Abstract
Background/Aim
The impact of traumatic dental injuries (TDI) in primary dentition on oral health-related quality of life indicates the need for the planning of prevention strategies. The aim of this study was to assess whether anthropometric characteristics in early life are associated with TDI by preschool age.
Materials and Methods
A birth cohort was recruited from the public healthcare system in the city of Porto Alegre, Brazil. Socio-demographic variables, type of birth, head circumference, weight and length were collected at birth (WHO standards). Head circumference, body mass index for age and height for age were collected at 12 months. TDI (Andreasen criteria) at three years of age (n = 458) were recorded by two examiners who had undergone training and calibration exercises. Multivariable analysis was carried out with Poisson regression with robust variance.
Results
A total of 31.0% of the children (142/458) exhibited TDI at three years of age. In the final model, the risk of TDI was 47% higher among children with a smaller head circumference upon birth and nearly 60% higher among those who were overweight/obese at 12 months of age (RR: 1.58; 95% CI: 1.15–2.17). The risk of TDI was also significantly higher among boys (RR 1.50; 95% CI: 1.13–2.00), but the outcome was not significantly associated with socioeconomic variables or other anthropometric variables.
Conclusion
The identification of overweight/obesity in the first year of life as a risk factor for TDI can contribute to the establishment of prevention strategies based on the common risk approach.
Keywords: Tooth injuries, risk factors, anthropometry, obesity, cohort studies
INTRODUCTION
The high prevalence of traumatic dental injury (TDI) in childhood and its impact on oral health-related quality of life indicate the need for the planning of prevention strategies.1,2 Such interventions should be based on the identification of risk factors for this outcome. To date, only accentuated overjet has been consistently recognized as a risk factor for TDI among preschool children,3,4 which at least partially explains the absence of TDI prevention protocols at the individual and collective levels.
TDI is an eminently physical event and factors that exert an influence on all steps of this process, such as postural balance, the force resulting from a fall, motor and mental disorders, all play a role in its etiology.5,6 Thus, it is plausible that anthropometric variables, especially those associated with balance, such as body mass, height and head circumference, may be associated with the occurrence of accidental trauma.7,8 A taller height in childhood was associated with a greater occurrence of bone fractures in a cohort form Dunedin; it is possible that taller children have less motor coordination and may be encouraged to participate in activities with older children of the same size, who have a better coordination and balance.9 However, in the only study to identify a greater occurrence of TDI among taller children, both variables were collected in a cross-sectional manner.10 A recent systematic review identified obesity as being associated with TDI, but nearly all studies analyzed had a cross-sectional design and involved schoolchildren.11 Thus, few longitudinal studies have evaluated the effects of anthropometric variables on the occurrence of TDI, especially among preschool children.
The World Health Organization (WHO) has suggested a strategy for combating risk factors common to different conditions to promote health.12,13 These factors include overweight and obesity, which are increasing in prevalence in several countries, and may represent risk factors for different relevant childhood health outcomes.14–16 Generally, anthropometric characteristics are influenced by environmental and behavioral factors during the prenatal period and early childhood and can therefore be modified.17 To contribute toward the establishment of prevention strategies, the effects of such variables on the occurrence of TDI should be investigated in longitudinal studies.
The aim of the present study was to investigate anthropometric risk factors at birth and 12 months of age for the occurrence of TDI in the primary dentition in a cohort of preschool children in southern Brazil.
MATERIAL AND METHODS
Participants and study design
The present prospective cohort study is nested in a cluster randomized clinical trial conducted in Porto Alegre, which is a city with 1.4 million inhabitants in southern Brazil. In the larger study, pregnant women were recruited from 20 primary health units between May 2008 and February 2009 with the aim of evaluating the impact of healthcare worker training in maternal nutritional counseling on child health outcomes.18 To be eligible for the study, the health units needed to have more than 100 annual appointments with children less than one year of age and not participate in any other intervention study.
Following the birth of children, mothers with a full-term gestation (> 37 weeks), no impediment with regard to breastfeeding (HIV/AIDS) and who had children with no congenital malformations were invited to participate in the study. Among the 736 women invited, 715 agreed to participate, corresponding to a 97.0% consent rate. The evaluations of the cohort were performed during household visits when the children were 12 months and three years of age. Oral health data were collected during the latter evaluation, which was performed when the children had an average of 38 months of age (n = 458). The originally recruited and analytic samples were similar in characteristics.19
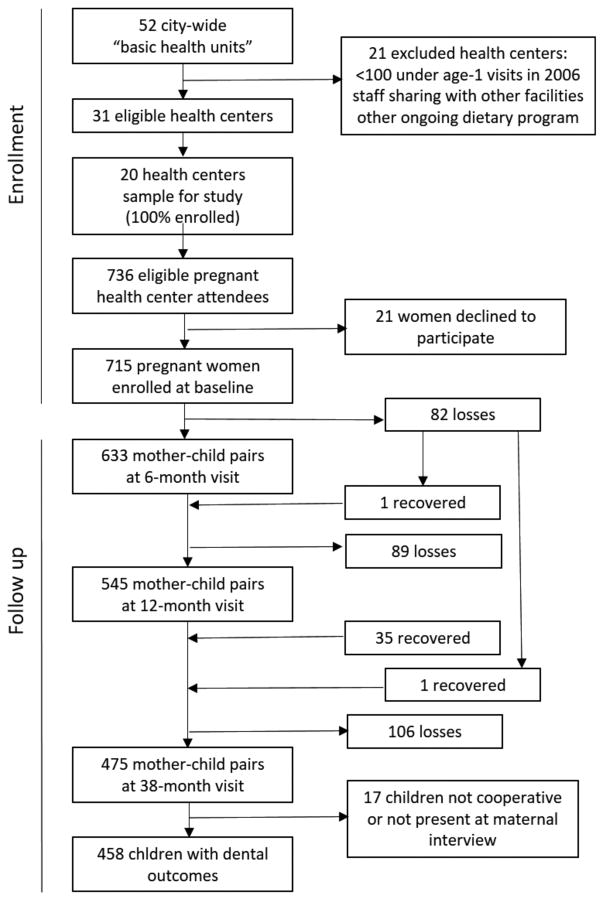
The number of participants recruited and who remained in the intervention study was used to determine the sample size of the present investigation. Based on a 95% confidence interval, 1:1 ratio of unexposed (shorter height for age) to exposed (taller height for age) children, an outcome prevalence rate of 17% among unexposed children and a relative risk of 1.79,10 the expected power of the study was estimated to be higher than 90%. Figure 1 displays the flowchart of the study.
Figure 1. Participant Flow.
Legend. Flow of participants: pregnant women were recruited from 20 municipal health centers in the city of Porto Alegre, Brazil, and followed to a mean child age of 38 months
Data collection
Collection of the independent (anthropometric) variables, potential confounding (demographic and socioeconomic) variables and the outcome (TDI) was performed through structured interviews, anthropometric examinations and dental examinations, as detailed below.
Baseline evaluation
After inclusion of the pregnant women to the cohort study, interviews were held to record mother’s schooling (categorized as more or less than eight years of study) and household income (in Brazilian currency [Real] and categorized in tertiles). Soon following the birth of the child, the following data were collected: sex (male or female), type of birth (natural or cesarean), birth weight (categorized as < 2,500 g, 2,500 g to 4,000 g and > 4,000 g), length at birth (< 48 cm or ≥ 48 cm) and head circumference (in mm, transformed into z-scores and categorized as < −1 standard deviation [SD] or ≥ −1 SD). The cutoff points were based on internationally accepted standards.20
Evaluation at 12 months of age
A team of extensively trained nutrition students collected data on the weight, height and body mass index (BMI) of the children at 12 months of age following international protocols. The data were converted into height/length-for-age and BMI-for-age z-scores using WHO standards.21 This was used to categorize the BMI as indicative of the ideal weight range (≤ 1 SD) or overweight/obesity (> +1 SD). Head circumference (in mm) was measured, transformed into z-scores and categorized as < −0.5 SD or ≥ − 0.5 SD. The cutoff point for this variable was defined by the lowest decile. It was not possible to use the same categorization at that used at birth, since the small number of children with a head circumference < −1 SD would impede the analysis.
Evaluation at three years of age
The oral health evaluation was performed with 458 of the 475 children followed up in the cohort when the children were three years of age. The evaluations were conducted by two trained examiners. To estimate reliability for TDI, each examiner previously evaluated 24 children aged three to five years on each of two occasions separated by a one-week interval. The unweighted inter-examiner kappa coefficient was 0.70 and unweighted intra-examiner kappa coefficients were 0.77 and 0.85.
The clinical examination followed the WHO protocol.22 The examiners first brushed the children’s teeth and dried the teeth with gauze. The examinations were performed using an intraoral mirror with a light (DenLite, Miltex Inc., York, PA, USA) with the children seated in a chair. The assessment of TDI, the outcome of this study, followed the criteria established by Andreasen.23
Statistical analysis
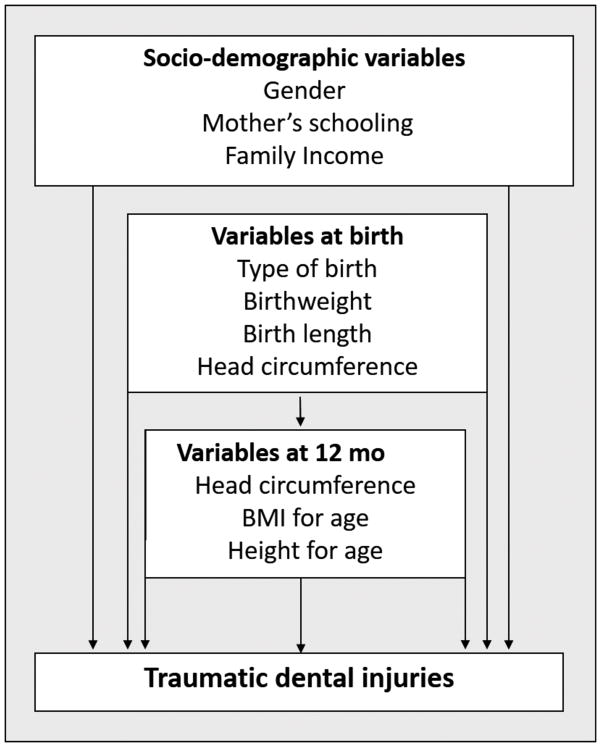
Statistical analysis was conducted with the aid of the SPSS 20.0 program for Windows (IBM, USA). Poisson regression with robust variance was performed to investigate associations between the anthropometric characteristics and TDI. Crude relative risk (RR) values and respective 95% confidence intervals (CI) were determined for the independent and adjustment variables. A hierarchical model was employed for the multivariable analysis,24 involving three levels: a) demographic and socioeconomic variables (sex, mother’s schooling and household income); b) anthropometric variables at birth (type of birth, birth weight and head circumference); and c) anthropometric variables at 12 months of age (BMI for age, height for age and head circumference) (Figure 2). All variables remained in the final model regardless of statistical significance and the effect measures were adjusted for variables on the same level or a higher level. The variable trial-group (intervention or control) was maintained in the final model regardless of statistical significance.
Figure 2. Conceptual hierarchical framework for traumatic dental injuries (TDI).
Legend. (none)
Ethical considerations
This study received approval from the Human Research Ethics Committee of the Porto Alegre Federal University of Health Sciences (UFSCPA) and the University of California – Berkeley and was conducted in accordance with the Declaration of Helsinki. The legal guardians received clarifications regarding the risks and discomfort their children may experience during the study and signed a statement of informed consent.
RESULTS
Among the 475 children who remained in the cohort at three years of age, 458 appeared for the clinical dental examination and constituted the final sample of the present study. The dropouts in each phase of the study are detailed in Figure 1. The sample was distributed similarly in terms of sex (50.9% boys). Approximately one third of the mothers had less than eight years of schooling; 69.2% of the children had a natural child birth and 94% had a normal birth weight. At 12 months of age, the BMI ranged from 14.3 to 25.4 (mean [SD]: 18.0 [1.8]; median [P25–P75]: 17.9 [16.6–19.1]). Nearly half of the children had overweight or obesity at 12 months of age (Table 1).
Table 1.
Characteristics of the sample and occurrence of traumatic dental injuries (TDI) according to the independent variables.
| Variables | N | (%) | TDI
|
p | |
|---|---|---|---|---|---|
| n | (%) | ||||
| Gender | 0.010 | ||||
| Male | 233 | (50.9) | 85 | (36.5) | |
| Female | 225 | (49.1) | 57 | (25.3) | |
| Mother’s schooling | 0.509 | ||||
| < 8 years | 142 | (31.0) | 41 | (28.9) | |
| ≥ 8 years | 316 | (69.0) | 101 | (32.0) | |
| Family Income | 0.987 | ||||
| 1st Tertile | 149 | (33.5) | 47 | (31.5) | |
| 2nd Tertile | 150 | (33.8) | 46 | (30.7) | |
| 3rd Tertile | 145 | (32.7) | 45 | (31.0) | |
| Birth weight | 0.451 | ||||
| <2,500 g | 27 | (6.2) | 06 | (22.2) | |
| 2,500 – 4,000 g | 376 | (85.8) | 116 | (30.9) | |
| > 4,000 g | 35 | (8.0) | 13 | (37.1) | |
| Birth length | 0.089 | ||||
| <48 cm | 110 | (25.3) | 27 | (24.5) | |
| ≥48 cm | 325 | (74.7) | 108 | (33.2) | |
| Head circumference at birth | 0.309 | ||||
| < −1SD | 63 | (13.8) | 23 | (36.5) | |
| ≥ −1SD | 395 | (86.2) | 119 | (30.1) | |
| Type of birth | 0.526 | ||||
| Cesarean | 136 | (30.8) | 45 | (33.1) | |
| Normal | 306 | (69.2) | 92 | (30.1) | |
| Head circumference at 12 months | 0.300 | ||||
| < −0.5SD | 56 | (12.2) | 14 | (25.0) | |
| ≥ −0.5SD | 402 | (87.8) | 128 | (31.8) | |
| BMI at 12 months | 0.004 | ||||
| Normal | 209 | (51.2) | 50 | (23.9) | |
| Overweight / obese | 199 | (48.8) | 74 | (37.2) | |
| Height for age at 12 months | 0.498 | ||||
| ≤1SD | 369 | (90.2) | 110 | (29.8) | |
| >1SD | 40 | (9.8) | 14 | (35.0) | |
SD - Standard Deviation
A total of 31.0% (142/458) of the children exhibited TDI at three years of age (95% CI: 27.1 to 34.9%), 106 of whom had one tooth affected, 34 had two teeth affected and two had more than two teeth affected. In the overall sample, 180 teeth had suffered TDI. The most common type of injury was enamel fracture, followed by enamel/dentin fracture and crown discoloration (data not shown not in a table).
The occurrence of TDI was significantly higher among boys (p = 0.011) and children with overweight or obesity at 12 months of age (p = 0.004). The multivariable analysis (Table 2) demonstrated that the risk of TDI was nearly 50% higher among children with a smaller head circumference at birth (RR 1.47; 95% CI: 1.02 to 2.11) and 60% higher among children with overweight/obesity at 12 months of age (RR: 1.58; 95% CI: 1.15 to 2.17). The risk of TDI was also significantly higher among boys (RR: 1.50; 95% CI: 1.13 to 2.00). The socioeconomic and other anthropogenic variables were not significantly associated with the outcome.
Table 2.
Unadjusted and adjusted risk ratios for Poisson Regression models and risk factors for traumatic dental injuries (TDI).
| Variables | Unadjusted
|
Adjusted*
|
||||
|---|---|---|---|---|---|---|
| RR | 95% CI | p | RR | 95% CI | p | |
| Level 1: Socio-demographic | ||||||
|
| ||||||
| Gender | 0.011 | 0.005 | ||||
| Male | 1.44 | (1.09–1.91) | 1.50 | (1.13–2.00) | ||
| Female | 1.00 | 1.00 | ||||
| Mother’s schooling | 0.513 | 0.345 | ||||
| < 8 years | 0.90 | (0.67–1.22) | 0.85 | (0.61–1.19) | ||
| ≥ 8 years | 1.00 | 1.00 | ||||
| Family Income | 0.987 | 0.867 | ||||
| 1st Tertile | 1.02 | (0.72–1.43) | 1.10 | (0.77–1.58) | ||
| 2nd Tertile | 0.99 | (0.70–1.39) | 1.03 | (0.73–1.45) | ||
| 3rd Tertile | 1.00 | 1.00 | ||||
|
| ||||||
| Level 2: Variables at birth | ||||||
|
| ||||||
| Birth weight | 0.464 | 0.431 | ||||
| <2,500 g | 0.72 | (0.35–1.48) | 0.64 | (0.29–1.44) | ||
| 2,500 – 4,000 g | 1.00 | 1.00 | ||||
| > 4,000 g | 1.20 | (0.76–1.90) | 1.20 | (0.75–1.92) | ||
| Birth length | 0.101 | 0.161 | ||||
| <48 cm | 0.74 | (0.51–1.06) | 0.75 | (0.50–1.12) | ||
| ≥48 cm | 1.00 | 1.00 | ||||
| Head circumference | 0.294 | 0.038 | ||||
| < −1SD | 1.21 | (0.85–1.73) | 1.47 | (1.02–2.11) | ||
| ≥ −1SD | 1.00 | 1.00 | ||||
| Type of birth | 0.532 | 0.403 | ||||
| Cesarean | 1.10 | (0.82–1.48) | 1.13 | (0.84–1.52) | ||
| Normal | 1.00 | 1.00 | ||||
|
| ||||||
| Level 3: Variables at 12 months | ||||||
|
| ||||||
| Head circumference | 0.319 | 0.656 | ||||
| < −0.5SD | 0.79 | (0.49–1.26) | 1.12 | (0.69–1.82) | ||
| ≥ −0.5SD | 1.00 | 1.00 | ||||
| BMI for age | 0.004 | 0.005 | ||||
| Normal | 1.00 | 1.00 | ||||
| Overweight / obese | 1.55 | (1.15–2.10) | 1.58 | (1.15–2.17) | ||
| Height for age | 0.485 | 0.835 | ||||
| ≤1SD | 1.00 | 1.00 | ||||
| >1SD | 1.17 | (0.75–1.84) | 0.95 | (0.60–1.50) | ||
adjusted for variables on the same or a higher level and child’s trial-group
SD - Standard Deviation
DISCUSSION
To the best of the authors’ knowledge, this is the first investigation to establish in a birth cohort that overweight and obese children in the first year of life have an increased risk of TDI in early childhood. A smaller head circumference at birth was also associated with the outcome. Few studies have investigated associations between anthropometric characteristics and TDI in childhood.
A recent systematic review described a 22% greater occurrence of TDI among children who were overweight or obese.11 However, among the 17 studies that contributed to the systematic review and meta-analysis, 15 involved the permanent dentition and 16 had a cross-sectional design, which impedes the identification of a causal relationship. Among the three studies conducted with preschool children, two had a cross-sectional design and presented conflicting results.25,26 The only previous longitudinal study to investigate this association found no greater incidence of TDI among children with a higher BMI.10 The cutoff point used – tertiles rather than categorization according to overweight and obesity – may at least partially explain the divergent results.
The identification of risk factors common to different adverse health conditions, including overweight and obesity, justifies the use of BMI for age and the cutoff points employed in the present investigation. BMI for age represents harmony between weight and height and is currently one of the most recommended indices for the assessment of individual and collective nutritional status.27,28
Overweight/obesity can lead to displacement of the center of mass and alter the axis of balance,29 with negative impacts on motor skills,30 postural stability and balance when walking.31–33 It should be stressed that the children in the present study were in the phase of learning to walk and establishing balance and the effect of obesity on such actions may be different at other ages. It is possible that the lower level of balance and motor skills in the early years of life may at least partially explain the association between obesity and bone fractures reported in previous studies involving preschool children as well as the findings of the present study.32,34,35 Another possible explanation is that children with a high body mass fall more heavily than lighter children.32,9
Head circumference, especially between birth and two years of age, is considered one of the indicators of healthy growth and may be associated with cognitive and visuospatial skills as well as motor and neurological disorders.8,36,37 Cutoff points for this variable vary depending on the objectives of each study and even for the definition of microcephaly. In the present study, the cutoff point was defined as the lowest decile. Although children with a small head circumference at birth and 12 months of age had a greater risk of TDI in childhood, these results should be evaluated with caution. Actually, the differences were only significant for head circumference at birth and after adjusting for potential confounding factors. The effect of a small head circumference has been increasingly studied in the medical literature and the present data suggest that TDI should also be included among the outcomes investigated. The recognition of a causal relationship between head circumference and TDI in childhood can only occur if the results of future longitudinal studies are consistent with the present findings.
The greater occurrence of TDI among male children has been previously reported for preschool children.25,38 However, this association is only consistent for older age groups, in which behavioral differences between genders are more evident. Although a statistically significant difference was found in the present study, it may not be clinically relevant, as it may not be large enough to warrant greater care or orientations given to the parents of male preschoolers.4
This study has limitations that should be considered. The considerable proportion of dropouts during the follow up may have influenced the results in an unknown manner. However, the possibility of selection bias is very low, as no differences were found in the baseline characteristics between the original cohort and the cohort analyzed, as reported above.18 The possibility of measurement bias is also very small due to exhaustive training with an experienced nutritionist conducted with children of different ages. Despite the good reproducibility between the examiners, non-differential classification error may have occurred with the outcome, especially due to the difficulty in separating enamel fractures from physiological wear or the results of tooth grinding. However, this type of poor classification would bias the results toward the null hypothesis and therefore does not account for the associations encountered.39
Another methodological aspect that merits discussion is the hierarchical approach used in the multivariable analysis. This approach recommends that statistical models first adjust for distal, or “upstream” variables, such as socioeconomic factors, before adding other proximal variables that might influence the outcome but are “downstream” or caused by the distal factors.24 There was no observed association between socioeconomic factors and TDI in any of the hierarchical models, suggesting that the lack of association with maternal education or family income in the present study was not due to over-adjustment for other potential causes of TDI that are downstream of socioeconomic position.
The identification of TDI as another consequence being overweight or obese is among the main implications of the present study. Such knowledge should be considered in the set of other potential outcomes that can stem from childhood obesity, such as morbidity and premature mortality in adulthood.15 The increase in overweight and obesity in childhood is one of the consequences of the nutritional transition that has marked the majority of developed and developing countries in the world.15
It should be stressed that overweight/obesity is a modifiable factor, since it is associated with a higher maternal pre-pregnancy BMI, excess maternal gestational weight gain and eating practices in the first two years of life, such as the consumption of sugary drinks and high energy density foods that are poor in micronutrients as well as the insufficient consumption of fruits, vegetables and grains.14,17,40 From the practical standpoint, the present findings underscore the need for prevention and control policies directed at childhood obesity.41 Programs aimed at the promotion of healthy eating in the first year of life are reported to reduce the frequency of hospitalizations and the use of medications.42 Among the implications for future studies, general and dental trauma should be included as outcomes to be evaluated in this type of intervention.
In conclusion, the results of the present study indicate overweight/obesity to be a risk factor for the occurrence of TDI in childhood and suggest that the prevention of childhood obesity is a plausible path for the reduction of this outcome. If proven consistent in future longitudinal studies, these findings add traumatic dental injury to other conditions that share common risk factors and combating such factors seems to be the most effective prevention strategy.
Acknowledgments
Thank you to members of the Federal University of Health Sciences of Porto Alegre Nutrition Research Group (NUPEN) for contributions in participant recruitment and data collection. Funding was provided from the NIH National Institute for Dental and Craniofacial Research (F30DE022208), the NIH National Center for Advancing Translational Sciences (KL2TR000143), the Rio Grande do Sul Research Support Foundation (FAPERGS), and the Coordination for the Improvement of Higher Education Personnel (CAPES). The information presented is solely the responsibility of the authors and does not necessarily represent the official views of the sponsoring organizations.
Footnotes
CONFLICT OF INTEREST
The authors confirm that they have no conflict of interest.
References
- 1.Viegas CM, Paiva SM, Carvalho AC, Scarpelli AC, Ferreira FM, Pordeus IA. Influence of traumatic dental injuries on quality of life of Brazilian preschool children and their families. Dent Traumatol. 2014;30:338–347. doi: 10.1111/edt.12091. [DOI] [PubMed] [Google Scholar]
- 2.Borges TS, Vargas-Ferreira F, Kramer PF, Feldens CA. Impact of traumatic dental injuries on oral health-related quality of life of preschool children: A systematic review and meta-analysis. PLoS One. 2017;12:e0172235. doi: 10.1371/journal.pone.0172235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petti, Stefano Over two hundred million injuries to anterior teeth attributable to large overjet: a meta-analysis. Dent Traumatol. 2015;31:1–8. doi: 10.1111/edt.12126. [DOI] [PubMed] [Google Scholar]
- 4.Feldens CA, Borges TS, Vargas-Ferreira F, Kramer PF. Risk factors for traumatic dental injuries in the primary dentition: concepts, interpretation, and evidence. Dent Traumatol. 2016;32:429–437. doi: 10.1111/edt.12281. [DOI] [PubMed] [Google Scholar]
- 5.Mau-Tsuen Yang, Min-Wen Chuang. Fall risk assessment and early-warning for toddler behaviors at home. Sensors. 2013;13:16985–17005. doi: 10.3390/s131216985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sabuncuoglu O, Irmak MY. The attention-deficit/hyperactivity disorder model for traumatic dental injuries: a critical review and update of the last 10 years. Dent Traumatol. 2016;33:71–76. doi: 10.1111/edt.12307. [DOI] [PubMed] [Google Scholar]
- 7.Xiang H, Smith GA, Wilkins JR, Chen G, Hostetler SG, Stallones L. Obesity and risk of nonfatal unintentional injuries. Am J Prev Med. 2005;29:41–45. doi: 10.1016/j.amepre.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Heinonen K, Raikkonen K, Pesonen AK, Kajantie E, Andersson S, Eriksson JG, Niemela A, Vartia T, Peltola J, Lano A. Prenatal and postnatal growth and cognitive abilities at 56 months of age: A longitudinal study of infants born at term. Pediatrics. 2008;121:1325–1333. doi: 10.1542/peds.2007-1172. [DOI] [PubMed] [Google Scholar]
- 9.Jones IE, Williams SM, Goulding A. Associations of birth weight and length, childhood size, and smoking with bone fractures during growth: Evidence from a birth cohort study. Am J Epidemiol. 2004;159:343–350. doi: 10.1093/aje/kwh052. [DOI] [PubMed] [Google Scholar]
- 10.Feldens CA, Kramer PF, Feldens EG, Pacheco LM, Vítolo MR. Socioeconomic, behavioral, and anthropometric risk factors for traumatic dental injuries in childhood: a cohort study. Int J Paediatr Dent. 2014;24:234–243. doi: 10.1111/ipd.12066. [DOI] [PubMed] [Google Scholar]
- 11.Corrêa-Faria P, Petti S. Are overweight/obese children at risk of traumatic dental injuries? A meta-analysis of observational studies. Dent Traumatol. 2015;31:274–282. doi: 10.1111/edt.12172. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization (WHO) Global strategy for the prevention and control of non-communicable diseases. Geneva: World Health Organization; 2000. pp. 1–4. [Google Scholar]
- 13.Sheiham A, Watt RG. The common risk factor approach: a rational basis for promoting oral health. Community Dent Oral Epidemiol. 2000;28:399–406. doi: 10.1034/j.1600-0528.2000.028006399.x. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization (WHO) Diet, nutrition, and the prevention of chronic diseases. World Health Organ Tech Rep Ser. 2003;916:1–7. [PubMed] [Google Scholar]
- 15.Reilly JJ, Kelly J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int J Obes. 2011;35:891–898. doi: 10.1038/ijo.2010.222. [DOI] [PubMed] [Google Scholar]
- 16.Broyles ST, Denstel KD, Church TS, Chaput JP, Fogelholm M, Hu G, Kuriyan R, et al. ISCOLE Research Group. The epidemiological transition and the global childhood obesity epidemic. Int J Obes Suppl. 2015;5:3–8. doi: 10.1038/ijosup.2015.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mameli C, Mazzantini S, Zuccotti GV. Nutrition in the first 1000 days: The origin of childhood obesity. Int J Environ Res Public Health. 2016;13:838–847. doi: 10.3390/ijerph13090838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chaffee BW, Vítolo MR, Feldens CA. The Porto Alegre early life nutrition and health study. Rev Bras Epidemiol. 2014;17:1015–1018. doi: 10.1590/1809-4503201400040018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chaffee BW, Feldens CA, Rodrigues PH, Vítolo MR. Feeding practices in infancy associated with caries incidence in early childhood. Community Dent Oral Epidemiol. 2015;43:338–348. doi: 10.1111/cdoe.12158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Puffer RR, Serrano CV. Patterns of birth weight. Pan American Health Organization (PAHO) - Scientific Publication nº 504; Washington, DC: 1987. p. 109. [Google Scholar]
- 21.World Health Organization (WHO) Methods and development. WHO (nonserial publication); Geneva: 2006. WHO Child Growth Standards: length/height-for-age, weight-forage, weight-for-length, weight-for-height and body mass index-for-age; pp. 139–300. [Google Scholar]
- 22.World Health Organization. Oral health surveys, basic methods. 4. Geneva: 1997. pp. 4–51. [Google Scholar]
- 23.Glendor U, Marcenes W, Andreasen JO. Classification, epidemiology and etiology. In: Andreasen JO, Andreasen FM, Andersson L, editors. Textbook and Color Atlas of Traumatic Injuries to the Teeth. 4. Oxford: Blackwell Munksgaard; 2007. pp. 217–54. [Google Scholar]
- 24.Victora CG, Huttly S, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26:224–227. doi: 10.1093/ije/26.1.224. [DOI] [PubMed] [Google Scholar]
- 25.Granville-Garcia AF, de Menezes VA, de Lira PIC. Dental trauma and associated factors in Brazilian preschoolers. Dent Traumatol. 2006;22:318–322. doi: 10.1111/j.1600-9657.2005.00390.x. [DOI] [PubMed] [Google Scholar]
- 26.Siqueira MB, Gomes MC, Oliveira AC, Martins CC, Granville-Garcia AF, Paiva SM. Predisposing factors for traumatic dental injury in primary teeth and seeking of post-trauma care. Braz Dent J. 2013;24:647–654. doi: 10.1590/0103-6440201302352. [DOI] [PubMed] [Google Scholar]
- 27.Bailey KV, Ferro-Luzzi A. Use of body mass index of adults in assessing individual and community nutritional status. Bull World Health Organ. 1995;73:673–680. [PMC free article] [PubMed] [Google Scholar]
- 28.WHO. [Accessed January 2017];Body mass index – BMI. 2016 Avaliable at: URL: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi.
- 29.Aleixo AA, Guimarães EL, Walsh IA, Pereira K. Influence of Overweight and Obesity on Posture, Overall Praxis and Balance in Schoolchildren. J Human Growth Development. 2012;22:239–245. [Google Scholar]
- 30.D’Hondt E, Deforche B, Bour-deaudhuij ID, Lenoir M. Childhood obesity affects fine motor skill performance under diferente postural constraints. Neurosci Lett. 2008;440:72–75. doi: 10.1016/j.neulet.2008.05.056. [DOI] [PubMed] [Google Scholar]
- 31.McGraw B, McClenaghan BA, Williams HG, Dickerson J, Ward DS. Gait and postural stability in obese and nonobese prepubertal boys. Arch Phys Med Rehabil. 2000;81:484–489. doi: 10.1053/mr.2000.3782. [DOI] [PubMed] [Google Scholar]
- 32.Goulding A, Jones IE, Taylor RW, Piggot JM, Taylor D. Dynamic and static tests of balance and postural sway in boys: effects of previous wrist bone fractures and high adiposity. Gait Posture. 2003;17:136–141. doi: 10.1016/s0966-6362(02)00161-3. [DOI] [PubMed] [Google Scholar]
- 33.Deforche BI, Hills AP, Worringham CJ, Davies PS, Murphy AJ, Bouckaert JJ, De Bourdeaudhuij IM. Balance and postural skills in normalweight and overweight prepubertal boys. Int J Pediatr Obes. 2009;4:175–182. doi: 10.1080/17477160802468470. [DOI] [PubMed] [Google Scholar]
- 34.Goulding A, Jones IE, Taylor RW, Manning PJ, Williams SM. More broken bones: a 4-year double cohort study of young girls with and without distal forearm fractures. J Bone Miner Res. 2000;15:2011–2018. doi: 10.1359/jbmr.2000.15.10.2011. [DOI] [PubMed] [Google Scholar]
- 35.Goulding A, Taylor RW, Jones IE, McAuley KA, Manning PJ, Williams SM. Overweight and obese children have low bone mass and area for their weight. Int J Obes. 2000;24:627–632. doi: 10.1038/sj.ijo.0801207. [DOI] [PubMed] [Google Scholar]
- 36.Sargoor RV, Ghattu VK, Andrew KW, Anura VK, Sumithra M, Jacqueline CH, Samuel CK, Kiran KN, Caroline HDF, Krishnamachari S. Association of birthweight and head circumference at birth to cognitive performance in 9- to 10-year-old children in South India: prospective birth cohort study. Pediatr Res. 2010;67:424–429. doi: 10.1203/PDR.0b013e3181d00b45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Geraedts EJ, van Dommelen P, Caliebe J, Visser R, Ranke MB, van Buuren S, Wit JM, Oostdijk W. Association between head circumference and body size. Horm Res Paediatr. 2011;75:213–219. doi: 10.1159/000321192. [DOI] [PubMed] [Google Scholar]
- 38.Robson F, Ramos-Jorge ML, Bendo CB, Vale MP, Paiva SM, Pordeus IA. Prevalence and determining factors of traumatic injuries to primary teeth in preschool children. Dent Traumatol. 2009;25:118–122. doi: 10.1111/j.1600-9657.2008.00725.x. [DOI] [PubMed] [Google Scholar]
- 39.Rothman KJ, Greenland S. Modern epidemiology. 2. Philadelphia, USA: Lippincott Williams & Wilkins; 1998. pp. 126–27. [Google Scholar]
- 40.Ehrenthal DB, Maiden K, Rao A, West DW, Gidding SS, Bartoshesky L, Carterette B, Ross J, Strobino D. Independent relation of maternal prenatal factors to early childhood obesity in the offspring. Obstet Gynecol. 2013;121:115–121. doi: 10.1097/aog.0b013e318278f56a. [DOI] [PubMed] [Google Scholar]
- 41.Dietz WH, Baur LA, Hall K, et al. Management of obesity: improvement of health-care training and systems for prevention and care. Lancet. 2015;385:2521–2533. doi: 10.1016/S0140-6736(14)61748-7. [DOI] [PubMed] [Google Scholar]
- 42.Vitolo MR, Bortolini GA, Feldens CA, Drachler ML. Impacts of the 10 Steps to healthy feeding in infants: a randomized Field trial. Cad Saude Publica. 2005;215:1448–1457. doi: 10.1590/s0102-311x2005000500018. [DOI] [PubMed] [Google Scholar]