Abstract
AIM
To evaluate the therapeutic role of double-balloon enteroscopy (DBE) in small bowel strictures and to propose a standard approach to small bowel strictures.
METHODS
Systematic review of studies involving DBE in patients with small bowel strictures. Only studies limited to small bowel strictures were included and those with ileo-colonic strictures were excluded.
RESULTS
In total 13 studies were included, in which 310 patients were dilated. The average follow-up time was 31.8 mo per patient. The complication rate was 4.8% per patient and 2.6% per dilatation. Surgery was avoided in 80% of patients. After the first dilatation, 46% were treated with re-dilatation and only 17% required surgery.
CONCLUSION
DBE-assisted dilatation avoids surgery in 80% of patients with small bowel strictures and is safe and effective. We propose a standardized approach to small bowel strictures.
Keywords: Double-ballloon enteroscopy, Dilatation, Small bowel stricture, Enteroscopy, Crohn’s disease, Systematic review
Core tip: At present there is a wealth of literature on the value of double-balloon enteroscopy (DBE) in the management of obscure gastrointestinal bleeding. However, there is only few data regarding its role in small bowel strictures and these patients often face surgery. In our study we show that DBE-assisted endoscopic balloon dilation offers safe and effective treatment of small bowel strictures. Surgery can be avoided in 80% of cases. Moreover, we propose a flow-chart representing a standard approach to small bowel strictures.
INTRODUCTION
Small bowel strictures are associated with major comorbidity and adequate management is therefore required. The aetiology of small bowel strictures is varied and includes Crohn’s disease (CD), post-surgical, ischemic, non-steroidal anti-inflammatory drugs (NSAIDs) induced, neoplastic and idiopathic[1,2]. Endoscopic access into the small bowel is not widely available. Hence, surgery has been the mainstay for treatment for small bowel strictures. However, surgery is associated with serious complications including bowel obstruction, intra-abdominal infections, wound infections, anastomotic leakages and fistulas. In patients with CD, the complication rate can be as high as 20%[3]. Besides the direct complications of surgery, there is also a > 70% chance of re-stricturing and it is known that multiple small intestinal resections can lead to short bowel syndrome and malnutrition[4-6]. Endoscopic balloon dilation (EBD) has been extensively described for fibrostenosing CD as it is minimally invasive and preserves intestinal length[7]. However, small bowel strictures are often more difficult to treat given their anatomical location.
In 2001 Yamamoto et al[8] first described double-balloon enteroscopy (DBE) as a new method to visualise the small bowel. Additionally, DBE provides the opportunity to perform therapeutics in the small bowel. Complications of DBE that have been described include bleeding, perforation and pancreatitis and however the rates are low ranging from 2%-18%[9,10]. There have been many publications regarding the diagnostic and therapeutic roles of DBE. However, most of these publications have been limited to obscure gastrointestinal bleeding and there is limited data on its role in the management of small bowel strictures[9,10]. Furthermore, previously published data are limited by small series and selection bias. Moreover, there is no clear data to recommend a safe and effective approach to endoscopic balloon dilatation (EBD) of small bowel strictures.
Our aim was to perform a systematic review of the published literature on DBE in small bowel strictures to evaluate the therapeutic role and safety of DBE in management of these strictures. Based on the reviewed data we aim to propose a standardized approach to EBD of small bowel strictures.
MATERIALS AND METHODS
A systematic search was performed in the Medline, PubMed and endbase databases including relevant references for English only articles using the following search terms: small bowel strictures, enteroscopy, balloon dilation/dilatation, double-balloon endoscopy. We only included small bowel strictures and excluded ileo-colonic anastomotic strictures. There were two papers from Hirai et al[11] that included the same patient population, so we excluded the first paper of Hirai et al[12] from 2010 as this data was updated in 2014. Moreover, Yamamoto’s paper from 2004 included overlapping data with the Sunada paper from 2005[13,14]. As the Yamamoto paper had a longer inclusion period with more patients we excluded the paper from Sunada et al[14]. Pinho et al[15] published a multicenter survey on the use of device-assisted enteroscopy in Portugal, which mentioned 6 cases of DBE-assisted dilatation. However, as these data are soley based on a survey and data with regard to efficacy and follow-up is lacking we decided to exclude this paper. In total, 13 original articles were included[2,11,13,16-25].
We performed a descriptive analysis studying patient demographics, stricture and disease characteristics, dilatation techniques, long-term and short-term complication and success rates. Short-term success was defined as improvement of symptoms after the dilatation. The endoscopic dilatation was only considered successful when the patient was free of surgery at the end of the follow-up period. Major complications such as bleeding, perforation, pancreatitis or any event leading to hospitalization were considered in the safety assessment. Long-term success was defined as the number of patients who did not need surgery during the follow-up period. Re-dilatation was reported separately. In the studies that also included diagnostic enteroscopies or other double-balloon assisted endoscopic interventions, only the data with regard to the dilatation cohort were included.
RESULTS
Study characteristics
General characteristics: In total 13 studies met the inclusion criteria mentioned above. The baseline study characteristics are listed in Table 1. All studies had a retrospective study design and the number of patients enrolled ranged from 8-156 patients. Fifty percent of the 626 patients (n = 316) that were included were not dilated. The reasons included technical difficulty reaching the stricture due to anatomical variations such as angulation or adhesions (n = 14) or once at the stricture, it was difficult to maintain a stable wire or scope position (n = 7). Other reasons were evidence of active inflammation at the stricture site which was then managed medically (n = 28), or the stricture was not obstructing and therefore not treated (n = 16) (Figure 1). In total, 581 dilatations were performed in the included 310 patients.
Table 1.
Descriptive analysis of the main variables in the studies
| Author | Year of publication | # patients | # patients undergoing dilatations | Total # strictures dilated | Aetiology stricture | Length stricture (cm) | FU (months) |
| Yamamoto et al[13] | 2004 | 23 | 6 | 6 | Mixed | NR | NR |
| Pohl et al[16] | 2006 | 19 | 9 | 13 | CD | ≤ 4 | 16 (4-26) |
| Ohmiya et al[17] | 2009 | 66 | 22 | 47 | Mixed | NR | 16 (2-43) |
| Despott et al[18] | 2011 | 11 | 9 | 18 | CD | < 5 | 20.5 (2-41) |
| Hayashi et al[19] | 2008 | 18 | 2 | 2 | NSAID | NR | NR |
| Hirai et al[11] | 2014 | 65 | 52 | 52 | CD | ≤ 5 | 41.8 ± 24.9 |
| Gill et al[20] | 2014 | 32 | 14 | 15 | Mixed | NR | 16 (3-60) |
| Irani et al[21] | 2012 | 13 | 12 | 17 | Mixed | ≤ 2 | 46 |
| Nishimura et al[22] | 2011 | 8 | 7 | 11 | Ischemic | ≤ 3 | 16 |
| Fukumoto et al[23] | 2007 | 156 | 31 | 50 | Mixed | NR | 11.9 (1-40) |
| Sunada et al[24] | 2016 | 99 | 85 | 291 | CD | < 5 | 41.9 |
| Kita et al[25] | 2006 | NR (at least 45) | 45 | 45 | Mixed | NR | NR |
| Kroner et al[2] | 2015 | 71 | 16 | 16 | Mixed | NR | NR |
| Total | 626 | 310 | 583 |
CD: Crohn’s disease; NSAIDS: Non-steroidal anti-inflammatory drugs; NR: Not reported.
Figure 1.
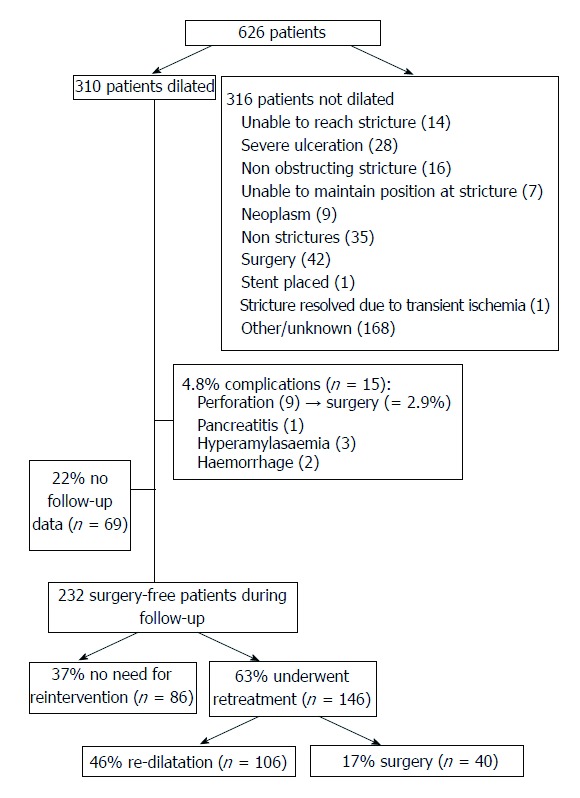
Study results. This flowchart summarizes the study results with the outcomes of the patients that were dilated.
Study heterogeneity: There was a significant heterogeneity among the studies and they differed in terms of study aims, patient population and dilatation techniques. However, all studies described at least the short-term success and complication rates of the EBD. Moreover, the enrolled patients differed between the studies: seven studies included all causes of small bowel strictures, whereas in four series the study population was limited to patients with CD, one series only described NSAID-related strictures and one series was limited to ischemic strictures. The length of the stricture varied but none of the studies included strictures above 5cm in length. The inclusion and exclusion criteria of the studies are reported in Table 2.
Table 2.
Inclusion and exclusion criteria of the included studies
| Author | Year of publication | Inclusion criteria | Exclusion criteria |
| Yamamoto et al[13] | 2004 | - Retrospective review of all DBEs | - NR |
| - Dilatation criteria NR | |||
| Pohl et al[16] | 2006 | - Known or suspected CD and proven or suspicious small bowel strictures | - Strictures > 5 cm or including significant angulation or severe active inflammation with ulcerations |
| - Dilatation criteria NR | |||
| Ohmiya et al[17] | 2009 | - Patients with SBO | - Acute obstruction with strangulation or suspected perforation |
| - The stricture was assumed to be restricted within narrow limits in the small bowel assessed by radiologic imaging | - A stricture with a deep open ulcer | ||
| - A second dilation session was only performed if obstructive symptoms recurred | |||
| Despott et al[18] | 2011 | - CD patients with small bowel stricture | - Strictures > 5 cm |
| - Dilatation criteria NR | |||
| Hayashi et al[19] | 2008 | - Retrospective case series of all patients who had undergone DBE | -NR |
| - In the case of a diaphragm-like stricture, all the strictures were dilated | |||
| Hirai et al[11] | 2014 | CD patients with: | - Stricture of the ileocolonic anastomosis |
| - Small bowel strictures causing obstructive symptoms | - Post-dilatation observation period < 6 mo | ||
| - Stricture length ≤ 5 cm | - Patients who did not meet dilatation criteria | ||
| - No associated fistula or abscess | |||
| - no deep ulcer | |||
| - No severe curvature of the stricture | |||
| Gill et al[20] | 2014 | - Retrospective review: All patients with suspected strictures in the small bowel undergoing DBE | - Patients with severely ulcerated or inflamed strictures |
| - Dilatation criteria NR | - Patients in whom the scope could not traverse the stricture | ||
| Irani et al[21] | 2012 | - Clinical and radiological evidence (CT or small bowel follow through) of small bowel obstruction | - Malignant strictures and masses found either at video capsule endoscopy or DBE |
| Nishimura et al[22] | 2011 | - Patients with ischemic enteritis and a segment of intestine that could not be passed by the enteroscope | - Deep ulcerations |
| - Dilation was indicated when there were symptoms of intestinal obstruction and evidence of caliber change by CT scan | |||
| Fukumoto et al[23] | 2007 | A stricture was defined by 1 or more of the following criteria: | -Asymptomatic patient (even when the endoscope did not pass through the stricture) |
| - DBE showed the internal diameter of the bowel lumen to be < 10 mm or the endoscope could not pass through the lesion | |||
| - The patient complained of obstructive symptoms | |||
| - Stricture was suggested or identified by other modalities. | |||
| Sunada et al[24] | 2016 | - Retrospective review of all DBEs | -NR |
| - Dilatation criteria NR | |||
| Kita et al[25] | 2006 | - Retrospective review of all DBEs | -NR |
| - Dilatation criteria NR | |||
| Kroner et al[2] | 2015 | - Retrospective review of consecutive patients who were found to have small bowel stricture at the time of DBE | - Malignant (appearance of) strictures |
| - Benign appearance of the stricture |
CD: Crohn’s disease; NR: Not reported; SBO: Small bowel obstruction; DBE: Double balloon enteroscopy.
Dilatation technique
Balloon characteristics: The details of the dilatation technique that was used are specified in Table 3. The controlled radial expansion (CRE) wire guided balloon dilator (Boston Scientific Corporation, Natick, Mass) was the most commonly used (at least 8/13 studies). Five papers did not specify the type of balloon that was used. Four studies reported a maximum dilatation diameter of 20 mm, whereas the other studies went up to 12 mm (one study), 13 mm (one study), 16.5 mm (one study) or 18 mm (two studies). In four studies the diameter was not reported. There was also some variability in the duration of each dilatation. Most studies dilated for 30-60 s, whereas in two studies the dilatation duration was up to 120 s per patient.
Table 3.
Technical details of dilatations
| Author | Year of publication | Balloon diameter (mm) | Duration of dilatation per stricture (s) | Type of balloon | Fluoroscopy | Sedation CS/ GA |
| Yamamoto et al[13] | 2004 | NR | NR | Boston Scientific, CRE | NR | CS |
| Pohl et al[16] | 2006 | Up to 20 | 120 | Boston Scientific, CRE | Yes | NR |
| Ohmiya et al[17] | 2009 | 8-20 | 60 | NR | NR | NR |
| Despott et al[18] | 2011 | 12-20 | 60 | Boston Scientific, CRE | No | CS and GA |
| Hayashi et al[19] | 2008 | NR | NR | Boston Scientific, CRE | NR | NR |
| Hirai et al[12] | 2014 | 12-18 | 30-120 | Boston Scientific, CRE | NR | CS |
| Gill et al[20] | 2014 | 10-16.5 | NR | Boston Scientific, CRE | No | CS or propofol |
| Irani et al[21] | 2012 | 10-18 | 30 or until waist effacement | NR | Yes | CS and GA |
| Nishimura et al[22] | 2011 | 8-12 | 30 (and 30 s interval) | Boston Scientific, CRE | Yes | CS |
| Fukumoto et al[23] | 2007 | NR | NR | NR | Yes | NR |
| Sunada et al[24] | 2016 | 8-20 | 30-60 | Boston Scientific, CRE | Yes | CS |
| Kita et al[25] | 2006 | NR | NR | NR | NR | NR |
| Kroner et al[2] | 2015 | 13 | NR | NR | NR | GA |
CS: Conscious sedation; GA: General anesthesia; CRE: Controlled radial expansion; NR: Not reported.
Fluoroscopy: Fluoroscopic guidance was used in five studies, whereas two studies performed the dilatation purely under direct vision. The other five papers did not make a remark regarding the use of fluoroscopy.
Sedation: In four studies all dilatations were done under conscious sedation, and in one study all dilatations were done under conscious sedation or propofol. In another five studies the method of sedation was not mentioned. Despott et al[18] used general anesthesia in 9 procedures, with midazolam and pethidine in 2 procedures and anesthesist-delivered propofol sedation in 1 procedure. Irani et al[21] used general anesthesia in seven patients and conscious sedation in 6 others.
Study outcomes
Follow-up: The follow-up duration was reported in 9 out of 13 studies and varied from 11.9 - 46.0 mo. In 68 patients (22%) there was no follow-up data, which was either not reported in the study or the patient was lost to follow-up. The total follow-up time was 7750.5 mo for 241 patients leading to an average follow-up time of 31.8 mo per patient.
Clinical efficacy: Among those who underwent EBD, 80% achieved long-term success without the need for surgery during follow-up (n = 192/241 patients). In total, 20% required surgery during the study-period (n = 49/241 patients), either because of a complication of the EBD (n = 9) or because of a relapse (n = 40).
Excluding those who needed surgery due to a complication of the EBD, 37% of patients did not need further treatment after the initial EBD. In total, 63% was retreated because of a relapse or underwent prophylactic re-dilatation. Unfortunately, one study with a high re-dilatation rate did not report the reason for re-dilatation and the relapse rate can therefore not be precisely reported[24]. Of the 146 patients who needed retreatment, 27% underwent surgery (n = 40) and 46% successfully underwent EBD (n = 106). The study results are summarized in Figure 1 below.
Complications: The complications are listed in Table 4. The total complication rate per patient was 4.8% (15/310 patients), whereas the total complication rate per dilatation was 2.6% (15/583 dilatations). This included 5 patients with a perforation, 3 patients with acute pancreatitis, 1 patient who suffered from hemorrhage that required blood transfusions and 3 patients with hyperamylasemia. The patient with pancreatitis recovered after a short hospital stay and the patients with perforations all underwent surgery.
Table 4.
Overview of endoscopic balloon dilation-associated complications per study
| Author | Complications | Type of complication | Complication rate per patient | Complication rate per dilatation | Short-term success2 (%) | Long-term success avoiding surgery2 (%) | Surgery2 (%) | Re-Dilatations23 (%) |
| Yamamoto et al[13] | NO | NA | 0% | 0% | 6/6 (100) | NR | NR | NR |
| Pohl et al[16] | NO | NA | 0% | 0% | 9/9 (100) | 6/9 (67) | 3/9 (33) | 2/9 (22) |
| Ohmiya et al[17] | NO1 | NA | 0% | 0% | 22/22 (100) | 18/22 (82) | 4/22 (18) | 3/22 (14) |
| Despott et al[18] | YES | Perforation (n = 1) | 11% | 5.6% | 8/9 (89) | 8/9 (89) | 1/9 (11) | 2/9 (22) |
| Hayashi et al[19] | NO | NA | 0% | 0% | 2/2 (100) | NR | NR | NR |
| Hirai et al[12] | YES | Haemorrhage (n = 1) | 12% | 12% | 48/52 (92.3) | 44/52 (85) | 8/52 (15) | 26/52 (50) |
| Acute pancreatitis (n = 1) | ||||||||
| Perforation (n = 1) | ||||||||
| Hyperamylasemia (n = 3) | ||||||||
| Gill et al[20] | YES | Perforation (n = 2) | 13% | 13% | 11/14 (79) | 11/14 (79) | 3/14(21) | 1/14 (7) |
| Irani et al[21] | YES | Perforation (n = 1) | 8% | 6% | 10/12 (83) | 10/12 (83) | 2/12 (15) | 2/12 (15) |
| Nishimura et al[22] | NO | NA | 0% | 0% | 6/7 (86) | 4/7 (60) | 3/7 (43) | 1/7 (14) |
| Fukumoto et al[23] | NO | NA | 0% | 0% | NR | 27/31 (87) | 4/31 (13) | 5/31 (16) |
| Sunada et al[24] | YES | Perforations (n = 4) | 6% | 2% | 80/85 (94) | 64/85 (75) | 21/85 (25) | 64/85 (75)4 |
| Bleeding (n = 1) | ||||||||
| Kita et al[25] | NO | NA | 0% | 0% | 45/45 (100) | NR | NR | NR |
| Kroner et al[2] | NO | NA | 0% | 0% | 16/16 (100) | NR | NR | NR |
| Total | Haemorrhage (n = 1) | 4.8% | 3% | 263/279 (94.3) | 192/241 (80) | 49/241 (20) | 106/241(44) | |
| Acute pancreatitis (n = 1) | ||||||||
| Perforation (n = 9) | ||||||||
| Hyperamylasemia (n = 3) | ||||||||
| Bleeding (n = 1) |
No complications mentioned in dilatation-cohort;
1 patient lost to follow-up;
Either because of a relapse or as prophylaxis;
No data reported on indication for repeat dilatation and relapse rate. NA: Not applicable; NR: Not reported.
DISCUSSION
In this systematic review we demonstrate that double-balloon assisted dilatation is a safe and effective treatment for small bowel strictures. Four out of five patients avoid surgery due to double-balloon assisted dilatation of their small bowel stricture in an average follow-up of 2.5 years per patient.
Small bowel strictures are associated with major comorbidity and usually require treatment. Surgery has been the main treatment option in the past. Moreover, the management of small bowel strictures, especially in CD, is often a clinical challenge because of the high recurrence rate and many patients need surgery more than once. Although surgery often results in symptomatic resolution, repeat surgery is often needed which can result in short bowel syndrome and malnutrition[26,27]. Our study showed that DBE-assisted balloon dilatation is effective in avoiding surgery as only 17% of patients required surgery due to a relapse.
In our study cohort, 47% of patients underwent re-dilatation during the follow-up period. It is known that strictures often recur, especially in CD[26,27]. Even after stricturoplasty, repeat surgery may be as high as 25% over a follow-up of 2.5 years[28]. In our study, surgery was avoided in 80% of cases.
Hirai et al[11] reported an unusually high repeat DBE rate (85.6%). This can be explained by the fact that their protocol included a routine re-examination and prophylactic re-intervention if a stricture was seen. In total 45 out of 52 successful EBD cases were re-examined to confirm the condition of the strictures after initial EBD. Of these 45 patients, 26 patients needed a secondary EBD of which 7 patients were asymptomatic. Sunada et al[24]. also reported a very high repeat DBE rate, but again they also performed repeat EBD in asymptomatic patients. They did not report how many patients actually needed retreatment because of a relapse. In the other studies, patients only underwent a repeat enteroscopy if they were symptomatic. There is currently no role for scheduled re-dilatation if patients are asymptomatic as there is no literature available to support scheduled re-dilatation. However, if patients are symptomatic re-dilatation would need to be considered.
In our study cohort a complication rate of 4.8% per patient and 2.6% per dilatation was demonstrated. This is comparable with previous studies. In 2007, Mensink et al[10] reported a complication rate of 4.3% in therapeutic double-balloon enteroscopic procedures. In the included study of Ohmiya et al[17] data of 668 DBE examinations were reported, of which there were 3 cases of complicating perforation that required surgery (0.45%). However, no complicating perforation occurred in patients during or after enteroscopic balloon dilation and these complications were therefore not included in our study cohort. In our cohort of 310 patients, nine patients (2.9%) needed surgery directly after the dilatation due to a perforation. Our reported rate of intestinal perforation is within the range of 0% to 3.7% reported in previous studies[26,27,29,30].
Known risk factors for perforation include adhered or angulated strictures, active inflammation and dilating to more than 15 mm[18,20]. Sunada et al[24] demonstrated that the surgery-free interval in patients with a fistula was significantly shorter than in patients without a fistula. Moreover, most of the included studies did not perform dilatation when there was active ulceration.
In this study we assess the role of DBE-assisted dilatation of small bowel strictures. The data on other modalities of enteroscopy including single balloon enteroscopy and spiral enteroscopy is very limited with only small numbers and limited follow-up. We therefore decided to focus our systematic review on DBE-assisted dilatation only. There is a large multicenter survey from Portugal on the use of device-assisted enteroscopy, which mentioned 6 cases of DBE-assisted dilatation with just one reported complication. This confirms the safety we also show in our study[15].
Endoscopic and surgical management of small bowel strictures are not mutually exclusive options. On the contrary, these two modalities complement each other as even patients who have undergone surgical resections in the past may still be considered for endoscopic therapy. In one of the studies in our systematic review, 10 of the 11 patients had undergone previous surgery and yet the procedure was successful in 9 of them[18].
The current study is limited by its retrospective design. Due to heterogeneity of the study designs and lack of randomized controlled trials it was not possible to perform a meta-analysis. However, this large systematic review includes a large patient group with a long average follow-up time of over 2.5 years per patient. Concomitant medical treatment was not evaluated, although we know this is important for preventing strictures and can influence the relapse-rate. Moreover, as the numbers are relatively small we could not analyze the outcomes stratified by disease. Finally, the published studies did not focus on multiple small bowel strictures. Therefore, based on this literature review we cannot analyze the outcomes of treatment of multiple small bowel strictures, nor can we comment on the optimal strategy to treat multiple small bowel strictures.
Recently, a clinical practice guideline to enteroscopy was published in Japan[31]. In this guideline the indications for enteroscopy-assisted balloon dilatation are discussed which include symptomatic strictures that are < 5 cm long and are not associated with active inflammation or fistula/abscesses. Although the indications to EBD are described in this guideline, the general, step-wise approach for the management of small bowel strictures is currently not available. A standardized approach is beneficial as it may reduce complication rates and therewith even further increase the beneficial effect of DBE-assisted balloon dilatation. Taking into account the known risk factors previously demonstrated in literature and discussed in the Japanese guideline we propose the algorithm demonstrated in Figure 2 as a standardized approach to small bowel strictures.
Figure 2.
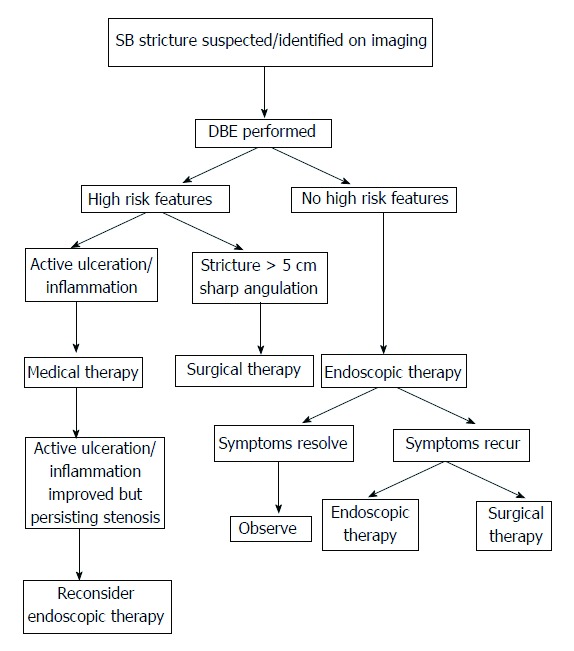
Suggested approach to small bowel. This algorithm proposes a standardized approach to small bowel strictures, taking into account the known risk factors previously demonstrated in literature.
In this algorithm we propose that at first high risk features such as active inflammation/ulceration, large stricture and sharp angulation should be considered. In case there are no high risk features endoscopic therapy can be performed safely. An illustration of endoscopic balloon dilatation is shown in Figure 3A-C. If the symptoms have resolved after endoscopic therapy no further dilatation is required and the patient should be observed. However, if symptoms do recur, endoscopic re-dilatation or finally surgery has to be considered.
Figure 3.
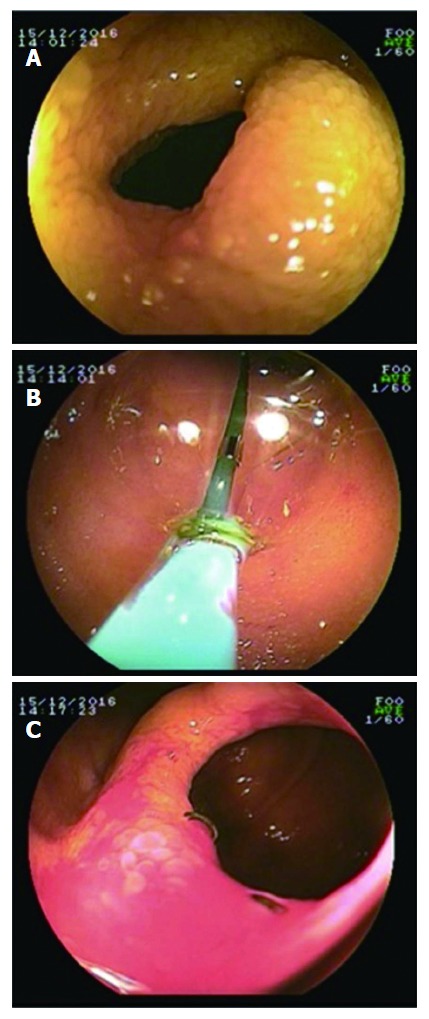
Double-balloon enteroscopy -assisted balloon dilatation. An example of a successful double-balloon enteroscopy (DBE)-assisted balloon dilatation is presented. A: shows the endoscopic image of a benign small bowel stricture in one of our patients. This patient was known with Crohn’s disease and had had prior small bowel surgery. She presented with obstructive symptoms and a fibrotic stricture at the side of the anastomosis. B: The stricture was dilated with DBE-assisted balloon dilation; C: Shows the anastomotic stricture after successful dilatation. This picture reveals the surgical staples at the anastomosis and there were no signs of active Crohn’s disease.
In conclusion, DBE is a safe and effective tool in the management of small bowel strictures and avoids unnecessary surgery in the majority of patients. DBE-assisted EBD should therefore be considered in all patients with small bowel strictures.
ARTICLE HIGHLIGHTS
Research background
At present there is a wealth of literature on the value of double-balloon enteroscopy (DBE) in the management of obscure gastrointestinal bleeding. However, there is only few data regarding its role in small bowel strictures. The management of small bowel strictures is complicated and these patients often face surgery, which has a huge impact on their quality of life.
Research motivation
In this study we aimed to evaluate the therapeutic role of DBE in small bowel strictures. In addition, we aimed to propose a standard approach to the management of small bowel strictures.
Research objectives
The main objective of this manuscript was to assess the efficacy and safety of DBE-assisted balloon dilatation of small bowel strictures. This is important as many of these patients often face surgery. The authors aimed to assess the role of DBE-assisted dilatation as an alternative for surgery.
Research methods
This study is a systematic review of published papers on DBE-assisted dilatation of small bowel strictures. Only studies limited to small bowel strictures were included and those with ileo-colonic strictures were excluded.
Research results
In total 13 studies were included, in which 310 patients were dilated. The average follow-up time was 31.8 mo per patient. The complication rate was 4.8% per patient and 2.6% per dilatation. Surgery was avoided in 80% of patients. After the first dilatation, 46% were treated with re-dilatation and only 17% required surgery.
Research conclusions
In this systematic review we demonstrate that double-balloon assisted dilatation is a safe and effective treatment for small bowel strictures. Four out of five patients avoid surgery due to double-balloon assisted dilatation of their small bowel stricture in an average follow-up of 2.5 years per patient. Moreover, we propose a flow-chart representing a standard approach to small bowel strictures.
Research perspectives
This research shows that double-balloon assisted balloon-dilatation is a safe and effective treatment for small bowel strictures and should be considered as a first treatment options. Future research is needed to explore the options of balloon-assisted enteroscopy in other device-assisted enteroscopy modalities.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Australia
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: All the authors declare that they have no competing interests.
Data sharing statement: No additional data are available.
Peer-review started: July 20, 2017
First decision: September 4, 2017
Article in press: October 17, 2017
P- Reviewer: Huang LY, Ogata H, Pinho R S- Editor: Qi Y L- Editor: A E- Editor: Huang Y
Contributor Information
Judith E Baars, AW Morrow Gastroenterology and Liver Centre, Royal Prince Alfred Hospital, Camperdown, Sydney NSW 2050, Australia.
Ruben Theyventhiran, AW Morrow Gastroenterology and Liver Centre, Royal Prince Alfred Hospital, Camperdown, Sydney NSW 2050, Australia.
Patrick Aepli, AW Morrow Gastroenterology and Liver Centre, Royal Prince Alfred Hospital, Camperdown, Sydney NSW 2050, Australia.
Payal Saxena, AW Morrow Gastroenterology and Liver Centre, Royal Prince Alfred Hospital, Camperdown, Sydney NSW 2050, Australia.
Arthur J Kaffes, AW Morrow Gastroenterology and Liver Centre, Royal Prince Alfred Hospital, Camperdown, Sydney NSW 2050, Australia. arthur@kaffes.com.
References
- 1.Jackson BT. Bowel damage from radiation. Proc R Soc Med. 1976;69:683–686. [PMC free article] [PubMed] [Google Scholar]
- 2.Kroner PT, Brahmbhatt BS, Bartel MJ, Stark ME, Lukens FJ. Yield of double-balloon enteroscopy in the diagnosis and treatment of small bowel strictures. Dig Liver Dis. 2016;48:446–448. doi: 10.1016/j.dld.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 3.Gardiner KR, Dasari BV. Operative management of small bowel Crohn’s disease. Surg Clin North Am. 2007;87:587–610. doi: 10.1016/j.suc.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 4.Lee EC, Papaioannou N. Minimal surgery for chronic obstruction in patients with extensive or universal Crohn’s disease. Ann R Coll Surg Engl. 1982;64:229–233. [PMC free article] [PubMed] [Google Scholar]
- 5.Parker MC, Wilson MS, Menzies D, Sunderland G, Clark DN, Knight AD, Crowe AM; Surgical and Clinical Adhesions Research (SCAR) Group. The SCAR-3 study: 5-year adhesion-related readmission risk following lower abdominal surgical procedures. Colorectal Dis. 2005;7:551–558. doi: 10.1111/j.1463-1318.2005.00857.x. [DOI] [PubMed] [Google Scholar]
- 6.Bellolio F, Cohen Z, MacRae HM, O’Connor BI, Victor JC, Huang H, McLeod RS. Strictureplasty in selected Crohn’s disease patients results in acceptable long-term outcome. Dis Colon Rectum. 2012;55:864–869. doi: 10.1097/DCR.0b013e318258f5cb. [DOI] [PubMed] [Google Scholar]
- 7.Saunders BP, Brown GJ, Lemann M, Rutgeerts P. Balloon dilation of ileocolonic strictures in Crohn’s disease. Endoscopy. 2004;36:1001–1007. doi: 10.1055/s-2004-825962. [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto H, Sekine Y, Sato Y, Higashizawa T, Miyata T, Iino S, Ido K, Sugano K. Total enteroscopy with a nonsurgical steerable double-balloon method. Gastrointest Endosc. 2001;53:216–220. doi: 10.1067/mge.2001.112181. [DOI] [PubMed] [Google Scholar]
- 9.Karstensen JG, Hendel J, Vilmann P. Endoscopic balloon dilatation for Crohn’s strictures of the gastrointestinal tract is feasible. Dan Med J. 2012;59:A4471. [PubMed] [Google Scholar]
- 10.Mensink PB, Haringsma J, Kucharzik T, Cellier C, Pérez-Cuadrado E, Mönkemüller K, Gasbarrini A, Kaffes AJ, Nakamura K, Yen HH, et al. Complications of double balloon enteroscopy: a multicenter survey. Endoscopy. 2007;39:613–615. doi: 10.1055/s-2007-966444. [DOI] [PubMed] [Google Scholar]
- 11.Hirai F, Beppu T, Takatsu N, Yano Y, Ninomiya K, Ono Y, Hisabe T, Matsui T. Long-term outcome of endoscopic balloon dilation for small bowel strictures in patients with Crohn’s disease. Dig Endosc. 2014;26:545–551. doi: 10.1111/den.12236. [DOI] [PubMed] [Google Scholar]
- 12.Hirai F, Beppu T, Sou S, Seki T, Yao K, Matsui T. Endoscopic balloon dilatation using double-balloon endoscopy is a useful and safe treatment for small intestinal strictures in Crohn’s disease. Dig Endosc. 2010;22:200–204. doi: 10.1111/j.1443-1661.2010.00984.x. [DOI] [PubMed] [Google Scholar]
- 13.Yamamoto H, Kita H, Sunada K, Hayashi Y, Sato H, Yano T, Iwamoto M, Sekine Y, Miyata T, Kuno A, et al. Clinical outcomes of double-balloon endoscopy for the diagnosis and treatment of small-intestinal diseases. Clin Gastroenterol Hepatol. 2004;2:1010–1016. doi: 10.1016/s1542-3565(04)00453-7. [DOI] [PubMed] [Google Scholar]
- 14.Sunada K, Yamamoto H, Kita H, Yano T, Sato H, Hayashi Y, Miyata T, Sekine Y, Kuno A, Iwamoto M, et al. Clinical outcomes of enteroscopy using the double-balloon method for strictures of the small intestine. World J Gastroenterol. 2005;11:1087–1089. doi: 10.3748/wjg.v11.i7.1087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pinho R, Mascarenhas-Saraiva M, Mão-de-Ferro S, Ferreira S, Almeida N, Figueiredo P, Rodrigues A, Cardoso H, Marques M, Rosa B, et al. Multicenter survey on the use of device-assisted enteroscopy in Portugal. United European Gastroenterol J. 2016;4:264–274. doi: 10.1177/2050640615604775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pohl J, May A, Nachbar L, Ell C. Diagnostic and therapeutic yield of push-and-pull enteroscopy for symptomatic small bowel Crohn’s disease strictures. Eur J Gastroenterol Hepatol. 2007;19:529–534. doi: 10.1097/MEG.0b013e328012b0d0. [DOI] [PubMed] [Google Scholar]
- 17.Ohmiya N, Arakawa D, Nakamura M, Honda W, Shirai O, Taguchi A, Itoh A, Hirooka Y, Niwa Y, Maeda O, et al. Small-bowel obstruction: diagnostic comparison between double-balloon endoscopy and fluoroscopic enteroclysis, and the outcome of enteroscopic treatment. Gastrointest Endosc. 2009;69:84–93. doi: 10.1016/j.gie.2008.04.067. [DOI] [PubMed] [Google Scholar]
- 18.Despott EJ, Gupta A, Burling D, Tripoli E, Konieczko K, Hart A, Fraser C. Effective dilation of small-bowel strictures by double-balloon enteroscopy in patients with symptomatic Crohn’s disease (with video) Gastrointest Endosc. 2009;70:1030–1036. doi: 10.1016/j.gie.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Hayashi Y, Yamamoto H, Taguchi H, Sunada K, Miyata T, Yano T, Arashiro M, Sugano K. Nonsteroidal anti-inflammatory drug-induced small-bowel lesions identified by double-balloon endoscopy: endoscopic features of the lesions and endoscopic treatments for diaphragm disease. J Gastroenterol. 2009;44 Suppl 19:57–63. doi: 10.1007/s00535-008-2277-3. [DOI] [PubMed] [Google Scholar]
- 20.Gill RS, Kaffes AJ. Small bowel stricture characterization and outcomes of dilatation by double-balloon enteroscopy: a single-centre experience. Therap Adv Gastroenterol. 2014;7:108–114. doi: 10.1177/1756283X13513995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Irani S, Balmadrid B, Seven G, Ross A, Gan SI, Gluck M, Kozarek R. Balloon dilation of benign small bowel strictures using double balloon enteroscopy: 5-year review from a single tertiary referral center. Gastrointestinal Intervention. 2012;1:74–78. [Google Scholar]
- 22.Nishimura N, Yamamoto H, Yano T, Hayashi Y, Sato H, Miura Y, Shinhata H, Sunada K, Sugano K. Balloon dilation when using double-balloon enteroscopy for small-bowel strictures associated with ischemic enteritis. Gastrointest Endosc. 2011;74:1157–1161. doi: 10.1016/j.gie.2011.07.024. [DOI] [PubMed] [Google Scholar]
- 23.Fukumoto A, Tanaka S, Yamamoto H, Yao T, Matsui T, Iida M, Goto H, Sakamoto C, Chiba T, Sugano K. Diagnosis and treatment of small-bowel stricture by double balloon endoscopy. Gastrointest Endosc. 2007;66:S108–S112. doi: 10.1016/j.gie.2007.02.027. [DOI] [PubMed] [Google Scholar]
- 24.Sunada K, Shinozaki S, Nagayama M, Yano T, Takezawa T, Ino Y, Sakamoto H, Miura Y, Hayashi Y, Sato H, et al. Long-term Outcomes in Patients with Small Intestinal Strictures Secondary to Crohn’s Disease After Double-balloon Endoscopy-assisted Balloon Dilation. Inflamm Bowel Dis. 2016;22:380–386. doi: 10.1097/MIB.0000000000000627. [DOI] [PubMed] [Google Scholar]
- 25.Kita H, Yamamoto H, Yano T, Miyata T, Iwamoto M, Sunada K, Arashiro M, Hayashi Y, Ido K, Sugano K. Double balloon endoscopy in two hundred fifty cases for the diagnosis and treatment of small intestinal disorders. Inflammopharmacology. 2007;15:74–77. doi: 10.1007/s10787-006-1568-7. [DOI] [PubMed] [Google Scholar]
- 26.Mueller T, Rieder B, Bechtner G, Pfeiffer A. The response of Crohn’s strictures to endoscopic balloon dilation. Aliment Pharmacol Ther. 2010;31:634–639. doi: 10.1111/j.1365-2036.2009.04225.x. [DOI] [PubMed] [Google Scholar]
- 27.Thienpont C, D’Hoore A, Vermeire S, Demedts I, Bisschops R, Coremans G, Rutgeerts P, Van Assche G. Long-term outcome of endoscopic dilatation in patients with Crohn’s disease is not affected by disease activity or medical therapy. Gut. 2010;59:320–324. doi: 10.1136/gut.2009.180182. [DOI] [PubMed] [Google Scholar]
- 28.Tichansky D, Cagir B, Yoo E, Marcus SM, Fry RD. Strictureplasty for Crohn’s disease: meta-analysis. Dis Colon Rectum. 2000;43:911–919. doi: 10.1007/BF02237350. [DOI] [PubMed] [Google Scholar]
- 29.Hassan C, Zullo A, De Francesco V, Ierardi E, Giustini M, Pitidis A, Taggi F, Winn S, Morini S. Systematic review: Endoscopic dilatation in Crohn’s disease. Aliment Pharmacol Ther. 2007;26:1457–1464. doi: 10.1111/j.1365-2036.2007.03532.x. [DOI] [PubMed] [Google Scholar]
- 30.Scimeca D, Mocciaro F, Cottone M, Montalbano LM, D’Amico G, Olivo M, Orlando R, Orlando A. Efficacy and safety of endoscopic balloon dilation of symptomatic intestinal Crohn’s disease strictures. Dig Liver Dis. 2011;43:121–125. doi: 10.1016/j.dld.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 31.Yamamoto H, Ogata H, T M, Ohmiya N. Clinical practice guideline for enteroscopy. Dig Endosc. 2017 doi: 10.1111/den.12883. [DOI] [PubMed] [Google Scholar]


