Abstract
Objective
Across healthcare systems, there is consensus on the need for independent and impartial assessment of performance. There is less agreement about how measurement and reporting performance improves healthcare. This paper draws on academic theories to develop a conceptual framework—one that classifies in an integrated manner the ways in which change can be leveraged by healthcare performance information.
Methods
A synthesis of published frameworks.
Results
The framework identifies eight levers for change enabled by performance information, spanning internal and external drivers, and emergent and planned processes: (1) cognitive levers provide awareness and understanding; (2) mimetic levers inform about the performance of others to encourage emulation; (3) supportive levers provide facilitation, implementation tools or models of care to actively support change; (4) formative levers develop capabilities and skills through teaching, mentoring and feedback; (5) normative levers set performance against guidelines, standards, certification and accreditation processes; (6) coercive levers use policies, regulations incentives and disincentives to force change; (7) structural levers modify the physical environment or professional cultures and routines; (8) competitive levers attract patients or funders.
Conclusion
This framework highlights how performance measurement and reporting can contribute to eight different levers for change. It provides guidance into how to align performance measurement and reporting into quality improvement programme.
Keywords: quality improvement, performance measurement, healthcare system change, conceptual framework
Strengths and limitations of this study.
One strength of this conceptualisation is that it draws on academic theories and integrates various streams of thinking.
The paper draws on a range of theoretical work to describe different types of organisational change and various facilitators and barriers to such change and synthesises levers into a straightforward typology.
The framework provides insights and guidance into how performance information can be used in healthcare systems to leverage change.
The model development is based on the synthesis of published literature and available grey literature—and so could be affected by any publication bias where levers that did not work in a particular context may not have featured in the retrieved publications.
The literature was reviewed using a layered approach, selecting seminal papers and reports through a iterative approach, and did not consist of a systematic review.
Introduction
That performance measurement is essential in healthcare systems is broadly accepted.1–3 Measurement and reporting performance plays a clear role in terms of management and in providing accountability, and also in terms of making a contribution to improvement efforts. When properly defined, applied and interpreted, performance measures provide insights into absolute and relative achievement of outcomes, patterns of delivery and efficiency of care, and highlight variation and areas where there are opportunities to improve.4
Performance however relates to real processes, actions and outcomes rather than to the structural, potential or planned delivery of services. Just as actors perform on stage and athletes perform on the field, surgeons perform in surgical theatres and nurses perform at the bedside or in community centres. Measuring performance in healthcare is therefore about quantifying what healthcare systems, organisations and professionals are really achieving rather than about how well they are designed or qualified. Meaningful performance measurement focuses on aspects such as services delivered relative to patient needs and expectations, processes and models of care relative to evidence and clinical workloads, and patient outcomes relative to their presenting problems and the resources invested.
Some studies have shown that the impact of performance measurement and reporting varies,5 and that they can have unintended consequences that result in deterioration of performance.6 However, the weight of accumulating evidence attests to the potential benefits and power of performance reporting, particularly in terms of securing change among clinicians and delivery organisations.7–9 This evidence suggests that performance measurement makes a contribution to improvement efforts but is not always sufficient to achieve, on its own, meaningful change in healthcare.7 10
Quality improvement efforts draw on a much broader array of activities than simply providing information about the performance of providers, organisations or systems.10–15 Change in complex systems is shaped by a range of factors including history, culture, social and legal context, policies and structures, availability of evidence, technology and economic incentives. Researchers from many different disciplines have investigated how such factors influence change processes and have described different ways in which change can be initiated, driven and managed both within16 17 and outside18–20 the healthcare sector.
While recent research has assessed the impact of performance measurement and reporting on various aspects, most studies seem to assume that public reporting of performance information either works on its own or only through patients’ choice of providers. To date, no integrative framework that conceptualises the role of performance information and the way in which this information interacts with, and facilitates different levers that support healthcare system change, has been developed. This paper presents a typology and proposes an integrated conceptual framework of levers for change in healthcare systems and discusses the ways in which health performance measurement and reporting can act on these levers to promote change and quality improvement.
Methods
The literature relevant to a review of the role of performance measurement in behavioural and organisational change is vast and unwieldy. Behaviour and organisational change literature has roots in substantial knowledge bases that span sociology, psychology, organisation sciences, health policy, management and economics. The breadth of the available literature overwhelms efforts to systematically synthesise it. Despite the huge number of studies and publications, well-delineated conceptual models that proffer typologies of levers for change are relatively rare. This means that there is simultaneously too much and too little literature. In order to overcome this dilemma, a layered inquiry was undertaken and the paper is underpinned by a targeted search strategy rather than the more usual systematic review.
The purpose of this paper is not to review all papers published but rather to canvass and classify the main levers for change in use in healthcare, with a particular focus on levers that rely on performance information. As a result, the paper draws on a mix of theoretical expositions, prescriptive models of change and descriptive accounts or typologies of the utilisation of performance information in pursuit of change.21–24
The starting point was a collection of seminal works by renowned experts in performance measurement. A snowballing approach was then adopted to explore references cited in their work and to review their theoretical underpinnings. In addition, key databases were searched CINAHL, Cochrane Effective Practice, MEDLINE, ProQuest, PsycInfo, PubMed and Web of Science databases for papers using the keywords: ‘behaviour change’, ‘behavioural interventions’, ‘health behaviour’, ‘levers for change’, ‘organisational change’, ‘performance indicators’, ‘performance measurement’, ‘performance reporting’, ‘quality improvement’, ‘quality measurement’ and ‘theories of behaviour change’. Publications were screened according to whether they outlined a conceptual framework or defined different types of approaches used to secure improvement in healthcare organisations and systems. Authors independently reviewed the frameworks and typologies, clustering conceptually similar levers for change. Any mismatch in clustering was resolved through discussion.
Furthermore, the typology and conceptual framework developed by this paper is informed by the authors’ experience in measurement and change in healthcare systems, particularly in Australia, Canada and the UK. The authors combined their assessment and iteratively synthesised the dimensions useful to organise levers into a coherent framework. The resulting framework was then mapped to the original studies to assess integrity and comprehensiveness of the integrated framework. Online supplementary appendix 1 summarises the main published work selected to build an integrated framework of levers for change.
bmjopen-2016-014825supp001.pdf (204.5KB, pdf)
Results
Theoretical foundation
Several levers for change are grounded in institutional theory which suggests that normative, coercive and mimetic pressures drive conformity among organisations through processes of comparing, compelling and copying.21 Similarly, studies on the diffusion of innovation have highlighted the roles that evidence, social context, perceptions about existing practice, organisational structures and norms, as well as attitudes and values play in promoting adoption of an innovation.22 23
Other levers are grounded in theories of behaviour change which focus on explaining, predicting and changing individual behaviour.24 These theories propose that change is influenced by factors that include attitudes, perceptions and motivation to comply with norms, as well as the perception of control over the behaviour.25 In a similar line, sociological theories identify factors that influence behaviour change such as intrinsic and extrinsic motivators, perceptions of fear or threat as well as norms, attitudes and intentions.
Two clear organising dimensions emerge. The first dimension (from psychology and sociology literature) focuses on why change occurs, and is based on the distinction between intrinsic and extrinsic motivation.26–28 Intrinsic motivation is grounded in self-awareness, self-reflection or tailored and specific feedback about performance—with subsequent catalysis of action or response. Data and information relevant to and reflective of the unit’s performance can result in a readiness for change.29 Extrinsic motivation, on the other hand, involves professionals, organisations and systems responding to directives, policies and economic or structural forces emanating from outside their direct control.
The second organising dimension (from innovation and organisational change literature) is based on the distinction between planned and emergent change.30–32 Planned change is the result of a deliberate effort, conscious reasoning and considered actions, and typically involves sequential steps enacted with the intention of changing the behaviours of individuals and organisations to secure improvement.33–36 Emergent change unfolds in a reactive or spontaneous way.37 It is iterative and develops as people adapt to the circumstances, constraints and requirements of their environment and seek to improve some aspect of performance.38
An integrated framework
When the previously described two dimensions are considered together, a matrix consisting of four quadrants is formed. Each quadrant represents a different way in which change occurs. Our review of the literature further suggests that each quadrant contains two different levers for change—resulting in a typology of eight levers in total (figure 1).
Figure 1.
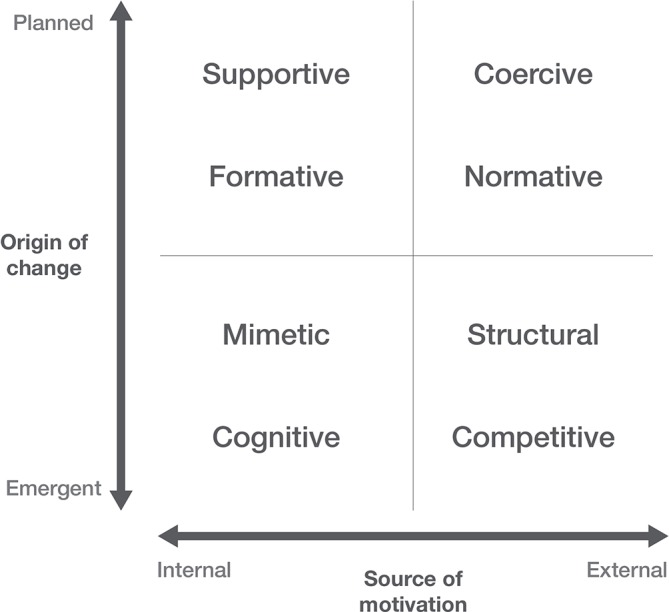
Integrated conceptual framework of levers for change in healthcare.
In the bottom left quadrant of the model are levers that seek to secure emergent and internally motivated change.
Cognitive levers,4 39 40 such as the provision of information through report cards, league tables and root cause analysis summaries, provide a means to gauge one’s own performance. They codify performance, quantifying it so that achievements are discernible and temporal trends can be tracked. In healthcare, this lever aims to improve clinicians’ and managers’ awareness of gaps. It is recognised as the starting point of many types of quality improvement processes.
Mimetic levers,4 15 21 39–43 such as the provision of benchmarking data that identifies best performers and their adopted models of care, set performance in a wider context, revealing the performance of peers. Mimetic levers act on a desire to belong, to conform to a respected group, to outperform—or at the very least, not be roundly outperformed by—peers. The role of data in mimetic levers is to enable comparisons and identify clearly who is performing well and who is not performing well. In the healthcare sector, public reporting of hospital or clinical units’ performance on a nominal basis can act on the desires of clinicians or organisations to emulate the activities and processes implemented in high-performance units.
In the top left quadrant of the model, where change is planned and internally motivated, levers rely heavily on evidence and knowledge about best practice. Variation in performance can be due to differences in knowledge, capabilities and competencies.
Formative levers,4 10 15 41–44 such as continuing professional education and development programmes and healthcare redesign courses, are based on the provision of feedback—often in a timely way, guiding change in dynamic situations. While often used in circumstances where change is deliberate and an evidence-based goal or model of best practice is clearly articulated, formative levers are flexible and responsive in terms of data provision. The role of data in formative levers is to clearly capture salient elements of the change process, guide action and signal when there is a need to respond to changing circumstances or unanticipated developments.
Supportive levers,4 10 15 43 44 such as quality improvement programmes and clinical collaboratives, enable, encourage and help change. They provide mentorship, guidance and facilitate learning. Data are used to inform where efforts should focus and guide change processes and investments.
In the top right quadrant, where change is planned and externally motivated, levers rely heavily on power and influence. Performance data are used primarily for monitoring or quality assurance purposes, ensuring minimum standards.
Coercive levers,4 15 21 39 40 43–45 such as pay for performance programme or regulatory or legal frameworks, are based on organisational power and often feature targets and powerful incentives and sanctions that drive change. Often referred to as ‘carrots and sticks’, coercive levers are favoured in circumstances where there is a powerful policy or strategic imperative. Goals are set, milestones defined and levers are used to ensure that objectives are achieved—often within a defined timeframe. Coercive levers may appear effective but on careful assessment be shown to result in unanticipated consequences. Key performance indicators and performance monitoring frameworks are clear example of how data are used to support coercive levers.
Normative levers,4 21 39–42 45 such as memberships of medical associations and organisations that define the state of current best practice, are based on professional standards and well-defined norms of acceptable performance. They are often enacted through licensing, registration, revalidation and accreditation processes acting as key motivators for change. The role of data is to target where the levers should be applied and to monitor anticipated and unanticipated effects.
In the bottom right quadrant, where change is emergent and externally driven—levers are primarily impersonal, relying neither on negotiation, counselling or cajoling.
Structural levers41 42 are based on organisational constraints such as staffing, defined roles and responsibilities or characteristics that contain and shape performance. They can include physical limits or barriers (eg, architectural design of clinical space, information and communication technologies) and also organisational processes and professional routines that channel professional and organisational behaviours (eg, clinical pathways, team-based processes, models of care). While the role of data is traditionally less prominent in supporting structural levers, it informs the placement of levers and monitoring their impact.
Competitive levers,10 15 39 40 43–45 such as the pressures imposed by the need to attract clients or contracts, rely on market forces that shape professional and organisation behaviour to attract or retain clients and funding. Performance data are often seen as playing a role in competitive levers through supporting patients’ choices and managers’ commissioning decisions. Ultimately, competitive levers work through fear of losing market share or clients, or through incentivising greater market share or increased client bases or service users. Commissioning and processes supporting patients’ selection of providers are examples of competitive levers in healthcare.
Discussion
A comprehensive and coherent framework of levers for change
The framework described in this paper provides a way to navigate the multitude of approaches available to secure change. It does so in two complementary ways. First, from a deductive perspective, it draws on a range of theoretical sources to describe different types of organisational change and various facilitators and barriers to such change. Second, from an inductive perspective, it brings together and describes levers previously described in the literature and by healthcare organisations internationally, synthesising and summarising them into a straightforward typology. The model provides a way to categorise levers, to inform decisions about the judicious application and use of levers both in isolation and in combination, to define information requirements and to set expectations about potential effects. Table 1 presents the eight levers and relates them to key publications retrieved through the literature review. While various existing models have touched on different aspects or levers, this framework integrates their perspectives.
Table 1.
Mapping of published frameworks and levers for change
| Cognitive | Mimetic | Formative | Supportive | Normative | Coercive | Structural | Competitive | Number of levers | |
| DiMaggio and Powell21 | * | * | * | 3 | |||||
| Plsek and Greenhalgh41 | * | * | * | * | * | * | * | 7 | |
| Institute of Medicine39 | * | * | * | * | 4 | ||||
| Leatherman40 | * | * | * | * | * | * | 6 | ||
| Naylor, Iron and Handa44 | * | * | * | * | * | * | * | * | 8 |
| Berwick, James and Coye10 | * | * | * | * | 4 | ||||
| Leatherman and Sutherland45 | * | * | * | * | 4 | ||||
| Boland and Fowler4 | * | * | * | * | * | * | 6 | ||
| NHS Quality Board/Health Foundation15 43 | * | * | * | * | * | * | 6 | ||
| Bevan46 | * | * | * | * | * | * | 6 | ||
| Number of frameworks | 8 | 5 | 7 | 7 | 8 | 9 | 3 | 8 |
The framework provides insights and guidance into how performance information can be used in healthcare systems to leverage change. The distinction between planned and emergent change is key. Routine release of information can guide planned efforts to improve and provide formative feedback according to agreed regular schedules. However, routine reporting can also lose salience if too many measures or too frequent reporting generates indicator chaos or fatigue. Performance measurement and reporting, if used only in the context of planned change, acts more as a monitoring tool (providing reassurance or accountability) rather than as a catalyst or lever for change. If meaningful change at an organisational or provider level is an objective, the framework highlights that performance measurement is more powerful if also applied in efforts to promote emergent change—capitalising on organisational learning, where information plays a role in building a felt need for change, an appreciation of the complexity of systems, and sustaining and guiding efforts to improve.
The framework also highlights how those seeking to secure change should be cognisant of the distinction between internal and external sources of motivation. Internal motivation is supported by information that can reasonably be attributed to an individual provider or organisation. Non-attributable, non-specific information is at risk of being explained away as outside the individual’s or organisation’s nexus of control. If responsibility for performance is diffuse and if opportunities to make change are limited, public release of performance data can be counterproductive. External motivation in contrast is principally supported by power and influence and valued benefits or feared consequences. The ability of performance information to secure change is largely determined by the extent to which external motivators are sustained, and perceptions about the value or impact of consequences.
Levers for change: in concert or conflict?
Data, information and knowledge support clinical delivery, the redesign of models of care and the consolidation of organisational structures to respond to changing population needs.20 46 The levers identified in this framework all rely, to varying degrees, on data—the result of codification of real phenomena into a form which can be systematically explored or interrogated. Their power relies on the transformation of these data into information, where numbers convey meaning about the measured phenomena, in order to build knowledge about how a system, organisation or clinician is performing.
Levers are the way to harness the power of data to secure improvement. However, a lever rarely operates in isolation—any system, organisation or healthcare professional is subject to multiple levers simultaneously. Meaningful and sustained change is more likely to be secured when different levers work in concert—aligning and reinforcing efforts to improve For example, normative levers, such as the publication of guidelines, have been shown to have a modest effect on behaviour when applied in isolation.47 48 When applied with cognitive, mimetic or coercive levers, they have been shown to be more effective than when acting on their own.49 For example, as a lever based on competition, the quasimarket reforms in the National Health Service have not been proven to bring about the beneficial outcomes that classical economic theory would predict of markets. This was due to misaligned levers and political interference, weak purchasers and barriers to exit and entry, as well as a lack of a stable policy environment to inspire staff commitment and enthusiasm.50
Conversely, when levers are in conflict—for example, when externally driven change objectives run counter to internally grounded self-assessment and felt need for change—change is unlikely to proceed smoothly. For example, when cognitive levers of performance information suggest a need to improve but remain in conflict with current recognised professional practice or clinicians’ sense of competence, change is unlikely. Similarly, coercive levers have been shown to be ineffective when in conflict with other levers that seek to improve or maintain non-incentivised aspects of care (eg, in the implementation of the Quality Outcomes Framework in the UK).51
In some cases, change may fail because of a mismatch between levers and the purpose of a performance measurement initiative—whether it aims to secure improvement or to provide accountability.52 Efforts that seek to secure quality improvement are often embedded in programme that facilitate clinical acceptance and buy-in through confidential sharing of information, while those that seek to provide accountability are often coercive and public in nature. Perceptions about the underlying purpose of performance information can shape acceptance and effectiveness of different types of levers for change.
A system perspective to address the variety of levers and change perspectives
Finally, the efficacy of levers is context dependent—both in terms of where they are directed and who is directing them. For example, it would be difficult for a single organisation to have both the internal capacity and the external credibility to operate in a supportive facilitator role and simultaneously act as a coercive ‘watchdog’ that penalises poor performance. Similarly, it would be challenging to simultaneously support mimetic influences while using competitive approaches such as patient choice or purchasing and commissioning functions. Specialisation or concentration of levers in separate organisations can allow systems to better use each potential type of lever. While some levers are synergistic, many are in tension and a multi-agency approach across collaborating yet different organisations would help allow these tensions to be identified and resolved.
Researchers, managers, clinicians, policymakers and patients agree that securing sustained and meaningful improvement in performance is an important objective across healthcare systems internationally. There is not as much consensus however about how to secure such change, with a wide range of approaches, initiatives and interventions available. While there are many to select from, they are all variants of the core eight types of levers for change (table 2).
Table 2.
Key applications of levers and examples of applications in healthcare systems
| Key applications | How has this been applied in healthcare systems? |
| Cognitive | |
| Performance profiles/report cards/dashboards Benchmarking/league tables Root cause analyses/morbidity and mortality reviews Clinical feedback |
Performance reporting efforts such as profiles, report cards or benchmarking often incorporate a range of performance indicators covering different patient groups and aspects of care. They are usually enacted by independent reporting agencies or by government departments or ministries. The more analytic applications such as root cause analyses provide cognition about specific events and are usually enacted by healthcare provider organisations, professional groups or safety agencies. Examples: In the USA, the Hospital Compare initiative of the Centers for Medicaid and Medicare (CMS); and in New South Wales (NSW), Australia, the Bureau of Health Information publish hospital level data on risk-adjusted 30-day mortality and readmissions. Time series data show that improvements have been associated with public release of this information. In the English National Health Service (NHS), a ‘star rating’ regime introduced in 2003 was predominantly cognitive in nature but was coupled with coercive levers that were applied forcefully—bonus payments and earned autonomy, ‘three-star’ rating and hospital Chief Executive job losses with zero ratings. |
| Mimetic | |
| Local champions/opinion leaders Demonstrator sites/beacon practices Case studies Study tours/exchange programme Secondments/rotations |
Efforts to identify and highlight organisations or providers who are leaders in their field, articulate lessons and diffuse learning from their approaches and methods are usually coordinated by improvement organisations, professional groups or healthcare provider organisations. Examples: Many healthcare systems have sought to emulate the Kaiser Permanente model with numerous study tours and case studies as well as a focus on learning from magnet hospitals—known for their desirable work environment. Within the English NHS, change initiatives have often used beacon and accelerator sites to share good practice, promulgate change and provide expert advice. In Australia, demonstrator and pilot sites are frequently used to lead and leverage wider change. |
| Formative | |
| Continuing professional development/training/fellowships Clinical governance/Grand Rounds Mentorship programme Local consensus building/deliberative processes Organisational learning/action research/systems thinking Communities of practice/learning circles/academies |
Providing feedback is generally enacted by professional groups or colleagues and healthcare improvement agencies. Formative levers are often used in concert with cognitive levers—tracking performance as change takes place. Examples: Continuing professional development was introduced by the American Medical Association and by 1960 had incorporated a coercive lever/credit system to reward physicians for attending. It is now a key feature in most healthcare systems. Many clinical training programme based on feedback on performance have emerged in the Canadian context. In England in 1997, the concept of clinical governance was introduced with the aim of embedding a comprehensive approach to improve clinical quality and secure change. The concept has subsequently been adopted by many healthcare systems, including Australia and Canada. |
| Supportive | |
| Quality improvement/cultural change programme Plan Do Study Act processes Facilitators/management consultants Innovation funding Collaboratives Models of care/care pathways Decision support/reminders/alerts |
Processes that seek to facilitate, support and guide change are often enacted by quality improvement agencies, government departments or ministries, academic institutions and professional organisations. Examples: Internationally, a number of organisations mandated to secure change have relied primarily on supportive levers, such as the Modernisation Agency in England in 2000; recast subsequently as the NHS Institute for Innovation and Improvement (2006), NHS Improving Quality (2013) and the Sustainable Improvement Team (2016). In the USA, the Institute for Healthcare Improvement uses a range of levers, particularly supportive and mimetic in nature that offer opportunities to learn from, collaborate with and be inspired by experts. In NSW, the Agency for Clinical Innovation uses supportive levers to secure change in the public hospital sector. In the Canadian context, the Canadian Foundation for Health Improvement uses performance data to support change programme and also supports capacity building with regard to the ability for healthcare systems stakeholders to use performance information to support change. |
| Normative | |
| Inspection and accreditation Registration, licensing and revalidation Clinical audits Guidelines/standards Awareness campaigns |
Efforts to alter performance to bring it into line with defined and codified practice—‘what should be done’—are generally enacted by professional groups and by regulators. Examples: Inspection and accreditation regimes were introduced in the English NHS by the Commission for Health Improvement (1999), subsequently renamed the Commission for Healthcare Audit and Inspection (2004) and the Care Quality Commission (2009). Also in England, national service frameworks were introduced in 1998—articulating guidelines for organising and delivering care. In NSW, centrally defined ‘models of care’ provide detailed guidance for care delivery for different patient groups and diseases. Medical revalidation was introduced in England in 2012 and is about to be introduced in Australia. The National Institute for Clinical Excellence was introduced in 1999 in England (renamed the National Institute for Health and Care Excellence 2005 after merging with the Health Development Agency) and has been a template for health technology assessment and clinical guideline development across many healthcare systems. Choosing Wisely has been implemented in more than 20 healthcare systems—seeking to leverage change and reduce unnecessary care. Clinical audits are ubiquitous across healthcare systems. |
| Coercive | |
| Legislation and policy/rules/contracts Targets Key Performacne Iindicators/performance agreement Incentives/penalties Pay for performance ‘Special measures’ (supplanting local management) |
Coercive levers are principally enacted by government departments, ministries or regulators. They are often based on clearly defined objectives that are quantified and monitored. Examples: Meeting objectives or failing to meet objectives have salient consequences for the organisation or provider being monitored. Targets were a key policy instrument for change in the English NHS in the late 1990s. There has been particular criticism of the targets for waiting times and the strong coercive levers that accompanied them but the strength of the target regime has been established empirically although with attendant unanticipated consequences. Pay for performance has been of considerable interest in healthcare systems in the past decade—in primary care in England’s NHS (the Quality and Outcomes Framework) and in CMS-mediated penalties for adverse events and poor patient outcomes in the USA (and proposed in Australia). Most health systems use performance agreements and compacts to leverage change. |
| Structural | |
| Reorganisation/restructure Capital investments/funding arrangements Decommissioning / ‘sun setting’ Staffing/skill mix Hub and spoke networks Physical arrangements Business process reengineering |
Physical changes can be enacted by healthcare provider organisations seeking to secure localised change and by government departments seeking to secure system-wide change. Examples: Specific examples of levers that have been implemented include information technology (Connecting for Health in England’s NHS; e-Health in NSW), skill mix changes (introduction of nurse practitioners in the NHS) and organisational restructures (regional health authorities split into local health authorities in the NHS, Canada and in NSW, Australia). |
| Competitive | |
| Patient choice/personal health budgets Markets/internal markets/purchaser provider splits Tendering processes Commissioning |
Government departments and policymakers typically enact at a system-level market mechanisms and competition. Local providers may apply competitive levers in seeking to change particular services, such as cleaning, through tendering processes. Examples: In England, the Patient Choice Framework (2016) seeks to secure change, particularly in hospital waiting times. Quasimarkets were introduced in the NHS in the 1990s—seeking to leverage competition within public funded healthcare system; the USA introduced various programmes to support the provision of information to patients in order to guide their choice of providers. Many organisations are now reporting publicly and transparently performance information in Australia, Canada, the UK and the USA to inform choice. |
When it comes to securing change in complex organisations and systems and in professional practice, it is clear that there are no magic bullets.47 53 That is not to say that levers are ineffective. Levers are powerful but need informed and often nuanced application. This means that for wide scale change, a deliberate assessment of the role of different levers is needed together with a coordinated approach to their application. In addition, in complex systems, there are many actors or organisations that have some recourse to various levers. However, no one group or organisation is able to apply all types of leverage with equal effectiveness.
For example, the public release of hospital level mortality data mobilises cognitive and mimetic levers for change such as the capacity to self-identify and identify peers in performance reporting. Subsequent mobilisation of normative, supportive and formative levers, such as guidelines, quality improvement or training programme, guides and sustains efforts to improve by professionals, providers and systems. Continuing poor performance can also be met with coercive levers such as regulatory interventions, financial penalties or contractual consequences. Ultimately, local communities, if informed about the results, can add to building a strong case for change.
Limitations of the framework
This study is not without limitations. First, the inductive component of the model development is based on the synthesis of published literature and available grey literature, and so will be affected by any publication bias where levers that did not work in a particular context may not have featured in the retrieved publications. Second, the deductive component of the model development did not comprehensively review the relevant disciplines to ensure an exhaustive set of conceptual constructs. Despite these two limitations, the concordance of various previously published models with the proposed framework and the fact that no other models contained all the elements of the proposed framework suggest that it provides a clear contribution to the field. Finally, the model has not to date been tested empirically and so the relative effects of context have not been fully elucidated. However, the model has face validity and resonates with published accounts about how performance reporting influences change.
Conclusion
The assertion that information is not enough to secure meaningful change or quality improvement in healthcare is uncontested. However, information is a key and often essential component of most levers for change. Data and information tell us how we are doing, whether we differ from our peers, provides a way to explore and compare options for new ways of working, delivers feedback as change progresses, informs policy and managerial decision making, and measures impact. The framework suggested in this paper raises awareness of the implications of applying levers in isolation without due regard for context.
Clearly, there is a wide variety of levers in use. In healthcare systems, the impetus for change can vary from subtle to strident; it can be founded on fear or on hope; built on pressure to conform or an imperative to be distinguished; adopt an attitude of support or challenge; can be tacit or codified; and focused or pervasive in scope. Pressure to change can come from within or from outside—inducements can take the form of hugs, nudges or shoves. Levers for change are varied and multifaceted and have been successfully applied in a range of contexts. In complex adaptive systems such as health, multiple levers are needed and multimodal approaches have been shown to have the biggest impact. This paper provides a clear framework to support better planning and evaluation of efforts to measure and publicly report performance in the healthcare sector.
Supplementary Material
Acknowledgments
We would like to thank Christopher Papadopoulos for his assistance to the literature search and revision of retrieved manuscripts.
Footnotes
Contributors: J-FL generated the original idea, presented the original ideas in scientific plenaries, participated in the scoping of the literature, conceptualised the framework and drafted the manuscript. KS participated in the scoping of the literature and in the conceptualisation of the framework and drafted the manuscript. Both authors deliberated the findings and produced the discussion of the manuscript and revised the manuscript following reception of comments from peer reviewers.
Competing interests: None declared.
Ethics approval: This work was conducted without direct contact with patients or providers, representing a synthesis of published academic and grey literature.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data available.
References
- 1. Murray CJ, Frenk J. A framework for assessing the performance of health systems. Bull World Health Organ 2000;78:717–31. [PMC free article] [PubMed] [Google Scholar]
- 2. Organization for Economic Cooperation and Development. Measuring up: improving health system performance in OECD countries. Paris: OECD, 2002. [Google Scholar]
- 3. Institute of Medicine. Vital signs: core metrics for health and health care. Washington: National Academies Press, 2015. [PubMed] [Google Scholar]
- 4. Boland T, Fowler A. A systems perspective of performance management in public sector organisations. International Journal of Public Sector Management 2000;13:417–46. 10.1108/09513550010350832 [DOI] [Google Scholar]
- 5. Sandmeyer B, Fraser I. New evidence on what works in effective public reporting. Health Serv Res 2016;51:1159–66. 10.1111/1475-6773.12502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Braithwaite RS, Caplan A. Who is watching the watchmen: Is quality reporting ever harmful? SAGE Open Med 2014;2:205031211452342 10.1177/2050312114523425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fung CH, Lim YW, Mattke S, et al. . Systematic review: the evidence that publishing patient care performance data improves quality of care. Ann Intern Med 2008;148:111–23. 10.7326/0003-4819-148-2-200801150-00006 [DOI] [PubMed] [Google Scholar]
- 8. Pearse J, Mazevska D. The impact of public disclosure of health performance data: a rapid review. Sydney: Sax Institute, 2010. [Google Scholar]
- 9. Campanella P, Vukovic V, Parente P, et al. . The impact of public reporting on clinical outcomes: a systematic review and meta-analysis. BMC Health Serv Res 2016;16:296 10.1186/s12913-016-1543-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Berwick DM, James B, Coye MJ. Connections between quality measurement and improvement. Med Care 2003;41:I–30. 10.1097/00005650-200301001-00004 [DOI] [PubMed] [Google Scholar]
- 11. McGlynn EA, Asch SM, Adams J, et al. . The quality of health care delivered to adults in the United States. N Engl J Med 2003;348:2635–45. 10.1056/NEJMsa022615 [DOI] [PubMed] [Google Scholar]
- 12. McGlynn EA. Introduction and overview of the conceptual framework for a national quality measurement and reporting system. Med Care 2003;41:I–1. 10.1097/00005650-200301001-00001 [DOI] [PubMed] [Google Scholar]
- 13. McLoughlin V, Leatherman S, Fletcher M, et al. . Improving performance using indicators. Recent experiences in the United States, the United Kingdom, and Australia. Int J Qual Health Care 2001;13:455–62. 10.1093/intqhc/13.6.455 [DOI] [PubMed] [Google Scholar]
- 14. Bohmer RM. The hard work of health care transformation. N Engl J Med 2016;375:709–11. 10.1056/NEJMp1606458 [DOI] [PubMed] [Google Scholar]
- 15. Molloy A, Martin S, Gardner T, et al. . A clear road ahead: creating a coherent quality strategy for the English NHS. London: The Health Foundation, 2016. [Google Scholar]
- 16. Custers T, Hurley J, Klazinga NS, et al. . Selecting effective incentive structures in health care: A decision framework to support health care purchasers in finding the right incentives to drive performance. BMC Health Serv Res 2008;8:66 10.1186/1472-6963-8-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Grol R, Wensing M, Eccles M, et al. , Improving patient care: the implementation of change in health care. 2nd ed: Wiley-Blackwell, 2013. [Google Scholar]
- 18. Caldwell SD, Herold DM, Fedor DB. Toward an understanding of the relationships among organizational change, individual differences, and changes in person-environment fit: a cross-level study. J Appl Psychol 2004;89:868–82. 10.1037/0021-9010.89.5.868 [DOI] [PubMed] [Google Scholar]
- 19. Pettigrew A, Whipp R. Managing change for competitive success. Blackwell: Oxford, 1991. [Google Scholar]
- 20. Walker H, Armenakis A, Bernerth J. Factors influencing organizational change efforts: An integrative investigation of change content, context, process and individual differences. J Organ Change Manag 2007;20:761–73. [Google Scholar]
- 21. DiMaggio P, Powell W. The iron cage revisited institutional isomorphism and collective rationality in organization fields : Powell W, DiMaggio P, The New institutionalism in organizational analysis. Chicago: University of Chicago Press, 1991. [Google Scholar]
- 22. Rogers E. Diffusion of innovations. 5th ed New York: Free Press, 2003. [Google Scholar]
- 23. Greenhalgh T, Robert G, Bate P, et al. . Diffusion of innovations in health service organisations: a systematic review. London: Blackwell, 2005. [Google Scholar]
- 24. Michie S. ABC of Behaviour Change Theories. London: Lulu publishing, 2014. [Google Scholar]
- 25. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- 26. : Glanz K, Lewis F, Rimers B, Health behaviour and health education: theory, research, and practice. San Francisco: Jossey-Bass, 1990. [Google Scholar]
- 27. Perry C, Barnowski T, Parcel G. How individuals, environments, and health behaviour interact: Social learning theory : Glanz K, Lewis F, Rimer B, Health behaviour and health education: theory, research and practice. San Francisco: Jossey-Bass, 1990. [Google Scholar]
- 28. Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, 1986. [Google Scholar]
- 29. Cummings T, Worley C. Organization development and change. 10th ed California: Cengage Learning, 2015. [Google Scholar]
- 30. Bamford DR, Forrester PL. Managing planned and emergent change within an operations management environment. Int J Oper Prod Manage 2003;23:546–64. 10.1108/01443570310471857 [DOI] [Google Scholar]
- 31. Burnes B. Managing change: a strategic approach to organisational dynamics. 4th ed Harlow: Prentice Hall, 2004. [Google Scholar]
- 32. Liebhart M, Garcia-Lorenzo L. Between planned and emergent change: decision maker’s perceptions of managing change in organisations. Int J Knowledge, Culture Change Manage 2010;5:214–25. [Google Scholar]
- 33. Burns B. Kurt Lewin and the planned change approach to change: a reappraisal Gallos J, Organisational development. San Francisco: Jossey-Bass, 2006. [Google Scholar]
- 34. Livne-Tarandach R, Bartunek J. A new horizon for organizational change and development scholarship: Connecting planned and emergent change In: Woodman R, Pasmore W, Shani A, eds Research in organizational change and development, vol 17 2009:1–35. [Google Scholar]
- 35. Burnes B. Complexity theories and organizational change. Int J Manag Rev 2005;7:73–90. 10.1111/j.1468-2370.2005.00107.x [DOI] [Google Scholar]
- 36. Lewin K. Field theory in social science. New York: Harper and Row, 1951. [Google Scholar]
- 37. Weick KE, Quinn RE. Organizational change and development. Annu Rev Psychol 1999;50:361–86. 10.1146/annurev.psych.50.1.361 [DOI] [PubMed] [Google Scholar]
- 38. Stacey R. Managing the unknowable: strategic boundaries between order and chaos in organizations. San Francisco: Jossey-Bass, 1992. [Google Scholar]
- 39. Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Washington: National Academies Press, 2001. [PubMed] [Google Scholar]
- 40. Leatherman S. Applying performance indicators to health system improvement Organization for economic development and cooperation. Measuring up: improving health system performance in OECD countries. Paris: OECD, 2002. [Google Scholar]
- 41. Plsek PE, Greenhalgh T. Complexity science: The challenge of complexity in health care. BMJ 2001;323:625–8. 10.1136/bmj.323.7313.625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Plsek PE, Wilson T. Complexity, leadership, and management in healthcare organisations. BMJ 2001;323:746–9. 10.1136/bmj.323.7315.746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Board NQ. NQB’s Shared commitment to quality. London: NQB, 2017. [Google Scholar]
- 44. Naylor D, Iron K, Handa K. Measuring health system performance: problems and opportunities in the era of assessment and accountability Organisation for economic cooperation and development measuring up: improving health systems performance in OECD countries. Paris: OECD, 2002. [Google Scholar]
- 45. Leatherman S, Sutherland K. The quest for quality: refining the NHS reforms. London: Nuffield Trust, 2008. [Google Scholar]
- 46. Bevan G. Incentives and models of governance. Health Econ Policy Law 2015;10:345–50. 10.1017/S1744133114000486 [DOI] [PubMed] [Google Scholar]
- 47. Oxman AD, Thomson MA, Davis DA, et al. . No magic bullets: a systematic review of 102 trials of interventions to improve professional practice. CMAJ 1995;153:1423–31. [PMC free article] [PubMed] [Google Scholar]
- 48. Oxman AD. Helping people make well-informed decisions about health care: old and new challenges to achieving the aim of the Cochrane Collaboration. Syst Rev 2013;2:77 10.1186/2046-4053-2-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. National Institute for Health and Clinical Excellence. How to change practice. Understand, identify and overcome barriers to change, 2007. [Google Scholar]
- 50. Brereton L, Vasoodaven V. The impact of the NHS market: An overview of the literature. London: CIVITAS: Institute for the Study of Civil Society, 2010. [Google Scholar]
- 51. Doran T, Roland M. Lessons from major initiatives to improve primary care in the United Kingdom. Health Aff 2010;29:1023–9. 10.1377/hlthaff.2010.0069 [DOI] [PubMed] [Google Scholar]
- 52. Solberg LI, Mosser G, McDonald S. The three faces of performance measurement: improvement, accountability, and research. Jt Comm J Qual Improv 1997;23:135–47. 10.1016/S1070-3241(16)30305-4 [DOI] [PubMed] [Google Scholar]
- 53. Burnes B. No such thing as … a ‘one best way’ to manage organizational change. Management Decision 1996;34:11–18. 10.1108/00251749610150649 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2016-014825supp001.pdf (204.5KB, pdf)


