Abstract
Posttraumatic stress disorder can develop after individual’s exposure or witnessing of life threatening events. It is characterized by three clusters of symptoms. The course of PTSD is often chronic and impedes individual’s functioning. Studies of PTSD treatment with paroxetine provide evidence for its efficacy in reducing symptoms and its favorable profile of side-effects. The objective of this work was to determine the efficacy of paroxetine in the treatment of PTSD.
The sample consisted of 30 subjects with chronic PTSD. All subjects received treatment with paroxetine in therapeutic dose range for six months. Subjects were assessed prior to therapy and following six months of treatment with paroxetine with the use of following instruments: SCL 90-R, Mississippi Questionnaire, and CGI.
The results indicate statistically significant reduction on all subscales of SCL 90-R following six months of treatment, P<0,05. The difference between two assessments with Mississippi Questionnaire was statistically significant, P< 0,05. PTSD rate in our sample was reduced from 100% before treatment to 64% after treatment. Paroxetine was administered in daily dose of 20 mg in 88% of the subjects, and 40 mg in the remaining 12%. Unwanted effects were registered in 16,7% of the subjects and they were mild. Objective improvement was registered in 84% of the sample, and subjective improvement was registered in 80%. Reduction of relapse symptoms was registered in 24% of the subjects.
Paroxetine proved to be efficient and safe in treatment of symptoms of PTSD in this study.
Keywords: PTSD, paroxetine, pharmacotherapy
INTRODUCTION
Post traumatic stress disorder (PTSD) is a psychiatric disorder that can develop subsequent to individual’s exposure or witnessing of life-threatening events, such as combat experience, natural disasters, serious accidents, terrorist attacks or interpersonal violence (1, 2). Individuals suffering from this disorder frequently develop symptoms such as: reliving the traumatic event, difficulty falling and staying asleep, frequent nightmares with the content of traumatic events that are subjectively so distressing and cause the individual to wake up with a startle and experience signs of significant autonomous system arousal such as profuse sweating and palpitations. These individuals gradually develop feeling of estrangement form their surroundings, they feel detached from the people who are important to them, they are tensed and irritable, and have exaggerated startle response. The symptoms described above can be so intense and distressing and last for long periods, thus leading to significant impairment in functioning of the affected individuals. The current diagnosis of PTSD adequately addresses the symptom developing in individuals exposed to short or singular traumatic events (1). In situations where individuals and groups of people survived exposure to prolonged and repetitive catastrophic stress events that has lasted for months and years, the situation changes substantially. This has led to a debate among the leading PTSD researchers about the need for introduction of a new diagnosis, new nosologic entity that will better address and describe the symptoms of long-term traumatization (2).
Epidemiological data for the populations lacking the experience of massive traumatization of whole communities as was the case in Bosnia and Herzegovina indicate the following: although 90% of the population will be exposed in their lifetime to potentially traumatic events that can lead to the development of PTSD, this disorder will be present in the course of the lifetime of 10,4% women and 5% men (3). These data from the National Commorbidity Survey (NCS) also indicate substantially high rate of co morbid Axis 1 psychiatric disorders that occur in 88,3% of individuals diagnosed with PTSD. In terms of course and prognosis, this study also provides data indicating the disorder’s chronicity: 50% of individuals developing PTSD recover within a year after the traumatic event, while the remaining 50% develop chronic PTSD, and one third of the individuals with chronic PTSD will remain symptomatic after 10 years. This explains the extent of the problem that PTSD presents for the public health system. The symptoms of PTSD such as hyper-arousal, intrusive memories, impulsivity and inflexibility present the consequence of the impaired functioning of a number of neurobiological systems that was caused by traumatization. Data from existing research studies have demonstrated the impairment in functioning and decrease in volume of hippocampal formation in chronic PTSD. This is in correlation with cognitive deterioration. Also, the activity of Broca’s area is decreased while there is evidence of increased activity of the amygdala, mesencephalon and hypothalamus (4, 5, 6). Treatment with selective serotonin reuptake inhibitors (SSRI) normalizes the activity in these areas and leads to reduction in psychological symptoms (7).
Psychopharmacological studies of PTSD treatment in current literature describe the efficacy of several groups of psychopharmacological agents (antipsychotic drugs, anti anxiety drugs, antidepressants, mood stabilizers). The largest number of studies describes SSRI drugs as the most efficacious. Hence this group of drugs presents today the first line of pharmacological treatment of PTSD in the majority of algorithms and guidelines for treatment of PTSD. Paroxetine proved to be safe and efficacious agent leading to a reduction in all three clusters of symptoms PTSD (reliving, avoidance and hyper-arousal) in the majority of published studies (7). The objective of this work was to determine the efficacy and safety of paroxetine in the treatment of Post traumatic stress disorder (PTSD).
SUBJECTS AND METHODS
The sample in this study consisted of 30 adult subjects who have been diagnosed with chronic PTSD. Prior to entering in the study all subjects have signed the informed consent form after the potential side-effects of treatment with paroxetine have been explained to them. The subjects did not receive financial compensation for being part of this study. This research was not sponsored by pharmaceutical industry.
All subjects received treatment with paroxetine in therapeutic dose range in the period of six months. The subjects were assessed with the following standardized psychometirc instruments: SCL 90-R for the registration of psychopathological symptoms, Mississippi Questionnaire for evaluation of PTSD symptoms and Clinical Global Impression Scale for the registration of efficacy and safety of paroxetine treatment.
RESULTS
SCL 90 -R
SCL 90 scale measures the severity of symptoms on a scale between 0 to 4. The results obtained on SCL 90-R Scale show statistically significant reduction in symptoms on all subscales after six months of treatment with paroxetine, p < 0,05. Depressive symptoms, interpersonal sensitivity, phobic symptoms, obsessive-compulsive symptoms and paranoid ideation show statistically somewhat less reduction compared with a reduction in anxiety, somatization, psychoticism and hostility. Nevertheless, the reduction on all subscales is statistically significant. (Figure 1).
FIGURE 1.

Descriptive statistics for SCL 90-R in three measurements
MISSISSIPPI QUESTIONNAIRE FOR PTSD
Reduction in PTSD symptoms is statistically significant. The difference between three measurements is statistically significant on p<0,05 level of significance (Table 1).
TABLE 1.
Mississippi Questionnaire (The difference between three measurements)

Percentage of subjects qualifying for the diagnosis of PTSD:
✓ before treatment 100%
✓ three months follow-up 80%
✓ six months follow-up 64%
The percentage of subjects qualifying for the diagnosis of PTSD was reduced from 100 percent pre-treatment to 80 percent in three months follow-up, and subsequently to 64 percent in six months follow-up.
Recommended doses of paroxetine for adults is in the range between 20 and 50 mg per day. The majority of subjects in this study (88 percent) achieved significant improvement with the initial adult dose of 20 mg a day (Table 2).
TABLE 2.
Daily dose of paroxetine

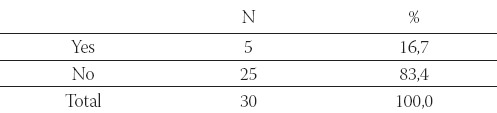
Adverse effects of paroxetine (nausea) were registered in 5 subjects, they were of mild intensity and required no additional treatment or drug discontinuation (Table 3). Results on the modified CGI (clinical global impression) scale
TABLE 3.
Unwanted effects of paroxetine treatment
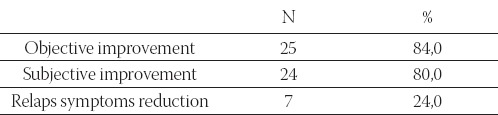
Objective improvement (the reduction of PTSD symptoms) was registered in 25 subjects. Subjective improvement was registered in 24 subjects. Relapse of symptoms was registered in 7 subjects (Table 4).
TABLE 4.
Efficacy of paroxetine
DISCUSSION
The results of this study are congruent with the results of previous research studies indicating the efficacy and safety of SSRIs in the treatment of PTSD (11, 12). The difference between three measurements on SCL 90-R Scale indicates a statistically significant reduction of symptoms on all subscales following six months of treatment with paroxetine. This agent proved to be very efficacious, leading to objective improvement in 84% of the subjects and subjective improvement in 80% of the subjects in this study. Depressive symptoms, interpersonal sensitivity, phobic symptoms, obsessive-compulsive symptoms and paranoid ideation showed statistically somewhat less reduction compared with a reduction in anxiety, somatization, psychoticism and hostility. Nevertheless, the reduction on all subscales was statistically significant. Clinical experience and treatment guidelines indicate that the reduction of these symptoms usually requires longer duration of treatment. Nevertheless, the reduction of these symptoms was statistically significant in this study. Total score of PTSD symptoms on Mississippi Scale showed a significant reduction, as well as a reduction in diagnosis of PTSD (caseness) after six months of treatment with paroxetine. Similar results were reported in preexisting studies of other researchers. Adverse effects of treatment with paroxetine were recorded in 16,7 of the subjects and they were of mild intensity. This indicates good tolerability of treatment with paroxetine, this also replicating the results of preexisting research.
CONCLUSION
The results of this study indicate a significant level of efficacy of paroxetine in the treatment of PTSD in this group of subjects.
In this study paroxetine proved to be a well tolerated drug that has led to significant reduction in all three PTSD symptom clusters (re-experiencing, avoidance and hyper-arousal).
Our results are congruent with the results of other studies of paroxetine efficacy and safety in the treatment of PTSD.
LIST OF ABBREVIATIONS
PTSD - Post traumatic stress disorder
SCL 90 -R - Symptom Checklist 90 Revised
NCS - National Commorbidty Survey
CGI - Clinical Global Impression Scale
SSRI - Selective Serotonin Reuptake Inhibitors
REFERENCES
- 1.American Psychiatric Association (APA) Diagnostic Statistical Manual of Mental Disorders. 4th edn. Washington, D.C: American Psychiatric Association; 1994. [Google Scholar]
- 2.Herman J. Trauma and recovery: The aftermath of violence from domestic abuse to political terror. New York: Basic Books; 1997. [Google Scholar]
- 3.Kessler R.C, Sonnega A, Bromet E.J, et al. Posttraumatic Stress Disorder in the National Commorbidity Survey. Arch. Gen. Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 4.Bremner J.D, Randall P, Scott T.M. MRI-based measurement of hippocampal volume in patients with combat -related posttraumatic stress disorder. Am. J. Psychiatry. 1995;152:973–981. doi: 10.1176/ajp.152.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gurvits T.V, Shenton M.E, Hokama H. Magnetic resonance imaging study of hippocampal volume in chronic, combat-related posttraumatic stress disorder. Biol. Psychiatry. 1996;40:1091–1099. doi: 10.1016/S0006-3223(96)00229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stein M.B, Koverola C, Hanna C. Hippocampal volume in women victimized by childhood sexual abuse. Psychol. Med. 1997;27:951–959. doi: 10.1017/s0033291797005242. [DOI] [PubMed] [Google Scholar]
- 7.Kučukalić A. Psihofarmakoterapija poremećaja uvjetovanih stresom. U: Tretman preživjelih torture i traume u postratnom društvu (Arcel-Tata L, PopovićS, KučukalićA, & Bravo-MehmedbašićA. ured.) CTV Sarajevo. 2003:174–80. [Google Scholar]
- 8.Marshall R.D, Schneier F.R, Fallon B.A, Knight C.B, Abbate L.A, Goetz D. An open trial of paroxetine in patients with non-combat-related, chronic posttraumatic stress disorder. J. Clin. Psychopharmacol. 1998;18:10. doi: 10.1097/00004714-199802000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Stein D.J. Improving treatment options-new clinical data on paroxetine. CINP. 2000 [Google Scholar]


