Summary
Background
Achilles tendon ruptures may lead to proximal retraction of the stump if not treated acutely, increasing the chances of poorer functional outcomes. The flexor halluces longus transfer is a well-established treatment option, usually performed as an open procedure. The aim of this paper is to report the preliminary results and describe the technique of endoscopic flexor halluces longus transfer.
Material and methods
Six patients with chronic Achilles tendon injuries or re-ruptures were treated with endoscopic FHL transfer. The Achilles Tendon Rupture Score was used to clinically evaluate the patients. Single leg heel rise ability, functional hallux weakness, complications and procedure length were also checked.
Results
On average, we took 56 minutes to perform the surgery. All patients had a major increase in the ATRS score value postoperatively. Single leg heel rise was possible for all patients without limitation. None of the patients noticed functional weakness of the hallux during daily life activity and no wound or soft tissue complications were seen.
Conclusion
Endoscopic FLH transfer is a reliable option for patients with high skin risk and soft tissue complications. Other studies are needed to compare this technique with the open procedure, gold standard by now, to ensure its safety and efficacy.
Level of evidence
4.
Keywords: Achilles tendon rupture, flexor halluces longus transfer, endoscopy, Achilles tendon re-rupture, minimally invasive surgery
Introduction
A chronic degenerated Achilles Tendon (AT) is expected in a chronic rupture and on neglected injuries. This could compromise the reparability capacity of the tendon and predispose to a muscle insufficiency of the gastroc-soleous complex1.
The management of acute and chronic AT ruptures is usually different due to the retraction and atrophy of the proximal stump and remaining gap between the proximal and distal stumps in the chronic setting. Moreover, the outcomes after chronic AT rupture or re-rupture treatment can be influenced by the time of injury, skin conditions, muscle contraction, muscle excursion and patient comorbidities2,3.
Many procedures have been described to treat this condition, such as the gastroc-soleus complex V-Y myotendinous lengthening or a reinforcing flap from proximal AT4. Other surgical techniques use the peroneus brevis (PB), flexor digitorum longus (FDL) or flexor hallucis longus (FHL) tendon transfers4–6. All these surgical procedures have been shown to yield satisfactory clinical results, although ankle plantar flexion strength and peak torque deficits can persist3–5,7. These techniques require open incisions, making skin problems or other local complications a serious concern.
The purpose of this study is to report the technique and present the preliminary results of six patients submitted to an endoscopic FHL transfer to treat chronic AT ruptures.
Material and methods
From June 2015 to February 2016, six patients with Achilles tendon chronic injuries or re-ruptures were treated with endoscopic FHL transfer. Chronic injuries were considered those with more than 6 weeks8. All lesions were at the AT zone 2 (2–6 cm proximal to its insertion).
One patient suffered a re-rupture in an acute injury and all other five were chronic injuries. They all presented loss of the physiologic equinus of the foot when positioned in prone position, difficulty walking and were not able to perform the single leg heel rise test. All patients were submitted to pre-operatory Magnetic Resonance to access tendon degeneration at the stumps level. Minimum follow-up was 5 months. Patients that presented with a persistent palpable gap with maximum plantar flexion were treated with the addition of the Percutaneous Achilles Repair System (PARS® - Arthrex, Naples).
All patients were evaluated and operated by the same fully trained foot and ankle surgeon. The Achilles Tendon Total Rupture Score (ATRS) was applied pre and postoperatively (at three months follow-up) in all patients9. Single leg heel rise and hallux strength were assessed at the post-operative period subjectively.
All patients signed an informed consent to be included in this study. Our local ethics committee has approved this work in accordance with previous described ethical requirements10.
Surgical Technique
Under sedation and peripheral block, patients were positioned in prone position with a tourniquet on the thigh inflated to 280 mmHg.
The posterior ankle endoscopy was performed with a 30° and 4.0 mm optic. The standard posterolateral and posteromedial portals, as described by van Dijk11, were used (Fig. 1). After debridement with shaver, the FHL tendon was identified (Fig. 2).
Figure 1.
Posterolateral and posteromedial portals for posterior ankle endoscopy
Figure 2.
FHL identification.
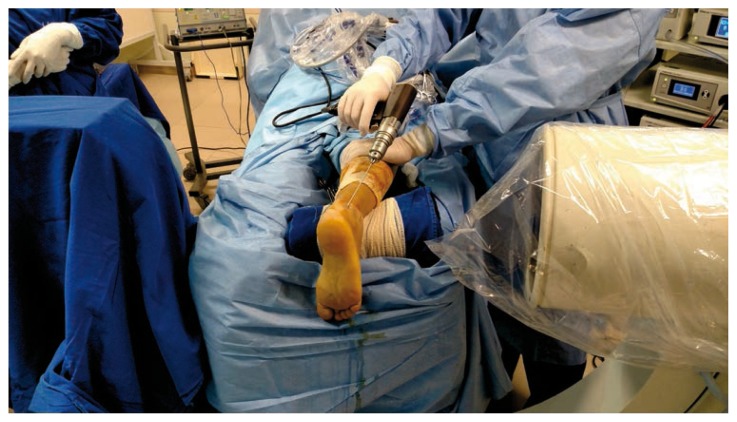
After proper identification of the FHL, the ankle and hallux were positioned at maximum plantar flexion. With an accessory clamp to pull proximally the tendon, we performed a tenotomy as distal as possible. (Fig. 3 a, b). The free FHL stump was externalized through the medial portal and a Krakow suture was applied using a nonabsorbable 2.0 fiber Wire® (Arthrex®, Naples) (Fig. 4). The tendon width was measured so we could drill the proper calcaneal tunnel.
Figure 3.
a. Ankle and hallux positioned in maximal plantar flexion, seeking the maximum tendon length; b. FHL proximal traction.
Figure 4.
Tendon stump externalized through de posteromedial portal.
The calcaneal tunnel was performed under endoscopy and fluoroscopy visualization through the posterolateral portal (Fig. 5). The tunnel was 30 mm deep and 0.5 mm wider than the tendon. The FHL was pulled out through the tunnel and externalized on the plantar surface of the hindfoot using the guide wire. At this moment, the ankle was maintained in 5 to 10° of plantar flexion (physiological equinus) while the proper tension on FHL was stablished pushing the fiber wire. After checking the correct tension endoscopically, the FHL tendon was fixed with a metallic interference screw with the same tunnel width (7×25mm) (Fig. 6A–B). After that, the ankle was positioned in maximum plantar flexion, observing by palpation if there was any gap between the tendon stumps. If present, the tendon gap was sutured using the PARS® (Arthrex, Naples) technique to approximate the Achilles tendon stumps.
Figure 5.
Calcaneal tunnel performed under endoscopy and radioscopic visualization through the posterolateral portal.
Figure 6.
A. Introduction of the interference screw; B. Endoscopic view of the tunnel after fixation.
A cast with the foot in 10° of plantar flexion was applied. All patients had the same postoperative protocol using plantar flexion cast immobilization for 2 weeks and then, a weight-bearing boot with progression to neutral position for the next 4 weeks.
Results
We evaluated all patients after an average follow-up of nine months (range, 5–12 months). Chronic ruptures ranged from 6 to 36 weeks after injury. Four males and two females, and four left and two right sides were included. Patients were 50 years old on average (33–65 years). Three patients had an associate procedure (PARS® - Arthrex, Naples) to repair the pre-existent gap (Tab. I).
Table I.
Patients submitted to the surgical procedure.
| Variables | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 |
|---|---|---|---|---|---|---|
| Gender | F | M | F | F | M | F |
| Age | 65 | 33 | 52 | 60 | 43 | 47 |
| Side | L | L | L | R | R | L |
| Time before treatment | 4 months | No delayed | 6 months | 7 months | 6 weeks | 2 months |
| Acute/chronic | Chronic | Acutererupture | Chronic | Chronic | Chronic | Chronic |
| Gap | Np | Palpable | Np | Palpable < 1 cm | Palpable >1 cm | Palpable |
| Degeneration | > 50% | No | > 50% | > 50% | > 50% | > 50% |
| Comorbities | Dm + tabagism | No | Local corticoid injection | Dm | Heavy tabagism | Wegner syndrome + corticoid |
| Follow up | 8 months | 1 year | 5 months | 11 months | 6 months | 1 year |
| Surgery time | 60 mim | 56 mim | 45 mim | 48 mim | 70 mim | 61 mim |
| Associate pars | No | Yes | No | No | Yes | Yes |
| ATRS pre | 83 | 87 | 82 | 79 | 85 | NC |
| ATRS post | 17 | 13 | 28 | 11 | 16 | NC |
NP - Not Palpable
NC - Not Collected/PARS - Percutaneous Achilles Repair System/ATRS - Achilles Tendon Total Rupture Score
All patients treated chronically had more than 50% of tendon degeneration. On average, we spent 56 minutes to perform the surgery, ranging from 45 to 70 minutes. No major or minor complications with regard to wound healing was noted. All patients had a major increase in the ATRS score values postoperatively, with an average of 17,8 (range from 11 to 28) preoperatively and 83,3 (range from 79 to 87) postoperatively.
Single leg heel raise was possible for all patients without limitation at the final follow-up. None of the patients noticed functional weakness of the hallux during daily life activity after the tendon transfer. One patient was athletic active and returned to play at 18 weeks. All other patients were sedentary.
Discussion
Chronic AT rupture can be treated with direct repair, AT advancement, tendon transfers or reconstructions with autograft, allograft, or synthetic material4,12–14. The best surgical management modality for the chronic AT rupture remains undetermined5. The size of the gap after debridement of the tendon ends has to be considered before choosing the surgical technique11–13. PB and FHL are the two most common transfered tendon, with similar mechanical properties3, 6, 15. The first usually results in diminished strength of eversion, but has good rates of return to pre-injury sport and daily activities with minimally invasive techniques16.
The FHL transfer to the calcaneus is traditionally performed through one or two long incision with extensive soft tissue dissection. Open surgery with a longitudinal incision can strip the peritendon, which is responsible for the blood supply to the damaged tendon. Wound complication rates among patients treated operatively are about 2,5 to 4%. Some Authors report an overall complication of 36% for open procedure and 10% for percutaneous repair5, 7, 17.
Endoscopic techniques allow direct visualization of the tendon ends without any additional incisions and a FHL tenotomy proximal to the knot of Henry, transferring it to the calcaneus in a minimally invasive way. We report in this study lower morbidity and postoperative complications compared to those reported for open procedures12, 18. We consider this technic a valuable option for patients with high risk for skin and soft tissue complications.
This study reports our experience and the technique of an endoscopic FHL transfer performed in six AT chronic ruptures or re-ruptures with a 9-month average follow-up. Functional outcome improved significantly with the mean ATRS of 17,8 preoperatively increasing to 83,3 postoperatively (at last follow-up). In our series, none of the patients reported functional weakness of the hallux during athletic or daily life activity.
Although we did not experienced complications in our case series, it is well known that this procedure is technically demanding, requires high level arthroscopic experience and is associated with potential complications as fixation failure and neurovascular bundle lesion11, 12. This approach needs further comparative studies with the open procedure.
Footnotes
Conflict of Interest
Caio Nery has received Consultor and Speaker honorarium from Arthrex. All the other Authors declare they have no conflict of interest.
References
- 1.Cretnik A, Frank A. Incidence and outcome of rupture of the Achilles tendon. Wiener klinische Wochenschrift. 2004;116(Suppl2):33–38. [PubMed] [Google Scholar]
- 2.Elias I, Besser M, Nazarian LN, Raikin SM. Reconstruction for missed or neglected Achilles tendon rupture with V-Y lengthening and flexor hallucis longus tendon transfer through one incision. Foot Ankle Int. 2007;28(12):1238–1248. doi: 10.3113/fai.2007.1238. [DOI] [PubMed] [Google Scholar]
- 3.Hahn F, Meyer P, Maiwald C, Zanetti M, Vienne P. Treatment of chronic achilles tendinopathy and ruptures with flexor hallucis tendon transfer: clinical outcome and MRI findings. Foot Ankle Int. 2008;29(8):794–802. doi: 10.3113/fai.2008.0794. [DOI] [PubMed] [Google Scholar]
- 4.Gabel S, Manoli A., 2nd Neglected rupture of the Achilles tendon. Foot Ankle Int. 1994;15(9):512–517. doi: 10.1177/107110079401500912. [DOI] [PubMed] [Google Scholar]
- 5.Khan RJ, Fick D, Brammar TJ, Crawford J, Parker MJ. Interventions for treating acute Achilles tendon ruptures. Cochrane Database Syst Rev. 2004;(3):Cd003674. doi: 10.1002/14651858.CD003674.pub2. [DOI] [PubMed] [Google Scholar]
- 6.Wapner KL, Pavlock GS, Hecht PJ, Naselli F, Walther R. Repair of chronic Achilles tendon rupture with flexor hallucis longus tendon transfer. Foot & ankle. 1993;14(8):443–449. doi: 10.1177/107110079301400803. [DOI] [PubMed] [Google Scholar]
- 7.Dalton GP, Wapner KL, Hecht PJ. Complications of achilles and posterior tibial tendon surgeries. Clinical orthopaedics and related research. 2001;(391):133–139. doi: 10.1097/00003086-200110000-00014. [DOI] [PubMed] [Google Scholar]
- 8.Gabel S, Manoli A., 2nd Neglected rupture of the Achilles tendon. Foot Ankle Int. 1994;15:512–517. doi: 10.1177/107110079401500912. [DOI] [PubMed] [Google Scholar]
- 9.Zambelli R, Pinto RZ, Magalhaes JM, et al. Development of the Brazilian Portuguese version of the Achilles Tendon Total Rupture Score (ATRS BrP): a cross-cultural adaptation with reliability and construct validity evaluation. BMC sports science, medicine and rehabilitation. 2016;8:11. doi: 10.1186/s13102-016-0034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Padulo J, Oliva F, Frizziero A, Maffulli N. Muscles, Ligaments and Tendons Journal - Basic principles and recommendations in clinical and field science research: 2016 update. MLTJ. 2016;6(1):1–5. doi: 10.11138/mltj/2016.6.1.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Dijk CN. Hindfoot endoscopy. Foot and ankle clinics. 2006;11(2):391–414. vii. doi: 10.1016/j.fcl.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Lui TH, Chan WC, Maffulli N. Endoscopic Flexor Hallucis Longus Tendon Transfer for Chronic Achilles Tendon Rupture. Sports Med Arthrosc. 2016;24(1):38–41. doi: 10.1097/jsa.0000000000000086. [DOI] [PubMed] [Google Scholar]
- 13.Goncalves S, Caetano R, Corte-Real N. Salvage Flexor Hallucis Longus Transfer for a Failed Achilles Repair: Endoscopic Technique. Arthroscopy techniques. 2015;4(5):e411–416. doi: 10.1016/j.eats.2015.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]; DeMaio M, Paine R, Drez DJ., Jr Achilles tendonitis. Orthopedics. 1995;18(2):195–204. doi: 10.3928/0147-7447-19950201-20. [DOI] [PubMed] [Google Scholar]
- 14.Myerson MS. Achilles tendon ruptures. Instr Course Lect. 1999;48:219–230. [PubMed] [Google Scholar]
- 15.Sebastian H, Datta B, Maffulli N, Neil M, Walsh WR. Mechanical properties of reconstructed achilles tendon with transfer of peroneus brevis or flexor hallucis longus tendon. J Foot Ankle Surg. 2007;46:424–428. doi: 10.1053/j.jfas.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 16.Maffulli N, Oliva F, Costa V, Del Buono A. The management of chronic rupture of the Achilles tendon: minimally invasive peroneus brevistendon transfer. Bone Joint J. 2015 Mar;97- B(3):353–357. doi: 10.1302/0301-620X.97B3.33732. [DOI] [PubMed] [Google Scholar]
- 17.Neufeld SK, Farber DC. Tendon transfers in the treatment of Achilles’ tendon disorders. Foot and ankle clinics. 2014;19(1):73–86. doi: 10.1016/j.fcl.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 18.Schmidt-Rohlfing B, Graf J, Schneider U, Niethard FU. The blood supply of the Achilles tendon. Int Orthop. 1992;16(1):29–31. doi: 10.1007/BF00182980. [DOI] [PubMed] [Google Scholar]