-to-face format or using videoconference to allow broader participation, giving equal representation to the different groups.
Discussion
The current scoping study will answer the question about the most frequent met and unmet needs reported by adults with traumatic and non-traumatic SCI, their family caregivers and their rehabilitation professionals from the time of rehabilitation admission to community reintegration. The results of the current scoping study could have implications from different viewpoints: (A) rehabilitation can be informed from the synthesis of SCI needs because clinicians can become more sensitive as they increase awareness about the complexity of SCI expressed and unmet needs from the time of rehabilitation admission to community reintegration, (B) service provision could be modified from gaining understanding about the gap between unmet and expressed needs, (C) the view of rehabilitation as a changing process with evolving needs in different phases of care can help clinicians to understand and modify their practice when considering SCI needs as dynamic in different stages of care, (D) the conception of new studies can be informed based on our comprehensive picture of SCI needs as it will suggest priorities in the research agenda, (E) the development of new interventions could benefit from our conclusions as they will provide information to help to make informed decisions to address the most important unmet needs as outcomes and (F) policy makers could benefit from these results as they will be able to implement modifications to existent programmes to adjust to the complexities of the interactions among different stakeholders involved in the provision of services to increase SCI needs satisfaction.
Scoping studies have some methodological limitations that include the fact that the quality of the evidence is not appraised. Compared with systematic reviews where the quality appraisal and the relative weight of evidence in favour or against a specific intervention is very important, scoping studies are descriptive and narrative.35 However, scoping studies provide valid specific research questions needing a systematic review through a careful process of scrutinising evidence coming from different methodologies and study designs. Also, scoping studies are not a short summary of many articles and, as such, they use frameworks or themes to articulate their findings.57 For the current scoping study, the theoretical frameworks guiding the analysis of the information have been carefully chosen and weighted against other competing models. However, we are aware that the findings could be interpreted using alternative analytical frameworks.
A few limitations regarding the search strategy need to be acknowledged. The search strategy includes the use of different keywords to address needs, SCI and the three groups of stakeholders that we would like to target (eg, individuals with SCI, their family caregivers and their rehabilitation professionals). However, even when we have clearly widened the keywords, it is possible that alterative terms could make that some of the peer-reviewed literature could not be captured. To overcome this limitation, we have the support of an experienced librarian in health sciences; iterative discussions led to the refinement of the search strategy to avoid missing important pieces of information that could be vital to respond to the research question. At the same time, the search strategy has been keenly refined to avoid having an unmanageable number of references. In addition, scoping studies involve practical issues related to time, funding and access to resources that must be considered when finding the balance between feasibility, breadth and comprehensiveness.57
Issues associated with the resource implications represent the fact that even if scoping studies provide a rapid appraisal and mapping of a specific field, it is wrong to assume that they are a quick or cheap option, with some cases reporting the full-time involvement of at least three staff members and the librarian for six consecutive months, with the study protocol as the starting point.35 Thus, these studies involve costs regarding the staff involved, the informatics resources needed and the time demanded in the selection of the studies by staff with the scientific qualifications required to critically select the information and optimally chart the data. For the current scoping study, the experience of our lab in this kind of studies, as well as the scientific qualifications of our staff (eg, healthcare professionals, graduate students, postdoctoral fellows and researchers), make it feasible considering the high levels of analytic skills needed.
In conclusion, this study protocol presents the rationale and methodology for a scoping study on SCI needs. Through a rigorous and transparent method, engaging individuals with SCI, family caregivers and health professionals at each step, it will provide a framework to understand the most frequent met and unmet needs as reported by adults with traumatic and non-traumatic SCI, their family caregivers and their rehabilitation professionals from the time of rehabilitation admission to community reintegration.
Ethics and dissemination
As a scoping study is an analysis of published materials, it does not require REB approval. However, for the consultation phase, the plan will be submitted for ethics approval and participants’ informed consent will be required at this stage. The dissemination of the results of the scoping study will include multiple steps. First, after the consultation meetings, an integrated master report will be available. The report will combine the needs of individuals with SCI from the perspectives of different stakeholders from the time of rehabilitation admission to community reintegration. Second, we will extract end-user specific information from the master report to be used as a knowledge translation strategy. That is, for each group of stakeholders targeted in the review, there will be specific recommendations to be communicated. For the current scoping study, relevant stakeholders include support groups of individuals with SCI and their family caregivers, clinicians and decision makers. The recommendations will be transmitted through meetings. Formats for those meetings include either a face to face or videoconferences to allow broader participation, giving equal representation to the different groups.
Supplementary Material
Footnotes
Contributors: AM: conception and design, preliminary literature review, drafting of the manuscript, integrations of the edits in the different versions and manuscript submission; DZ: edits and feedback; CR: edits and feedback; JB: MLIS, AHIP database search; SA: conception and design, edits and feedback.
Funding: This paper is part of the Lindsay foundation funded reserach program, Initiativesfor the Development of New Technologies and Innovative Practices in Rehabilitation (INSPIRE). Fonds de la recherche du Québec-Santé (FRQS). Networks of Centres of Excellence of Canada (AGE-WELL NCE).
Competing interests: None declared.
Patient consent: N/A.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: N/A.
References
- 1. Government of Canada, Public Health Agency of Canada. Mapping connections: an understanding of neurological conditions in Canada, 2014. [Google Scholar]
- 2. Lenehan B, Street J, Kwon BK, et al. . The epidemiology of traumatic spinal cord injury in British Columbia, Canada. Spine 2012;37:321–9. 10.1097/BRS.0b013e31822e5ff8 [DOI] [PubMed] [Google Scholar]
- 3. Noonan VK, Fingas M, Farry A, et al. . Incidence and prevalence of spinal cord injury in Canada: a national perspective. Neuroepidemiology 2012;38:219–26. 10.1159/000336014 [DOI] [PubMed] [Google Scholar]
- 4. Munce SE, Wodchis WP, Guilcher SJ, et al. . Direct costs of adult traumatic spinal cord injury in Ontario. Spinal Cord 2013;51:64–9. 10.1038/sc.2012.81 [DOI] [PubMed] [Google Scholar]
- 5. Chen HY, Boore JR. Living with a relative who has a spinal cord injury: a grounded theory approach. J Clin Nurs 2009;18:174–82. 10.1111/j.1365-2702.2008.02355.x [DOI] [PubMed] [Google Scholar]
- 6. Hou S, Rabchevsky AG. Autonomic consequences of spinal cord injury. Compr Physiol 2014;4:1419–53. 10.1002/cphy.c130045 [DOI] [PubMed] [Google Scholar]
- 7. Guilcher SJ, Craven BC, Lemieux-Charles L, et al. . Secondary health conditions and spinal cord injury: an uphill battle in the journey of care. Disabil Rehabil 2013;35:894–906. 10.3109/09638288.2012.721048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Craig A, Nicholson Perry K, Guest R, et al. . Prospective study of the occurrence of psychological disorders and comorbidities after spinal cord injury. Arch Phys Med Rehabil 2015;96:1426–34. 10.1016/j.apmr.2015.02.027 [DOI] [PubMed] [Google Scholar]
- 9. Khazaeipour Z, Taheri-Otaghsara SM, Naghdi M. Depression following spinal cord Injury: its relationship to demographic and socioeconomic Indicators. Top Spinal Cord Inj Rehabil 2015;21:149–55. 10.1310/sci2102-149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Williams R, Murray A. Prevalence of depression after spinal cord injury: a meta-analysis. Arch Phys Med Rehabil 2015;96:133–40. 10.1016/j.apmr.2014.08.016 [DOI] [PubMed] [Google Scholar]
- 11. Lidal IB, Hjeltnes N, Røislien J, et al. . Employment of persons with spinal cord lesions injured more than 20 years ago. Disabil Rehabil 2009;31:2174–84. 10.3109/09638280902946952 [DOI] [PubMed] [Google Scholar]
- 12. Lidal IB, Huynh TK, Biering-Sørensen F. Return to work following spinal cord injury: a review. Disabil Rehabil 2007;29:1341–75. 10.1080/09638280701320839 [DOI] [PubMed] [Google Scholar]
- 13. Craven C, Verrier M, Balioussis C, et al. . Rehabilitation environmental scan atlas: capturing capacity in canadian SCI rehabilitation. Vancouver: Rick Hansen Institute, 2012. [Google Scholar]
- 14. Dickson A, O’Brien G, Ward R, et al. . The impact of assuming the primary caregiver role following traumatic spinal cord injury: an interpretative phenomenological analysis of the spouse’s experience. Psychol Health 2010;25:1101–20. 10.1080/08870440903038949 [DOI] [PubMed] [Google Scholar]
- 15. Chiu S. Using triangulation methodology study on role strain and demands of family caregivers for spinal cord injury patients during discharge transition. Nursing Research 1998;6:513–25. [Google Scholar]
- 16. Middleton JW, Simpson GK, De Wolf A, et al. . Psychological distress, quality of life, and burden in caregivers during community reintegration after spinal cord injury. Arch Phys Med Rehabil 2014;95:1312–9. 10.1016/j.apmr.2014.03.017 [DOI] [PubMed] [Google Scholar]
- 17. Nogueira PC, Rabeh SA, Caliri MH, et al. . [Caregivers of individuals with spinal cord injury: caregiver burden]. Rev Esc Enferm USP 2013;47:607–14. [DOI] [PubMed] [Google Scholar]
- 18. Raj JT, Manigandan C, Jacob KS. Leisure satisfaction and psychiatric morbidity among informal carers of people with spinal cord injury. Spinal Cord 2006;44:676–9. 10.1038/sj.sc.3101899 [DOI] [PubMed] [Google Scholar]
- 19. Ellenbogen PS, Meade MA, Jackson M, et al. . The impact of spinal cord injury on the employment of family caregivers. J Vocat Rehabil 2006;25:35–44. [Google Scholar]
- 20. Dickson A, O’Brien G, Ward R, et al. . Adjustment and coping in spousal caregivers following a traumatic spinal cord injury: an interpretative phenomenological analysis. J Health Psychol 2012;17:247–57. 10.1177/1359105311411115 [DOI] [PubMed] [Google Scholar]
- 21. Glass CA, Krishnan KR, Bingley JD. Spinal injury rehabilitation: do staff and patients agree on what they are talking about? Paraplegia 1991;29:343–9. 10.1038/sc.1991.49 [DOI] [PubMed] [Google Scholar]
- 22. Kroll T. Rehabilitative needs of individuals with spinal cord injury resulting from gun violence: the perspective of nursing and rehabilitation professionals. Appl Nurs Res 2008;21:45–9. 10.1016/j.apnr.2006.06.001 [DOI] [PubMed] [Google Scholar]
- 23. Trezzini B, Phillips B. Impact of legal regulations and administrative policies on persons with SCI: identifying potential research priorities through expert interviews. Disabil Rehabil 2014;36:1883–91. 10.3109/09638288.2014.881564 [DOI] [PubMed] [Google Scholar]
- 24. Harvey LA, Adams R, Chu J, et al. . A comparison of patients’ and physiotherapists’ expectations about walking post spinal cord injury: a longitudinal cohort study. Spinal Cord 2012;50:548–52. 10.1038/sc.2012.1 [DOI] [PubMed] [Google Scholar]
- 25. Whalley Hammell K. Experience of rehabilitation following spinal cord injury: a meta-synthesis of qualitative findings. Spinal Cord 2007;45:260–74. 10.1038/sj.sc.3102034 [DOI] [PubMed] [Google Scholar]
- 26. LaVela SL, Landers K, Etingen B, et al. . Factors related to caregiving for individuals with spinal cord injury compared to caregiving for individuals with other neurologic conditions. J Spinal Cord Med 2015;38:505–14. 10.1179/2045772314Y.0000000240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Smith EM, Boucher N, Miller WC. Caregiving services in spinal cord injury: a systematic review of the literature. Spinal Cord 2016;54:562–9. 10.1038/sc.2016.8 [DOI] [PubMed] [Google Scholar]
- 28. Stiens SA, Fawber HL, Yuhas SA. The person with a spinal cord injury: an evolving prototype for life care planning. Phys Med Rehabil Clin N Am 2013;24:419–44. 10.1016/j.pmr.2013.03.006 [DOI] [PubMed] [Google Scholar]
- 29. Sweet SN, Noreau L, Leblond J, et al. . Understanding quality of life in adults with Spinal Cord Injury Via SCI-related needs and secondary complications. Top Spinal Cord Inj Rehabil 2014;20:321–8. 10.1310/sci2004-321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Beauregard L, Guindon A, Noreau L, et al. . Community needs of people living with spinal cord injury and their family. Top Spinal Cord Inj Rehabil 2012;18:122–5. 10.1310/sci1802-122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. van Loo MA, Post MW, Bloemen JH, et al. . Care needs of persons with long-term spinal cord injury living at home in the Netherlands. Spinal Cord 2010;48:423–8. 10.1038/sc.2009.142 [DOI] [PubMed] [Google Scholar]
- 32. Noreau L, Noonan VK, Cobb J, et al. . Spinal cord injury community survey: a national, comprehensive study to portray the lives of canadians with spinal cord injury. Top Spinal Cord Inj Rehabil 2014;20:249–64. 10.1310/sci2004-249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Meade MA, Taylor LA, Kreutzer JS, et al. . A preliminary study of acute family needs after spinal cord Injury: analysis and implications. Rehabil Psychol 2004;49:150–5. 10.1037/0090-5550.49.2.150 [DOI] [Google Scholar]
- 34. New PW. A multidisciplinary consultation team to address the unmet needs of hospitalized patients with spinal cord injury. Arch Neurol 2010;67:1074–6. 10.1001/archneurol.2010.204 [DOI] [PubMed] [Google Scholar]
- 35. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 36. Maslow AH, Frager R, Fadiman J. Motivation and personality. 3rd ed New York: Harper & Row, 1987. [Google Scholar]
- 37. Ferrans CE, Zerwic JJ, Wilbur JE, et al. . Conceptual model of health-related quality of life. J Nurs Scholarsh 2005;37:336–42. 10.1111/j.1547-5069.2005.00058.x [DOI] [PubMed] [Google Scholar]
- 38. Schubart JR, Hilgart M, Lyder C. Pressure ulcer prevention and management in spinal cord-injured adults: analysis of educational needs. Adv Skin Wound Care 2008;21:322–9. 10.1097/01.ASW.0000323521.93058.47 [DOI] [PubMed] [Google Scholar]
- 39. Kennedy P, Lude P, Taylor N, life Qof. Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord 2006;44:95–105. 10.1038/sj.sc.3101787 [DOI] [PubMed] [Google Scholar]
- 40. Taormina RJ, Gao JH. Maslow and the motivation hierarchy: measuring satisfaction of the needs. Am J Psychol 2013;126:155–77. 10.5406/amerjpsyc.126.2.0155 [DOI] [PubMed] [Google Scholar]
- 41. Minshull J, Ross K, Turner J. The human needs model of nursing. J Adv Nurs 1986;11:643–9. 10.1111/j.1365-2648.1986.tb03381.x [DOI] [PubMed] [Google Scholar]
- 42. Majercsik E. Hierachy of needs of geriatric patients. Gerontology 2005;51:170–3. 10.1159/000083989 [DOI] [PubMed] [Google Scholar]
- 43. Jackson JC, Santoro MJ, Ely TM, et al. . Improving patient care through the prism of psychology: application of Maslow’s hierarchy to sedation, delirium, and early mobility in the intensive care unit. J Crit Care 2014;29:438–44. 10.1016/j.jcrc.2014.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Zalenski RJ, Raspa R. Maslow’s hierarchy of needs: a framework for achieving human potential in hospice. J Palliat Med 2006;9:1120–7. 10.1089/jpm.2006.9.1120 [DOI] [PubMed] [Google Scholar]
- 45. Calabro LE. "First things first": Maslow’s hierarchy as a framework for rebt in promoting disability adjustment during rehabilitation. J Ration Emot Cogn Behav Ther 1997;15:193–213. 10.1023/A:1025039816806 [DOI] [Google Scholar]
- 46. Scholzel-Dorenbos CJ, Meeuwsen EJ, Olde Rikkert MG. Integrating unmet needs into dementia health-related quality of life research and care: introduction of the hierarchy model of needs in dementia. Aging Ment Health 2010;14:113–9. 10.1080/13607860903046495 [DOI] [PubMed] [Google Scholar]
- 47. Beran D. Developing a hierarchy of needs for type 1 diabetes. Diabet Med 2014;31:61–7. 10.1111/dme.12284 [DOI] [PubMed] [Google Scholar]
- 48. Best D, Day E, McCarthy T, et al. . The Hierarchy of needs and care planning in addiction services: what maslow can tell us about addressing competing priorities? Addict Res Theory 2008;16:305–7. 10.1080/16066350701875185 [DOI] [Google Scholar]
- 49. Henwood BF, Derejko KS, Couture J, et al. . Maslow and mental health recovery: a comparative study of homeless programs for adults with serious mental illness. Adm Policy Ment Health 2015;42:220–8. 10.1007/s10488-014-0542-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ishikura R, Tashiro N. Frustration and fulfillment of needs in dissociative and conversion disorders. Psychiatry Clin Neurosci 2002;56:381–90. 10.1046/j.1440-1819.2002.01026.x [DOI] [PubMed] [Google Scholar]
- 51. Bakas T, McLennon SM, Carpenter JS, et al. . Systematic review of health-related quality of life models. Health Qual Life Outcomes 2012;10:134 10.1186/1477-7525-10-134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Manns PJ, May LA. Perceptions of issues associated with the maintenance and improvement of long-term health in people with SCI. Spinal Cord 2007;45:411–9. 10.1038/sj.sc.3101973 [DOI] [PubMed] [Google Scholar]
- 53. Conti A, Garrino L, Montanari P, et al. . Informal caregivers’ needs on discharge from the spinal cord unit: analysis of perceptions and lived experiences. Disabil Rehabil 2016;38:159–67. 10.3109/09638288.2015.1031287 [DOI] [PubMed] [Google Scholar]
- 54. Farace DJ, Schöpfel J. Grey literature in library and information studies. Berlin; New York: De Gruyter Saur, 2010. [Google Scholar]
- 55. McGowan J, Sampson M, Salzwedel DM, et al. . PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol 2016;75:40–6. 10.1016/j.jclinepi.2016.01.021 [DOI] [PubMed] [Google Scholar]
- 56. Higgins J, Green S, Cochrane handbook for systematic reviews of interventions Version 5.1.0. The Cochrane Collaboration, 2011. [Google Scholar]
- 57. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


