Abstract
HIV stigma – both ‘self-stigma’ towards positive individuals and ‘stigma by association’ towards their families – is linked with adverse mental health. This study examined how stigma was associated with the mental health of parents and children in South Africa. Parent-child dyads (n=2477 dyads) in South Africa participated in a cross-sectional survey. For both parents and children, greater stigma was associated with their own reports of greater anxious and depressive symptoms. Parents reports of stigma was associated with children’s greater anxious and depressive symptoms. Children’s reports of stigma was related to parents greater anxious and depressive symptoms. There was a significant interaction, such that the association between parent stigma and depression was stronger when children also reported high levels of stigma. Findings provide support the effect of HIV stigma on the mental health of families and illustrate the importance of taking a family-based approach to stigma-reduction interventions to alleviate mental health problems.
Keywords: HIV, self-stigma, stigma by association, family, anxiety, depression, South Africa
South Africa has the largest population of individuals living with HIV and 2.3 million youths orphaned by HIV/AIDS (UNAIDS, 2014). A burgeoning body of global research demonstrates that the HIV/AIDS epidemic can have a detrimental effect on the mental health outcomes of children as a result of living with a parent with HIV/AIDS or through orphanhood (Chi & Li, 2013). Most often the burden of care for children orphaned by HIV/AIDS falls on women (MacNeil, 1996; Olenja, 1999). This gender differential in the burden of care can exacerbate stress on women who are already disparately engaged in family responsibilities (Kipp, Nkosi, Laing, & Jhangri, 2006). In addition, people living with HIV/AIDS and their family members in sub-Saharan Africa live in communities where stigma surrounding HIV/AIDS is rampant (Anderson, 1994; Kipp et al., 2006). HIV is one of the most stigmatised diseases in history (Parker & Aggleton, 2003), with stigma emerging as an important risk factor for poor mental health outcomes among children (Boyes & Cluver, 2013), as well as adults affected by HIV/AIDS in South Africa (Simbaya et al., 2007).
Stigma is a powerful negative societal process, which profoundly alters people’s social identity (Goffman, 1963). HIV stigma can result in social ostracism, prejudice, discrimination, and even in severe forms violence (Herek, Capitanio, & Widaman, 2002). Thus, HIV stigma can create a source of stress for people living with HIV/AIDS in the form of perceived “self-stigma” (Herek et al., 2002). Self-stigma involves experiences of rejection and discrimination from others, anticipation of discrimination from others, and internalization of social devaluation due to a devalued social identity (Bos, Pyor, Reeder, & Stutterheim, 2013; Earnshaw et al., 2014). South Africa has incredibly high levels of HIV stigma, which range from peer rejection to violence, and even murder (Skinner & Mfecane, 2004). Associations between HIV self-stigma and adverse mental health have been well-documented for HIV-affected children and adults in South Africa (Cluver & Orkin, 2009). Recent advancements in conceptual models of stigma have developed our understanding of HIV stigma. For example, the HIV Stigma Framework illustrates that social relationships are key to understanding the mechanisms through which stigma effects behaviour and poor physical and psychological health (Talley & Bettencourt, 2010; Tsai et al., 2013). These conceptual advancements in our understanding of stigma are particularly relevant to families who might be affected by HIV in multiple ways, including any combination of the following: a parent (a term we will also use to include caregivers serving as a parental surrogate) is living with HIV illness, a child is living with a parent who has HIV, a child is living with HIV, or a child has been orphaned by AIDS.
Family members of people living with HIV/AIDS (PLWH) may experience stigma by association including experiences of ostracism or discrimination (Talley & Bettencourt, 2010; Tsai et al., 2013). According to Goffman (1963) stigma by association occurs when a person is devalued, rejected, or victimized based on her or his relationship with a stigmatized individual, such as a PLWH. Studies have shown that stigma by association can produce the same negative consequences for caregivers as it does for PLWH (Wight, Aneshensal, Murphy, Miller-Martinez, & Beals, 2006). Qualitative studies indicate that HIV stigma can be experienced by association with family members living with HIV (Antle, Wells, Goldie, DeMatteo, & King, 2001; DeMatteo, Wells, Salter Goldie, & King, 2002). Quantitative studies have also found high levels of stigma among AIDS-orphaned and AIDS-affected children in South Africa (Cluver & Gardner, 2007), and these findings are particularly pronounced among children living in extreme poverty as operationalized by food insecurity (Cluver & Orkin, 2009). However, to our knowledge, few studies have quantitatively captured whether HIV stigma impacts the mental health of both parents and children in families affected by HIV in generalized epidemic settings such as South Africa.
To adequately capture the complexity of HIV stigma within the family context, models must account for the dyadic or reciprocal influence of parents on children and vice versa (Talley & Bettencourt, 2010; Wight et al., 2006). Building on these frameworks, HIV stigma is a stressor that can have a negative impact on the mental health of parent-child dyads. Accordingly, the stress of HIV stigma could have a ‘cross-over’ effect within the parent-child dyad, with one person’s experience of HIV stigma negatively impacting the other family member’s well-being. Accordingly, HIV stigma, whether self-stigma or stigma by association, experienced by one member of the dyad can effect the other member, such that greater HIV stigma may negatively impact family functioning, and lead to adverse mental health. However, studies have yet to examine the reciprocal influence of HIV stigma on children and their parents. As such, there is a need to focus on the impact of HIV stigma from a dyadic context; an examination of dyads allows one to evaluate the impact of stigma on both family members as a unit – rather than an individual context alone.
The purpose of the current study was to investigate the association between parents reports of HIV self-stigma and by association, as well as their children’s reports of stigma by association on both family members’ mental health outcomes using findings from a large household survey in South Africa. Consistent with previous research, we hypothesized that greater exposure to HIV stigma (parents) and stigma by association (children) would be associated with greater depressive and anxious symptoms at the individual level. In accordance with a relationship-orientated HIV stigma framework (Talley & Bettencourt, 2010), we proposed that the family’s experience of HIV stigma would be associated with greater levels of depressive symptoms and anxious symptoms for each family member after adjusting for food insecurity, child orphan status, and other sociodemographic factors. Specifically, we hypothesized that parent’s appraisals of HIV stigma would also negatively influence their child’s outcomes. Furthermore, we hypothesized that children’s perceptions of stigma by association would have a detrimental impact on parent’s mental health outcomes independent of their parents’ experiences of HIV stigma.
Methods
Sampling and Procedures
The cross-sectional data used was collected in KwaZulu-Natal Province, South Africa between 2009 and 2010 as part of a larger household health survey with 2477 parent-child pairs (N = 4,954 individuals). Details of the study methods have been published elsewhere (Casale, Wild, Cluver, & Kuo, 2014, 2015; Cluver & Orkin, 2009; Kuo, Cluver, Casale, & Lane, 2014; Lachman, Cluver, Boyes, Kuo, & Casale, 2014) and for updated information on papers emerged from this study and related studies in South Africa, see http://www.youngcarers.org.za/.
The study team selected urban and rural sites in KwaZulu-Natal Province. These sites were selected based on high HIV prevalence rates (each site had ≥ 30% antenatal HIV prevalence) (Department of Health, 2007) and provincial health deprivation indices (Noble et al., 2006). Study interviewers recruited participants via household door to door sampling within a selected geographical area to determine household eligibility. Specifically, study interviewers visited each residence by going door-to-door, (visiting a maximum of three time on different days and at different times) to screen for eligibility. This procedure was designed to limit bias in the sampling process. If parents and children were eligible at the residence, they were asked if they were interested in participating. If both parents and children were interested in participating, interviewers obtained informed consent and assent prior to conducting interviews using survey instruments that had been translated and back-translated into isiZulu.
Eligibility criteria included a child living in the home who was 10–17 years of age and parent-child concurrence that the parent taking part in the study was their parent/caregiver (for the child) and the child was in their care (for the parent). This child age range was based on the World Health Organizations (2003) definition of adolescence which begins at age 10. Given the focus of the study on understanding the familial impacts of HIV, we sampled to ensure a large enough subsample of ill parents (or caregiver serving in the parental surrogate role), self-report surveys with ill adults caring for children were prioritized. This meant that in households where both ill and healthy caregivers of children 10–17 were present, ill caregivers were selected for the study. When more than one ill caregiver or eligible parent-child dyad existed within the same household, we used random selection to determine invitation to the study. The only additional eligibility criteria was that the child needed to confirm that the adult identified was their parent or caregiver.
Survey interviews lasted approximately an hour and were conducted in isiZulu. Parents were not present for the child’s interview in order to reduce social desirability. The refusal rate for study participation was low (i.e. less than 0.5%). The research team obtained approval to work at each of the study sites from key stakeholders including community and political leaders as well as the provincial departments of health and education. In addition, ethical approval was granted by the University of KwaZulu-Natal and University of Oxford.
Measures
Sociodemographics
Parents were asked their gender (1=female versus 0=male), age, educational level (1=No school versus 0=Any School), HIV status (1=HIV-positive versus 0=HIV-negative/unknown). Children were asked their age and gender (1=female versus 0=male). Given that food insecurity has been consistently associated with stigma and adverse mental health conditions (Cluver & Orkin, 2009, parents were asked about food insecurity, which was assessed based on one question in which the household ranked their experience of hunger ranging from ‘never’=1, to ‘often’=4, which was then dichotomized into “never” versus “ever.”
HIV status and child orphan status
HIV-illness status for the parent and AIDS-orphaned status for the child were assessed based on self-report of parent’s HIV status and a verbal HIV-symptom approach (VA). The verbal HIV-symptom-based approach was to identify HIV illness or AIDS-related causes of death has been used by other researchers in areas with high HIV prevalence and poor medical and death records, as well as low health systems utilization, or otherwise unreliable data on cause of death or illness. The VA questionnaire used was validated originally in Zimbabwe and demonstrated 83% sensitivity and 75% specificity for identification of AIDS death (Lopman et al., 2006), and was then adapted for use in identifying HIV illness in this study (Becker, Kuo, Cluver, Operario, & Moshabela, 2015). Consistent with the United Nations, orphanhood was defined as the loss of one or both biological parents by HIV or another condition (UNAIDS, 2004). Additionally, other illness’ status was determined through questions on illnesses and symptoms pertaining to the most common causes of adult illness in South Africa, including diabetes, arthritis, epilepsy and hypertension. ‘Other orphanhood’ referred to parental death from causes such as road accidents, homicide and other illnesses.
Parent Stigma
At the time the study was conducted, only one validated scale existed for evaluating stigma, but this measure did not fit the needs of this study because it was designed for people living with HIV (Kalichman et al., 2005) and did not encompass the experiences of people caring for orphaned children. Therefore, parents completed a 17-item stigma scale which was designed by USAID to measure self-stigma and stigma by association (example item: “In the last year, have you or your family…been excluded from a social gathering”) (USAID, 2006), In the current sample, the parent stigma scale was able to discriminate between HIV-positive and HIV-negative parents, such that HIV-positive parents reported significantly higher stigma scores (M = 1.54, SD = 2.28) compared to their HIV-negative counterparts (M = 0.57, SD = 1.24), p<0.001. Responses were summed to compute a total score, in which higher scores indicated greater stigma.This measure demonstrated adequate psychometric properties in this sample (α = 0.78).
Child Stigma
At the time of the study, no validated instruments to measure stigma among children affected by HIV existed. Therefore, a 4-item scale was used, derived from an existing HIV stigma scale (Berger, Ferrans, & Lashley, 2001). Participants reported experiences of being teased, unfairly treated, or facing negative social experiences due to family illness (i.e., “Because someone in my family is sick or has died… I’ve been treated badly”). Validation on this stigma scale was recently published for South African use, showing that validated for use with South African youth the measure was able to discriminate between HIV-affected and unaffected youth such that HIV-affected youth reported significantly higher reports of stigma by association compared to HIV-unaffected youth (Boyes, Mason, & Cluver, 2013). Responses were aggregated to compute a total score, in which higher scores indicated higher reports of stigma. The scale had good performance for internal reliability in the current sample (α = 0.87).
Parent Depressive Symptoms
Parents completed the 20-item Center for Epidemiologic Studies Depression Scale (CES-D), which evaluated depressive symptoms in the past week (Radloff, 1977). Responses were aggregated to compute a total score, in which higher scores indicated greater depressive symptoms. The CES-D showed high internal reliability in this sample (α = 0.95).
Child Depressive Symptoms
Depressive symptoms were measured with the Child Depression Inventory – Short Form (Kovacs, 1992). This 10-item scale evaluates depressive symptoms in the past two weeks. The Children’s Depression Inventory (Short Form) is strongly correlated with the full version (Kovacs, 1992), and has been used in prior studies in South Africa and had adequate psychometric properties in the current sample (α = 0.65). Responses were aggregated to compute a total score, in which higher scores indicated greater depressive symptoms.
Parent Anxious Symptoms
The Beck Anxiety Inventory (BAI) was used to assess anxious symptoms (Steer, Ranieri, Beck, & Clark, 1993). This tool has been widely used, including within South Africa (Steele & Edwards, 2008). Parent’s completed a 21-item scale which assesses the extent to which they have been bothered by anxious symptoms experienced over the past month (Casale et al., 2014). Responses are summed to compute a total score, in which higher scores indicated greater anxious symptoms. The BAI showed good psychometric properties in this sample (α = 0.95).
Child Anxious Symptoms
Children completed the Children’s Manifest Anxiety Scale-Revised (RCMAS) (Reynolds & Richmond, 1978), which has been validated for use with children in South Africa (Boyes & Cluver, 2013). Example items include “I worry a lot of the time” and “I am nervous”. Responses were aggregated to compute a total score, in which higher scores indicated greater anxious symptoms. The RCMAS demonstrated good internal reliability in the current sample (α = 0.84).
Statistical Analysis
We utilized dyadic analysis procedures described by Kenny, Kashy, and Cook (2006). We also conducted descriptive analyses including examination of frequency distributions or means and standard deviations by summarizing demographic characteristics, stigma, depressive symptoms and anxious symptoms for both family members. Pearson’s product-moment correlations were used to assess associations between parent-child dyad scores on continuous variable (Kenny, Kash, & Cook, 2006). Non-significant Pearson’s correlation coefficients indicate no relationship between responses of dyad members. In contrast, statistically significant values indicate dependence between responses of dyad members.
We used Actor-Partner Interdependence Model (APIM) (Kenny et al., 2006) to examine two aspects of the dyad: actor effects refer to an evaluation of whether an individual’s response to a measure can be used to predict his/her own score on the outcome, and partner effects refers to an evaluation of whether an individual’s response to a measure is can be used to predict his/her dyad pair’s score for a particular outcome (see Figure 1 for conceptual model). For example, in the context of this study, the Actor-Partner Interdependence model is being used to assess whether a child’s stigma scores can reliably predict their own depressive symptoms (i.e., an actor effect); relatedly, this model is being used to assess whether the child’s stigma score can reliably predict her or his parent’s stigma score (a partner effect). We also fit an interaction term between parent and child stigma scores for both anxious and depressive symptoms. APIM analyses was used to in our structural equation modeling to examine associations between stigma, depression, and anxiety in which each scale score was modeled as a single indicator variable, and account for the correlation between parent and child scores on both independent and dependent variables. All models statistically adjusted for child and parent age and gender, child orphan status, as well as parent HIV status, education, and reports of food insecurity. We used Mplus 7.1 to conduct APIM analyses, and SPSS version 23 to evaluate descriptive statistics and bivariate analyses.
Figure 1.
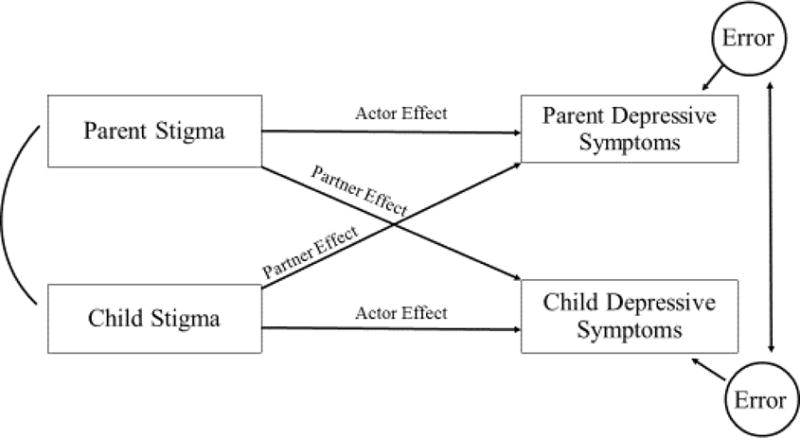
Figure of Actor and Partner Effects of Stigma on Depressive Symptoms
Results
Table 1 contains descriptive statistics for parents and children, respectively. Most of the participants were Black African (99.8%) while a sample proportion identified as Colored (0.2%). The majority of the participants spoke isiZulu (95.9%), with others reporting their primary language as isiXhosa (2.6%), Sesotho/Southern Sotho/Sotho (0.5%), Siswati/Swazi (0.1%), Xitsonga/Tsonga (0.1%), English (0.1%), and Shangani (0.1%). Similarly, most of the parents were female (88.9%). On average, parents were 44.2 years of age (range 18–92 years) and a small proportion completed high school (18.1%). Children were more evenly split for gender with just over half being female (53.9%). Children ranged in age from 10 to 17 years (M = 13.6). A large proportion of households (40.4%) reported food insecurity. Over one-quarter of the parents was classified as HIV-positive (27.7%, n = 676). Approximately 44% of the children were orphaned by HIV or some other condition and a large proportion of households (32.2%) were affected by HIV illness and/or orphanhood.
Table 1.
Demographic Characteristics of Study Sample (N=2477 dyads)
| Black African | 4,944 (99.8) |
| isiZulu language | 4751 (95.9) |
| Parent socio-demographic variables | |
| Female (n, %) | 2199 (88.9) |
| Age (mean, SD) | 44.2 (13.9) |
| Completed high school (n, %) | 448 (18.1) |
| Child socio-demographic variables | |
| Female (n, %) | 1319 (53.9) |
| Age (mean, SD) | 13.6 (2.2) |
| Type of orphanhood (n, %) | 1095 (44.2) |
| Maternal | 381 (15.6) |
| Paternal | 577 (23.6) |
| Double | 137 (5.6) |
| HIV-affected households (n, %) | 788 (32.2) |
| Parent is living with HIV but children are not orphaned by AIDS | 607 (24.8) |
| Parent of a child orphaned by AIDS but not living with HIV | 113 (4.6) |
| Parent is living with HIV and children are orphaned by AIDS | 69 (2.8) |
| Food Insecurity (n, %) | 989 (40.4) |
As shown in Table 2, parent’s stigma scores were positively associated with their own depressive symptoms and anxious symptoms, as well as their child’s stigma scores, depressive symptoms and anxious symptoms scores. Additionally, children’s stigma scores were positively correlated with their own depressive symptoms and anxious symptoms, and positively correlated with their parent’s depressive and anxious symptoms.
Table 2.
Bivariate Comparisons
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. Parent Stigma | – | |||||
| 2. Child Stigma | .120*** | – | ||||
| 3. Parent Depressive Symptoms | .247*** | .115*** | – | |||
| 4. Child Depressive Symptoms | .116*** | .259*** | .133*** | – | ||
| 5. Parent Anxiety Symptoms | .131*** | .094*** | .675*** | .079*** | – | |
| 6. Child Anxiety Symptoms | .158*** | .225*** | .206*** | .300*** | .136*** | – |
p<0.001;
p<0.01;
p<0.05
The impact of stigma on depressive symptoms
As shown in Table 3, actor reports of stigma were positively associated with actor depressive symptoms for both parents and children. In addition, there were significant partner effects such that both parent and children’s stigma scores were positively associated with the other’s depressive symptoms. There was also a significant interaction between parent and child-reported stigma for parent’s depressive symptoms, such that the association between parent-reported stigma and parent depression was stronger when their children also reported high levels of stigma. The interaction between parent and child reported stigma was not significant for children’s depressive symptoms. With regard to covariates, parent HIV-positive status, parent older age, parent female sex, food insecurity, and parent lower’s not having any education were positively associated with parent’s depressive symptoms. For children, food insecurity and parent’s not having any education were positively associated with their own depressive symptoms.
Table 3.
Actor and Partner Effects of Stigma on Depressive Symptoms
| Parent | Child | |||
|---|---|---|---|---|
|
| ||||
| B (SE) | p-value | B (SE) | p-value | |
| Parent Stigma | 1.23 (0.17) | 0.001 | 0.05 (0.02) | 0.010 |
| Child Stigma | 0.53 (0.14) | 0.001 | 0.19 (0.02) | 0.007 |
| Parent × Child Stigma | 0.02 (0.01) | 0.003 | 0.04 (0.17) | 0.534 |
| Parent HIV-positive | 5.77 (0.61) | 0.001 | 0.08 (0.08) | 0.242 |
| Child Orphaned | −0.43 (0.56) | 0.446 | 0.07 (0.08) | 0.310 |
| Parent Age | 0.07 (0.02) | 0.001 | −0.00 (0.00) | 0.371 |
| Child Age | 0.02 (0.12) | 0.870 | 0.03 (0.02) | 0.053 |
| Parent Female | 1.68 (0.84) | 0.048 | −0.10 (0.10) | 0.347 |
| Child Female | −0.88 (0.54) | 0.101 | 0.01 (0.07) | 0.876 |
| Food Insecurity | 3.32 (0.65) | 0.001 | 0.35 (0.08) | 0.001 |
| Parent No School | 3.69 (0.67) | 0.001 | 0.19 (0.08) | 0.018 |
The impact of stigma on anxious symptoms
Table 4 also presents actor and partner effects of stigma on both parent and their children’s anxious symptoms scores. For both parents and their children, one’s own report (i.e., the actor effect) of stigma were positively associated with anxious symptoms. Results also indicated that there was a partner effect for both partners, such that their family members’ stigma scores (partner effects) were positively associated with anxious symptoms. There was no significant interaction for parent and child stigma scores on either family members reports of anxious symptoms. With regard to covariates, parent HIV-positive status, parent older age, and parent’s not having any education were each positively associated with the parent’s reports of anxious symptoms. Additionally, parent’s HIV-positive status, child’s older age, food insecurity, and parent’s not having any education were each independently associated with children’s greater reports of anxious symptoms.
Table 4.
Actor and Partner Effects of Stigma on Anxious Symptoms
| Parent | Child | |||
|---|---|---|---|---|
|
| ||||
| B (SE) | p-value | B (SE) | p-value | |
| Parent Stigma | 0.38 (0.18) | 0.036 | 0.20 (0.04) | 0.001 |
| Child Stigma | 0.48 (0.16) | 0.002 | 0.31 (0.04) | 0.001 |
| Parent × Child Stigma | 0.00 (0.01) | 0.980 | 0.33 (0.19) | 0.144 |
| Parent HIV-positive | 5.33 (0.66) | 0.001 | 0.33 (0.15) | 0.031 |
| Child Orphaned | 0.37 (0.61) | 0.544 | 0.15 (0.14) | 0.281 |
| Parent Age | 0.15 (0.02) | 0.001 | −0.00 (0.01) | 0.776 |
| Child Age | −0.00 (0.13) | 0.987 | 0.07 (0.03) | 0.022 |
| Parent Female | 1.07 (0.91) | 0.241 | −0.28 (0.21) | 0.182 |
| Child Female | −0.05 (0.58) | 0.936 | 0.13 (0.13) | 0.332 |
| Food Insecurity | 0.81 (0.70) | 0.245 | 0.68 (0.16) | 0.001 |
| Parent No School | 3.66 (0.72) | 0.001 | 0.57 (0.17) | 0.001 |
Discussion
The primary purpose of the current study was to investigate the association between HIV stigma on the mental health of children and their parents in South Africa. Consistent with previous research in South Africa and globally, we found that family members’ perceptions of HIV stigma were independently associated with their own reports of greater depressive and anxious symptoms. Furthermore, the effects of parent stigma on their reports of depressive symptoms was exacerbated when children also reported higher levels of stigma. It is plausible that when both parents and their children both experience stigma it creates hopelessness and despair for parents, which may cause further isolation to protect their children. It is also possible, even likely that there may be both shared stigma experiences as well as unique experiences of stigma for each family member. For example, both parents and children may be involved in the provision of care for an HIV ill family member in the household.
Consistent with hypotheses, parent reports of greater stigma were independently related with their children’s greater depressive and anxious symptoms, over and above covariates including children’s own reports of stigma by association. Notably, the same pattern was also observed parents such that children’s reports of stigma by association was related with parent’s worse mental health outcomes. Our findings demonstrate that the mental health of children affected by HIV must be understood within a larger ecological framework, which includes social, parental, and child risk factors (Lachman et al., 2014). Increasing evidence illustrates that stigma can change the family environment, create challenges in parenting, and potentially have a negative impact on parent-child interactions (Lachman et al., 2014), which can in turn, negatively impact the mental health of children. Consistent with prior research (MacNeil, 1996; Olenja, 1999), we found that women were more likely to be caregivers of children compared to men. While we were unable to examine gender differences, caregiver burden and stigma may acerbate adverse mental health outcomes particularly among women, which can impact their ability to care for children. As such, future research is warranted to better understand the gender differences in stigma, mental health, and parenting among families affected by HIV/AIDS in South Africa.
The presence of HIV in the home has the potential to severely challenge the family system and child care as a result of poverty, stigma and illness (Sherr et al., 2014). Notably, we found that lower socioeconomic status and food insecurity were also independent risk factors for parent’s and children’s mental health over and above HIV stigma. There is a growing recognition that HIV has severe social, psychological, and health consequences for children and families in generalized epidemic settings, in part due to lack of supportive services and resources. Therefore, research is warranted to better understand the nature of these associations and the potential mechanisms to guide effective interventions and programming.
To date, existing stigma-reduction interventions primarily only target one form of stigma and have not attended to the family context (Sengupta, Banks, Jonas, Miles & Smith, 2011; Stangl, Lloyd, Brady, Holland, & Baral, 2013). However, our findings illustrate that stigma is much more complex phenomena and there is an urgent need to develop and test stigma-reduction interventions and other supportive services for parents and children which target the different manifestations of stigma to optimize the health of families affected by HIV/AIDS. Evidence suggests that positive social networks may offset the negative effects of stigma on mental health outcomes for children in South Africa (Cluver, Bowes, & Gardner, 2010). As such, stigma interventions delivered by peers may provide an important source of support for families while simultaneously changing social norms within communities.
While there have been declines in HIV-related stigma over time, stigmatizing attitudes persist towards people living with HIV, especially in sub-Saharan Africa (UNAIDS, 2015). Thus, policies are needed which promote health systems, education, employment, and housing environments that are supportive of families living with or experiencing HIV. Policy efforts are urgently needed to establish and sustain non-discriminatory environments with appropriate legal resource for those that experience stigma and discrimination related to living with or being affected by HIV.
Limitations
We recognize several limitations in this study. The cross-sectional study design limited our ability to investigate the temporal effect of HIV stigma on parent and children’s mental health. While accumulating evidence illustrates that HIV stigma impacts mental health of HIV/AIDS orphaned youth, there have been few longitudinal studies examining the directionality of these associations (Boyes & Cluver, 2013). As such, future longitudinal studies are needed to examine the directionality of these associations using dyadic data. Further research is also needed to understand the precise family processes and mechanisms linking stigma to poor mental health outcomes for parents and children, as well as the family processes and mechanisms that promote resilience for mental health despite exposure to HIV stigma. Parent HIV status was measured through self-report, which could have been affected by social desirability bias, and we were unable to assess children’s HIV status. HIV-positive children may experience both HIV self-stigma due to living with HIV themselves, orphanhood, or stigma by association due to their family being infected with HIV. Similarly, our measure of parent HIV stigma captured both self-stigma and stigma by association (e.g., a family member). As such, future research should explore how families’ experiences with HIV may result in different types of stigma. As such, research is warranted which utilizes more precise measures of these constructs to better understand how different types of stigma impact mental health.
Conclusions
Despite these limitations, study findings offer several promising directions for enhancing our HIV stigma intervention toolbox. Recent systematic reviews of interventions to address HIV stigma indicate that current intervention approaches are dominated by individual or community level interventions (Sengupta, Banks, Jonas, Miles, & Smith, 2011; Stangl et al., 2013). These findings indicate HIV stigma has a detrimental impact on both parent’s and children’s mental health, and family members experience of HIV can profoundly impact psychological well-being. The impact of HIV illness and orphanhood is rarely limited to an individual experience. To effectively reduce HIV stigma and limit detrimental effects of HIV stigma, mental health interventions need to incorporate dyadic and family-based approaches. Our results also indicate the need to develop effective community- and structural-level interventions to reduce HIV stigma in South Africa in order to support families affected by HIV, as well as continued research focusing on mental health interventions which address stigma and discrimination.
References
- Anderson S. Community responses to AIDS. World Health Forum. 1994;15:35–38. [PubMed] [Google Scholar]
- Antle BJ, Wells LM, Goldie RS, DeMatteo D, King SM. Challenges of parenting for families living with HIV/AIDS. Social Work. 2001;46:159–169. doi: 10.1093/sw/46.2.159. [DOI] [PubMed] [Google Scholar]
- Becker EE, Kuo C, Cluver L, Operario D, Moshabela M. Measuring child awareness for adult symptomatic HIV using a verbal assessment tool: Concordance between adult-child dyads on adult HIV symptoms. Sexually Transmitted Infections. 2015;91(7):528–533. doi: 10.1136/sextrans-2014-051728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berger B, Ferrans C, Lashley F. Measuring stigma in people with HIV: Psychometric assessment of the HIV Stigma Scale. Research in Nursing and Health. 2001;24:518–529. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- Bos AE, Pyor JB, Reeder GD, Stutterheim SE. Stigma: Advances in Theory and Research. Basic and Applied Social Psychology. 2013;35(1):1–9. [Google Scholar]
- Boyes ME, Cluver L. Performance of the revised children’s manifest axiety scale in a sample of children and adolscents from poor urban communities in Cape Town. European Journal of Psychological Assessment. 2013;29:113–120. [Google Scholar]
- Boyes ME, Cluver LD. Relationships among HIV/AIDS orphanhood, stigma, and symtpoms of anxiety and depression in South African Youth: A longitudinal investigatioon using a path analysis framework. Clinical Psychological Science. 2013;1(3):232–330. [Google Scholar]
- Boyes ME, Mason SJ, Cluver L. Validation of a brief stigma-by-association scale for use with HIV/AIDS-affected youth in South Africa. AIDS Care. 2013;25:215–222. doi: 10.1080/09540121.2012.699668. [DOI] [PubMed] [Google Scholar]
- Casale M, Wild L, Cluver L, Kuo C. The relationship between social support and anxiety among caregivers of children in HIV-endmic South Africa. Psychology, Health, & Medicine. 2014;19(4):490–503. doi: 10.1080/13548506.2013.832780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casale M, Wild L, Cluver L, Kuo C. Social support as a protective factor for depression among women caring for children in HIV-endmic South Africa. Journal of Behavioral Medicine. 2015;38(1):17–27. doi: 10.1007/s10865-014-9556-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chi P, Li X. Impact of parental HIV/AIDS on children’s psychological well-being: A systematic review of global literature. AIDS and Behavior. 2013;17(7):2554–2574. doi: 10.1007/s10461-012-0290-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cluver L, Bowes L, Gardner F. Risk and protective factors for bullying vicitimization among AIDS-affected and vulnerable children in South Africa. Child Abuse & Neglect. 2010;34(10):793–803. doi: 10.1016/j.chiabu.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Cluver L. Gardner Risk and protective factors for psychological well-being for children orphaned by AIDS in Cape Town: A qualitative study of children and caregivers’ perspectives. AIDS Care. 2007;19(3):318–325. doi: 10.1080/09540120600986578. [DOI] [PubMed] [Google Scholar]
- Cluver L, Orkin M. Cumulative risk and AIDS-orphanhood: Interactions of stigma, bullying and poverty on child mental health in South Africa. Social Science and Medicine. 2009;69:1186–1193. doi: 10.1016/j.socscimed.2009.07.033. [DOI] [PubMed] [Google Scholar]
- DeMatteo D, Wells LM, Salter Goldie R, King SM. The ‘family’ context of HIV: A need for comprehensive health and social policies. AIDS Care. 2002;14:261–278. doi: 10.1080/09540120120076940. [DOI] [PubMed] [Google Scholar]
- Department of Health. South Africa Demographic and Health Survey 2003. Pretoria: Department of Health; 2007. pp. 258–297. [Google Scholar]
- Earnshaw VA, Smith LA, Shuper PA, Fisher WA, Cornman DH, Fisher JD. HIV stigma and unprotected sex among PLWH in KwaZulu-Natal, South Africa: A longitudinal exploration of mediating mechanisms. AIDS Care. 2014;26(12):1506–1513. doi: 10.1080/09540121.2014.938015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E. Stigma: Notes on the management of spoiled identity. New York: Simon & Schuster; 1963. [Google Scholar]
- Herek G, Capitanio J, Widaman K. HIV-related stigma and knowledge in the United States: Prevalence and trends, 1991–1999. American Journal of Public Health. 2002;92:371–377. doi: 10.2105/ajph.92.3.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Jooste S, Toefy Y, Cain D, Cherry C, Kagee A. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS and Behavior. 2005;9(2):135–143. doi: 10.1007/s10461-005-3895-x. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic Data Analysis. New York, NY: The Guilford Press; 2006. [Google Scholar]
- Kipp W, Nkosi TM, Laing L, Jhangri GS. Care burden and self-reported health status of informal caregiving of HIV/AIDS patients in Kinshasa, Democratic Republic of Congo. AIDS Care. 2006;18(7):694–697. doi: 10.1080/13548500500294401. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children’s Depression Inventory. Niagra Falls, NY: Multi-health Systems; 1992. [Google Scholar]
- Kuo C, Cluver L, Casale M, Lane T. Cumulative effects of HIV illness and caring for children orphaned by AIDS on anxiety symptoms among adults caring for children in HIV-endemic South Africa. AIDS Patient Care and STDs. 2014;28(6):318–326. doi: 10.1089/apc.2013.0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachman JM, Cluver LD, Boyes ME, Kuo C, Casale M. Positive parenting for positive parents: HIV/AIDS, poverty, caregiver depression, child behavior, and parenting in South Africa. AIDS Care. 2014;26(3):304–313. doi: 10.1080/09540121.2013.825368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopman B, Barnabas R, Boerma J, Chawira G, Gaitskell K, Harrop T, Gregson S. Creating and Validating an Algorithm to Measure AIDS Mortality in the Adult Population using Verbal Autopsy. PLoS Medicine. 2006;3(8):e312. doi: 10.1371/journal.pmed.0030312. doi:310.1371/journal.pmed.0030312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacNeil JM. Use of culture care theory with Buganda women as AIDS caregivers. Journal of Transcultural Nursing. 1996;7(2):14–20. doi: 10.1177/104365969600700204. [DOI] [PubMed] [Google Scholar]
- May J, Carter M, Haddad L, Maluccio J. KwaZulu-Natal Income Dynamics Study (KIDS) 1993–1998: A Longitudinal Household Data Set for South African Policy Analysis. School of Development Studies, University of Kwazulu-Natal Durban; 1999. (Working Paper No. 21). [Google Scholar]
- Noble M, Babita M, Barnes H, Dibben C, Magasela W, Noble SN, Zungu S. The provincial indices of multiple deprivation for South Africa 2001. Oxford: University of Oxford; 2006. [Google Scholar]
- Olenja JM. Assessing community attitude towards home-based care for people with AIDS (PWAs) in Kenya. Journal of Community Health. 1999;24:187–199. doi: 10.1023/a:1018709314503. [DOI] [PubMed] [Google Scholar]
- Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Social Science and Medicine. 2003;57:13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reynolds C, Richmond B. What I think and feel: A revised measure of children’s anxiety. Journal of Abnormal Child Psychology. 1978;6:271–280. doi: 10.1007/BF00919131. [DOI] [PubMed] [Google Scholar]
- Sengupta S, Banks B, Jonas D, Miles M, Smith G. HIV Interventions to Reduce HIV/AIDS Stigma: A Systematic Review. AIDS and Behavior. 2011;15(6):1075–1087. doi: 10.1007/s10461-010-9847-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherr L, Cluver LD, Betancourt TS, Kellerman SE, Richter LM, Desmond C. Evidence of impact: Health, psychological and social effects of adult HIV on children. AIDS. 2014;28(Suppl 3):S251–S259. doi: 10.1097/QAD.0000000000000327. [DOI] [PubMed] [Google Scholar]
- Simbaya LC, Kalichman S, Strebel A, Cloete A, Henda N, Mqeketo A. Internalizated stigma, discrimination, and depression among men and women living with HIV/AIDS in Cape Town, South Africa. Social Science & Medicine. 2007;64(9):1823–1831. doi: 10.1016/j.socscimed.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner D, Mfecane S. Stigma, discrimination, and the implications for people living with HIV/AIDS in South Africa. Journal of Social Aspects of HIV/AIDS. 2004;1:157–164. doi: 10.1080/17290376.2004.9724838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? Journal of the International AIDS Society. 2013;16(Suppl 2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele DI, Edwards DJA. Development and validation of the Xhosa translation of the Beck inventories: 2. Item analysis, internal consistency, and factor analysis. Journal of Psychology in Africa. 2008;18(2):217–226. [Google Scholar]
- Steer RA, Ranieri WF, Beck AT, Clark DA. Further evidence for the validity of the beck anxiety inventory with psychiatric outpatients. Journal of Anxiety Disorders. 1993;7(3):195–205. [Google Scholar]
- Talley AE, Bettencourt BA. A relationship-orientated model of HIV-related stigma derived from a review of the HIV-affected couples literature. AIDS and Behavior. 2010;14(1):72–86. doi: 10.1007/s10461-008-9493-y. [DOI] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, Weiser SD. Internalized stigma, social distance, and disclosure of HIV seropositivity in rural Uganda. Annals of Behavioral Medicine. 2013;46:285–294. doi: 10.1007/s12160-013-9514-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. Children on the Brink 2004: A joint report of new orphan estimates and a framework for action. New York: UN; 2004. [Google Scholar]
- UNAIDS. The GAP Report Geneva: Joint United Nations Programme on HIV/AIDS. 2014. [Google Scholar]
- UNAIDS. How AIDS changed everything. 2015. [Google Scholar]
- USAID. Can we measure HIV/AIDS-related stigma and discrimination? 2006. [Google Scholar]
- Wight RG, Aneshensal CS, Murphy DA, Miller-Martinez D, Beals KP. Perceived HIV stigma in AIDS caregiving dyads. Social Science & Medicine. 2006;62:444–456. doi: 10.1016/j.socscimed.2005.06.004. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Strategic Directions for Improving the Health of Children and Adolescents. WHO; Geneva: 2003. [Google Scholar]


