Abstract
Lasers have come up as the newest therapeutic modality in dermatological conditions including melasma. In this article, as a group of experts from Pigmentary Disorders Society in collaboration with South Asian Pigmentary Disorders Forum (SPF), we have tried to discuss the lasers which have been used in melasma and formulate simple consensus guidelines. Following thorough literature search, we have summarised the rationale of using the lasers and the supporting evidences have also been provided. It is clear that laser cannot be the first line treatment for melasma. However, it can be used as an adjuvant therapy in resistant cases, provided the selection of patient and counselling has been done properly.
Keywords: Lasers, melasma, expert opinion, consensus
What was known?
Numerous lasers and light devices have been used in melasma with unsatisfactory results. Besides, lasers are not advisable as monotherapy in the treatment of melasma. Q-switched lasers (QSL), fractional lasers, ablative lasers, intense pulsed lights (IPLs), copper bromide laser, thulium laser, and their combinations have all been used, but response is unpredictable, and the pigmentation frequently recurs. Since melanin has a broad absorption spectrum (630–1100 nm), a variety of lasers and light sources can be used, but the selection of patient, counselling and post-procedural follow-up form the backbone of laser therapy.
Introduction
Melasma is a common acquired facial pigmentary disorder and challenging to treat. Triple combination (FTC) creams and sunscreens remain the cornerstone of therapy followed by maintenance with hydroquinone (HQ) and non-HQ skin-lightening agents. Peels have made successful inroads and are used frequently as an adjunct to medical management.
A variety of lasers and light devices have been used with varying degrees of success in melasma. The vast array of devices and combination protocols that have been tried in melasma clearly indicate that no single modality is singularly effective. Q-switched lasers (QSL), fractional lasers, ablative lasers, intense pulsed lights (IPLs), copper bromide laser, thulium laser, and their combinations have all been used, but response is unpredictable, and the pigmentation frequently recurs. Lasers can be used in selected patients with resistant melasma after thorough counseling and preferably after conducting test treatments. This article discusses available evidence and brings forward a suggested treatment algorithm by 15 experts from Pigmentary Disorders Society (PDS) in a collaborative discussion called South Asian Pigmentary Forum (SPF).
The lasers and light-based devices used in melasma include:
IPL[1]
-
Fractional lasers - Fractional nonablative lasers and fractional ablative lasers[2]
1540 nm/1550 nm Er:Glass laser
2940 nm Er:YAG laser
10,600 nm CO2 laser
Ablative lasers[3]
Fractional lasers with transdermal drug delivery
QSLs-QS 1064 nm, QS 585/595 nm laser
Fractional QSNY laser and fractional QS ruby 694 nm lasers
Picosecond lasers
Sublative lasers - fractional 1927 nm, thulium fiber laser
Other lasers - copper bromide laser
-
Combination techniques.
Laser toning has gained immense popularity in Southeast Asia. The concept of laser toning (low fluence, multipass technique, multiple sessions at weekly intervals) is based on the proposed novel theory of subcellular selective photothermolysis, proposed by Mun et al. in 2011.[6] They studied the ultrastructural changes within melanosome, using transmission electron microscopy. They found a reduction in the dendrites of epidermal melanocytes, following laser treatment. Laser treatment caused selective photothermolysis on Stage IV melanosomes, wherein the melanocytes remained intact and only the melanosomes were destroyed. They concluded that laser toning was an effective method for treating melasma through subcellular-selective photothermolysis.
Traditional treatments were based on the principle of selective photothermolysis which results in destruction and death of pigment-containing cells. In response to cell death, inflammation follows and results in repigmentation and recurrence or in postinflammatory hyperpigmentation (PIH). The adverse effects were attributed to laser-induced basal layer damage and dermal inflammation leading to recurrence of melasma on sun exposure, PIH, rebound hyperpigmentation, and mottled depigmentation. This is in contrast to the principle of subcellular selective photothermolysis, which uses high-peak power, ultrashort pulse duration [5ns], and flat-top beam resulting in destruction of only melanin in the target cell but leaving the cell alive. Since fluence used is very less and there is no cell death, inflammation and heating is minimum, thus reducing the chances of recurrence.
Rationale for Use of Lasers in Melasma
Melanin has a broad absorption spectrum (630–1100 nm) allowing a variety of lasers and light sources to be used. Melanosomes have a short thermal relaxation time (50–500 nanoseconds). Longer wavelengths penetrate deeper to target the dermal pigment, but melanin absorption is better with shorter wavelengths.
QS Nd:YAG laser [(QSNY) 1064 nm] has a pulse duration of 10 ns. Hence, the QSNY laser seems like a logical choice for some cases of melasma, especially in individuals with darker skin tones.
Q-Switched Nd:YAG Laser
Low-fluence Q-switched (LFQS) Nd-YAG laser is the most widely studied laser for the treatment of melasma. However, there are no randomized controlled trials (RCTs) comparing the effectiveness, safety, and tolerability of Q-switched Nd-YAG laser (532 nm) versus topical corticosteroids or hydroquinone.
We have considered 10 studies [Table 1] which evaluated the role of LFQS Nd:YAG laser on 446 patients of melasma.[7,8,9,10,11,12,13,14,15,16]
Table 1.
Summary of a few important studies conducted on the safety and effectiveness of various lasers in melasma
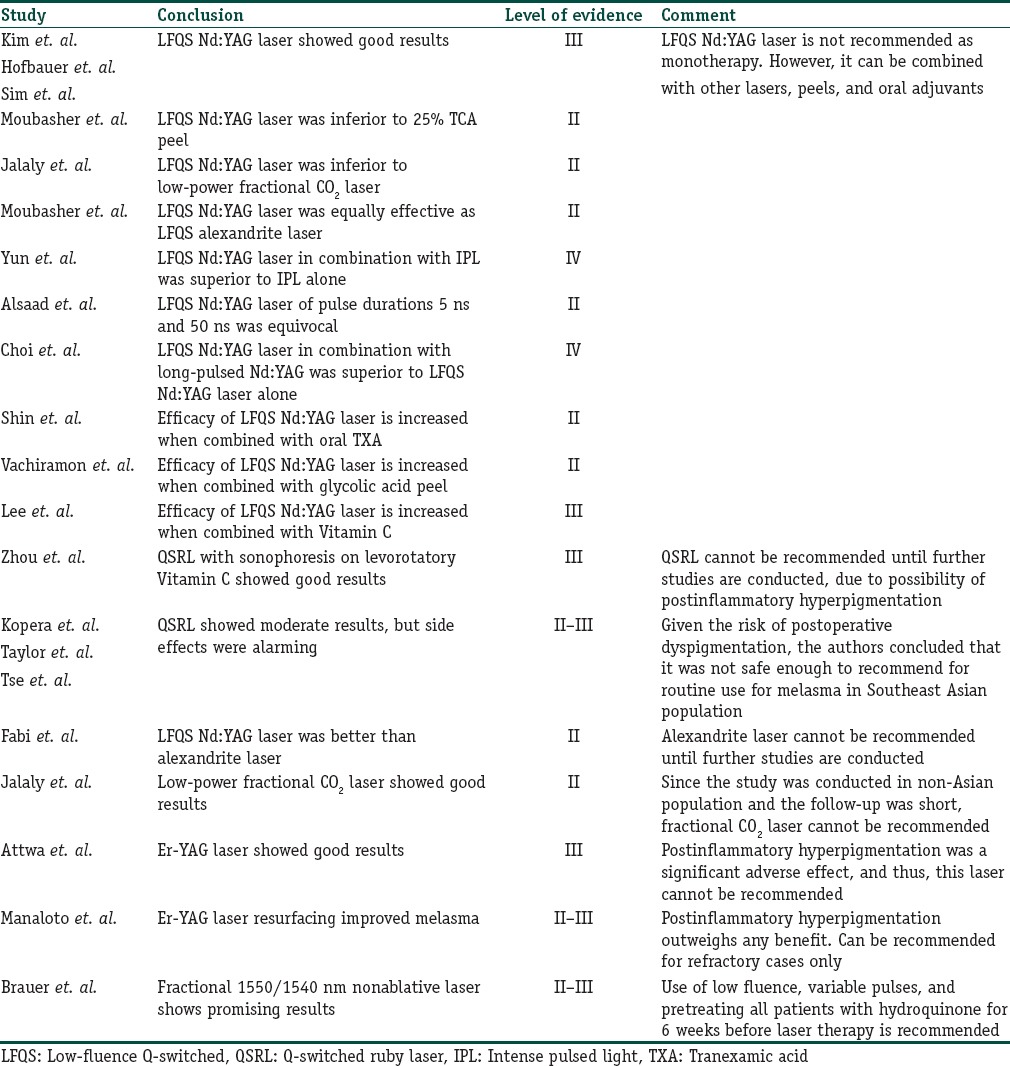
Out of these 10 studies, 6 were RCTs, 3 were nonrandomized uncontrolled studies, and 1 of them was a simple case–control study. Ninety-two patients were evaluated in the three uncontrolled studies and the authors concluded that LFQS Nd:YAG laser monotherapy had good results in melasma.[7,8,9]
However, the drawback of these studies was the small sample size, which puts a question mark on the effectiveness of LFQS Nd:YAG laser monotherapy in melasma. The effectiveness of Nd:YAG laser was found to be inferior to low-power fractional CO2 laser[11] and equal to that of LFQS alexandrite laser (755 nm).
To note, Chan et al. reported a series of facial depigmentation with the use of low-fluence QSNY laser. They concluded that laser toning with LFQS 1,064 nm Nd:YAG laser for skin rejuvenation and melasma can be associated with mottled depigmentation. Hence, caution needs to be exercised while performing this procedure and the risks need to be explained to patients.[17]
The results of LFQS Nd:YAG laser (1,064 nm) were found to be better when combined with IPL. However, number of patients was less and follow-up period was small.[13]
In addition, Na et al. observed that combination treatment may provide more rapid clinical resolution in mixed-type melasma with possible long-term clinical benefits.[18]
Besides, LFQS when combined with long-pulse Nd:YAG has shown better results in terms of reduction in melasma area severity index (MASI) score and significantly less adverse effects, when compared with LFQS Nd:YAG laser alone.[16]
Tian et al. reported a novel technique using a combination of fractional 2940-nm Er:YAG and 1064-nm Q-switched Nd:YAG lasers. Authors reported a rapid improvement in two cases, within a month of treatment. The novel strategy was found to deliver a safe, tolerable, and sustained result within a short period of treatment.[19]
Efficacy of LFQS Nd:YAG laser is increased when combined with oral tranexamic acid, glycolic acid peel, Vitamin C, etc.[20,21,22]
Q-switched Ruby Laser
We did not find any study which has evaluated the role of Q-switched ruby laser (QSRL) as a monotherapy in the treatment of melasma. Zhou et al. published a study which was conducted on Chinese patients, on the role of 694-nm fractional Q-switched ruby laser (fluence 2.5–3.5 J/cm2, 7.1 × 7.1 mm spot size, 27.7% area coverage) in combination with sonophoresis on levorotatory Vitamin C. There was a reduction in MASI score by 35% at the end of the study. However, there are no further studies to validate the results in Indian population.[23] Besides, previous studies have reported the development of PIH and recurrence of melasma following the use of ruby lasers.[24,25,26] Hence, it is not safe to use QSRL routinely in Southeast Asian population.
Intense Pulsed Light
IPL, a nonlaser light source that emits light with wavelengths between 515 and 1200 nm, has been studied alone and in comparison with hydroquinone for the treatment of melasma. IPL appears to give modest improvement as an adjunctive therapy in patients with melasma refractory to topical therapy alone and may be useful in patients who do not mind the 1- to 2-week recovery time.
Alexandrite Laser
Fabi et al. reported a randomized split-face clinical trial, comparing the effectiveness of alexandrite laser and LFQS Nd:YAG laser. The latter was found to be better, though statistically insignificant.[12]
Fractional and Ablative Lasers (CO2 Laser)
These are not used as monotherapies on account of the high incidence of side effects. However, low-fluence lasers are being used. Jalaly et al. conducted a split-face double-blinded randomized trial and compared low-power fractional CO2 laser with LFQS 1,064 nm Nd:YAG laser.[11] Fractional CO2 laser showed good results in terms of reduction in melanin index and MASI score. However, it is not wisely to recommend the use of this laser in Indian population due to financial constraints, short follow-up period, and the fact which cannot be overlooked is that the study was conducted in non-Asian population.
Er-Yag Laser
Attwa et al. conducted an uncontrolled study on the effectiveness of Er-YAG laser and reported significant improvement in MASI score. However, PIH was a statistically significant side effect.[27]
Besides, Manaloto et al. concluded that Er-YAG laser can be recommended for refractory cases only.[3]
Er-Glass Laser
Tourlaki et al. conducted a nonrandomized study on Er-glass laser. The reduction in MASI score was significant at the end of 1 month, but this was not sustained.[28]
Vascular Laser
Angiogenic melasma has been shown to respond to vascular lasers, which act by targeting vascular endothelial growth factors and the blood vessels of dermis.
Copper Bromide Laser
Copper bromide laser produces 2 wavelengths – 511 nm green light to treat pigmentary lesions and 578 nm yellow light to treat vascular lesions. Both wavelengths can be used simultaneously to treat melasma, every 2 weeks for 8 weeks. It may target vascular component as well as pigmentation in melasma.
Eimpunth et al. conducted a nonrandomized study in Thailand. They used copper bromide laser (dual-wavelength, 511 and 578 nm, fluence 7–19 J/cm2) but could not find any statistically significant improvement.[29]
In another split-face RCT conducted by Hammami et al., copper bromide laser was not found to be better than triple combination creams.[30]
Thulium Fiber Laser
Thulium fiber laser (1927 nm) nonablative laser has also shown promise in the management of melasma. Treatments are performed once a month for 3–4 months. It is a fractionated laser that produces small amount of epidermal ablation and greater amount of dermal heating.[31]
Fractional Nonablative Lasers
Fractional 1550/1540 nm nonablative laser therapy is the only laser treatment for melasma that has been approved by the FDA, and it has shown promising results. Given the risk for hyperpigmentation, some authors suggest using lower fluences, variable pulses, and pretreating all patients with hydroquinone for up to 6 weeks before laser therapy, especially in patients with a history of PIH.
Brauer et al. studied a low energy, low density, nonablative fractional 1927 nm laser for melasma, PIH, and photodamage. In this study, favorable outcomes were demonstrated and results were maintained at the 3-month follow-up.[32]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
What is new?
Lasers can be used in selected patients with resistant melasma after thorough counseling and preferably after conducting test treatments.
Low-fluence Q-switched (LFQS) Nd-YAG laser seems to be the best option for refractory cases of melasma, especially in individuals with darker skin tones. However, it is not recommended as monotherapy. It can be combined with other lasers, peels, and oral adjuvants.
Q-switched ruby laser and Erbium YAG laser are better avoided, due to the risk of developing post-inflammatory hyperpigmentation.
Fractional 1550/1540 nm non-ablative laser therapy is the only laser that has been approved by the FDA for melasma. To minimise the chances of post-inflammatory hyperpigmentation, it is advisable to use lower fluencies, variable pulses and pre-treatment with hydroquinone for4- 6 weeks before laser therapy.
Acknowledgment
The Consensus Meeting of a group South Asian Pigmentary Forum (SPF) with Pigmentary Disorders Society (PDS) was made possible by an educational grant by Galderma, India.
References
- 1.Wang CC, Hui CY, Sue YM, Wong WR, Hong HS. Intense pulsed light for the treatment of refractory melasma in Asian persons. Dermatol Surg. 2004;30:1196–200. doi: 10.1111/j.1524-4725.2004.30371.x. [DOI] [PubMed] [Google Scholar]
- 2.Rokhsar CK, Fitzpatrick RE. The treatment of melasma with fractional photothermolysis: A pilot study. Dermatol Surg. 2005;31:1645–50. doi: 10.2310/6350.2005.31302. [DOI] [PubMed] [Google Scholar]
- 3.Manaloto RM, Alster T. Erbium:YAG laser resurfacing for refractory melasma. Dermatol Surg. 1999;25:121–3. doi: 10.1046/j.1524-4725.1999.08103.x. [DOI] [PubMed] [Google Scholar]
- 4.Nouri K, Bowes L, Chartier T, Romagosa R, Spencer J. Combination treatment of melasma with pulsed CO2 laser followed by Q-switched alexandrite laser: A pilot study. Dermatol Surg. 1999;25:494–7. doi: 10.1046/j.1524-4725.1999.08248.x. [DOI] [PubMed] [Google Scholar]
- 5.Angsuwarangsee S, Polnikorn N. Combined ultrapulse CO2 laser and Q-switched alexandrite laser compared with Q-switched alexandrite laser alone for refractory melasma: Split-face design. Dermatol Surg. 2003;29:59–64. doi: 10.1046/j.1524-4725.2003.29009.x. [DOI] [PubMed] [Google Scholar]
- 6.Mun JY, Jeong SY, Kim JH, Han SS, Kim IH. A low fluence Q-switched nd:YAG laser modifies the 3D structure of melanocyte and ultrastructure of melanosome by subcellular-selective photothermolysis. J Electron Microsc (Tokyo) 2011;60:11–8. doi: 10.1093/jmicro/dfq068. [DOI] [PubMed] [Google Scholar]
- 7.Kim JY, Choi M, Nam CH, Kim JS, Kim MH, Park BC, et al. Treatment of melasma with the photoacoustic twin pulse mode of low-fluence 1,064 nm Q-switched nd:YAG laser. Ann Dermatol. 2016;28:290–6. doi: 10.5021/ad.2016.28.3.290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hofbauer Parra CA, Careta MF, Valente NY, de Sanches Osório NE, Torezan LA. Clinical and histopathologic assessment of facial melasma after low-fluence Q-switched neodymium-doped yttrium aluminium garnet laser. Dermatol Surg. 2016;42:507–12. doi: 10.1097/DSS.0000000000000653. [DOI] [PubMed] [Google Scholar]
- 9.Sim JH, Park YL, Lee JS, Lee SY, Choi WB, Kim HJ, et al. Treatment of melasma by low-fluence 1064 nm Q-switched Nd: YAG laser. J Dermatolog Treat. 2014;25:212–7. doi: 10.3109/09546634.2012.735639. [DOI] [PubMed] [Google Scholar]
- 10.Moubasher AE, Youssef EM, Abou-Taleb DA. Q-switched Nd:YAG laser versus trichloroacetic acid peeling in the treatment of melasma among Egyptian patients. Dermatol Surg. 2014;40:874–82. doi: 10.1097/DSS.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 11.Jalaly NY, Valizadeh N, Barikbin B, Yousefi M. Low-power fractional CO2 laser versus low-fluence Q-switch 1,064 nm Nd: YAG laser for treatment of melasma: A randomized, controlled, split-face study. Am J Clin Dermatol. 2014;15:357–63. doi: 10.1007/s40257-014-0080-x. [DOI] [PubMed] [Google Scholar]
- 12.Fabi SG, Friedmann DP, Niwa Massaki AB, Goldman MP. A randomized, split-face clinical trial of low-fluence Q-switched neodymium-doped yttrium aluminum garnet (1,064 nm) laser versus low-fluence Q-switched alexandrite laser (755 nm) for the treatment of facial melasma. Lasers Surg Med. 2014;46:531–7. doi: 10.1002/lsm.22263. [DOI] [PubMed] [Google Scholar]
- 13.Yun WJ, Moon HR, Lee MW, Choi JH, Chang SE. Combination treatment of low-fluence 1,064-nm Q-switched Nd:YAG laser with novel intense pulse light in Korean melasma patients: A prospective, randomized, controlled trial. Dermatol Surg. 2014;40:842–50. doi: 10.1097/DSS.0000000000000057. [DOI] [PubMed] [Google Scholar]
- 14.Vachiramon V, Sirithanabadeekul P, Sahawatwong S. Low-fluence Q-switched Nd:YAG 1064-nm laser and intense pulsed light for the treatment of melasma. J Eur Acad Dermatol Venereol. 2015;29:1339–46. doi: 10.1111/jdv.12854. [DOI] [PubMed] [Google Scholar]
- 15.Alsaad SM, Ross EV, Mishra V, Miller L. A split face study to document the safety and efficacy of clearance of melasma with a 5 ns q switched Nd YAG laser versus a 50 ns q switched Nd YAG laser. Lasers Surg Med. 2014;46:736–40. doi: 10.1002/lsm.22303. [DOI] [PubMed] [Google Scholar]
- 16.Choi CP, Yim SM, Seo SH, Ahn HH, Kye YC, Choi JE, et al. Retrospective analysis of melasma treatment using a dual mode of low-fluence Q-switched and long-pulse Nd: YAG laser vs. Low-fluence Q-switched Nd: YAG laser monotherapy. J Cosmet Laser Ther. 2015;17:2–8. doi: 10.3109/14764172.2014.957217. [DOI] [PubMed] [Google Scholar]
- 17.Chan NP, Ho SG, Shek SY, Yeung CK, Chan HH. A case series of facial depigmentation associated with low fluence Q-switched 1,064 nm Nd: YAG laser for skin rejuvenation and melasma. Lasers Surg Med. 2010;42:712–9. doi: 10.1002/lsm.20956. [DOI] [PubMed] [Google Scholar]
- 18.Na SY, Cho S, Lee JH. Combinational treatment using intense pulsed light and low fluence Q-switched Nd: YAG laser over laser treatment alone. Lasers Surg Med. 2010;42:712–9. [Google Scholar]
- 19.Tian WC. Novel technique to treat melasma in Chinese: The combination of 2940-nm fractional Er: YAG and 1064-nm Q-switched Nd: YAG laser. J Cosmet Laser Ther. 2016;18:72–4. doi: 10.3109/14764172.2015.1063662. [DOI] [PubMed] [Google Scholar]
- 20.Shin JU, Park J, Oh SH, Lee JH. Oral tranexamic acid enhances the efficacy of low-fluence 1064-nm quality-switched neodymium-doped yttrium aluminum garnet laser treatment for melasma in Koreans: A randomized, prospective trial. Dermatol Surg. 2013;39:435–42. doi: 10.1111/dsu.12060. [DOI] [PubMed] [Google Scholar]
- 21.Vachiramon V, Sahawatwong S, Sirithanabadeekul P. Treatment of melasma in men with low-fluence Q-switched neodymium-doped yttrium-aluminum-garnet laser versus combined laser and glycolic acid peeling. Dermatol Surg. 2015;41:457–65. doi: 10.1097/DSS.0000000000000304. [DOI] [PubMed] [Google Scholar]
- 22.Lee MC, Chang CS, Huang YL, Chang SL, Chang CH, Lin YF, et al. Treatment of melasma with mixed parameters of 1,064-nm Q-switched Nd: YAG laser toning and an enhanced effect of ultrasonic application of vitamin C: A split-face study. Lasers Med Sci. 2015;30:159–63. doi: 10.1007/s10103-014-1608-2. [DOI] [PubMed] [Google Scholar]
- 23.Zhou HL, Hu B, Zhang C. Efficacy of 694-nm fractional Q-switched ruby laser (QSRL) combined with sonophoresis on levorotatory vitamin C for treatment of melasma in Chinese patients. Lasers Med Sci. 2016;31:991–5. doi: 10.1007/s10103-016-1938-3. [DOI] [PubMed] [Google Scholar]
- 24.Kopera D, Hohenleutner U. Ruby laser treatment of melasma and postinflammatory hyperpigmentation. Dermatol Surg. 1995;21:994. doi: 10.1111/j.1524-4725.1995.tb00545.x. [DOI] [PubMed] [Google Scholar]
- 25.Taylor CR, Anderson RR. Ineffective treatment of refractory melasma and postinflammatory hyperpigmentation by Q-switched ruby laser. J Dermatol Surg Oncol. 1994;20:592–7. doi: 10.1111/j.1524-4725.1994.tb00152.x. [DOI] [PubMed] [Google Scholar]
- 26.Tse Y, Levine VJ, McClain SA, Ashinoff R. The removal of cutaneous pigmented lesions with the Q-switched ruby laser and the Q-switched neodymium: Yttrium-aluminum-garnet laser. A comparative study. J Dermatol Surg Oncol. 1994;20:795–800. doi: 10.1111/j.1524-4725.1994.tb03707.x. [DOI] [PubMed] [Google Scholar]
- 27.Attwa E, Khater M, Assaf M, Haleem MA. Melasma treatment using an erbium: YAG laser: A clinical, immunohistochemical, and ultrastructural study. Int J Dermatol. 2015;54:235–44. doi: 10.1111/ijd.12477. [DOI] [PubMed] [Google Scholar]
- 28.Tourlaki A, Galimberti MG, Pellacani G, Bencini PL. Combination of fractional erbium-glass laser and topical therapy in melasma resistant to triple-combination cream. J Dermatolog Treat. 2014;25:218–22. doi: 10.3109/09546634.2012.671911. [DOI] [PubMed] [Google Scholar]
- 29.Eimpunth S, Wanitphakdeedecha R, Triwongwaranat D, Varothai S, Manuskiatti W. Therapeutic outcome of melasma treatment by dual-wavelength (511 and 578 nm) laser in patients with skin phototypes III-V. Clin Exp Dermatol. 2014;39:292–7. doi: 10.1111/ced.12267. [DOI] [PubMed] [Google Scholar]
- 30.Hammami Ghorbel H, Boukari F, Fontas E, Montaudié H, Bahadoran P, Lacour JP, et al. Copper bromide laser vs. Triple-combination cream for the treatment of melasma: A Randomized clinical trial. JAMA Dermatol. 2015;151:791–2. doi: 10.1001/jamadermatol.2014.5580. [DOI] [PubMed] [Google Scholar]
- 31.Ho SG, Yeung CK, Chan NP, Shek SY, Chan HH. A retrospective study of the management of Chinese melasma patients using a 1927 nm fractional thulium fiber laser. J Cosmet Laser Ther. 2013;15:200–6. doi: 10.3109/14764172.2012.761346. [DOI] [PubMed] [Google Scholar]
- 32.Brauer JA, Alabdulrazzaq H, Bae YS, Geronemus RG. Evaluation of a low energy, low density, non-ablative fractional 1927 nm wavelength laser for facial skin resurfacing. J Drugs Dermatol. 2015;14:1262–7. [PubMed] [Google Scholar]


