Summary
Background
Lower extremity muscle mass, strength, power, and physical performance are critical determinants of independent functioning in later life. Isokinetic dynamometers are becoming very common in assessing different features of muscle strength, in both research and clinical practice; however, reliability studies are still needed to support the extended use of those devices.
Objective
The purpose of this study is to assess the test-retest reliability of knee and ankle isokinetic and isometric strength testing protocols in a sample of older healthy subjects, using a new and untested isokinetic multi-joint evaluation system.
Methods
Sixteen male and fourteen female older adults (mean age 65.2 ± 4.6 years) were assessed in two testing sessions. Each participant performed a randomized testing procedure that includes different isometric and isokinetic tests for knee and ankle joints.
Results
All participants concluded the trial safety and no subject reported any discomfort throughout the overall assessment. Coefficients of correlation between measures were calculated showing moderate to strong effects among all test-retest assessments and paired-sample t test showed only one significant difference (p<0.05) in the maximal isokinetic bilateral knee flexion torque.
Conclusions
The multi-joint evaluation system for the assessment of knee and ankle isokinetic and isometric strength provided reliable test-retest measures in healthy older adults.
Level of evidence
Ib.
Keywords: isokinetic test, isometric test, isokinetic dynamometers, knee/ankle strength, torque
Introduction
During the last century, demographic trend is showing a marked decline of mortality and with an increase of the lifespan that leads to a general ageing of the population. It is estimated that approximately 13% of the 7 billion people worldwide are older adults aged 60 years and above; this number is expected to increase in proportion to 21% in the year 20501.
Overall, aging-associated concerns have been under the global lens for some time, especially the physical function. One crucial issue is the decline of neuromuscular activation2, strength and power that are a hallmarks of the aging process. In fact, aging process leads to a distinct muscle mass and strength loss3: the age-related loss of muscle mass (i.e. sarcopenia) entails a loss of functional and aerobic capacity, reduced mobility, and it is strongly connected to a loss of independence, disability, and frailty4, 5. In particular, lower extremity muscle mass, strength, power, and physical performance are critical determinants of independent functioning in later life, and a central tenet of quality of life6.
Some studies established that functional capacities, such as the ability to stand up and sit down from a chair, climb stairs and walk quickly, may be more closely associated with power than strength, and the loss of power7–9 may be more related to the etiology of falls10, 11. Interestingly, a study of Kwon et al.12 also showed that lower extremity muscle strength is strongly associated with gait speed and, from the opposite perspective, maximum walking speed is associated with knee strength13. In fact, the distal leg muscles, such as ankle muscles, are important for walking14, maintaining balance and avoiding falls15.
Functional evaluation then acquires increasing importance. The adoption of reliable testing techniques with precise instruments is also essential to define disability cut-off scores and, at the same time, to avoid inaccuracies in strength and power evaluations for the lower limbs. One type of assessment tool, largely used in the last few years, is the isokinetic dynamometer. It works providing a movement with defined velocity accommodating the resistance (of the examined joint) during a range of motion (ROM). This type of muscle contraction has become very common in the assessment of a large variety of types of muscle strength, useful in both research setting and clinical practice. One example is to assess ratios of quadriceps and hamstring muscle torques; where unbalanced ratios can increase injury frequency16. Other uses are consolidated to represent dynamic muscle function and are basis for pre-season screenings, return to play decisions, treatment efficacy and insurance reimbursement17. Last but not least, isokinetic devices are commonly used as therapeutic (and testing) exercise such as in patients with knee osteoarthritis18 or for knee rehabilitation after surgery for the anterior cruciate ligament reconstruction19.
Therefore, the aim of this investigation is to assess the test-retest reliability of a knee and ankle isokinetic and isometric strength testing protocols using a new and untested multi-joint system dynamometer in a sample of older healthy adults.
Material and methods
Participants
Sixteen male and fourteen female older adults recruited from cultural associations in Padova (IT) agreed to participate in the study. Sample size was consistent with those reported in other investigations examining dynamometer measures in older adults11,20. Inclusion criteria were: age ≥ 60 years old, apparently healthy conditions and MMSE ≥ 26. Participants were excluded from the investigation if they had history of cardiovascular, pulmonary, neurologic, musculoskeletal, or other major systemic problems that can negatively influence study results. Moreover, all older adults had no previous experience with isometric or isokinetic muscular test, thus before testing a familiarization trial was performed to limit bias. Each participant was informed about the experimental purpose and procedures, and gave written consent for their participation in the trial accordingly with Declaration of Helsinki and following specific guideline for researchers operating in the interdisciplinary field of exercise and sports sciences21. In addition, participants were administered the Mini-Mental State Examination (MMSE)22, that was used as a screening device to rule out significant cognitive impairments23. All procedures were approved by the Ethics Committee of the University of Padova (IT).
Device
The multi-joint evaluation system (Prima Plus, Easytech, Italy) is composed by a sit and a mechanic unit. Dimensions are 70 × 140 × 135 cm with an overall weight of 193 kg. The system measures knee flexion and extension, dorsal and plantar flexion of the ankle, intra- and extra-rotation of the shoulder. The device is conformed to the EU standards for the safety (directive 93/42 CEE). Certificate No. 114091-2012-CE-ITA-NA attests the quality for design, production and final product inspection/testing. The calibration of the dynamometer is checked applying a known weight in specific points of the lever (distance from fulcrum to the point which the force is exerted) (Fig. 1). Each calibration sampling is repeated three times in different angles (15 angle measures, randomly). Largest error during isokinetic testing is 0.6 Nm (0.23%).
Figure 1.
Calibration process, D is the distance between fulcrum and Force (F) exerted to the lever.
Procedure
The same randomized test procedure was performed on 2 separate occasions (test, retest), 7 days apart, by the same two investigators. This time period between test and retest was used in previous studies assessing the reliability of isokinetic parameters24. Testing sessions were conducted using the same shoes, in the same weekday and the same time of the day (from 2 to 4 p.m.), in order to reduce possible bias and the potential effect of physical activities and diurnal variation. Before testing, a warm up was performed to reduce the risk of injuries. A 60-second recovery period was allowed between all testing procedures.
Subjects were seated on the multi-joint evaluation system with the backrest angled at 90° to the seat. Belts were placed across the thighs, the pelvis, and the shoulders to minimize body movements and to optimally isolate the movement of knee joints and ankles. Subjects folded their arms across their chest and were not permitted to hold on to the equipment during the tests. The assessed parameters were: maximal isometric bilateral knee extension at 75° of extension, maximal isokinetic bilateral knee extension and flexion with a range of movement between 0° (anatomic 0°) to 85° of knee flexion, right and left maximal isometric ankle plantar and dorsal flexor at 30° of plantar flexion and right and left maximal isokinetic ankle plantar and dorsal flexor with a range of movement between 0° (anatomic 0°) to 65° of ankle plantar flexion.
During knee trials the lever fulcrum was aligned with the rotation axis of knee, with the lateral femoral epicondyle used as landmark, and the shin pad was placed 2 cm above the medial malleoli. Instead, during the ankle trials, the lever fulcrum was aligned with the medial malleoli. The lengths of the lever arm were recorded and used in the retest trials to avoid position bias. Before all isokinetic tests, the weight of the legs and the ankles were noted and a gravity adjustment was made using the computer software.
Four measures were quantified: maximal isometric bilateral knee extension, maximal isokinetic bilateral knee extension and flexion, maximal isometric ankle plantar and dorsal flexion (right and left ankles), maximal isokinetic ankle plantar and dorsal flexion (right and left ankles). During the maximal isometric bilateral knee extension, the leaver arm was set at 75° extension, calculated on the maximum knee extension of each participant. Subjects had to push as stronger as possible, with both legs, the shin pad for 5 seconds. Differently, during maximal isokinetic bilateral knee extension and flexion participants pushed and pulled the shin pad as fast as possible for five times uninterruptedly. The velocity of isokinetic movement was set at 90°/sec. When testing the maximal isometric ankle plantar and dorsal flexion, the lever arm was set at 30° of plantar flexion, calculated from the maximum ankle dorsal flexion (0°) of each participant, and the foot was fixed on a support with two stripes. Subjects had to push down and pull up the ankle support as stronger as possible for 5 seconds, during extension and flexion trials. Finally, during maximal isokinetic ankle plantar flexion and extension participants had to push down and pull up the ankle support as fast as possible for five times continuously. The velocity of this isokinetic movement was set at 90°/sec.
Data analysis
Data were acquired at 1000 Hz. All testing procedures were performed three times and for each one the maximum torque produced (in newton-meters) was recorded. For the analysis, the average of three trials was taken into consideration. With the same procedure, also the mean of average power was calculated. Statistical analyses were conducted using SPSS (Version 22.0 for Windows, SPSS Inc., Chicago, IL) and Microsoft Excel 2016. The Kolmogorov-Smirnoff (K-S) test was performed to check if data were normally distributed. Means and standard deviations were calculated for each variable in both test and retest conditions. Bland and Altman plots25 were created in order to examine test-retest reliability; limits of agreement (mean of the differences ± 1.96 × SD) were also reported in the plots. Paired-sample t-tests were performed to detect significant bias between test sessions (p<0.05). Moreover, Intraclass Correlations Coefficients (ICC), 95% Lower and 95% Upper Confidential Limits were calculated. Finally, differences between the mean values were also expressed as a percentage in order to allow comparisons among measures and across studies.
Results
Characteristics of the sample are reported in Table I. The average age for women was 65.15 ± 5.29 years, body mass was 63.46 ± 11.06 kg, height was 1.63 ± 0.05 meters, and BMI 23.68 ± 3.02. Whereas the average age for man was 65.38 ± 4.13, body mass was 76.13 ± 9.33, height was 1.77 ± 0.04, and BMI 24.3 ± 2.56. All participants concluded the trial safety and no subject reported any discomfort throughout the overall assessment.
Table I.
Participant characteristics.
| N. Subjects | Weight (kg) | Height (m) | BMI (kg/m2) | Age (years) |
|---|---|---|---|---|
| 30 (16 M, 14 F) | 69.93 ± 11.99 | 1.70 ± 0.86 | 23.97 ± 2.78 | 65.2 ± 4.66 |
Abbreviation: BMI, body mass index.
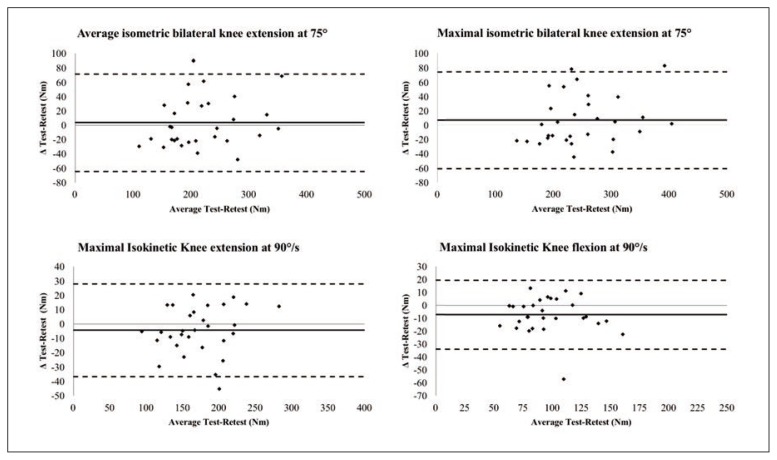
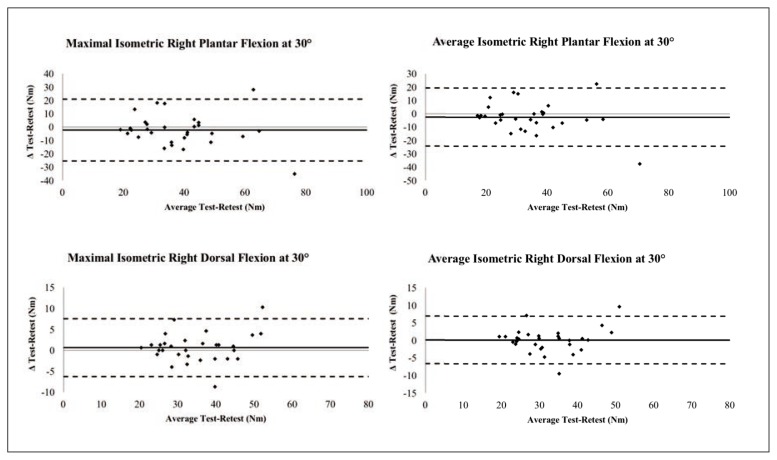
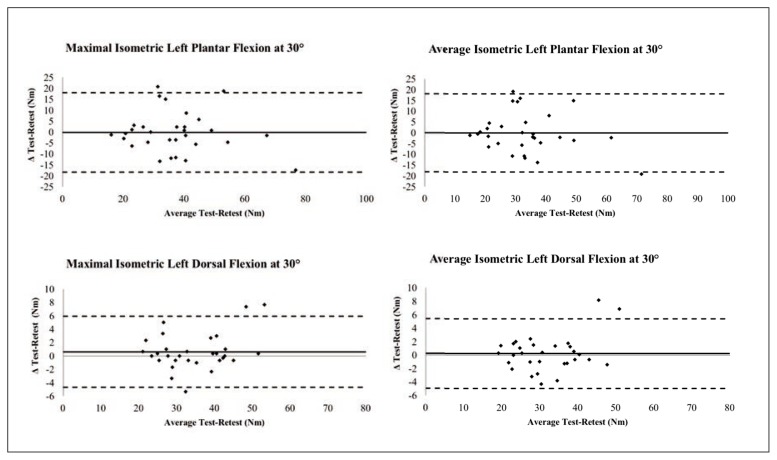
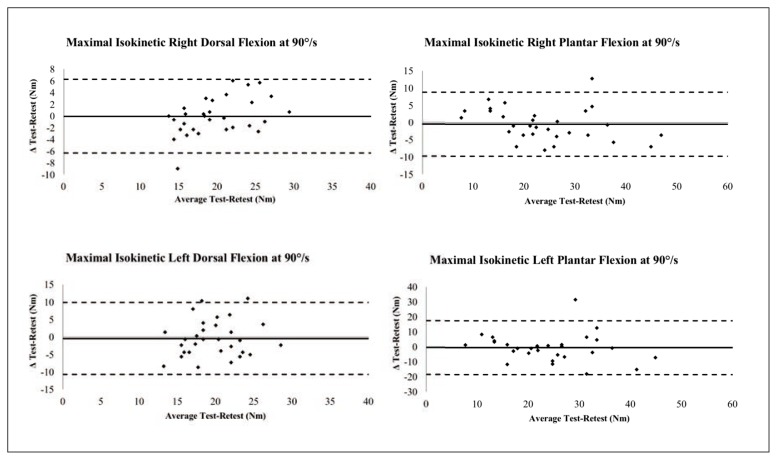
Coefficients of correlation between measures were calculated showing moderate to strong effects among all test-retest assessments while Bland and Altman analyses were performed to detect mean error scores between test and retest measures. Separate analyses for each measure were displayed in Figures 2–5. The mean errors (average errors between estimated points) were calculated as deviation from 0 Nm. Mean errors are 6.82 Nm in the maximal isometric bilateral knee extension at 75°, 3.5 Nm for average isometric bilateral knee extension at 75°, −4.39 Nm in the maximal isokinetic knee extension at 90°/s, −7.1 Nm in the maximal isokinetic knee flexion at 90°/s, −2.33 Nm in the maximal isometric right plantar flexion at 30°, −2.5 Nm for average isometric right plantar flexion at 30°, 0.67 Nm for maximal isometric right dorsal flexion at 30°, 0.16 Nm for average isometric right dorsal flexion at 30°, −0.23 Nm for maximal isometric left plantar flexion at 30°, −0.11 Nm for average isometric right plantar flexion at 30°, 0.62 Nm for maximal isometric left dorsal flexion at 30°, 0.24 Nm for average isometric left dorsal flexion at 30°, −0.04 Nm for maximal isokinetic right dorsal flexion at 90°/s, −0.5 Nm for maximal isokinetic right plantar flexion at 90°/s, −0.42 Nm for maximal isokinetic left dorsal flexion at 90°/s and −0.5 Nm for maximal isokinetic left plantar flexion at 90°/s. Upper and lower limits of agreement were represented in Figures 2–5 with dashed lines. For each test (maximal isometric bilateral knee extension, maximal isokinetic bilateral knee extension and flexion, right and left maximal isokinetic and isometric ankle plantar and dorsal flexion), results showed that most values were included within the upper and lower limits of agreement. The examination of the plots indicates that during maximal isokinetic right and left dorsal flexion at 90°/s (Fig. 5), a tighter distribution was observed when compared with the maximal isokinetic right and left plantar flexion at 90°/s (Fig. 5). The most accurate measure was detected in the maximal isometric left plantar flexion at 30° test (Fig. 4), while the worst was in the maximal isometric right plantar flexion at 30° test (Fig. 3). Pair-sample analysis showed only one significant difference (p<0.05) in the maximal isokinetic bilateral knee flexion, indicating a test-retest discrepancy only in this specific measure (Tab. II).
Figure 2.
Bland and Altman plots reproducing average isometric bilateral knee extension at 75°, maximal isometric bilateral knee extension at 75°, maximal isokinetic knee extension at 90°/s and maximal isokinetic knee flexion at 90°/s.
Figure 3.
Bland and Altman plots reproducing maximal isometric right plantar flexion at 30°, average isometric right plantar flexion at 30°, maximal isometric right dorsal flexion at 30° and average isometric right dorsal flexion at 30°.
Figure 4.
Bland and Altman plots reproducing maximal isometric left plantar flexion at 30°, average isometric left plantar flexion at 30°, maximal isometric left dorsal flexion at 30° and average isometric left dorsal flexion at 30°.
Figure 5.
Bland and Altman plots reproducing maximal isokinetic right dorsal flexion at 90°/s, maximal isokinetic right plantar flexion at 90°/s, maximal isokinetic left dorsal flexion at 90°/s and maximal isokinetic left plantar flexion at 90°/s.
Table II.
Means and standard deviations for isometric and isokinetic tests.
| Test (Nm) | Retest (Nm) | p value | Ø % | ICC | LCL 95% | UCL95% | |
|---|---|---|---|---|---|---|---|
| Isometric Knee Extension | |||||||
| Highesta | 251.61 ± 73.30 | 244.79 ± 65.50 | 0.286 | −2.71% | 0.88 | 0.77 | 0.94 |
| Averageb | 220.52 ± 69.73 | 217.03 ± 62.46 | 0.586 | −1.59% | 0.87 | 0.75 | 0.94 |
| Isokinetic Knee at 90°/s | |||||||
| Extension | 170.16 ± 44.11 | 174.55 ± 41.38 | 0.154 | 2.58% | 0.93 | 0.88 | 0.96 |
| Flexion | 92.42 ± 26.50 | 99.52 ± 28.21 | 0.007* | 7.68% | 0.88 | 0.77 | 0.94 |
| Isometric Ankle R Flexion (pl.) | |||||||
| Highesta | 37.07 ± 13.91 | 39.3 ± 16.29 | 0.307 | 6.03% | 0.71 | 0.48 | 0.85 |
| Averageb | 32.60 ±12.58 | 35.10 ± 15.5 | 0.224 | 7.69% | 0.71 | 0.47 | 0.85 |
| Isometric Ankle R Flexion (do.) | |||||||
| Highesta | 35.09 ± 9.41 | 34.42 ± 8.81 | 0.307 | −1.90% | 0.93 | 0.86 | 0.97 |
| Averageb | 32.43 ± 8.88 | 32.26 ± 8.27 | 0.797 | −0.51% | 0.92 | 0.84 | 0.96 |
| Isometric Ankle L Flexion (pl.) | |||||||
| Highesta | 36.94 ± 13.60 | 37.17 ± 14.90 | 0.891 | 0.63% | 0.80 | 0.62 | 0.90 |
| Averageb | 33.09 ± 12.45 | 33.19 ± 14.37 | 0.949 | 0.32% | 0.78 | 0.58 | 0.89 |
| Isometric Ankle L Flexion (do.) | |||||||
| Highesta | 35 ± 9.39 | 34.38 ± 8.64 | 0.218 | −1.78% | 0.96 | 0.91 | 0.98 |
| Averageb | 32.02 ± 9.03 | 31.78 ± 8.25 | 0.619 | −0.75% | 0.96 | 0.91 | 0.98 |
| Isokinetic Ankle R at 90°/s | |||||||
| Flexion (pl.) | 23.83 ± 9.39 | 24.33 ± 10.73 | 0.565 | 2.10% | 0.90 | 0.80 | 0.95 |
| Flexion (do.) | 19.82 ± 5.26 | 19.87 ± 3.92 | 0.939 | 0.22% | 0.77 | 0.58 | 0.89 |
| Isokinetic Ankle L at 90°/s | |||||||
| Flexion (pl.) | 23.83 ± 9.39 | 24.33 ± 10.73 | 0.767 | 2.10% | 0.60 | 0.31 | 0.79 |
| Flexion (do.) | 19.48 ± 4.84 | 19.9 ± 4.30 | 0.661 | 2.17% | 0.36 | 0.01 | 0.63 |
Abbreviation: ICC, Intraclass Correlation Coefficient; LCL, lower confidential limit; UCL, upper confidential limit;
Highest value of 3 testing procedures;
Average value of 3 testing procedures; R, right; L, left;
, p < 0.05;
pl., plantar; do., dorsal.
Discussion
This study was conducted to establish the test-retest reliability of knee and ankle isokinetic and isometric strength measures using a new and untested multi-joint evaluation system (Prima Plus, Easytech, Italy). Participants involved in our study showed different activity level varying from sedentary to a regular active lifestyle, representing a heterogeneous group and with a wide range of strength values. Moreover, the sample size was larger than previous studies analyzing reliability of isometric and isokinetic leg extension26 and flexion16. To minimize errors, this procedure was standardized and randomized. Participants’ position was recorded and the same instructions were specified. No verbal encouragements were given and subjects were asked to wear the same shoes and comfortable clothes.
In summary, results revealed a high reliability in: isometric knee extension, isokinetic knee extension at 90°/s, isometric right and left ankle plantar and dorsal flexion, and isokinetic right ankle plantar and dorsal flexion at 90°/s. Specifically, the prevalence of values is placed within the limits of agreements and the correspondence between test and retest differences confirmed the reproducibility of the assessments performed with the multi-joint evaluation system. With more detail, a very high correlation was observed between the values reached for isometric left (ICC = 0.96) and right (ICC = 0.93) ankle dorsal flexion; this is probably due to the movement reproducing a daily activity such as stand-up from a chair or start the stance phase during locomotion. Contrarily, the lowest correlation was found on left ankle isokinetic dorsal flexion test (ICC = 0.36) and left ankle isokinetic plantar flexion test (ICC = 0.60), despite the mean values were similar to those of the right ankle isokinetic test. This could be explained in terms of dominance; in fact, the vast majority of the participants was right handed and the dominant leg was the right.
Our results demonstrated from good to excellent inter-rater agreement measures, with the exclusion of the isokinetic ankle left dorsal flexion, and the percentage differences between test and retest measures were similar to previous studies involving older subjects11, 27. The only statistically significant difference (Δ % = 7.68%) was found in the isokinetic bilateral knee flexion test (p = 0.007). This discrepancy may be due to the result of a learning effect. This effect was explained by Connely et al.28 showing that, especially for older people, once learned a specific motor task (in this case the isokinetic), the second performance can result as enhanced without any real increase of strength and power by the same subject. Following this reasoning, it is possible that a learning effect influenced this specific trial specifically; hamstring muscles were exerted in a non-traditional way and then mirroring an increase of the values during the retest session. Additionally, in the Hartmann et al. study27, participants affirmed that the movement toward gravity was more difficult to be performed than against gravity, and isokinetic bilateral knee flexion of our test is toward gravity indeed.
From a clinical standpoint, as comparison with our data, we extract data from Ruhdorfer et al.29 and Ribeiro et al.30. In the first study, the relationship between thigh muscle strength and clinically relevant differences in self-assessed lower limb function was estimated, while in the second investigation test-retest reliability of lower limb isokinetic endurance in COPD patients was taken in examination. Averagely, both studies described a threshold of about 6%29 and 10%30 respectively to determine a minimally clinical relevant change. It has to be considered that our data reflected a performance in a healthy population; however, the magnitude of error in the system showed a range concretely inferior to the minimal clinically relevant differences detected in these investigations.
A first limitation we recognize in our study was the use of only one isokinetic testing velocity (90°/sec), which was chosen to help non-expert participants to facilitate testing sessions. Probably the average and the highest peak torque could be reached using a lower velocity. A further limitation is the non-specificity of the tests for the knee that does not reproduce completely an everyday activity although it is well accepted that leg extensor power is associated with walking speed and rising up from a chair31.
Conclusion
Within the limitations of this study, data indicated that the multi-joint evaluation system for the assessment of knee and ankle isokinetic and isometric strength provided reliable test-retest measures in healthy older adults. Future investigations should consider the variety of tests that can be administered with this device; further directions could involve either athletes and patients, using different isokinetic velocities, for instance 60°/sec, rather than different angles of extension for isometric tests. Lastly, no study has so far evaluated data using the eccentric modality of this specific dynamometer; we preferred to test only isokinetic and isometric modalities since the testing sample was composed of older adults that seemed to have a lower eccentric knee extension torque compared to young adults32.
Footnotes
Conflict of interest
No relationships/conditions/circumstances present potential conflict of interest.
References
- 1.Kowal P, Chatterji S, Naidoo N, Biritwum R, Fan W, Lopez Ridaura R, et al. Data resource profile: the World Health Organization Study on global AGEing and adult health (SAGE) Int J Epidemiol. 2012;41(6):1639–1649. doi: 10.1093/ije/dys210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reid KF, Pasha E, Doros G, Clark DJ, Patten C, Phillips EM, et al. Longitudinal decline of lower extremity muscle power in healthy and mobility-limited older adults: influence of muscle mass, strength, composition, neuromuscular activation and single fiber contractile properties. Eur J Appl Physiol. 2014;114(1):29–39. doi: 10.1007/s00421-013-2728-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keller K, Engelhardt M. Strength and muscle mass loss with aging process. Age and strength loss. Muscles Ligaments Tendons J. 2013;3(4):346–350. [PMC free article] [PubMed] [Google Scholar]
- 4.Walston JD. Sarcopenia in older adults. Curr Opin Rheumatol. 2012;24(6):623–627. doi: 10.1097/BOR.0b013e328358d59b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roubenoff R. Sarcopenia: effects on body composition and function. J Gerontol A Biol Sci Med Sci. 2003;58(11):1012–1017. doi: 10.1093/gerona/58.11.m1012. [DOI] [PubMed] [Google Scholar]
- 6.Trombetti A, Reid KF, Hars M, Herrmann FR, Pasha E, Phillips EM, et al. Age-associated declines in muscle mass, strength, power, and physical performance: impact on fear of falling and quality of life. Osteoporos Int. 2016;27(2):463–471. doi: 10.1007/s00198-015-3236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Suzuki T, Bean JF, Fielding RA. Muscle power of the ankle flexors predicts functional performance in community-dwelling older women. J Am Geriatr Soc. 2001;49(9):1161–1167. doi: 10.1046/j.1532-5415.2001.49232.x. [DOI] [PubMed] [Google Scholar]
- 8.Bean JF, Leveille SG, Kiely DK, Bandinelli S, Guralnik JM, Ferrucci L. A comparison of leg power and leg strength within the InCHIANTI study: which influences mobility more? J Gerontol A Biol Sci Med Sci. 2003;58(8):728–733. doi: 10.1093/gerona/58.8.m728. [DOI] [PubMed] [Google Scholar]
- 9.Bean JF, Kiely DK, Herman S, Leveille SG, Mizer K, Frontera WR, et al. The relationship between leg power and physical performance in mobility-limited older people. J Am Geriatr Soc. 2002;50(3):461–467. doi: 10.1046/j.1532-5415.2002.50111.x. [DOI] [PubMed] [Google Scholar]
- 10.Skelton DA, Kennedy J, Rutherford OM. Explosive power and asymmetry in leg muscle function in frequent fallers and non-fallers aged over 65. Age Ageing. 2002;31(2):119–125. doi: 10.1093/ageing/31.2.119. [DOI] [PubMed] [Google Scholar]
- 11.Webber SC, Porter MM. Reliability of ankle isometric, isotonic, and isokinetic strength and power testing in older women. Phys Ther. 2010;90(8):1165–1175. doi: 10.2522/ptj.20090394. [DOI] [PubMed] [Google Scholar]
- 12.Kwon IS, Oldaker S, Schrager M, Talbot LA, Fozard JL, Metter EJ. Relationship between muscle strength and the time taken to complete a standardized walk-turn-walk test. J Gerontol A Biol Sci Med Sci. 2001;56(9):B398–404. doi: 10.1093/gerona/56.9.b398. [DOI] [PubMed] [Google Scholar]
- 13.Ko SU, Stenholm S, Metter EJ, Ferrucci L. Age-associated gait patterns and the role of lower extremity strength - results from the Baltimore Longitudinal Study of Aging. Arch Gerontol Geriatr. 2012;55(2):474–479. doi: 10.1016/j.archger.2012.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McGibbon CA, Krebs DE. Effects of age and functional limitation on leg joint power and work during stance phase of gait. J Rehabil Res Dev. 1999;36(3):173–182. [PubMed] [Google Scholar]
- 15.Cattagni T, Scaglioni G, Laroche D, Van Hoecke J, Gremeaux V, Martin A. Ankle muscle strength discriminates fallers from non-fallers. Front Aging Neurosci. 2014;6:336. doi: 10.3389/fnagi.2014.00336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sole G, Hamren J, Milosavljevic S, Nicholson H, Sullivan SJ. Test-retest reliability of isokinetic knee extension and flexion. Arch Phys Med Rehabil. 2007;88(5):626–631. doi: 10.1016/j.apmr.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 17.Drouin JM, Valovich-mcLeod TC, Shultz SJ, Gansneder BM, Perrin DH. Reliability and validity of the Biodex system 3 pro isokinetic dynamometer velocity, torque and position measurements. Eur J Appl Physiol. 2004;91(1):22–29. doi: 10.1007/s00421-003-0933-0. [DOI] [PubMed] [Google Scholar]
- 18.Huang MH, Lin YS, Yang RC, Lee CL. A comparison of various therapeutic exercises on the functional status of patients with knee osteoarthritis. Semin Arthritis Rheum. 2003;32(6):398–406. doi: 10.1053/sarh.2003.50021. [DOI] [PubMed] [Google Scholar]
- 19.Van Grinsven S, van Cingel RE, Holla CJ, van Loon CJ. Evidence-based rehabilitation following anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2010;18(8):1128–1144. doi: 10.1007/s00167-009-1027-2. [DOI] [PubMed] [Google Scholar]
- 20.Symons TB, Vandervoort AA, Rice CL, Overend TJ, Marsh GD. Reliability of isokinetic and isometric knee-extensor force in older women. J Aging Phys Act. 2004;12(4):525–537. doi: 10.1123/japa.12.4.525. [DOI] [PubMed] [Google Scholar]
- 21.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal - Basic principles and recommendations in clinical and field science research: 2016 update. MLTJ. 2016;6(1):1–5. doi: 10.11138/mltj/2016.6.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 23.Tombaugh TN, McIntyre NJ. The mini-mental state examination: a comprehensive review. J Am Geriatr Soc. 1992;40(9):922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 24.Larsson B, Karlsson S, Eriksson M, Gerdle B. Test-retest reliability of EMG and peak torque during repetitive maximum concentric knee extensions. J Electromyogr Kinesiol. 2003;13(3):281–287. doi: 10.1016/s1050-6411(03)00022-1. [DOI] [PubMed] [Google Scholar]
- 25.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–310. [PubMed] [Google Scholar]
- 26.Jenkins ND, Buckner SL, Bergstrom HC, Cochrane KC, Goldsmith JA, Housh TJ, et al. Reliability and relationships among handgrip strength, leg extensor strength and power, and balance in older men. Exp Gerontol. 2014;58:47–50. doi: 10.1016/j.exger.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 27.Hartmann A, Knols R, Murer K, de Bruin ED. Reproducibility of an isokinetic strength-testing protocol of the knee and ankle in older adults. Gerontology. 2009;55(3):259–268. doi: 10.1159/000172832. [DOI] [PubMed] [Google Scholar]
- 28.Connelly DM, Carnahan H, Vandervoort AA. Motor skill learning of concentric and eccentric isokinetic movements in older adults. Exp Aging Res. 2000;26(3):209–228. doi: 10.1080/036107300404868. [DOI] [PubMed] [Google Scholar]
- 29.Ruhdorfer A, Wirth W, Eckstein F. Relationship between isometric thigh muscle strength and minimum clinically important differences in knee function in osteoarthritis: data from the osteoarthritis initiative. Arthritis Care Res (Hoboken) 2015;67(4):509–518. doi: 10.1002/acr.22488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ribeiro F, Lepine PA, Garceau-Bolduc C, Coats V, Allard E, Maltais F, et al. Test-retest reliability of lower limb isokinetic endurance in COPD: A comparison of angular velocities. Int J Chron Obstruct Pulmon Dis. 2015;10:1163–1172. doi: 10.2147/COPD.S81806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bassey EJ, Fiatarone MA, O’Neill EF, Kelly M, Evans WJ, Lipsitz LA. Leg extensor power and functional performance in very old men and women. Clin Sci (Lond) 1992;82(3):321–327. doi: 10.1042/cs0820321. [DOI] [PubMed] [Google Scholar]
- 32.Melo RC, Takahashi AC, Quiterio RJ, Salvini TF, Catai AM. Eccentric Torque-Producing Capacity is Influenced by Muscle Length in Older Healthy Adults. J Strength Cond Res. 2016;30(1):259–266. doi: 10.1519/JSC.0000000000001047. [DOI] [PubMed] [Google Scholar]