Abstract
Background:
Parents’ knowledge of and attitudes toward concussions are often vital factors that affect care for injured adolescent athletes. It is important to understand the role that parents’ personal experiences with concussions play with regard to current concussion knowledge and attitudes so that clinicians may tailor their educational approaches.
Purpose/Hypothesis:
The purpose of this study was to determine an association between parents’ personal experiences and their child’s experiences with concussions as well as parental concussion knowledge and attitudes. We hypothesized that parents who have personally experienced symptoms or have a child who has experienced symptoms would have better knowledge and more favorable attitudes toward concussions.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Parents of youth sport athletes (N = 234 [82 male, 144 female, 8 unreported]; mean age, 44.0 ± 6.3 years) completed a prevalidated survey for concussion knowledge (maximum score possible, 29) and attitudes (maximum score possible, 49). Higher scores indicated better knowledge and more favorable attitudes toward concussive injuries. Parents reported the frequency of concussion diagnoses and/or experiences of concussion-related symptoms and whether their child had suffered a diagnosed concussion or experienced concussion symptoms (yes/no). Spearman rank correlation and multivariable regression were used to examine the association between experience of symptom clusters (self or child) and concussion knowledge and attitudes.
Results:
Knowledge was moderate (mean, 23.3 ± 2.5 of 29), while attitudes prioritized disclosure (mean, 46.3 ± 3.7 of 49). Parents’ experience of the sleep-arousal symptom cluster was positively associated with concussion attitudes (r = 0.22, P = .002; β = –3.301, P = .011). Parents with children who experienced sleep-arousal and vestibular-somatic symptom clusters were weakly associated with parental concussion knowledge (sleep-arousal: r = 0.15, P = .041; vestibular-somatic: r = 0.17, P = .020; β = 0.540, P = .012).
Conclusion:
Our findings suggest that parents’ personal experiences with concussion-related symptoms have little effect on parental knowledge and attitudes as a whole. However, clinicians should consider particular symptom clusters that may provide insight into targets for future concussion education. According to these findings, parents of youth sport participants would benefit from increased concussion education focusing on the types of symptoms as well as the consequences of suffering a concussion.
Keywords: concussion, knowledge, attitudes, symptom clusters, education
A concussion is a complex injury often defined by 4 primary characteristics: (1) a direct blow to the head or body, (2) rapid onset of short-lived neurological impairments, (3) functional deficits rather than structural impairments, and (4) graded clinical symptoms that sequentially resolve.17 As the level of sport participation rises, a greater incidence of concussions is seen, particularly within contact and collision sports23; however, it is unknown whether it is truly an increase in the number of injuries or an increase in those reporting injuries, as nondisclosure of a concussion is a reported issue within athletics.16,21 Another possible reason for the increase in concussions may be the presence of on-site medical providers who are trained to recognize and evaluate such injuries. Without proper disclosure of concussion-related symptoms by athletes, it is difficult to effectively diagnose, manage, and treat these injuries.
Because concussions are primarily a functional injury, which infrequently result in structural damage to the brain as visible through currently available neuroimaging modalities, they are diagnosed primarily by the presence of symptoms. These symptoms are commonly assessed subjectively through patient reporting; however, in early adolescents (ages 8-12 years), it may be difficult to gauge a child’s understanding of the symptoms because of misunderstandings with the terminology as well as symptom overlap with other abnormalities that may not be specific to a concussion.3,14 Therefore, it is advocated that the parent be included as an integral part of the concussion evaluation process as a supplement to not only how the patient feels but also how he or she acts in the home environment.6
Previous reports have suggested that the greatest influence on child care–seeking behavior is parental involvement.27 Common themes relating to parental influence include discrepancies in the parent’s versus child’s perception of illness severity as well as the parent’s wanting to do what is best for the child.8,18 Parents are often the source of care-seeking for their child after a concussion. Therefore, they play a vital role in the management of sport-related concussions, from initial recognition and response through to recovery. Parents have the ability to provide insight to those providing care about their child’s demeanor and functioning before and after the injury6 and may supplement and/or verify the child’s description. As such, concussion education targeted toward parents may be important to ensure appropriate recognition of the injury. In a sample of youth rugby players, most parents stated that they were able to recognize a potential concussive injury in their teenager, with nearly all being aware of the consequences of playing through a concussion; however, only half were actually aware of the return-to-play guidelines to be followed after the injury.25 Stevens et al24 observed that parents reported their child as asymptomatic despite he or she having postconcussive symptoms. Therefore, even though parents may be able to provide insight into injury recognition, they should not replace the athlete’s self-report and the authority of medical personnel regarding concussion recognition and management.
Many organizations have attempted to target education for parents regarding the signs and symptoms of a concussion along with red flags that would warrant the immediate referral to a medical professional.12 Without proper knowledge, parents may be less inclined to seek appropriate care for their child and therefore be more susceptible to negative outcomes of an injury. Parents’ reports of their child’s symptoms are often used to supplement the self-reports of young athletes.2,6 As such, parental attitudes toward a concussive injury are of great importance. If attitudes are negative, or hesitant to disclosure, they may be less inclined to report their child’s symptoms or be cognizant of the injury occurring. Specific components of positive versus negative attitudes are listed in Table 1. These attitudes and parental knowledge may also be influenced by previous experiences of concussions through their own experience or that of their child.
TABLE 1.
Components of Positive and Negative Attitudes
| Positive (Favorable) Attitudes |
|---|
|
It is serious when an athlete experiences a headache or dizziness after a blow to the head or body. It is important for an athlete not to participate in activity when experiencing signs and/or symptoms of a concussion. It is important to be informed of how concussions happen. It is important to be informed of how concussions can be prevented. It is important to know the steps to follow if an athlete has a concussion. It is important for an athlete to report possible symptoms to a medical professional or coach. |
| Negative Attitudes |
|
It is not serious when an athlete experiences a headache or dizziness after a blow to the head or body. It is not important for an athlete not to participate in activity when experiencing signs and/or symptoms of a concussion. It is not important to be informed of how concussions happen. It is not important to be informed of how concussions can be prevented. It is not important to know the steps to follow if an athlete has a concussion. It is not important for an athlete to report possible symptoms to a medical professional or coach. |
The purpose of this study was to determine if there was an association between parents’ own personal experience of suffering a concussion or their child suffering a concussion and their knowledge and attitudes toward concussions. By identifying this link, clinicians can better target parents needing supplemental information. We hypothesized that parents who have prior exposure to concussion symptoms, through either their own or their child's experience, would have better knowledge and more positive attitudes, indicating disclosure as a priority, of concussive injuries than those who have never experienced concussion-related symptoms. We further hypothesized that such prior experience of the vestibular-somatic and cognitive-sensory concussion-related symptom clusters may influence parental concussion-related knowledge and attitudes.
Methods
Institutional review board approval was attained before commencement of this study. A convenience sample of 234 youth sport parents (82 male, 144 female, 8 unreported) participated in this study. Cross-sectional surveys were distributed to parents in attendance at an educational meeting as part of a larger study aimed at exploring concussion education. This survey aimed to identify parental knowledge and attitudes regarding the recognition and response to concussions. The study sample included parents from North Carolina and Arizona, representing 3 middle schools and 21 youth sport teams (including football, boys’ and girls’ soccer, boys’ and girls’ basketball, boys’ and girls’ ice hockey, boys’ lacrosse, and baseball). Parent participants were between the ages of 19 and 68 years (mean age, 44.0 ± 6.3 years). Demographics for participants in this study are listed in Table 2.
TABLE 2.
Parents’ Demographics (N = 234)
| Variable | n (%) |
|---|---|
| Age (n = 15 missing) | |
| 18-24 y | 1 (0.4) |
| 25-34 y | 15 (6.4) |
| 35-44 y | 108 (46.2) |
| 45-54 y | 85 (36.3) |
| 55-64 y | 8 (3.4) |
| ≥65 y | 2 (0.8) |
| Sex (n = 8 missing) | |
| Male | 82 (35.0) |
| Female | 144 (61.5) |
| Formal concussion education (n = 10 missing) | |
| Yes | 48 (20.5) |
| No | 176 (75.2) |
| Concussion history | |
| Parent (self-reported) | |
| Diagnosed | 63 (26.9) |
| Symptoms | 98 (41.9) |
| Child (parent-reported) | |
| Diagnosed | 19 (8.1) |
| Symptoms | 61 (26.1) |
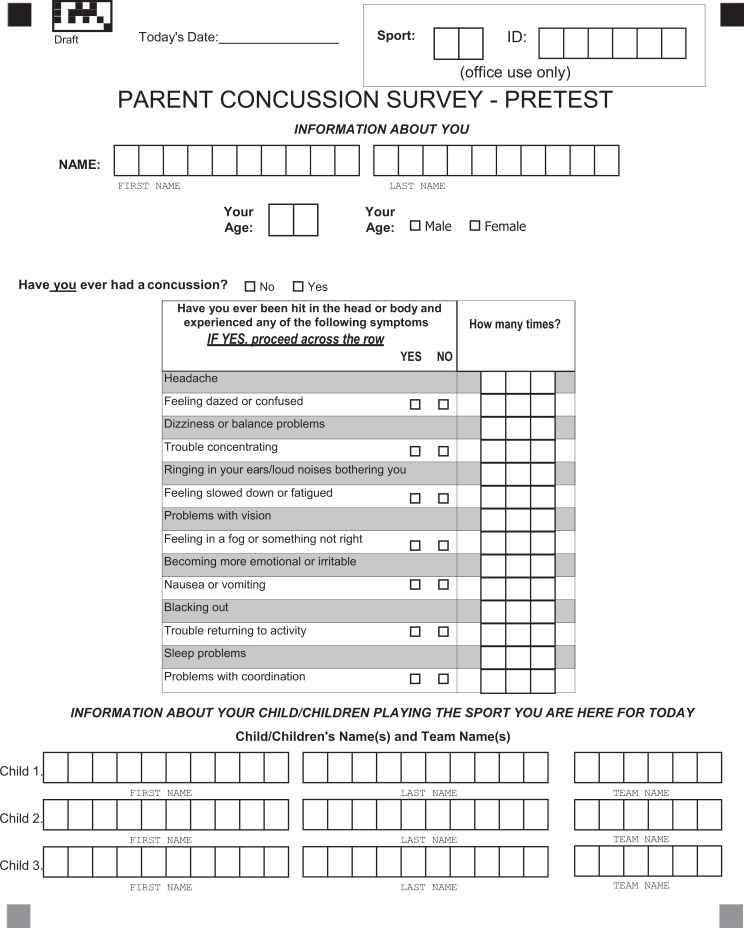
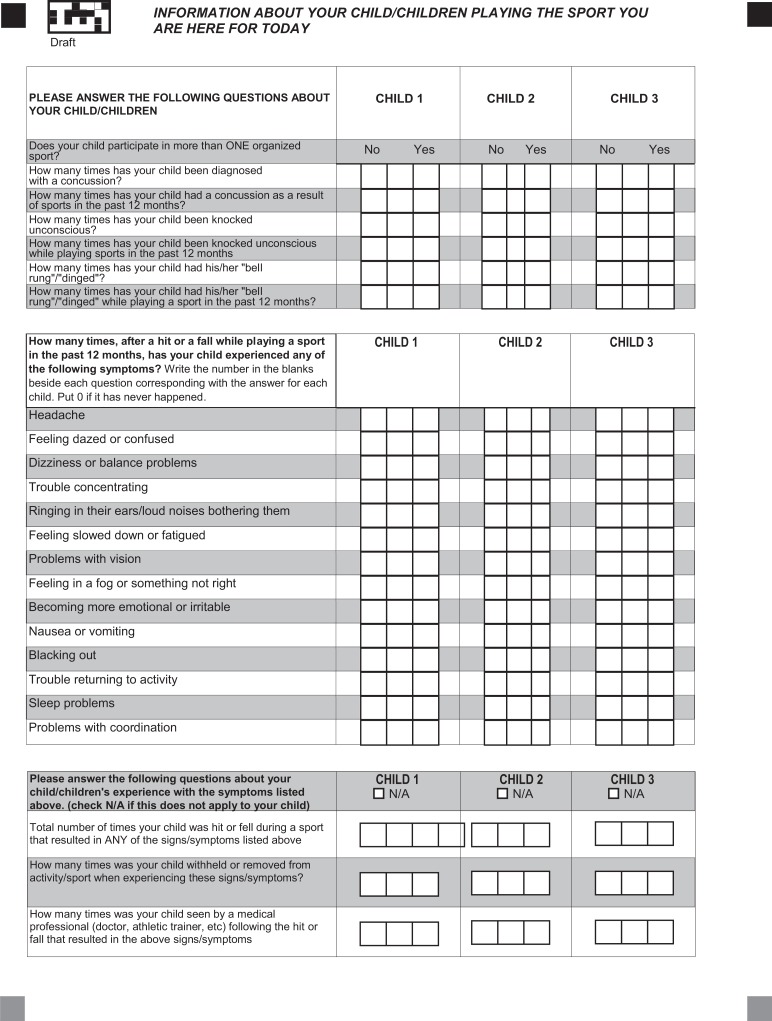
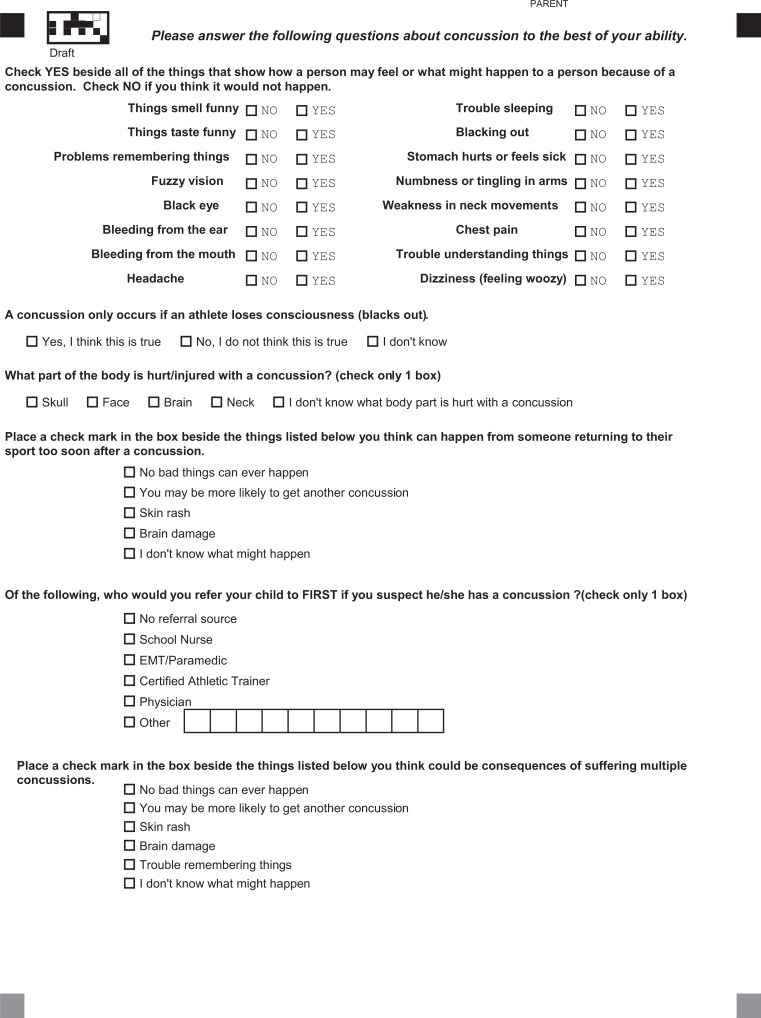
The survey was piloted and assessed for content validity on 19 youth sport parents before commencement of the study. The survey (see the Appendix) was modified from one that had previously been used.20,21 Internal consistency was acceptable for both the knowledge and attitude constructs, with Cronbach alpha beyond .70. The research team presented the study, approved consenting participants, and distributed the surveys to and collected the surveys from parents at preseason parent meetings. The survey took approximately 15 to 20 minutes to complete.
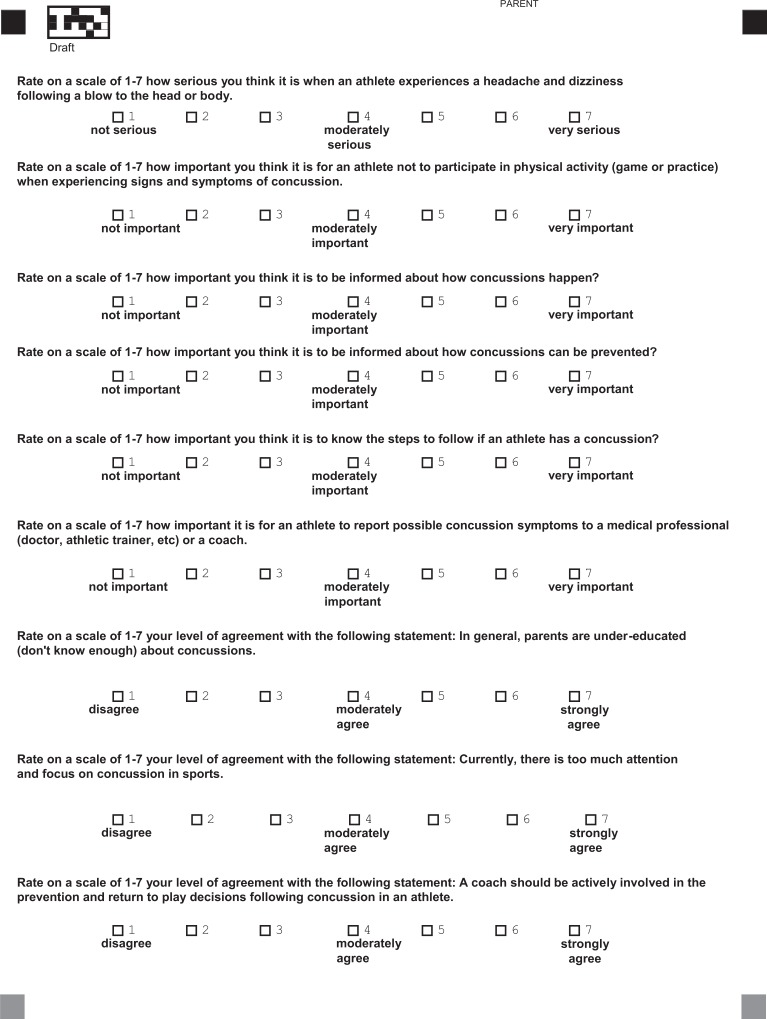
Descriptive statistics were calculated to summarize concussion knowledge and attitude questions and total scores. Parental concussion knowledge was assessed through a series of 29 questions, with a total score calculated by summing the number answered correctly. The higher the score, the better the knowledge of concussions (possible range, 0-29). Attitudes were assessed with a 7-item questionnaire, which was scored by summing the number of favorable/correct responses. Higher scores indicated a more favorable attitude (see Table 1) toward the need for concussion education, reporting, and treatment (possible range, 7-49).
Symptoms were grouped into 4 clusters for the parents’ and child’s experiences: vestibular-somatic, affective, sleep-arousal, and cognitive-sensory.10 These clusters were modified based on the literature of protracted symptom recovery11 as well as the ease of understanding. The specific symptoms that fall into each category are provided in Table 3. The total number of symptoms that each parent endorsed as having either experienced himself or herself (parents’ symptom report) or experienced by their child (child’s symptom report) was summed respectively to calculate each symptom cluster score (8 total: 4 parent, 4 child). To examine the association between each individual symptom cluster and the outcome variables of interest (knowledge and attitude totals), correlations (Spearman rank) were performed because of the nonnormal distribution of data. Symptom clusters were also used to create a multivariate model for parents’ experience, and an independent multivariate model for the child’s experience, on parental knowledge and attitudes of concussions. Data were analyzed in their entirety using an alpha level of .05 (set a priori) with SAS 9.4 software (SAS Institute).
TABLE 3.
Symptom Clustersa
| Cluster | Parent Experience | Child Experience (Parent-Reported) |
|---|---|---|
| Vestibular-somatic | 1.6 ± 2.3b | 0.5 ± 1.3b |
| Headache | 84 (39.8) | 52 (23.5) |
| Feeling dazed or confused | 66 (31.6) | 21 (9.5) |
| Dizziness or balance problems | 49 (23.4) | 13 (5.9) |
| Ringing in ears/bothersome loud noises | 25 (12.0) | 3 (1.4) |
| Vision problems | 27 (12.9) | 4 (1.8) |
| Nausea or vomiting | 26 (12.5) | 6 (2.7) |
| Blacking out | 38 (18.1) | 4 (1.8) |
| Trouble returning to activity | 17 (8.1) | 10 (4.5) |
| Coordination problems | 13 (6.2) | 6 (2.7) |
| Cognitive-sensory | 0.6 ± 1.0b | 0.2 ± 0.6b |
| Trouble concentrating | 33 (15.8) | 10 (4.5) |
| Feeling slowed down or fatigued | 41 (19.7) | 20 (9.0) |
| Feeling in a fog or something not right | 41 (19.6) | 13 (5.9) |
| Sleep-arousal | 0.1 ± 0.2b | 0.0 ± 0.1b |
| Sleep problems | 13 (6.2) | 3 (1.4) |
| Affective | 0.1 ± 0.3b | 0.0 ± 0.2b |
| Becoming more emotional or irritable | 15 (7.2) | 7 (3.2) |
aData are shown as n (%) of participants reporting the symptom from a total sample experiencing a diagnosed concussion or symptoms of a concussion unless otherwise indicated.
bMean ± SD number of symptoms within the cluster experienced by the parent or child.
Results
Concussion Knowledge and Attitudes
Overall, parents showed moderate concussion-related knowledge (23.3 ± 2.5 of 29) but high (positive) attitudes (46.3 ± 3.7 of 49). For knowledge, incorrect answers consisted of both errors of omission (concussion-related symptoms not identified as such) and errors of commission (inaccurately responding that a nonconcussion symptom is associated with a concussion). The concussion symptoms most often omitted by participants included numbness or tingling in the arms (27.5% incorrect), nausea/feeling sick (15.7% incorrect), and trouble sleeping (10.3% incorrect). The symptoms most often improperly reported as being concussion related included chest pain (68.1% incorrect), bleeding from the mouth (56.9% incorrect), and having a black eye (47.9% incorrect). It is important to note that participants often seemed to overestimate the effects of a concussion, having more commission than omission errors. Headache and loss of consciousness were the most common correctly identified symptoms (97.6% correct), followed closely by dizziness (96.7% correct) (Table 4).
TABLE 4.
Parental Knowledge of Concussion-Related Symptoms
| Variable | Yes/No | Correct Response/Total Response, n (%) |
|---|---|---|
| Signs and symptoms | ||
| Things smell funny | No | 117/213 (54.9) |
| Things taste funny | No | 119/213 (55.9) |
| Problems remembering things | Yes | 201/212 (94.8) |
| Fuzzy vision | Yes | 205/213 (96.2) |
| Black eye | No | 110/211 (52.1) |
| Bleeding from the ear | No | 139/212 (65.6) |
| Bleeding from the mouth | No | 91/212 (43.1) |
| Headache | Yes | 207/213 (97.6) |
| Trouble sleeping | Yes | 191/213 (89.7) |
| Blacking out | Yes | 200/211 (94.8) |
| Stomach hurts or feel sick | Yes | 177/210 (84.3) |
| Numbness or tingling in the arms | Yes | 153/211 (72.5) |
| Weakness in neck movements | No | 163/208 (78.4) |
| Chest pain | No | 67/210 (31.9) |
| Trouble understanding things | Yes | 201/210 (95.7) |
| Dizziness (feeling woozy) | Yes | 204/211 (96.7) |
| A concussion only occurs if an athlete loses consciousness (blacks out) | No | 207/212 (97.6) |
| The brain is the body part hurt/injured with a concussion | Yes | 194/202 (96.0) |
| Consequences of suffering a concussion | ||
| No bad things can ever happen | No | 213/214 (99.5) |
| One may be more likely to get another concussion | Yes | 162/214 (75.6) |
| Skin rash | No | 208/214 (97.2) |
| Brain damage | Yes | 176/214 (82.2) |
| Consequences of suffering multiple concussions | ||
| No bad things can ever happen | No | 215/215 (100.0) |
| One may be more likely to get another concussion | Yes | 139/215 (64.5) |
| Skin rash | No | 210/215 (97.7) |
| Brain damage | Yes | 207/215 (96.3) |
| Trouble remembering things | Yes | 148/215 (68.7) |
The attitude variables with the largest differences in their responses included the amount of attention currently placed on concussions in sport (6.0 ± 1.6; range, 1-7) and how serious parents think a headache or dizziness is after a blow to the head or body (6.3 ± 1.0; range, 3-7). Variables with the most protective attitudes (see Table 1) included the importance of reporting possible concussion symptoms to someone in authority (6.9 ± 0.4; range, 5-7) and the importance of knowing the steps to follow once a concussion occurs (6.9 ± 0.4; range, 5-7) (Table 5).
TABLE 5.
Parental Attitudes of Sport-Related Concussions
| Variable | Range | Mean |
|---|---|---|
| 1. How serious do you think it is when an athlete experiences a headache and dizziness after a blow to the head or body? | 3-7 (not to very serious) | 6.3 ± 1.0 |
| 2. How important do you think it is for an athlete not to participate in physical activity when experiencing signs and symptoms of a concussion? | 1-7 (not to very important) | 6.7 ± 0.9 |
| 3. How important do you think it is to be informed about how concussions happen? | 4-7 (not to very important) | 6.7 ± 0.7 |
| 4. How important do you think it is to be informed about how concussions can be prevented? | 3-7 (not to very important) | 6.8 ± 0.6 |
| 5. How important do you think it is to know the steps to follow if an athlete has a concussion? | 4-7 (not to very important) | 6.9 ± 0.4 |
| 6. How important is it for an athlete to report possible concussion symptoms to a medical professional or coach? | 5-7 (not to very important) | 6.9 ± 0.4 |
| 7. Currently, there is too much attention and focus on concussions in sports. | 1-7 (disagree to strongly agree) | 6.0 ± 1.6 |
Symptom Clusters
Separate clusters were formed from all possible symptoms experienced by both the parent and the child. The specific symptoms within each cluster and their respective incidence can be found in Table 3. For parents’ symptom reports, the vestibular-somatic symptom cluster had the widest potential range of 0 to 9, with parents experiencing a mean of 1.60 ± 2.33 symptoms at some point during their life. The cognitive-sensory symptom cluster had a potential range of 0 to 3, with the parent experiencing a mean of 0.55 ± 0.98 symptoms related to cognition. The sleep-arousal and affective symptom clusters each had a range of 0 to 1, with the parent experiencing a mean of 0.06 ± 0.24 and 0.07 ± 0.26 symptoms, respectively. The same symptoms comprised the child’s symptom reports. Parents reported the following mean values for each symptom cluster for their child: vestibular-somatic (0.54 ± 1.26), cognitive-sensory (0.19 ± 0.62), sleep-arousal (0.01 ± 0.11), and affective (0.03 ± 0.18).
Associations Between Symptom Clusters and Outcomes
A series of bivariate Spearman rank correlations revealed 3 statistically significant relationships, despite weak correlations: parents’ sleep-arousal cluster and attitudes (r = 0.22, P = .002, r 2 = 0.048), child’s sleep-arousal cluster and knowledge (r = 0.15, P = .041, r 2 = 0.023), and child’s vestibular-somatic cluster and knowledge (r = 0.17, P = .020, r 2 = 0.020). For parents, the experience of sleep-arousal symptoms was associated with their total attitude score. Total parental knowledge was associated with their child’s experience of both the sleep-arousal and vestibular-somatic symptom clusters. All other relationships were not statistically significant (Table 6). Multivariate regression models were then conducted to explore these relationships while controlling for multiple comparisons.
TABLE 6.
Influence of Symptom Clusters on Parental Knowledge and Attitudes
| Symptom Cluster | Spearman Correlation Coefficient (r) | Correlation P Value | r 2 Value (Effect Size) | Raw Regression Coefficient (β) | P Value |
|---|---|---|---|---|---|
| Knowledge | |||||
| Parent | |||||
| Vestibular-somatic | 0.14 | .063 | 0.020 | 0.150 | .261 |
| Cognitive-sensory | 0.12 | .125 | 0.014 | 0.002 | .996 |
| Sleep-arousal | 0.10 | .206 | 0.010 | –0.921 | .315 |
| Affective | –0.01 | .865 | 0.000 | 0.597 | .440 |
| Child | |||||
| Vestibular-somatic | 0.17 | .020a | 0.029 | 0.540 | .012a |
| Cognitive-sensory | 0.00 | .980 | 0.000 | –0.574 | .163 |
| Sleep-arousal | 0.15 | .041a | 0.023 | –0.902 | .705 |
| Affective | 0.09 | .236 | 0.008 | 0.097 | .938 |
| Attitudes | |||||
| Parent | |||||
| Vestibular-somatic | 0.05 | .465 | 0.003 | 0.052 | .797 |
| Cognitive-sensory | 0.01 | .926 | 0.000 | –0.507 | .323 |
| Sleep-arousal | 0.22 | .002b | 0.048 | –3.301 | .011a |
| Affective | 0.05 | .503 | 0.003 | –0.816 | .478 |
| Child | |||||
| Vestibular-somatic | 0.00 | .970 | 0.000 | –0.219 | .477 |
| Cognitive-sensory | 0.08 | .230 | 0.006 | 0.672 | .237 |
| Sleep-arousal | 0.13 | .064 | 0.017 | –3.004 | .251 |
| Affective | 0.10 | .158 | 0.010 | –0.029 | .986 |
aSignificance at alpha level of .05.
bSignificance at alpha level of .01.
Multivariate Regression Models
To examine the effects of experienced symptom cluster scores on the 2 outcomes of interest (attitudes and knowledge), separate multiple regression models were conducted, predicting each outcome of interest (total parental knowledge score or total attitude score) from either the child’s symptom cluster or parents’ symptom cluster total scores. In each of the 4 models, all symptom clusters were included as explanatory variables. These variables were kept separate because of the potential independent effects of each cluster. Within the 2 multivariate models testing the effects of the parents’ past symptom experience on concussion knowledge and attitudes, respectively, only parents’ experience of sleep-arousal concussion symptoms emerged as a significant predictor of the total parental attitude score (β = –3.301, P = .011) (Table 6). This indicates that parents who have experienced sleep-arousal–related symptoms also have better attitudes toward concussions. Within the 2 multivariate models for the child’s experience of symptom clusters, only the child’s experience of vestibular-somatic–related concussion symptoms had a significant effect on the total parental knowledge score (β = 0.540, P = .012) (Table 6).
Discussion
Nearly double the number of parents, compared with their children, reported experiencing concussion-related symptoms during their lifetime. The primary reason for this is likely that parents have had more time to accumulate a concussion history. However, the difference in reports may also be overestimated because of the lack of reporting from the young athletes.20 Many of the young athletes in this sample may also have not yet experienced a concussive injury, which thus may influence the knowledge and attitudes of the parent. This is important, as parents may learn and absorb concussion education most effectively after a concussion has been experienced in some capacity. Recent research highlights that athletes with a concussion history have been found to have more negative attitudes, lessening their likelihood of concussion disclosure, but no significant effect has been found related to concussion-related knowledge.22 No studies prior to ours have examined this relationship in parents. As these are parents of youth athletes (not high school age), they are often not exposed to concussion education through the school environment (as in secondary school); therefore, clinicians should be engaged in concussion education with this population in conjunction with coaches to support and promote its inclusion.
Another reason for higher parents’ self-reports may include the types of symptoms assessed through common symptom scales. Some current symptom scales, such as the Acute Concussion Evaluation,5 have been shown to be less valid in younger populations because of the terminology used to describe the symptoms.6 Parents may not have recognized their child’s concussion presentation because of their child complaining of symptoms not directly listed on the survey (even if they were similar) as well as the injury’s often not presenting an outward appearance.17 Therefore, without the child complaining of symptoms, the parent may not know that an injury occurred. This is supported in the literature related to other injuries. For example, in a study by Brudvik et al,2 parents’ perceptions of their child’s injury only moderately correlated with their child’s self-report. Parents have been found to both underestimate and overestimate the amount of pain that their child was in for a variety of diagnoses.19,23,26 The current literature suggests that parents and athletes have difficulty identifying concussion symptoms within themselves, and parents may underestimate the number of symptoms that their child is experiencing,4 while children do not feel that symptoms are a reason to stop participation when they are not severe or burdensome.3
Parental knowledge encompassed the ability to identify signs and symptoms of a concussion as well as distractors that are not actually signs/symptoms or consequences of a concussion. Parents most commonly correctly identified vestibular-somatic and cognitive-sensory symptoms including headache, blacking out, dizziness, trouble understanding, and trouble remembering. This is consistent with previous literature stating that physical signs of an injury are the most commonly recognized by parents.15 It is also important to note that headache and dizziness were the 2 symptoms most commonly experienced by participants, potentially indicating a link (although not found to be statistically significant) between personal experience and knowledge on an item-specific level. These physical signs of an injury are also most often focused on in concussion education provided by clinicians. Nearly all participants were also able to identify that a concussion can occur without a loss of consciousness. This is evidence of a knowledge shift, as years ago, this was a common misconception of concussive injuries.9,13 Despite this increased knowledge, the consequences of suffering a concussion are still less known. Therefore, clinicians should discuss potential long-term implications (eg, depression and mood disorders, memory problems, persistent symptoms, and the potential for repeat injuries) that may occur if the injury is not managed and treated properly. Such concussion education efforts should be made at all levels and should include coaches, parents, and athletes themselves.17
Overall, the diversity of responses related to concussion attitudes was minimal, indicating that participants may have positive attitudes around the constructs examined or simply “know” the right answer and how they should respond to a concussive injury. This finding is consistent with other studies showing that attitudes are typically more favorable on self-reported surveys, indicating that participants would do the right thing.12 Parents agreed that it is important to be informed of how concussions happen, how they can be prevented, the steps to follow once a concussion occurs, and the role of disclosure; however, participants had less agreement on actions that would reflect these attitudes, such as removing someone from play or thinking the amount of attention placed on concussions in sports is too high. These attitudes could potentially lead to risky parental decision making related to concussions, particularly within youth sports. If the coaches and/or parents have poor attitudes toward follow-through on these injuries, youth athletes may not be getting the proper care to avoid negative outcomes after an injury. They also have a risk of dismissing symptoms that a child is self-reporting by thinking that there is too much attention placed on concussions within sport.
Although our initial hypothesis posited that personal experience (via self or child) of particular concussion-related symptom clusters would influence parental knowledge and attitudes, the findings of this study do not fully support this hypothesis. Despite several statistically significant correlations, there were no clinically meaningful relationships. There was a weak positive correlation between the parents’ experience of sleep-arousal symptoms and better attitudes toward concussions. One of the potential reasons for this relationship is the disruption of daily life caused by sleep problems and other health-related disorders.1,7 However, only 5% of the variance in concussion-related attitudes was associated with sleep-arousal symptom experience (and vice versa).
There was also a weak positive correlation found between the child’s experience of vestibular-somatic symptoms and parental knowledge toward concussions. This finding may indicate the bidirectionality of parental knowledge. One explanation is that increased parental knowledge causes parents to ask their kids about these symptoms, resulting in a higher symptom presence. An alternative interpretation is that children may be telling their parents about symptoms that they are experiencing, resulting in increased parental knowledge. The present study does not include a way to differentiate the mechanism driving this relationship. Another reason is that these symptoms are most often associated with a concussion, as many of these same symptoms were also assessed via the symptom checklist for knowledge.17 However, only 3% of the variance in concussion-related knowledge was because of the experience of vestibular-somatic concussion symptoms (and vice versa). Because of the weak relationships and small effect sizes, these results should be interpreted with caution. Another potential limitation is that the total pool of parents who participated is unknown; however, all parents who attended the educational meeting participated in the survey. Future concussion education efforts should primarily focus on parents and children who have not experienced a concussive injury as well as the cognitive-sensory and the affective symptom clusters, which may not be experienced as often.
Conclusion
Our findings suggest that personal experience of concussion-related symptoms has little effect on parental knowledge and attitudes as a whole. However, this does not imply that clinicians should stop educational efforts. In fact, particular symptom clusters may provide insight into targets for future concussion education because of their impact on parental knowledge and attitudes. Parents of youth sport participants would benefit from increased education targeting the consequences of suffering a concussion as well as symptom clusters that do not receive as much attention, such as cognitive-sensory and affective symptoms; therefore, clinicians conducting concussion education should make these areas the primary target of discussion. Larger efforts should be made to educate parents of youth sport athletes, as they are frequently in a position to identify potential injuries, and current knowledge within this sample is low. Clinicians have the ability to expedite this need by providing targeted concussion education to parents of youth in their respective locations.
Appendix
Survey Constructs for Current Study
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: This study was funded in part by a grant from the National Operating Committee on Standards for Athletic Equipment.
Ethical approval for this study was obtained from the WakeMed Institutional Review Board (IRBNet No. 317759-1, WakeMed study No. 907), the University of North Carolina at Chapel Hill Institutional Review Board (IRB No. 12-1232), and the A.T. Still University Institutional Review Board (IRB No. 2012-53).
References
- 1. Al Khatib HK, Harding SV, Darzi J, Pot GK. The effects of partial sleep deprivation on energy balance: a systematic review and meta-analysis. Eur J Clin Nutr. 2017;71(5):614–624. [DOI] [PubMed] [Google Scholar]
- 2. Brudvik C, Moutte S-D, Baste V, Morken T. A comparison of pain assessment by physicians, parents and children in an outpatient setting. Emerg Med J. 2017;34(3):138–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chrisman SP, Quitiquit C, Rivara FP. Qualitative study of barriers to concussive symptom reporting in high school athletics. J Adolesc Health. 2013;52(3):330–335.e3. [DOI] [PubMed] [Google Scholar]
- 4. Elbin RJ, Knox J, Kegel N, et al. Assessing symptoms in adolescents following sport-related concussion: a comparison of four different approaches. Appl Neuropsychol Child. 2016;5(4):294–302. [DOI] [PubMed] [Google Scholar]
- 5. Gioia GA, Collins M, Isquith PK. Improving diagnosis and identification of mild traumatic brain injury with evidence: psychometric support for the acute concussion evaluation. J Head Trauma Rehabil. 2008;23:230–242. [DOI] [PubMed] [Google Scholar]
- 6. Gioia GA, Schneider JC, Vaughan CG, Isquith PK. Which symptom assessments and approaches are uniquely appropriate for paediatric concussion? Br J Sports Med. 2009;43(suppl 1):I13–I22. [DOI] [PubMed] [Google Scholar]
- 7. Itani O, Jike M, Watanabe N, Kaneita Y. Short sleep duration and health outcomes: a systematic review, meta-analysis, and meta-regression. Sleep Med. 2017;32:246–256. [DOI] [PubMed] [Google Scholar]
- 8. Janicke DM, Finney JW, Riley AW. Children’s health care use: a prospective investigation of factors related to care-seeking. Med Care. 2001;39(9):990–1001. [DOI] [PubMed] [Google Scholar]
- 9. Kelly JP. Loss of consciousness: pathophysiology and implications in grading and safe return to play. J Athl Train. 2001;36(3):249–252. [PMC free article] [PubMed] [Google Scholar]
- 10. Kontos AP, Elbin RJ, Schatz P, et al. A revised factor structure for the post-concussion symptom scale: baseline and postconcussion factors. Am J Sports Med. 2012;40(10):2375–2384. [DOI] [PubMed] [Google Scholar]
- 11. Lau BC, Collins MW, Lovell MR. Cutoff scores in neurocognitive testing and symptom clusters that predict protracted recovery from concussions in high school athletes. Neurosurgery. 2012;70(2):371–379. [DOI] [PubMed] [Google Scholar]
- 12. Lin AC, Salzman GA, Bachman SL, et al. Assessment of parental knowledge and attitudes toward pediatric sports-related concussions. Sports Health. 2015;7(2):124–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lovell MR, Iverson GL, Collins MW, McKeag D, Maroon JC. Does loss of consciousness predict neuropsychological decrements after concussion? Clin J Sport Med. 1999;9(4):193–198. [DOI] [PubMed] [Google Scholar]
- 14. Mailer BJ, Valovich-McLeod TC, Bay RC. Healthy youth are reliable in reporting symptoms on a graded symptom scale. J Sport Rehabil. 2008;17(1):11–20. [DOI] [PubMed] [Google Scholar]
- 15. Mannings C, Kalynych C, Joseph MM, Smotherman C, Kraemer DF. Knowledge assessment of sports-related concussion among parents of children aged 5 years to 15 years enrolled in recreational tackle football. J Trauma Acute Care Surg. 2014;77(3)(suppl 1):S18–S22. [DOI] [PubMed] [Google Scholar]
- 16. McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14(1):13–17. [DOI] [PubMed] [Google Scholar]
- 17. McCrory P, Meeuwisse W, Dvorak J, et al. Consensus statement on concussion in sport: the 5th International Conference on Concussion in Sport held in Berlin, October 2016. Br J Sports Med. 2017;51(11):838–847. [DOI] [PubMed] [Google Scholar]
- 18. Neill SJ, Jones CHD, Lakhanpaul M, Roland DT, Thompson MJ. Parents’ help-seeking behaviours during acute childhood illness at home: a contribution to explanatory theory. J Child Health Care. 2016;20(1):77–86. [DOI] [PubMed] [Google Scholar]
- 19. Petsios K, Priftis KN, Tsoumakas C, et al. Level of parent-asthmatic child agreement on health-related quality of life. J Asthma. 2011;48(3):286–297. [DOI] [PubMed] [Google Scholar]
- 20. Register-Mihalik JK, Guskiewicz KM, McLeod TCV, Linnan LA, Mueller FO, Marshall SW. Knowledge, attitude, and concussion-reporting behaviors among high school athletes: a preliminary study. J Athl Train. 2013;48(5):645–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Register-Mihalik JK, Linnan LA, Marshall SW, Valovich McLeod TC, Mueller FO, Guskiewicz KM. Using theory to understand high school aged athletes’ intentions to report sport-related concussion: implications for concussion education initiatives. Brain Inj. 2013;27(7-8):878–886. [DOI] [PubMed] [Google Scholar]
- 22. Register-Mihalik JK, Valovich McLeod TC, Linnan LA, Guskiewicz KM, Marshall SW. Relationship between concussion history and concussion knowledge, attitudes, and disclosure behavior in high school athletes. Clin J Sport Med. 2017;27(3):321–324. [DOI] [PubMed] [Google Scholar]
- 23. Rosenthal JA, Foraker RE, Collins CL, Comstock RD. National high school athlete concussion rates from 2005-2006 to 2011-2012. Am J Sports Med. 2014;42(7):1710–1715. [DOI] [PubMed] [Google Scholar]
- 24. Stevens PK, Penprase B, Kepros JP, Dunneback J. Parental recognition of postconcussive symptoms in children. J Trauma Nurs. 2010;17(4):178–182 , quiz 183-184. [DOI] [PubMed] [Google Scholar]
- 25. Sullivan SJ, Bourne L, Choie S, et al. Understanding of sport concussion by the parents of young rugby players: a pilot study. Clin J Sport Med. 2009;19(3):228–230. [DOI] [PubMed] [Google Scholar]
- 26. Varni JW, Thissen D, Stucky BD, et al. Item-level informant discrepancies between children and their parents on the PROMIS(®) pediatric scales. Qual Life Res. 2015;24(8):1921–1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wahlin T, Deane F. Discrepancies between parent- and adolescent-perceived problem severity and influences on help seeking from mental health services. Aust N Z J Psychiatry. 2012;46(6):553–560. [DOI] [PubMed] [Google Scholar]