Abstract
Purpose
To identify trajectories of smoking behaviors of a cohort of youth followed through young adulthood from 2000 to 2013.
Design
The Minnesota Adolescent Community Cohort study, a population-based cohort study.
Setting
Nationwide, originating in Midwest U.S.
Subjects
Cohort of youth surveyed for 14 years beginning at ages 12–16 (n=4241 at baseline; 59% recruitment rate).
Measures
Main variable of interest was number of days smoked in past 30 days. Also included time varying and time invariant covariates.
Analysis
We utilized growth mixture modeling to group individuals into trajectories over time.
Results
We identified five distinct trajectories: Non-Smokers (59.5%), Early Onset Regular Smokers (14.2%), Occasional Smokers (11.5%), Late Onset Regular Smokers (9.4%), and Quitters (5.3%). Adjusted models showed that early- and late-onset regular smokers (compared to non-smokers) had lower odds of attending or graduating from a four-year college (p<.05). Participants in all smoking classes compared to non-smokers had greater odds of having more close friends who smoked (p<.05).
Conclusions
Our results show that individuals in their teens through young adulthood can be classified into five smoking trajectories. More people in this age range remained abstainers than found in most previous studies; however, a sizable group was identified as regular smokers by the time they reached young adulthood. Interventions targeted at teens, including those that address social and environmental influences, are clearly still needed to prevent escalation of smoking as they move toward young adulthood.
Keywords: Cigarettes, smoking, young adults, trajectory, longitudinal
PURPOSE
Cigarette smoking among adolescents and young adults continues to be a public health problem in the U.S. Most adult smokers initiate smoking during their teen or young adult years.1–3 Identifying and tracking smoking patterns among individuals as they move from adolescence through young adulthood is important for targeting interventions to smokers as well as implementing prevention strategies to reduce uptake of smoking. Cohort studies are ideal for this as they can allow for examination of trajectories of smoking behaviors through developmental smoking stages, taking into account temporal factors that may affect any given cohort.
Numerous cohort studies have examined smoking trajectories across the adolescent years, e.g., 4–6 but fewer have examined smoking behaviors from adolescence through young adulthood. Among the studies that assessed participants from early adolescence (e.g., age 12 or 13) through young adulthood (e.g., 20s or 30s), the number and type of trajectories identified vary considerably. Researchers have identified three to six trajectories to characterize change in smoking behaviors from early teens to the young adult years.7–13. The trajectory groups vary in size and the labels used to describe them also vary across studies. Most have identified a fairly large non-smoker or abstainer trajectory, and many have identified smaller trajectories labeled as early starters, late starters, and experimenters/triers.
Differences in the results across studies can likely be attributed to variations in the: (1) sample used, (2) the number of data collection time points, (3) types of smoking measures utilized, and (4) analytic methods. The studies limited to small samples from one city identified three or four trajectories12–13 while the rest identified five or six. The studies that included more than one city still varied considerably in the type and size of the samples—some included nationwide samples 9–10 and others were limited to a few counties or states. 7–8, 11 The number of data collection time points ranged from three9 to fifteen12 with most having 4–6 data collection points. Although most studies used some type of quantity-frequency measure of smoking (e.g., number of cigarettes per day multiplied by number of days smoked in last 30) to identify trajectories, the specific measures varied considerably. Similarly, although all the studies utilized growth curve modeling to identify trajectories, different types of statistical software (i.e., MPlus14; SAS15 Proc Traj) and slightly different types of models were used.
Although these studies provide important information on the various smoking behavior trajectories that can be identified, the inconsistent methods and results along with several study limitations prevent drawing clear conclusions. Having a small number of data collection points with large gaps in time between these data collection points is common and applies specifically to two studies that included nationwide samples.9–10 In addition, the studies limited to one or two cities or counties may have limited generalizability.7–8, 13–14 Most of the studies also used no data beyond 2005. Results of these studies may not be as relevant as more recent ones, particularly given the continuing changing culture around smoking such as bans on smoking in many indoor and outdoor public places.
In this study, we addressed some of the key limitations in previous studies to identify trajectories of smoking behaviors of a cohort of youth followed through young adulthood. We included numerous data collection points with small time intervals, more recent data than previous studies, and data from across the U.S. Participants were first surveyed in 2000 when they were aged 12–16 and were subsequently surveyed every six months or annually for 14 years through 2013. The community-based randomly selected cohort originates from multiple U.S. states and expanded to many states as the cohort matured. We used latent growth curve mixture modeling. Our results provide information on initiation of, quitting, and other variations in smoking during this crucial developmental period and during changing societal norms pertaining to smoking.
METHODS
The data used in this study are part of the Minnesota Adolescent Community Cohort (MACC) study, a population-based observational cohort study. The University of Minnesota Institutional Review Board approved this study.
Design/Sample
Sampling methods and the full study design for MACC are described in detail in a previous paper.16 In brief, 3636 youth (12 to 16 years old) who lived in Minnesota were recruited in 2000–2001. The state was divided into 129 geopolitical units (GPUs) and youth were recruited from 60 randomly selected GPUs. In addition, 605 youth of the same ages were recruited from four comparison states (Kansas, Michigan, North Dakota and South Dakota). Within each selected GPU, Clearwater Research Inc. used modified random digit dialing, probability and quota sampling to recruit an even distribution of participants by age. The overall recruitment rate was 59%. Participants were surveyed through computer assisted telephone interviews (CATI) every 6 months through 2007–2008 and then annually between 2008 and 2013 using the phone numbers provided by the participants (including mobile phone numbers). There were a total of 18 rounds of the survey (n=2420 at round 18; see analysis section for information on handling of missing data). By the 18th round, participants resided in 47 states and 4 countries (with 43% in Midwestern U.S.). For these analyses we used data from all rounds, aligning the data by age. We used data from when the participants were ages 12, 14, 16, 18, 20, 22, and 24 (we excluded ages 25–28 due to limited participants at these ages). Our sample size was 4,241.
Measures
Our primary measure of interest was number of days smoked in past 30 days, a continuous variable from 0 to 30. This was measured at each round of the survey. Several covariates, both time-invariant and time-varying, that have been shown in numerous studies to be associated with smoking behaviors were included. Time invariant measures were sex, age cohort (established at baseline, ranging from ages 12 to 16), race/ethnicity (white vs. other), parents’ highest education level at baseline considering both parents (4-year college degree or higher vs. no 4-year college degree), and participant’s highest education level obtained between the ages of 21 to 28 (4-year college student/graduate vs. no 4-year college). Because of a fair amount of missing data for participant education (primarily due to attrition) as well as for some of the other covariates, we conducted imputation analyses using data from all our measures across all ages (see analysis section). The time-varying measures were number of four closest friends who smoke (continuous measure 0–4) and parent smoking (0=neither parent smokes; 1=one or both parents smoke). For both measures we used values at each of the ages (12, 14, 16, 18, 20, 22, 24). Because the complex analytic models were not able to accommodate separate values for each age, we created two average measures. One measure averaged across ages 12–18, and the second averaged across ages 20–24. Although using average measures limits variation across the age span, the two measures are supported conceptually, with parent and friend influences likely differing markedly before and after youth enter young adulthood (at about age 18).
Analysis
Variable creation and descriptive statistics were conducted in SAS 9.3.15 Trajectory analyses was conducted with MPLUS Version 7.14 We utilized latent growth curve mixture models that group individuals into clusters over time based on the main measure (number of days smoked in last 30) using a zero-inflated Poisson distribution to account for the large number of zeroes in our smoking days variable. We first computed unadjusted models with 2, 3, 4, 5, and 6 classes to identify the best fitting model based on standard statistical measures (Bayesian Information Criterion [BIC], adjusted BIC, entropy, likelihood ratio test) as well as size of classes and interpretability. We then computed an adjusted model with the same number of trajectories as in the best fitting unadjusted model but including all covariates. In this adjusted model, maximum likelihood was used to accommodate msissing data on the outcome over time (loss to follow-up). Imputation was used to account for missing data among the covariates (five datasets were utilized). The number of missing data points for covariates were: sex=0, race/ethnicity=3, parent education=829, participant education=1904, friend smoking (ages 12–18)=30, friend smoking (ages 20–24)=905, parent smoking (ages 12–18)=30, and parent smoking (ages 20–24)=2607. There were no differences at baseline between cases where we imputed data (n=3113) and cases where we did not (1128) for sex or parent smoking, but cases with imputed data were more likely to be non-white and have more friends that smoke. To compare participants across classes for each covariate we used odds ratios (with 95% confidence intervals).
RESULTS
Descriptive statistics of all variables are included in Table 1. Approximately half of the sample was female and 85% was white. Just over half of participants’ parents had a college degree, and nearly 60% of participants had attended or graduated from a four-year college. About 60% of participants reported that none of their close friends smoked and about two-thirds reported that neither parent smoked (at baseline).
Table 1.
Descriptive statistics (n=4241)
| Percent (n) | |
|---|---|
|
| |
| Sex | |
| Male | 49.4 (2093) |
| Female | 50.7 (2148) |
| Age cohorta | |
| 12 | 19.7 (836) |
| 13 | 20.4 (863) |
| 14 | 19.9 (844) |
| 15 | 20.1 (851) |
| 16–17 | 20.0 (847) |
| White | 84.8 (3593) |
| Parent education (highest level) | |
| College degree or higher | 54.2 (1850) |
| No college degree | 45.8 (1562) |
| Participant education (highest level) | |
| 4-year college student/graduate | 57.6 (1345) |
| No 4-year college | 42.5 (992) |
| Number of friends who smokeda | |
| 0 | 61.1 (25.83) |
| 1 | 17.0 (718) |
| 2 | 10.7 (451) |
| 3 | 5.0 (210) |
| 4 | 6.3 (266) |
| Parent smokinga | |
| One or both smoke | 34.1 (1446) |
| Neither smoke | 65.9 (2794) |
At baseline
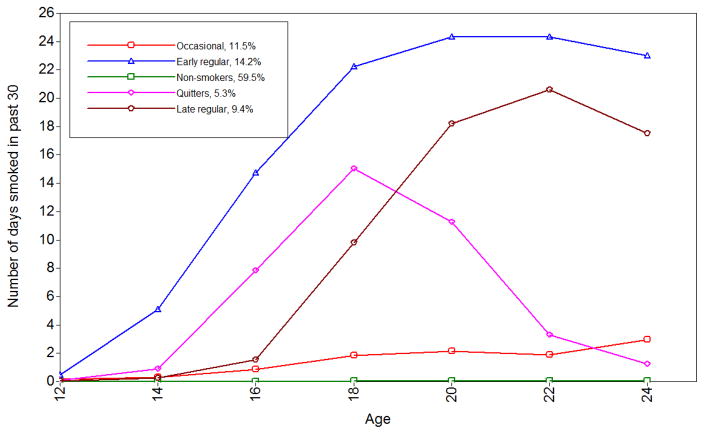
For the unadjusted analyses, we chose the 5-class model as the best fitting. Although the 6-class model had a lower BIC and adjusted BIC, the likelihood ratio test comparing the 5- and 6-class models indicated that the 5-class model was better fitting (Table 2). The 5-class model also had good entropy (0.85) and only one relatively small class (5%). The trajectory classes for the 5-class model are depicted in Figure 1. We assigned labels to the classes as follows: the largest trajectory class was the Non-Smokers (59.5%); the next largest trajectory class was the Early Onset Regular Smokers (14.2%), followed by the Occasional Smokers (11.5%), the Late Onset Regular Smokers (9.4%), and finally the Quitters (5.3%).
Table 2.
Latent class growth curve model fit statistics
| Number of classes | BIC | Adjusted BIC | Entropy | Smallest class size | Likelihood ratio text (p-value)a |
|---|---|---|---|---|---|
| 2 | 56057 | 56025 | .41 | 44% | 0.0 |
| 3 | 52140 | 52096 | .39 | 24% | 0.04 |
| 4 | 47845 | 47788 | .86 | 11% | 0.02 |
| 5 | 45718 | 45649 | .85 | 5% | 0.0002 |
| 6 | 44569 | 44485 | .88 | 4% | 0.60 |
Compares model with the model with one less class (p<.05 indicates model fits better than model with one less class)
Figure 1.
Five-class model smoking trajectory model
In the adjusted model (Table 3), with the largest class (Non-Smokers) used as the referent, five of the independent variables were significant. White participants (vs. other races) had over twice the odds of being early onset regular smokers than non-smokers, and 1.6 greater odds of being occasional smokers. Early- and late-onset regular smokers (compared to non-smokers) had lower odds of attending or graduating from a four-year college. Participants in all smoking classes compared to the non-smoking class had greater odds of having more close friends who smoked. Compared to non-smokers, occasional smokers had 1.7 greater odds, quitters had over twice the odds, late-onset regular smokers had 1.7–3.0 greater odds, and early-onset regular smokers had over 3.0 greater odds of having more friends who smoke. The number of friends who smoked when the participant was aged 12–18 (compared to aged 20–24) appears to have slightly more influence on smoking behavior for all smoking trajectory classes except late-onset regular smokers. For example, early-onset regular smokers (compared to non-smokers) had 3.8 greater odds of having more friends who smoked as reported at ages 12–18 compared to 3.5 greater odds as reported at ages 20–24.
Table 3.
Adjusted 5-class latent growth curve model: Smoking trajectory classes by covariates
| Covariates | Smoking Trajectory | ||||
|---|---|---|---|---|---|
| Non- smokers (59.0%) | Occasional smokers (11.7%) | Quitters (5.4%) | Late onset regular (10.4%) | Early onset regular (13.4%) | |
| Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | Odds ratio (95% CI) | ||
| White (vs. other races) | Ref | 1.61 (1.10, 2.37) | 1.43 (0.83, 2.47) | 1.33 (0.88, 2.00) | 2.06 (1.27, 3.33) |
| Male | Ref | 1.12 (0.88, 1.42) | 0.94 (0.66, 1.36) | 1.22 (0.92, 1.62) | 1.10 (0.80, 1.49) |
| Parent education: college degree or higher | Ref | 1.16 (0.89, 1.53) | 1.36 (0.89, 2.06) | 1.18 (0.88, 1.60) | 1.30 (0.92, 1.84) |
| Participant education: 4-year college student/grad or higher | Ref | 1.00 (0.75, 1.35) | 0.97 (0.60, 1.56) | 0.52 (0.36, 0.73) | 0.51 (0.31, 0.86) |
| Number of friends who smoked (measured at ages 12– 18) | Ref | 1.70 (1.46, 1.97) | 2.87 (2.29, 3.59) | 1.68 (1.41, 2.01) | 3.76 (3.05, 4.63) |
| Number of friends who smoked (measured at ages 20– 24) | Ref | 1.67 (1.47, 1.91) | 2.17 (1.78, 2.64) | 2.99 (2.57, 3.49) | 3.47 (2.89, 4.16) |
| Parent smokes: one or both (measured at ages 12–18) | Ref | 1.14 (0.80, 1.63) | 1.04 (0.59, 1.84) | 1.17 (0.79, 1.71) | 1.64 (1.11, 2.44) |
| Parent smokes: one or both (measured at ages 20–24) | Ref | 0.94 (0.52, 1.69) | 1.08 (0.43, 2.72) | 0.82 (0.42, 1.58) | 0.65 (0.35, 1.21) |
Boldface indicates statistical significance (p<.05)
CI= Confidence Interval
DISCUSSION
We examined smoking patterns from adolescence to young adulthood among a community cohort, identifying five distinct trajectories. Considering the seven similar previous studies7–13 along with the current study, four studies have now identified five distinct trajectories of smoking from the early teen years to the 20s or early 30s.7–8, 10 The types of trajectories identified are somewhat similar across these four studies. All found a fairly large non-smoking group and two medium-sized groups of occasional/light smokers and late-onset regular/stable smokers. All but one of the studies found a small group of quitters or “decreasers” and a relatively small group of early-onset regular/stable smokers. Given that our study along with three previous studies found a similar number and types of trajectories, some consensus seems to be building on identifying smoking typologies for the teen to young adult years. The overall agreement between our results and those from several previous studies despite differences in time frame, smoking measures, type and size of the samples, number of data collection points, and analytic techniques is noteworthy.
One key difference in our findings compared to previous studies is the size of the non-smoking trajectory. Our non-smoking group was larger than all but one of the previous studies we identified. The clear distinction of a quitting group is also encouraging. These results might be expected given decreases in smoking rates nationwide in recent years among teens and young adults.2,18 Nevertheless, the second largest trajectory was the early onset regular smoking group. And considering the early and late onset regular smoking trajectories together indicated that a quarter of our participants were regular smokers by early adulthood, which is only slightly smaller than most previous studies.
Our study has the advantage of having data collection time points at short intervals (6-months or 1-year) and over a long time period (14 years). Frequent data collection time points allows for identifying more subtle changes in smoking patterns, an advantage that is particularly important for the teen and young adult years when smoking habits are often not well established. Only one of the previous studies we identified had a similar number of time points (n=15; but it was conducted in only one community12 so it is difficult to compare results between that study and ours. Our study is also one of the few that used a community-based cohort versus a school-based cohort. A community cohort has the benefit of potentially reaching individuals not enrolled or present in school at the time of the surveys. The two most recent of previous studies also used community-based samples;7,10 again, the similar results found in these and our study perhaps points to a trend in identifying five smoking trajectories for adolescents through adulthood.
Our study is unique in including time-varying covariates in the analyses. We measured peer and parent smoking across the time span of the study. Due to complexities in modelling effects of time-varying covariates in the already complex trajectory models, we collapsed responses to two time points. Our results suggest that having more close friends who smoke was associated with being in all of the smoking trajectories (compared with non-smokers) throughout the ages we studied, particularly when comparing regular smokers to non-smokers. The covariates examined in previous studies vary considerably so it is difficult to compare results, although several of the studies found peer smoking to be associated with belonging to a smoking versus non-smoking trajectory.8,10 This is also consistent with many studies on the factors that affect smoking behaviors of youth and young adults.17 Although it may seem counterintuitive that quitting smoking is associated with more friends who smoke, this association may be secondary to the stronger likelihood of smoking (a pre-condition to quitting) if more friends smoke. Also, parent smoking, frequently found to be associated with adolescent uptake, was specifically associated with early onset regular smoking, the largest smoking class and possibly the most intractable in terms of quitting. This association might be related to access to cigarettes. The effects of covariates across time provides a more nuanced picture of adolescent and young adult smoking, and identifies important points for intervention for various smoking patterns. Family-based interventions as reviewed by Thomas et al. 19 showed particular effectiveness in preventing uptake of smoking, though primarily delivered to young adolescents. Community-based interventions, designed to affect a broader range of ages through social networks, were also shown to be effective in reducing onset of smoking but not cessation.20 A review of long-term outcomes of school-based smoking interventions, largely focused on peer influences, showed little long-term effects on smoking rates.21 Promising interventions to increase smoking cessation among young adults are using social branding or social media. 22–24
Considering the time invariant covariates we included in the models, we found white participants compared to non-whites were more likely to be early onset regular smokers and occasional smokers (compared to non-smokers). Because our sample had a large majority of white participants, comparisons with other studies as well as generalizing to larger populations is limited. Finally, those with some exposure to four-year colleges were less likely to be regular smokers, either early or late onset, suggesting the college environment may be protective against becoming a regular smoker. Encouraging young adults to seek a formal education beyond high school may have health benefits in addition to career and financial benefits.
Our results should be considered in light of several limitations. All data are self-reported and could be affected by social desirability bias; however, telephone surveys are an accepted form of data collection for health behaviors including smoking. Although our sample was community-based which has a broader reach than school-based samples, a large portion of our participants resided in the Midwestern U.S. and most were white. This limits generalizability to other geographic regions particularly those with more racial/ethnic diversity. In addition, the proportion whose parents had at least a college degree was 54% which is higher than comparable estimates for Minnesota and the US (36% and 30% respectively for highest education level among adults ages 35–44 in 2009; http://factfinder.census.gov/). The rather large non-smoking trajectory we identified may be partly explained by the higher parental education of our sample given that educational levels tend to be inversely associated with smoking rates. Furthermore, our smoking measure captured frequency of smoking (number of days smoked in past 30 days) but not number of cigarettes smoked on those days. Although measures that capture both frequency and quantity of smoking were used in most previous studies, we chose to use number of days smoked for ease of interpretation of results. Also, there was some attrition from the study over time as is found in all cohort studies. There was also missing data for several covariates for which we used multiple imputation to address. Finally, not all potential covariates were included in the models such as use of other tobacco and nicotine-delivery products, or environmental influences such as smoking bans.
Our study provides an updated picture of the smoking trajectories of teens as they mature into young adults. We collected data from 2000–2013 in short time intervals and used the latest in modelling techniques to identify five distinct trajectories. Our results show that more people in this age range remained abstainers than found in most previous studies and a small group quit smoking by age 24; however, a sizable group were identified as regular smokers by the time they reached young adulthood. Interventions targeted at teens are clearly still needed to prevent escalation of smoking as they move toward young adulthood. Peer influences on smoking behaviors, more so than parental influences, appear to be particularly important to consider. Future studies taking into account potential environmental factors, such as smoking bans, that may affect smoking trajectories are also recommended.
SO WHAT?
What is already known on this topic?
Studies have identified various smoking trajectories for adolescents as they move to young adulthood but the number of trajectories has varied from three to six, and types of descriptions of these trajectories also have varied.
What does this article add?
We collected more recent data at short time intervals and used the latest in modelling techniques to identify five distinct trajectories among a cohort followed from ages 12 to 24. Trajectories included a large group of Non-Smokers (60%), two groups of regular smokers (Early Onset=14%; Late Onset=9%), Occasional Smokers (12%) and Quitters (5%).
What are the implications for health promotion practice or research?
Results of the study suggest that a larger proportion of young people are never taking up smoking compared to most previous studies, but nearly a quarter were identified as regular smokers by the time reached young adulthood. Interventions targeted at teens are clearly still needed to prevent them from becoming regular smokers as they move into their young adult years and beyond.
Acknowledgments
This work was supported by a grant from the National Cancer Institute at the National Institutes of Health (R01-CA086191; Jean Forster, PI)
Footnotes
Declaration of Conflicting Interests
The authors declare that there is no conflict of interest.
References
- 1.Freedman KS, Nelson NM, Feldman LL. Smoking initiation among young adults in the United States and Canada, 1998–2010: A systematic review. Prev Chronic Dis. 2012:9. [PMC free article] [PubMed] [Google Scholar]
- 2.Miech RA, Johnston LD, O’Malley PM, et al. Monitoring the Future National Survey Results on Drug Use, 1975–2014: Volume I, Secondary School Students. Ann Arbor Institute for Social Research, The University of Michigan; 2015. [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. Contract No.: HHS Publication No. (SMA) 13–4795. [Google Scholar]
- 4.Bernat DH, Erickson DJ, Widorne R, et al. Adolescent smoking trajectories: results from a population-based cohort study. J Adolesc Health. 2008;43(4):334–340. doi: 10.1016/j.jadohealth.2008.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Colder CR, Mehta P, Balanda K, et al. Identifying trajectories of adolescent smoking: An application of latent growth mixture modeling. Health Psychol. 2001;20(2):127–135. doi: 10.1037//0278-6133.20.2.127. [DOI] [PubMed] [Google Scholar]
- 6.Karp I, O’Loughlin J, Paradis G, et al. Smoking trajectories of adolescent novice smokers in a longitudinal study of tobacco. Ann Epidemiol. 2005;15(6):445–452. doi: 10.1016/j.annepidem.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 7.Brook DW, Brook JS, Zhang CS, Whiteman M, Cohen P, Finch SJ. Developmental trajectories of cigarette smoking from adolescence to the early thirties: Personality and behavioral risk factors. Nicotine Tob Res. 2008;10(8):1283–1291. doi: 10.1080/14622200802238993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chassin L, Presson CC, Pitts SC, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood in a Midwestern community sample: Multiple trajectories and their psychosocial correlates. Health Psychol. 2000;19(3):223–231. [PubMed] [Google Scholar]
- 9.Costello DM, Dierker LC, Jones BL, Rose JS. Trajectories of smoking from adolescence to early adulthood and their psychosocial risk factors. Health Psychol. 2008;27(6):811–818. doi: 10.1037/0278-6133.27.6.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fuemmeler B, Lee C-T, Ranby KW, et al. Individual- and community-level correlates of cigarette-smoking trajectories from age 13 to 32 in a U.S. population-based sample. Drug Alcohol Depend. 2013;132(1–2):301–308. doi: 10.1016/j.drugalcdep.2013.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Orlando M, Tucker JS, Ellickson PL, Klein DJ. Developmental trajectories of cigarette smoking and their correlates from early adolescence to young adulthood. J Consult Clin Psychol. 2004;72(3):400–410. doi: 10.1037/0022-006X.72.3.400. [DOI] [PubMed] [Google Scholar]
- 12.Riggs NR, Chou CP, Li CY, Pentz MA. Adolescent to emerging adulthood smoking trajectories: When do smoking trajectories diverge, and do they predict early adulthood nicotine dependence? Nicotine Tob Res. 2007;9(11):1147–1154. doi: 10.1080/14622200701648359. [DOI] [PubMed] [Google Scholar]
- 13.White HR, Pandina RJ, Chen PH. Developmental trajectories of cigarette use from early adolescence into young adulthood. Drug Alcohol Depend. 2002;65(2):167–178. doi: 10.1016/s0376-8716(01)00159-4. [DOI] [PubMed] [Google Scholar]
- 14.Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2012. [Google Scholar]
- 15.SAS Institute Inc, editor. SAS/STAT 9.3 User’s Guide. Cary, NC: SAS Institute, Inc; 2011. [Google Scholar]
- 16.Forster J, Chen V, Perry C, et al. The Minnesota Adolescent Community Cohort Study: Design and baseline results. Prev Sci. 2011;12(2):201–210. doi: 10.1007/s11121-011-0205-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Villanti A, Boulay M, Juon HS. Peer, parent and media influences on adolescent smoking by developmental stage. Addict Behav. 2011;36(1–2):133–136. doi: 10.1016/j.addbeh.2010.08.018. [DOI] [PubMed] [Google Scholar]
- 18.Johnston LD, O’Malley PM, Bachman JG, et al. Monitoring the Future National Survey Results On Drug Use, 1975–2014: Volume 2, College Students and Adults Ages 19–55. Ann Arbor: Institute for Social Research, The University of Michigan; 2015. [Google Scholar]
- 19.Thomas RE, Baker P, Thomas BC, Lorenzetti DL. Family-based programmes for preventing smoking by children and adolescents. Cochrane Database Syst Rev. 2015;2:CD004493. doi: 10.1002/14651858.CD004493.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carson KV, Brinn MP, Labiszewski NA, et al. Community interventions for preventing smoking in young people. Cochrane Database Syst Rev. 2011:CD001291. doi: 10.1002/14651858.CD001291.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wiehe SE, Garrison MM, Christakis DA. A systematic review of school-based smoking prevention trials with long-term follow-up. J Adolesc Health. 2005;36:162–169. doi: 10.1016/j.jadohealth.2004.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Kalkhoran S, Lisha NE, Neilands TB, Jordan JW, Ling PM. Evaluation of bar and nightclub intervention to decrease young adult smoking in New Mexico. J Adolesc Health. 2016 Aug;59(2):222–229. doi: 10.1016/j.jadohealth.2016.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baskerville NB, Struik LL, Hammond D, et al. Effect of a mobile phone intervention on quitting smoking in a young adult population of smokers: randomized controlled trial study protocol. JMIR Res Protoc. 2015;4(1):e10. doi: 10.2196/resprot.3823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ramo DE, Thrul J, Delucchi KL, Ling PM, Hall SM, Prochaska JJ. The Tobacco Status Project (TSP): Study protocol for a randomized controlled trial of a Facebook smoking cessation intervention for young adults. BMC Public Health. 2015;15:897. doi: 10.1186/s12889-015-2217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]