Abstract
Objective
Psychosocial factors, including pressure to be thin and body dissatisfaction, have been hypothesized to mediate the relationship between obesity and depression, especially during adolescence when vulnerability to social pressures around body shape and image is heightened. The objective was to test a model of the relationships among adiposity, psychosocial factors and depression in adolescents.
Method
In a population-based sample of 1127 boys and 1167 girls aged 13 and 16 years, a model of the relationships between adiposity, pressure to be thin, body dissatisfaction and depressive symptoms was tested using structural equation modeling.
Results
Among girls, adiposity accounted for 62% of the total effect of depressive symptoms through its association with pressure to be thin and body dissatisfaction. Pressure to be thin was also uniquely related to depressive symptoms. Among boys, only body dissatisfaction was associated with depressive symptoms.
Conclusion
Results support a relationship between adiposity, body satisfaction, pressure to be thin and depressive symptoms. Depressive symptoms should be assessed in obese adolescents, and interventions to prevent and treat obesity should incorporate elements targeting body dissatisfaction.
Keywords: depressive symptoms, adolescents, structural equation model, pressure to be thin, body satisfaction
Introduction
Adiposity and depression are both associated with prevalent chronic conditions, including hypertension, dyslipidemia, diabetes mellitus, coronary heart disease, stroke and myocardial infarction, as well as with increased mortality.1 Adolescent adiposity and depression often track into adulthood, and at least one study reports that preventing adiposity and depression during adolescence can reduce the burden of these chronic conditions in adulthood.2
Although findings are not consistent across studies,3,4 several population-based investigations report that body weight is associated with depression.3–5 A recent systematic review by Atlantis and Baker6 reported that there is some evidence that obesity increases the incidence of depression. In adults, the association may have a biological basis as both obesity and depression have been linked to abnormal functioning of the hypothalamic–pituitary–adrenal axis and serotonin imbalances.7–9 Alternatively, the relationship may result from an interaction of psychosocial pathways that mediate the relation between adiposity and depression. More specifically, body-related psychosocial constructs, such as pressure to be thin and body dissatisfaction, have been linked to depressive symptoms.5,10–13 Among adolescents, body dissatisfaction affects depressive symptoms.6,14,15 Fulkerson et al.14 found that depressive symptoms were associated with body dissatisfaction among 4734 middle and high school students. In addition to the direct relationship showing that increases in body dissatisfaction are associated with increases in depression, both McCarthy16 and Stice and Bearman17 suggested that body dissatisfaction may mediate the relationship between overweight and depression. Specifically, several studies show that overweight adolescents may encounter stigma and discrimination, which increase body dissatisfaction and increase depressive symptoms.18–20 This condition suggests an indirect association, whereby depressive symptoms are affected by weight through the effects of body dissatisfaction. To date, there is little evidence examining the simultaneous direct and indirect effects of obesity, body dissatisfaction and depression.
Social pressure to be thin arising from family, friends and cultural norms has also been hypothesized to affect the relationship between increased adiposity, body dissatisfaction and depression.21–23 Internalization of a cultural ideal of thinness and a comparison of oneself with cultural norms may promote body dissatisfaction, which may in turn lead to depression.17 Specifically, family attitudes toward weight and eating habits were associated with depressed mood among overweight adolescents.24 Stice and Bearman17 also found that pressure to be thin predicted subsequent increased depressive symptoms, and mediated the relationship between body weight and depression. In sum, pressure to be thin may directly affect body dissatisfaction and depressive symptoms, and may also mediate the relationship between adiposity and depression.
The relationship between adiposity and depression differs by sex, possibly because the cultural norms about body size and the pressure to be thin differ for boys and girls.22 Body dissatisfaction is of concern in both sexes, but may have strikingly different effects in boys and girls.25 In a study of body dissatisfaction, Kostanski et al.25 found girls were more dissatisfied with their bodies with increasing weight; however, both overweight and underweight boys expressed increased levels of body dissatisfaction.
One concern with earlier studies is that neither body weight nor body mass index (BMI) can distinguish between fat and muscle mass.26,27 Although body weight and BMI are generally good proxies for unhealthy body weight, other measures, such as skinfold thickness and waist circumference, represent other important dimensions of adiposity. Assessing both body weight and fat composition could better represent unhealthy body weight than body weight or BMI alone.
We posit a conceptual model (Figures 1 and 2) of the relationship between adiposity and depressive symptoms. In this model, we depict a direct relationship, in which increased adiposity would be associated with higher levels of depressive symptoms. We also suggest an indirect relationship, whereby higher adiposity levels are associated with higher depressive symptoms when there are reports of greater body dissatisfaction and pressure to be thin. The purpose of this study is to test the relationships depicted in the model in a representative population-based sample of adolescents in Quebec, Canada.
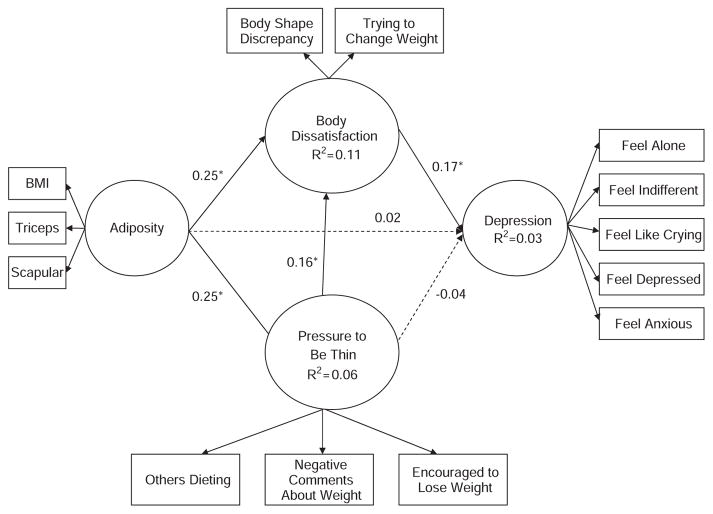
Figure 1.
Conceptual model, including empirical information depicting the standardized solution for the direct and indirect effects of adiposity, pressure to be thin and body dissatisfaction on depression for adolescent boys.
Figure 2.
Conceptual model, including empirical information depicting the standardized solution for the direct and indirect effects of adiposity, pressure to be thin and body dissatisfaction on depression for adolescent girls.
Methods
Study population
Data were drawn from the 1999 Quebec Child and Adolescent Health and Social Survey. The survey design and methodology have been reported in detail elsewhere,28 and are only summarized here. Three independent, representative samples of youth aged 9, 13 and 16 years (one sample per age) were drawn using a province-wide cluster sampling design. Participants completed an age-adapted self-report questionnaire on lifestyle habits and psychosocial indicators, including depressive symptoms. Anthropometric measurements, including height, weight, and triceps and subscapular skinfold thickness, were collected at school by 10 teams of pediatric nurses, kinesiologists and trained interviewers according to a standardized protocol.28 In addition, parents completed a questionnaire sent home and returned it to school with the participant.
This analysis was restricted to participants aged 13 and 16 years because data on depressive symptoms were not collected among 9-year-old children. A total of 1186 of 1498 eligible participants aged 13 years (79%) and 1160 of 1495 (78%) of 16 years completed the questionnaire. Parent questionnaires were completed by 69% (1031/1498) and 64% (952/1495) of parents of 13- and 16-year-old participants, respectively. Complete data were available for 1167 girls and 1127 boys (51% of participants aged 13 years and 49% of those aged 16 years) on adiposity, symptoms of depression and all other variables used in the analysis. There were no significant differences in the study variables between adolescents retained in the analysis and those excluded because of missing or incomplete data (data not shown).
The Quebec Child and Adolescent Health and Social Survey was approved by the Ethics Review Boards of the Direction Santé Québec, Institut de la statistique du Québec and the Centre Hospitalier Universitaire Sainte-Justine. Written informed consent was obtained from the parents and legal guardians of participants. Participant assent was obtained from all students at time of the survey.
Study variables
Socio-demographic data included sex and language usually spoken with best friends (French, English, other). Data on mothers’ level of education (elementary school, secondary school, trade school, CEGEP (college), university), used as a measure of socioeconomic position, were drawn from the parent questionnaire.
Depressive symptoms
Depressive symptoms were measured using the French version of the depression subscale of the Psychological Distress Scale.29 The scale was translated into French and validated for use in Quebec.29–32 The scale contains five items that asked students/respondents to report how often in the past week (never, sometimes, fairly often, very often) they felt, alone; indifferent or uninterested in things; cry easily or feel like crying; depressed or disheartened; and anxious about the future. Scores were computed by averaging responses. Cronbach’s α coefficient for the translated version of the depression subscale was 0.93 suggesting excellent internal consistency29 and the 1-year test-retest reliability coefficient was 0.68.30 Depressive symptom subscale scores correlate well with the Center for Epidemiology Studies-Depression scale (r=0.89),31 and persons with high scores were 6.5 times more likely to be hospitalized for a mental health problem than those with lower scores.29,32 For the current analysis, each item was used as an observed indicator (that is, manifest variable) of a ‘depressive symptoms’ latent variable.
Adiposity
Body mass index was computed as weight (kg)/height (m)2. For the analysis, BMI and measures of skinfold thickness at two different sites (triceps and subscapular) were log transformed and then age- and sex-standardized on the basis of the sample characteristics (due to non-normally distributed data), and were used as indicators of an ‘adiposity’ latent variable.
Pressure to be thin
Three items were used as manifest indicators of a ‘pressure to be thin’ latent variable. Development of the construct of pressure to be thin relies on Bandura’s33 social learning theory, wherein pressure is exerted through direct encouragement for behavior change, negative feedback/comments or through role modeling of behavior. Participants were asked to indicate whether their mother/adult woman they live with, father/adult male they live with, brothers or sisters, friends and others: (i) ever go on a diet to lose weight or maintain their weight (labeled others dieting herein); (ii) make negative comments about your weight (labeled negative comments about weight herein); and (iii) ever encourage or push you to lose weight (labeled encouraged to lose weight herein). For each question, responses included does not apply or do not know (scored 0), no (scored 1) and yes (scored 2).
Body dissatisfaction
Two items were used as manifest indicators of a ‘body dissatisfaction’ latent variable. First, using the adolescent-specific Stunkard’s34 Figure Rating Scale, the adolescents were asked to indicate the body size that best corresponded to their current appearance, as well as the body size that represented what they would like to look like. A body shape discrepancy score was computed by taking the absolute value of the difference between the current and ideal body size. A second item (labeled trying to change weight herein) asked ‘Are you currently doing anything about your weight?’ Response choices included: I am trying to lose weight (scored 1), I am trying to maintain my weight (scored 0), I am trying to gain weight (scored 1), I am not doing anything about my weight (scored 0).
Data analysis
Means and standard deviations, and Spearman Rho correlation coefficients were evaluated among observed variables using SPSS 13.0. Differences on key variables by sex and age (including sex×age interactions) were evaluated using ANOVA. The maximum likelihood estimation method for structural equation modeling was used to test the conceptual model (Figure 1) with LISREL 8.71 software program. In the measurement model, reliability was examined by assessing the proportion of variance accounted for in each indicator (that is, the questionnaire items) by the adiposity, pressure to be thin, body dissatisfaction and depressive symptoms latent variables, whereas validity was assessed by examining the magnitude and significance of the factor loading between each indicator and latent variable, and the error variances associated with each indicator. The relationships among latent variables were also examined.35 The effects of adiposity, pressure to be thin, body dissatisfaction and depressive symptoms were tested using path analysis modeling, 35,36 wherein the model fit was examined, as well as the significance of the direct and indirect effects. Finally, mother’s education (dichotomized into less than high school education vs at least high school education), age (13 vs 16) and sex were tested as effect modifiers using multigroup invariance analyses.7,35
The following indicators were used to assess the goodness of fit of the models:37 (a) Comparative Fit Index (CFI; values approximating 0.95), (b) Non-Normed Fit Index (NNFI; values approximating 0.95) and (c) Root Mean Square Error of Approximation (RMSEA; values approximating 0.05).35 χ2-statistic was used for the structural invariance tests to determine significant effect modifiers. In all analyses, critical t-test values (t≥1.96 and/or P≤0.05) were used to determine statistical significance. Finally, the relative contribution of the indirect effects in the model were calculated as follows: Percentage (%) of indirect effects=(indirect effects/total effects)×100, where total effects=indirect+direct effects.
Results
Descriptive statistics
The sample was predominantly French speaking (88%). Seventy-nine percent of participants perceived that their family economic situation was the same as that of their classmates. One-fifth of mothers had less than secondary school education, 27% had completed high school, and 54% attended trade school, college or university. 13 and 10%, respectively, of 13 and 16-year-old boys, and 14 and 7% of 13 and 16-year-old girls were overweight or obese. Approximately 29% of boys and 36% of girls indicated that they were trying to change their weight. Girls had significantly higher triceps and scapular skinfold thickness compared with boys. They also had significantly more people in their surroundings who were dieting, made negative comments about their weight and encouraged them to lose weight. Finally, girls reported having more depressive symptoms than boys (Table 1). Spearman Rho correlation coefficients among observed (manifest) study variables are presented in Table 2. Of importance, the relationships among the adiposity measures were strong, the associations among the pressure to-be-thin items were moderate, and the two items for body dissatisfaction showed a low-moderate significant relationship.
Table 1.
Descriptive statistics for anthropometric measurements, psychosocial factors and depressive symptoms
| Boys (n =1127) Mean (s.d.) |
Girls (n =1167) Mean (s.d.) |
F-statistica (for comparison by sex) | Effect sizec Cohen’s d | |
|---|---|---|---|---|
| BMI (kg/m2) | 21.3 (3.9) | 21.4 (4.2) | 0.0 | −0.02 |
| Triceps skinfold thickness (mm) | 13.1 (7.2) | 18.7 (6.9) | 358.4* | −0.81 |
| Scapular skinfold thickness (mm) | 10.9 (6.7) | 14.0 (7.0) | 115.5* | −0.44 |
| Absolute body shape discrepancy score | 0.8 (0.9) | 0.7 (0.8) | 0.4 | 0.13 |
| Percent trying to change weightb | 28.7% | 36.1% | — | — |
| Others dieting | 4.0 (1.9) | 4.7 (1.6) | 82.6* | −0.44 |
| Negative comments about weight | 4.1 (1.3) | 4.3 (1.2) | 21.3* | −0.17 |
| Encouraged to lose weight | 3.9 (1.2) | 4.1 (1.1) | 9.6* | −0.18 |
| Depressive symptoms | 1.5 (0.6) | 1.8 (0.7) | 113.2* | −0.43 |
Abbreviations: ANOVA, analysis of variance; BMI, body mass index.
P<0.05.
F-statistics for the ANOVA models comparing boys and girls.
Percentage of boys and girls reporting ‘yes’ to trying to change weight.
Negative effect size indicates that boys’ standard deviation units were lower than girls’.
Table 2.
Spearman rho correlation coefficients for relationships among adiposity, pressure to be thin, body dissatisfaction and depressive symptoms for adolescent boys and girls
| Boys (n =1127)
|
Girls (n =1167)
|
|||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | |
| BMI (kg/m2) | — | — | ||||||||||||||||
| Triceps skinfold thickness | 0.67* | — | 0.78* | — | ||||||||||||||
| Scapular skinfold thickness | 0.78* | 0.81* | — | 0.79* | 0.82* | — | ||||||||||||
| Discrepancy | 0.04 | 0.14* | 0.16* | — | 0.40* | 0.32* | 0.34* | — | ||||||||||
| Trying to change weight | 0.08* | 0.07* | 0.10* | 0.20* | — | 0.36* | 0.25* | 0.28* | 0.34* | — | ||||||||
| Others dieting | 0.04 | 0.01 | 0.03 | −0.05 | 0.01 | — | 0.07* | 0.05 | 0.06* | 0.02 | 0.10* | — | ||||||
| Negative comments about weight | 0.13* | 0.13* | 0.14* | 0.07* | 0.08* | 0.35* | — | 0.27* | 0.19* | 0.21* | 0.16* | 0.19* | 0.29* | — | ||||
| Encouraged to lose weight | 0.25* | 0.25* | 0.22* | 0.09* | 0.12* | 0.33* | 0.60* | — | 0.34* | 0.24* | 0.26* | 0.19* | 0.21* | 0.29* | 0.61* | — | ||
| Depressive symptoms | 0.05 | 0.05 | 0.05 | 0.08* | 0.06 | −0.07* | 0.01 | −0.01 | — | 0.11* | 0.08* | 0.07* | 0.14* | 0.13* | 0.06* | 0.17* | 0.13* | — |
Abbreviation: BMI, body mass index.
P value <0.05.
Main analyses
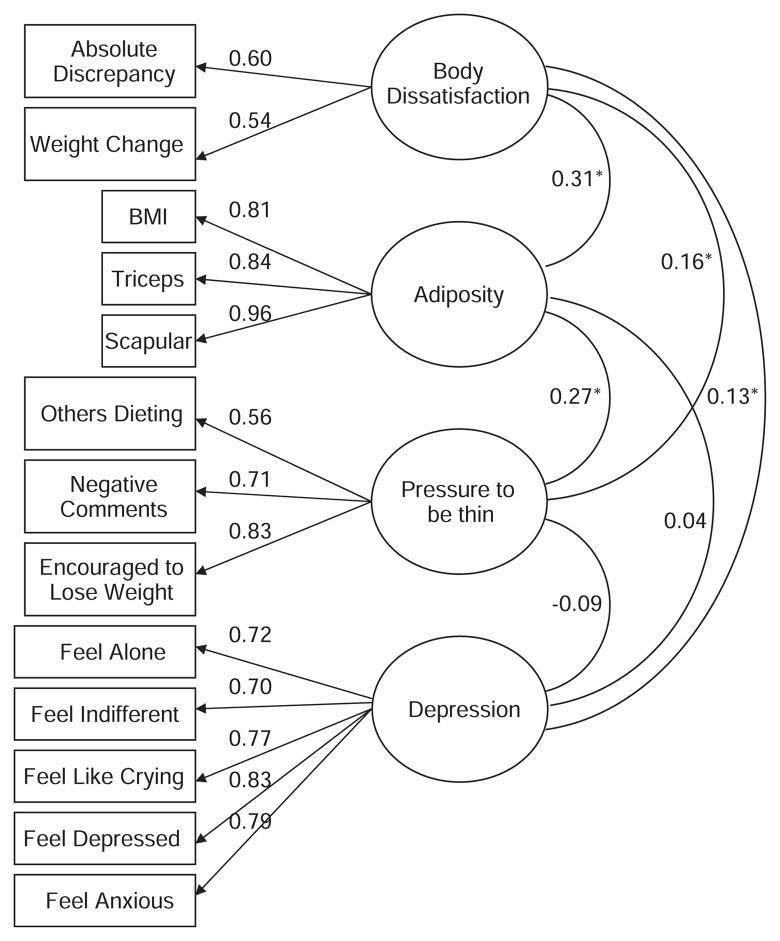
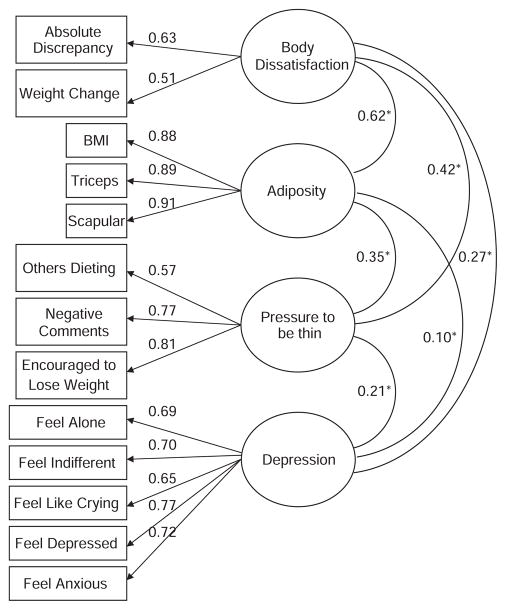
In the measurement models, all factor loadings between each indicator and latent variable were relatively high and statistically significant (85% of the loadings >0.60), with low (<0.05) standard error variances, highlighting the construct validity and indicator reliability of the adiposity, pressure to be thin, body dissatisfaction and depression latent variables (Figures 3 and 4). The proportion of explained variance in each indicator was also moderate to high (R2 values ranging from 0.24 to 0.96), providing evidence of reliability. The correlations among latent factors were statistically significant for girls, with coefficients ranging from 0.10 to 0.62. For boys the correlation coefficients ranged between 0.13 and 0.31, and all attained statistical significance with two exceptions including the correlation between adiposity and depression, and between pressure to thin and depression. Fit statistics indicated that the measurement models were adequate for both girls and boys (RMSEA=0.05, CFI=0.97, NNFI= 0.96–0.97).
Figure 3.
Measurement model, including factor loadings between the indicator variables (rectangles) and latent variables (ovals), and covariance among factors for adolescent boys.
Figure 4.
Measurement model, including factor loadings between the indicator variables (rectangles) and latent variables (ovals), and covariance among latent variables for adolescent girls.
The path model was also a good fit with the data (RMSEA=0.05, CFI=0.97, NNFI=0.96) for both boys (Figure 1) and girls (Figure 2). The paths between adiposity and depressive symptoms did not attain statistical significance for boys or girls, although most of the other hypothesized relationships were supported in the model. For girls, the indirect effect of adiposity on depressive symptoms mediated by body dissatisfaction and pressure to be thin variables was significant, accounting for 62% of the total effects (Table 3). The indirect effect of pressure to be thin on depression, as mediated by body dissatisfaction, was also significant (29% of the total effects). For boys, there were no significant indirect effects (Table 3) and the direct effect of the pressure to be thin on depressive symptoms was not significant. The path model was then tested to see if socioeconomic position (assessed by mother’s education), age or sex were effect modifiers of the tested relationships in the model. Although there were no differences in the path coefficients for socioeconomic position or age, all paths were statistically significantly different in boys and girls, with two exceptions: the path between body dissatisfaction and depressive symptoms, and the path between adiposity and pressure to be thin. These results suggest that the effects in the relationships between adiposity and body dissatisfaction, pressure to be thin and body dissatisfaction, and pressure to be thin and depressive symptoms were statistically significantly stronger in girls than in boys.
Table 3.
Standardized parameter estimates for the total and indirect paths of adiposity, pressure to be thin and body dissatisfaction on depression
| Boys (n =1127)
|
Girls (n =1167)
|
|||||
|---|---|---|---|---|---|---|
| Indirect effect | Direct effect | Total effect | Indirect effect | Direct effect | Total effect | |
| Adiposity | 0.03 | 0.01 | 0.04 | 0.16* | 0.10 | 0.26* |
| Pressure to be thin | 0.02 | −0.03 | −0.01 | 0.06* | 0.15* | 0.21* |
| Body dissatisfaction | — | 0.21* | 0.21* | — | 0.33* | 0.33* |
P<0.05.
Discussion
Results of this study support a model depicting the existence of a relationship between adiposity, body satisfaction, pressure to be thin and depressive symptoms. The results also highlight important differences in these relationships between boys and girls. In terms of treatment, clinicians should assess depressive symptoms in obese adolescents, and interventions to prevent and treat obesity should consider incorporating elements targeting body dissatisfaction. In interventions aimed at weight change, neglecting the psychosocial dimensions of pressure to be thin and body dissatisfaction could increase depressive symptoms and reduce the chances of successful intervention.
In support of earlier reports,20,38–40 adiposity in girls was related to depression only through psychosocial factors, including body dissatisfaction and pressure to be thin. Cross-sectional data for 16- to 18-year-old girls in the Youth Risk Behavioral Surveillance System suggested no relationship between depressive symptoms and weight, but self-perceived underweight or overweight was related to increases in depressive symptoms.41 Similarly, Shin and Shin5 reported that body dissatisfaction was a mediator between BMI and self-esteem, and that depressive symptoms were higher in obese children with body dissatisfaction. Collectively, these studies suggest that dissatisfaction with body size and pressure to be thin (rather than actual adiposity) may lead to poor mental health in adolescents. Social and cultural attitudes toward healthy behaviors, weight and body image may affect perceptions of body size and shape, which in turn may determine whether or not actual body size is associated with depressive symptoms among adolescents.
Stice’s19 model of depression proposes that girls have additional risk factors for depression over and above those experienced by boys. Stice’s19 gender-additive model suggests that cultural factors valuing appearance and thinness lead to greater concern about body image and increased risk of developing depression.34,42 Our results support this gender additive model, in that the pathway to depression in boys and girls seems to differ in important respects. These findings are also consistent with a nationally representative longitudinal study conducted in the United States, which found that weight was associated with depressive symptoms for girls, but not boys.4 The thin ideal, as a standard of beauty, is thought to apply almost exclusively to girls43 and our study supports that in girls, the pressure to be thin relates to both body dissatisfaction and depression.
There are limited studies examining the relationship between body dissatisfaction and depression in boys.44 In this analysis, body dissatisfaction related to depression in boys. There may be pressures on boys to gain muscle mass such that body weight may not translate into body dissatisfaction, if weight is perceived by boys to substitute for muscle.
Although adiposity and depressive symptoms relate cross-sectionally in this analysis through the psychosocial pathways of body dissatisfaction and pressure to be thin, an alternative hypothesis is that depressive symptoms may influence weight gain. In longitudinal studies, depression among adolescents has also been shown to predict increases in weight as an adult.7,42,45 There may be a ‘vicious cycle’, wherein an increase in body dissatisfaction lead to depression, which in turn could promote subsequent obesity in adulthood.
Strengths of this analysis include a large, population-based representative sample of adolescents. Use of structural equation modeling allows for simultaneous evaluation of multiple relationships. This analytic design also enables the identification of latent variables, such as adiposity, with aggregate information on BMI and skinfold thickness. Our conceptualization of adiposity as a latent variable may better reflect the construct of unhealthy body size because of the inability of BMI or body weight alone to discern between fat and muscle mass.
Limitations of this study include the cross-sectional design, which precludes conjecture about causality and the direction of the effects beyond the theory used to develop the model. We did not measure pubertal status, which has been associated with both depression and obesity in earlier work.44 However, we showed that age did not moderate the associations of interest. Our age groups, 13 and 16 years, were purposely chosen to reflect adolescents in mid-puberty and those at the end of puberty. Although the survey was administered in 1999, it is one of the few large-scale, population-based, representative surveys of adolescents that include data on weight and height measured by trained technicians. It is the most recent survey of this kind in Quebec and Canada. Although the prevalence of depression and obesity varies from year to year, the relationships between the variables investigated in this analysis should not differ substantially across a decade.
In conclusion, our results provide support for a model of indirect effects between depressive symptoms and obesity in adolescent girls. Although body dissatisfaction is an important correlate of depression in boys, adiposity and pressure to be thin influence body satisfaction differently in boys. Clinicians should be aware that both boys and girls are susceptible to depressive symptoms associated with dissatisfaction with body size. Psychosocial factors, such as the perception of adiposity and attitude toward adiposity, can be targeted and modified through prevention efforts. Programs that target body dissatisfaction and pressure to be thin could help reduce depressive symptoms among adolescents, and lead to more effective obesity prevention interventions.
Acknowledgments
The Quebec Child and Adolescent Health and Social Survey survey was funded by the Quebec Ministry of Health and Social Services and by Health Canada. The study of cardiovascular risk factors in youth was funded by the Canadian Institutes of Health Research. Dr Jennifer O’Loughlin holds a Canada Research Chair in the Early Determinants of Adult Chronic Disease. Katerina Maximova holds a strategic training fellowship in Transdisciplinary Public and Population Health Research from the Canadian Institutes of Health Research and Quebec Population Health Research Network. She is also supported through an NCIC grant.
Catherine Sabiston and Michael Chaiton had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Dragan A, Akhtar-Danesh N. Relation between body mass index and depression: a structural equation modeling approach. BMC Med Res Methodol. 2007;7:17. doi: 10.1186/1471-2288-7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, et al. Overweight in children and adolescents: pathophysiology, consequences, prevention, and treatment. Circulation. 2005;111:1999–2012. doi: 10.1161/01.CIR.0000161369.71722.10. [DOI] [PubMed] [Google Scholar]
- 3.Erickson SJ, Robinson TN, Haydel KF, Killen JD. Are overweight children unhappy?: Body mass index, depressive symptoms, and overweight concerns in elementary school children. Arch Pediatr Adolesc Med. 2000;154:931–935. doi: 10.1001/archpedi.154.9.931. [DOI] [PubMed] [Google Scholar]
- 4.Needham BL, Crosnoe R. Overweight status and depressive symptoms during adolescence. J Adolesc Health. 2005;36:48–55. doi: 10.1016/j.jadohealth.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 5.Shin NY, Shin MS. Body dissatisfaction, self-esteem, and depression in obese Korean children. J Pediatr. 2008;152:502–506. doi: 10.1016/j.jpeds.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 6.Atlantis E, Baker M. Obesity effects on depression: systematic review of epidemiological studies. Int J Obes (Lond) 2008;32:881–891. doi: 10.1038/ijo.2008.54. [DOI] [PubMed] [Google Scholar]
- 7.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 8.Mustillo S, Worthman C, Erkanli A, Keeler G, Angold A, Costello EJ. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003;111:851–859. doi: 10.1542/peds.111.4.851. [DOI] [PubMed] [Google Scholar]
- 9.Raber J. Detrimental effects of chronic hypothalamic-pituitaryadrenal axis activation. From obesity to memory deficits. Mol Neurobiol. 1998;18:1–22. doi: 10.1007/BF02741457. [DOI] [PubMed] [Google Scholar]
- 10.Ohring R, Graber JA, Brooks-Gunn J. Girls’ recurrent and concurrent body dissatisfaction: correlates and consequences over 8 years. Int J Eat Disord. 2002;31:404–415. doi: 10.1002/eat.10049. [DOI] [PubMed] [Google Scholar]
- 11.Rierdan J, Koff E. Weight, weight-related aspects of body image, and depression in early adolescent girls. Adolescence. 1997;32:615–624. [PubMed] [Google Scholar]
- 12.Wichstrom L. The emergence of gender difference in depressed mood during adolescence: the role of intensified gender socialization. Dev Psychol. 1999;35:232–245. [PubMed] [Google Scholar]
- 13.Wardle J, Cooke L. The impact of obesity on psychological well-being. Best Pract Res Clin Endocrinol Metab. 2005;19:421–440. doi: 10.1016/j.beem.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Fulkerson JA, Sherwood NE, Perry CL, Neumark-Sztainer D, Story M. Depressive symptoms and adolescent eating and health behaviors: a multifaceted view in a population-based sample. Prev Med. 2004;38:865–875. doi: 10.1016/j.ypmed.2003.12.028. [DOI] [PubMed] [Google Scholar]
- 15.Johnson F, Wardle J. Dietary restraint, body dissatisfaction, and psychological distress: a prospective analysis. J Abnorm Psychol. 2005;114:119–125. doi: 10.1037/0021-843X.114.1.119. [DOI] [PubMed] [Google Scholar]
- 16.McCarthy M. The thin ideal, depression and eating disorders in women. Behav Res Ther. 1990;28:205–215. doi: 10.1016/0005-7967(90)90003-2. [DOI] [PubMed] [Google Scholar]
- 17.Stice E, Bearman SK. Body-image and eating disturbances prospectively predict increases in depressive symptoms in adolescent girls: a growth curve analysis. Dev Psychol. 2001;37:597–607. doi: 10.1037//0012-1649.37.5.597. [DOI] [PubMed] [Google Scholar]
- 18.Adams PJ, Katz RC, Beauchamp K, Cohen E, Zavis D. Body dissatisfaction, eating disorders, and depression: a developmental perspective. J Child Fam Stud. 1993;2:37–46. [Google Scholar]
- 19.Stice E, Hayward C, Cameron RP, Killen JD, Taylor CB. Body-image and eating disturbances predict onset of depression among female adolescents: a longitudinal study. J Abnorm Psychol. 2000;109:438–444. [PubMed] [Google Scholar]
- 20.Friedman KE, Reichmann SK, Costanzo PR, Musante GJ. Body image partially mediates the relationship between obesity and psychological distress. Obes Res. 2002;10:33–41. doi: 10.1038/oby.2002.5. [DOI] [PubMed] [Google Scholar]
- 21.Stice E, Maxfield J, Wells T. Adverse effects of social pressure to be thin on young women: an experimental investigation of the effects of ‘fat talk’. Int J Eat Disord. 2003;34:108–117. doi: 10.1002/eat.10171. [DOI] [PubMed] [Google Scholar]
- 22.Presnell K, Bearman SK, Stice E. Risk factors for body dissatisfaction in adolescent boys and girls: a prospective study. Int J Eat Disord. 2004;36:389–401. doi: 10.1002/eat.20045. [DOI] [PubMed] [Google Scholar]
- 23.Veron-Guidry S, Williamson DA, Netemeyer RG. Structural modeling analysis of body dysphoria and eating disorder symptoms in preadolescent girls. Eat Disord. 1997;5:15–27. [Google Scholar]
- 24.Fulkerson JA, Strauss J, Neumark-Sztainer D, Story M, Boutelle K. Correlates of psychosocial well-being among overweight adolescents: the role of the family. J Consult Clin Psychol. 2007;75:181–186. doi: 10.1037/0022-006X.75.1.181. [DOI] [PubMed] [Google Scholar]
- 25.Kostanski M, Fisher A, Gullone E. Current conceptualisation of body image dissatisfaction: have we got it wrong? J Child Psychol Psychiatry. 2004;45:1317–1325. doi: 10.1111/j.1469-7610.2004.00315.x. [DOI] [PubMed] [Google Scholar]
- 26.Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB. How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol. 1996;143:228–239. doi: 10.1093/oxfordjournals.aje.a008733. [DOI] [PubMed] [Google Scholar]
- 27.Prentice AM, Jebb SA. Beyond body mass index. Obes Rev. 2001;2:141–147. doi: 10.1046/j.1467-789x.2001.00031.x. [DOI] [PubMed] [Google Scholar]
- 28.Paradis G, Lambert M, O’Loughlin J, Lavallee C, Aubin J, Berthiaume P, et al. The Quebec Child and Adolescent Health Survey: design and methods of a cardiovascular risk factor survey for youth. Can J Cardiol. 2003;19:523–531. [PubMed] [Google Scholar]
- 29.Preville M, Potvin L, Boyer R. The structure of psychological distress. Psychol Rep. 1995;77:275–293. doi: 10.2466/pr0.1995.77.1.275. [DOI] [PubMed] [Google Scholar]
- 30.Miller AC, Gordon RM, Daniele RJ, Diller L. Stress, appraisal, and coping in mothers of disabled and nondisabled children. J Pediatr Psychol. 1992;17:587–605. doi: 10.1093/jpepsy/17.5.587. [DOI] [PubMed] [Google Scholar]
- 31.Riddle AS, Blais MR, Hess U. A Multi-Group Investigation of the CESD’s Measurement Structure Across Adolescents, Young Adults and Middle-Aged Adults. Scientific Series. Centre interuniversitaire de recherche en analyse des organisations; Montreal: 2002. [Google Scholar]
- 32.Preville M, Cote G, Boyer R, Hebert R. Detection of depression and anxiety disorders by home care nurses. Aging Ment Health. 2004;8:400–409. doi: 10.1080/13607860410001725009. [DOI] [PubMed] [Google Scholar]
- 33.Bandura A. Social Learning Theory. viii. Prentice Hall; Englewood Cliffs, NJ: 1977. p. 247. [Google Scholar]
- 34.Stunkard AJ, Faith MS, Allison KC. Depression and obesity. Biol Psychiatry. 2003;54:330–337. doi: 10.1016/s0006-3223(03)00608-5. [DOI] [PubMed] [Google Scholar]
- 35.Byrne BM. Structural Equation Modeling with LISREL, PRELIS, and SIMPLIS: Basic Concepts, Applications, and Programming. xiii. L Erlbaum Associates; Mahwah, NJ: 1998. p. 412. [Google Scholar]
- 36.Holmbeck GN. Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: examples from the child-clinical and pediatric psychology literatures. J Consult Clin Psychol. 1997;65:599–610. doi: 10.1037//0022-006x.65.4.599. [DOI] [PubMed] [Google Scholar]
- 37.Hu L, Bentler PM. Cutoff criteria for fit indeces in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Model. 1999;6:1–55. [Google Scholar]
- 38.ter Bogt TF, van Dorsselaer SA, Monshouwer K, Verdurmen JE, Engels RC, Vollebergh WA. Body mass index and body weight perception as risk factors for internalizing and externalizing problem behavior among adolescents. J Adolesc Health. 2006;39:27–34. doi: 10.1016/j.jadohealth.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 39.Sjoberg RL, Nilsson KW, Leppert J. Obesity, shame, and depression in school-aged children: a population-based study. Pediatrics. 2005;116:e389–e392. doi: 10.1542/peds.2005-0170. [DOI] [PubMed] [Google Scholar]
- 40.Ozmen D, Ozmen E, Ergin D, Cetinkaya AC, Sen N, Dundar PE, et al. The association of self-esteem, depression and body satisfaction with obesity among Turkish adolescents. BMC Public Health. 2007;7:80. doi: 10.1186/1471-2458-7-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Daniels J. Weight and weight concerns: are they associated with reported depressive symptoms in adolescents? J Pediatr Health Care. 2005;19:33–41. doi: 10.1016/j.pedhc.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 42.Richardson LP, Davis R, Poulton R, McCauley E, Moffitt TE, Caspi A, et al. A longitudinal evaluation of adolescent depression and adult obesity. Arch Pediatr Adolesc Med. 2003;157:739–745. doi: 10.1001/archpedi.157.8.739. [DOI] [PubMed] [Google Scholar]
- 43.Levine MP, Smolak L. Media as a context for the development of disordered eating. In: Smolak L, Levine MP, editors. Developmental Psychopathology of Eating Disorders: Implications for Research, Prevention, and Treatment. Earlbaum Associates; Hillsdale, NJ: 1996. pp. 235–257. [Google Scholar]
- 44.Santos M, Richards CS, Bleckley MK. Comorbidity between depression and disordered eating in adolescents. Eat Behav. 2007;8:440–449. doi: 10.1016/j.eatbeh.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 45.Hasler G, Pine DS, Kleinbaum DG, Gamma A, Luckenbaugh D, Ajdacic V, et al. Depressive symptoms during childhood and adult obesity: the Zurich Cohort Study. Mol Psychiatry. 2005;10:842–850. doi: 10.1038/sj.mp.4001671. [DOI] [PubMed] [Google Scholar]