Abstract
Purpose: Resuming normal activities, such as work and school, is an important dimension of psychosocial recovery in cancer survivorship. Minimal data exist regarding adolescents or young adults' experiences of returning to school or work after cancer. The purpose of this study was to explore the processes of resuming work and school among adolescents and young adults after hematopoietic cell transplantation (HCT).
Methods: In-depth interviews were conducted with 18 adolescents and young adults, who were 15–29 years when they underwent HCT and 6–60 months post-transplant at study enrollment. Interview transcripts were systematically analyzed using Grounded Theory methodology.
Results: Participants described the context in which they attempted to return to work or school, specific challenges they faced, and strategies they developed in these environments. Feeling left behind from their peers and their pre-diagnosis selves, participants described “rushing” back to school and work impulsively, taking on too much too quickly while facing overwhelming physical and cognitive demands. Factors motivating this sense of urgency as well as barriers to successful and sustainable reentry in these settings are also addressed.
Conclusion: Findings are discussed in the context of important opportunities for clinical management, age-appropriate interventions, and implications for future research. A better understanding of psychosocial late effects, specifically related to school and work trajectories after cancer, is critical to survivorship care for adolescent and young adult cancer survivors.
Keywords: : work, school, survivorship, hematopoietic cell transplantation
Background
Leukemia and lymphoma represent two of the most common cancer types among adolescents and young adults (AYAs), and they may require hematopoietic cell transplantation (HCT) as a part of treatment.1,2 HCT aims at restoring hematopoietic function by transplanting stem cells from oneself (autologous) or a donor (allogeneic) after a conditioning regimen of high-dose chemotherapy with or without total body irradiation.3 The infusion of hematopoietic cells (i.e., “transplant day”) is followed by a prolonged engraftment and immunosuppression period that requires intensive supportive care and close monitoring for complications. HCT is an extremely toxic therapy with known post-treatment physical and psychosocial sequelae that can persist for many years, if not the remainder of life.1,4,5
In broader samples of adult and pediatric cancer survivors, more intense treatment regimens have been associated with significant challenges during reentry and poorer social functioning during the post-treatment period.6–10 HCT survivors face substantial risk for treatment-related morbidity that can contribute to non-relapse mortality and impaired functioning, such as chronic graft-versus-host disease, endocrinopathies, cardiopulmonary effects, musculoskeletal disorders, and subsequent malignancies.1,4,5,11–14 In addition, psychosocial challenges among HCT survivors include neurocognitive impairments,13,15 diminished quality of life,16 difficulty resuming social roles,17 fatigue,18 infertility and sexual dysfunction,19–22 distress,23 post-traumatic stress disorder,24 and depression.25 Although many survivors are able to work after HCT,26–28 they often report long-term challenges in this area, such as job insecurity, financial losses, physical and mental barriers to working, career derailment, and poorer quality of life.29–31
The impact of treatment intensity on psychosocial outcomes among AYAs remains largely unexplored.32,33 In one of the few studies available, AYAs who endured more intensive treatments were less likely to resume full-time work or school and four times more likely to report that cancer had negatively impacted their school and work plans compared with those who received less intense treatments.34 These findings suggest that survivors of HCT are a particularly vulnerable group of AYAs in terms of work and school outcomes. Despite the prevalence of hematological malignancies in early adulthood2 and the intensity of HCT,35 little is known about AYA cancer survivors who have undergone HCT. Therefore, we selected a qualitative approach to highlight the experiences of this subgroup of AYAs. In this article, we describe the process of resuming activities related to work and school among AYAs after HCT, including factors that influenced their decisions if and when to resume, specific challenges related to functioning and sustaining engagement (initially and over the long term), and strategies they developed to adapt to work- or school-specific demands.
Methods
Setting and recruitment
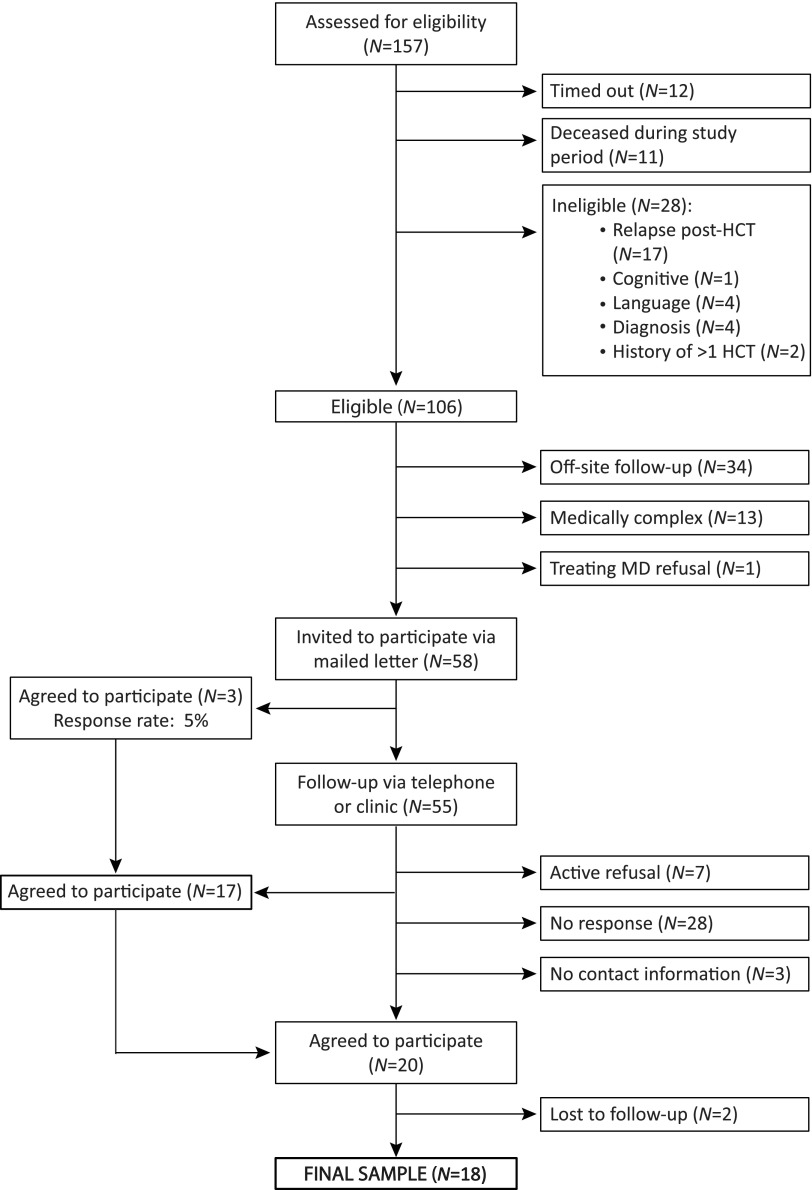
After institutional review board approval at both the University of California, Los Angeles and City of Hope National Medical Center, we identified potentially eligible patients by using a medical chart review, and then obtained permission from treating hematologists (Fig. 1). Study eligibility included individuals who were 15–29 years old at the time of a single bone marrow or stem cell transplant for a primary diagnosis of hematologic cancer and who were currently 6–60 months post-HCT. Exclusion criteria included: history of previous HCT, disease relapse after HCT, non-English speaking, or younger than 18 years old at study enrollment. Of the 106 eligible patients identified, medically complex patients, defined by suspected relapse or recent hospitalization for HCT complications (n = 13), were not approached. Patients receiving follow-up care elsewhere (n = 34) or without physician permission (n = 1) were also not approached. Invitations to participate were mailed to the remaining 59 potential participants. We followed up by telephone or at scheduled appointments in the outpatient clinic to discuss possible study participation.
FIG. 1.
Summary of recruitment.
Data collection and analysis
Grounded theory methodology, influenced by Constructivism, guided all aspects of the study.36,37 Using this inductive, qualitative approach, data collection and analysis occurred concurrently to allow for constant comparison.37 After obtaining informed consent, participants completed a sociodemographic questionnaire followed by an in-depth interview conducted by the first author in a convenient, private location or via telephone. A semi-structured interview guide was developed from a previous pilot study with AYAs by the first and last authors (Table 1). Interviews were digitally audio-recorded, transcribed verbatim, and de-identified. The duration of interviews was, on average, 102.4 minutes (range: 56.4–164.2 minutes). Participants received a $50 gift card for their time.
Table 1.
Excerpt from Semi-Structured Interview Guide
| Area of focus | Examples of questions and prompts |
|---|---|
| Resuming activities | After you finished your treatment, what were the biggest challenges you faced at that time? |
| Prompt: If you returned to work/school, when did you and what was it like? | |
| Prompt: If you were able, what hobbies/interests did you engage in again? | |
| Prompt: If not, why not? What was different? How did that feel? | |
| Can you please tell me about any things that continue to be challenging since having HCT? | |
| Prompt: What has been the most challenging or difficult aspect socially and why? | |
| Prompt: What has been the most challenging or difficult aspect emotionally and why? | |
| Prompt: What has been the most challenging or difficult aspect in terms of the things you do (behaviorally) and why? | |
| Perspectives on cancer, HCT, and health | How often do you think about your cancer and transplant experience? |
| Prompt: When you do think of it, what comes to mind? | |
| How do you feel about your health now? | |
| Prompt: What does “being healthy” mean to you now? | |
| Impact on future plans | When you think about your life now, do you feel it has changed because of your cancer/transplant experience? If so, how? |
| Prompt: How, if at all, has having cancer and undergoing HCT affected your future plans? |
HCT, hematopoietic cell transplantation.
Through a systematic yet flexible coding process, we attached analytic meaning to segments of data. We began with the initial coding of each transcript to study the data while remaining open. Then, we used focused coding to develop salient codes and identify tentative categories. In later interviews, theoretical sampling allowed us to gain needed insights, fill out properties of emergent categories, and elaborate relationships between categories. We refined our theoretical interpretation of the data through memos and diagrams.36,37 This analytic process continued until major theoretical categories were deemed saturated and robust and no new properties emerged.36 To enhance rigor, we ensured sufficient breadth and depth of observations, engaged in reflexive memo-writing, recorded field notes and process memos, and involved at least two researchers in independent analysis and collaboration at each stage.36,37 The Atlas.ti software program supported overall data management.38
Results
Sample characteristics
A total of 18 individuals were interviewed. Participants were, on average, 23.3 years of age at HCT and 26.0 years at study enrollment. The average time since HCT was 32.8 months (range: 8–60). Medical and sociodemographic characteristics are listed in Table 2. In the following sections, we describe theoretical categories of “rushing” to resume school and work after HCT, fears contributing to this urgency, and barriers to successful, sustainable reentry (Table 3).
Table 2.
Sample Characteristics (n = 18)
| Characteristic | Mean | Range | n (%) |
|---|---|---|---|
| Mean time since HCT (months) | 32.8 | (8–60) | |
| Mean age at HCT (years) | 23.3 | (18.5–29.7) | |
| Mean age at study enrollment (years) | 26.0 | (19.8–34.6) | |
| Sex | |||
| Male | 11 (61) | ||
| Female | 7 (39) | ||
| Ethnicity | |||
| White/Caucasian | 7 (39) | ||
| Hispanic/Latino | 8 (44) | ||
| Asian/South Asian | 3 (17) | ||
| Diagnosis | |||
| Hodgkin's lymphoma | 2 (11) | ||
| Acute myeloid leukemia | 10 (56) | ||
| Acute lymphoblastic leukemia | 5 (28) | ||
| Non-Hodgkin's lymphoma | 1 (5) | ||
| HCT type | |||
| Allogeneic, HLA-matched unrelated donor | 9 (50) | ||
| Allogeneic, sibling donor | 3 (17) | ||
| Allogeneic, cord blood | 3 (17) | ||
| Autologous | 3 (17) | ||
| Living situation at study enrollment | |||
| Family of origin (parent(s) and siblings) | 10 (56) | ||
| Roommate(s) | 1 (6) | ||
| Spouse/Partner | 5 (28) | ||
| Spouse/Partner and family of origin | 1 (6) | ||
| Extended family | 1 (6) | ||
| Highest level of education completed at study enrollment | |||
| Some high school | 1 (6) | ||
| High school degree | 2 (11) | ||
| Some college | 9 (50) | ||
| 4-year college degree | 5 (28) | ||
| Graduate degree | 1 (6) | ||
| School/employment status at study enrollment | |||
| No school and unemployed | 6 (33) | ||
| Student (full- or part-time) | 5 (28) | ||
| Employed (full- or part-time) | 6 (33) | ||
| Student and employed | 1 (6) | ||
| Total annual household income | |||
| Don't know | 5 (28) | ||
| $19,999 or less | 4 (22) | ||
| $20,000–$49,999 | 5 (28) | ||
| $50,000–$74,999 | 3 (17) | ||
| $75,000–$99,999 | 0 (0) | ||
| $100,000 or more | 1 (6) | ||
| Relationship status at study enrollment | |||
| Not in a significant relationship | 8 (44) | ||
| In significant relationship, not living together | 4 (22) | ||
| Living with spouse/partner | 6 (33) | ||
| Marital status at diagnosis | |||
| Never married | 17 (94) | ||
| Married | 1 (6) | ||
| Marital status at study enrollment | |||
| Never married | 14 (78) | ||
| Married | 4 (22) | ||
Table 3.
Theoretical Categories and Examples
| Category | Example |
|---|---|
| “Rushing” to resume | I was really determined to catch up, so I actually went to summer school. […] I would say that I maybe overcompensated for my time that I was away. So, this was stupid. I don't know why I did this, but I accepted four jobs. Yeah. I don't know why I did that. […] Part of it, I think, was you missed out on something and you've got to make up for it kind of mentality. Part of it was just enjoyment. I was back at school. I could handle this job. I can do this for this professor. I could take this class. It was really darn cool. Like, it was just exciting. And part of it, I think, was maybe to prove something […] and so now I had to compensate by doing a job, being independent, earning my own money, paying my own way, being equal or being adult, whatever that meant. So, it was a–I don't know. I just had no impulse control, perhaps. So, I just dove in the deep end, and it was sink or swim. |
| Motivating factors | |
| Feeling left behind | I can only be around cancer or sick people who can relate with me now. I cannot relate with, you know, “Oh, yeah. I got a tattoo. Yeah. I got laid. Yeah. We went to this concert. We went to see Pitbull, went to Cabo, went to Hawaii, went to all this.” “I went through a blood infusion. I went through a CAT scan, and they opened me up. I have a hole in my stomach. What's that? Nevermind.” |
| Danger in “dwelling” | I went through nine months of extreme dependence where I couldn't do anything on my own. […] I felt like I wanted to sort of branch out and move away from that as quickly as possible. I saw it as like the first step on the return to normalcy. |
| I just felt like [other survivors] were so caught up in their experience and in their treatment, and it sort of was like a dominating force in their lives. And I just did not want to be like that. It kind of felt like going back. It kept me engaged in this world that I didn't want to be in. | |
| Salvaging “my old life” | Through all this cancer experience, […] what scared me was not being able to finish school, to be left behind, to kind of have my life be ruined from all this, and then being able to say, “Yeah. I was in college once. I didn't make it. Now I'm working some dead-end job, and my life is miserable.” That, to me, is worse than death. […] That was what scared me more, was the thought of failure rather than the thought of death. |
| Life just didn't fit into the puzzle that it had before. […] It was hard to be the person I was before. And I didn't know what person I was left to be. I was lost. | |
| Barriers to successful, sustainable reentry | |
| Fatigue | [The fatigue] has taken on a different entity than the cancer. […] It's so persistent that it's become its own capital “F” Fatigue rather than a capital “C” Cancer. […] Same thing with stamina and energy - capital “E,” capital “S” kind of situation. […] How do I deal with the fatigue? Is my fatigue too much today? Can I do this, or is my fatigue a problem for me? |
| It would make me so tired that pretty much all I would do is go to work. Even though I was leaving early, I'd go home and fall asleep. I didn't have the strength to do much else. | |
| Cognitive difficulties | They say like, “It's normal. It's to be expected,” and it should get better, but I've heard anecdotal stories on the Internet from people who've said it hasn't gotten better, over like, five years. They still had like, holes. And I feel like it's getting worse, which is no good. That's really worrisome because it makes my life harder. |
| I'm just worried about not doing as well as I could in school, which will set me up for not as good opportunities as I would have had if I had not had these mental issues. | |
| Susceptibility to illness | I tried taking a class and I couldn't do it. I couldn't focus because I was like, what if somebody's sick sitting next to me? I'm going to get sick, and I'm going to end up in the hospital and not finish this class. So, I just stopped the class. I couldn't focus, so I dropped it. I wasn't ready to be out yet. And I still feel like that. I'm not ready. |
| Impact of breaks in school | It wasn't so much the health that was affecting me. It was the big gaps I was taking between classes that really made my classes difficult academically. […] It became too difficult. So, I failed a good amount of classes. And, again, it was one of those things that got really depressing for me because I was worried that, if it kept going, if you fail so many classes, you're going to get kicked out of school. And then, at that point, you know, you start feeling stupid when you keep taking a class over and over and you keep failing it. |
| I had to withdraw from that whole semester, that whole year that I was there. And pay the fee of attending the school when I didn't even get credit for being there, because I missed finals. […] It was basically, “Hey, you missed finals. That's how our grading system works. There's no exception about it. And here's your five, ten thousand dollar fee that you owe.” | |
“Rushing” to resume
As participants emerged from the isolation of treatment and recovery, they aimed at moving beyond the cancer and HCT experience “as if it hadn't happened.” Rather than accommodate persistent health issues, participants described a fierce determination to “catch up” by “rushing” to make up for “lost” or “wasted” time. After being “obsolete for a while” due to illness, participants admitted that they were “chomping at the bit,” “begging,” or even “harassing” their medical teams for permission to resume school or work as soon as possible. One participant compared this rush with the slow pace of treatment, “I went from snail mode to rocket ship mode. Those are just two very big extremes.” Rushing was characterized by an overriding urgency to resume school and work, often resulting in overextension, lack of preparation, and unrealistic expectations.
Fears of falling further behind and never catching up superseded concerns about lingering health issues. Participants acknowledged that rushing was entirely self-generated; neither their family nor medical team pressured them to do so. As one participant explained, “I had to do what helped me get through the post-cancer part.” On reflection, participants regretted rushing back to work or school and admitted feeling unprepared physically or emotionally. They commented that a longer period of physical and psychological rehabilitation would have been beneficial.
Motivating factors
“Rushing” to resume pre-illness activities of work and school was motivated by three major fears: being left behind, never moving on, and losing the life they had known before diagnosis.
Feeling “left behind”
The prospect of school and work activities outside of the home required participants to survey the aftermath of their cancer and HCT experiences in a broader context. Participants described navigating a changed reality and felt alienated from their pre-diagnosis lives. Many struggled to relate to peers, who had accumulated life experiences without them. Participants also felt behind compared with what they understood to be the normal milestones of young adulthood, or “the regular flow of things,” such as education, career, home ownership, intimate partnerships, or family building. Feeling left behind in these areas triggered jealousy, anger, depression, and deeper fears of failure.
Danger in “dwelling”
Despite feeling uncertain about their health, participants worried that “dwelling,” or overanalyzing their situation, would prevent them from moving on. They described hustling to “get on with my life already” because they feared that if too much time elapsed, the window to catch up and reclaim their pre-illness potential would close entirely. One participant shared, “If I don't push myself enough, I just won't go back to the point where I was before,” while another explained, “I was worried that if I waited too long, I would lose that ambition and just get to a point where I'm like, ‘forget it,’ and I didn't want that for myself.” In this vein, participants also avoided connecting with other cancer survivors. One participant quit her volunteer work with a community-based cancer support network, explaining, “I felt like, if I continue, I'm just going to constantly stay in that mindset that cancer's always going to be around me. And I didn't want that.”
Salvaging “my old life”
Participants also rushed back to work and school in the hope of salvaging what they remembered of their pre-diagnosis lives. Many wanted to hold on to their “old lives,” seeing them as superior to any future they could now imagine for themselves. Participants strongly preferred returning to their pre-illness work and school settings, although this was often impossible. For many, physical limitations prevented them from work-related tasks such as sitting on the floor as a preschool teacher or lifting large boxes at a warehouse store, whereas others could not return to jobs without adequate health insurance. Participants who did return to pre-illness jobs described a smoother transition due to flexible accommodations compared with those who returned to school or started in new settings. One participant explained that his boss allowed him to return full-time for salary and health benefits, even though he “knew that I wasn't going to be at full capacity.”
Barriers to successful, sustainable reentry
Attempts to “catch up” by rushing “into the deep end” of work and school revealed new health issues not previously faced at home. As physical and mental demands increased, many participants felt painfully aware of treatment-related limitations, particularly fatigue, cognitive difficulties, and susceptibility to illness. Participants also tried to curtail the impact of breaks in their schooling due to treatment.
Fatigue
Simply attempting to participate in school or work necessitated substantial increases in activity levels and subsequently higher levels of fatigue. Attending a single class involved a long list of mental and physical tasks, including getting ready, commuting, parking, walking to class, possibly climbing stairs, concentrating, socializing, and commuting home. Many participants described coming home after school or work and collapsing from utter exhaustion.
Participants developed strategies to manage overwhelming fatigue. One participant used a wheelchair to increase independence and conserve energy on a college campus, explaining, “I could walk, but I would take a few steps and I felt like I ran a marathon.” Several participants also learned the value of incorporating recovery time into their schedules, such as avoiding classes 2 days in a row because “back-to-back was too much.” However, many participants ultimately sacrificed healthy behaviors, such as adequate exercise, nutrition, and sleep, and resorted to skipping classes to compensate for fatigue.
Cognitive difficulties
Post-HCT cognitive changes, particularly in memory, attention, and concentration, became more apparent to participants as their mental workload increased at school or work. Particularly at school, struggles with slower thinking, memorization, and working under the pressure of exams or deadlines added a significant layer of difficulty. “Chemobrain” was more elusive than other symptoms because it was difficult to understand, predict, and self-manage. Input from healthcare providers about managing cognitive difficulties was also vague. Although some participants utilized school services for students with disabilities, they often found the offerings unhelpful. For example, extended time on exams did not make it easier to recall information when their mind went blank.
Cognitive changes were also emotionally disturbing and “frightened” participants. Although adaptive strategies, such as daily lists and calendar reminders, were useful in managing these issues in daily life, participants reported dismay that their symptoms seemed to be worsening rather than improving. They agonized about the long-term impact of treatment on their brain and how this might affect their futures.
Susceptibility to illness
Participants' weakened immune system and susceptibility to infection further complicated the return to school and work. Outside of the home, participants experienced frequent illnesses, which exacerbated their worry about relapses and readmissions to the hospital. For one participant, sickness dominated his first year of college; he reported, “every single person that I encountered who was sick, I caught the sickness.” This susceptibility also heightened anxiety about exposure to “germs” and the school or work environment itself as a health threat.
Impact of breaks in school
Overcoming disruptions in school trajectories due to treatment was another significant challenge at reentry. Participants were not able to stay in school during HCT, and many were forced to withdraw mid-year. Unfortunately, these abrupt departures resulted in distressing losses in academic credits and financial investments due to rigid school policies. Many participants lacked support in coordinating formal medical leaves from school. Therefore, when they attempted to return, many were surprised to face administrative hurdles. One participant, who stopped attending college “without telling them anything,” became depressed when he was told, “You didn't take a leave of absence. So, you're no longer a student here.”
As participants attempted to resume work and school, they felt determined to overcome challenges initially. However, the experience of repeated disappointments and failures in these settings left most participants dejected, as one explained, “I just couldn't rebound.”
Discussion
Our findings are among the first to articulate AYA cancer survivors' experiences of returning to work and school after HCT, an intense treatment with significant long-term sequelae. At diagnosis, all participants were in school, employed, or both. At the time of their interviews, participants were, on average, in their third year of recovery and although most had attempted to resume pre-illness activities, six were neither employed nor in school and 11 were managing only one role (school or work), often at part-time status. We found that when AYAs rushed back to school and work after HCT, they experienced immense challenges, a lack of preparation, and a need for specific guidance from healthcare and education professionals to facilitate this important step of survivorship.
The ability to resume work-related activities after HCT is an important indicator of psychosocial recovery and can affect quality of life.29,39 Current research suggests that adult HCT survivors face long-term challenges at work.29–31 Adults who are unemployed 1 year after HCT report higher rates of fatigue and pain, poorer perceived health, and lower quality of life than those who return to work.39 In our study, several participants did not return to work and many worried about their future employability. Those who returned to previous jobs relied on the empathy of supervisors rather than knowledge of specific policies intended to protect cancer survivors in the workforce. Thus, AYAs may need additional support in navigating return to work and connecting to resources on work protections.
Consistent with other studies on adult cancer survivors returning to work, participants overestimated their functional ability.40,41 Particularly at school, the tendency to take on too much too quickly resulted in demoralizing struggles and even failures. Our findings suggest that AYAs may be particularly at risk for these overestimations because of their developmental determination to catch up with peers and deep fear of losing their ambition. Pediatric care models commonly include school reintegration programs to minimize the effects of cancer-related breaks in education because of federal mandates to protect children with cancer.42–45 Unfortunately, these programs do not typically extend beyond the K-12 setting, leaving AYAs who are in post-secondary programs without much needed resources.
AYAs in our study received a “green light” from their medical teams to resume pre-illness activities, but little guidance about how to implement this decision in light of lingering health issues. Participants expressed frustration that healthcare providers did not understand the rigidity of school requirements, whereas school-based disability services seemed ill-equipped to deal with the complexity of cancer survivorship. Unsurprisingly, this disjointed approach results in distress and difficulty for AYAs who are trying to resume activities. Expertise related to cancer survivorship, particularly late effects of high toxicity treatments, is needed to develop realistic, meaningful education plans that leave room for adjustments and enhance chances for success.
Future research should focus on more formal school and work reintegration interventions for AYAs that are tailored to the specific demands of higher education, early workforce status, and young adult developmental needs. A rehabilitation-focused approach that begins well in advance of actual resumption could provide substantial assistance to this patient population. Interventions, such as occupational or physical therapy, that target persistent post-treatment issues including fatigue and cognitive difficulties may better prepare AYAs for work and school demands.46–49 Another promising but relatively untapped area is the use of internet-based health interventions,50 mobile apps and m-health,51,52 or video game technology53 to ease the transition back to school or work for AYAs.
There are several limitations from this small qualitative sample. Participants were recruited from a single specialized institution with an established survivorship program for HCT patients. It is possible that AYAs receiving care elsewhere may be connected to fewer resources. The 5-year post-HCT span provides insight into various experiences along the HCT trajectory, whereas the cross-sectional design does not reflect longitudinal trends. Many participants underwent extensive treatment before HCT, and therefore, disruption in work and school trajectories is not necessarily a direct result of HCT. Because of the younger age of our sample (15–29 years at HCT) with respect to the National Cancer Institute definition of AYA (15–39 years),54 our findings may be disproportionately focused on school rather than work issues.
Nevertheless, we have documented major challenges in return to work and school for AYAs after high-intensity treatment with HCT. Longitudinal studies are needed that track educational and work outcomes in relation to medical and developmental changes. In the future, differences across important AYA subgroups should be further investigated to develop risk profiles and identify preferences, concerns, and areas of greatest need for support.
Acknowledgments
The authors would like to acknowledge the Oncology Nursing Society (ONS)/ONS Foundation (Dissertation Research Grant), the NIH/NINR Ruth L. Kirschstein National Research Service Award (NRSA) Institutional Research Training Grant T32 NR 07077 for financial support for this project. They would also like to extend their appreciation to Dr. Julie Wolfson, Dr. Saro Armenian, Dr. Stephen Forman, Lindsey Hageman, Alysia Bosworth, and Laura Gustafson for their administrative support of this project.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review boards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Baker KS, Armenian S, Bhatia S. Long-term consequences of hematopoietic stem cell transplantation: current state of the science. Biol Blood Marrow Transplant. 2010;16(1 Suppl):S90–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barr RD, Ferrari A, Ries L, et al. Cancer in adolescents and young adults: a narrative review of the current status and a view of the future. JAMA Pediatr. 2016;170(5):495–501 [DOI] [PubMed] [Google Scholar]
- 3.Wood WA, Lee SJ. Malignant hematologic diseases in adolescents and young adults. Blood. 2011;117(22):5803–15 [DOI] [PubMed] [Google Scholar]
- 4.Sun CL, Francisco L, Kawashima T, et al. Prevalence and predictors of chronic health conditions after hematopoietic cell transplantation: a report from the Bone Marrow Transplant Survivor Study. Blood. 2010;116(17):3129–39; quiz 377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sun CL, Kersey JH, Francisco L, et al. Burden of morbidity in 10+ year survivors of hematopoietic cell transplantation: report from the bone marrow transplantation survivor study. Biol Blood Marrow Transplant. 2013;19(7):1073–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62(4):220–41 [DOI] [PubMed] [Google Scholar]
- 7.Stanton AL, Rowland JH, Ganz PA. Life after diagnosis and treatment of cancer in adulthood: contributions from psychosocial oncology research. Am Psychol. 2015;70(2):159–74 [DOI] [PubMed] [Google Scholar]
- 8.Pang JW, Friedman DL, Whitton JA, et al. Employment status among adult survivors in the Childhood Cancer Survivor Study. Pediatr Blood Cancer. 2008;50(1):104–10 [DOI] [PubMed] [Google Scholar]
- 9.Wengenroth L, Rueegg CS, Michel G, et al. ; Swiss Paediatric Oncology Group (SPOG). Life partnerships in childhood cancer survivors, their siblings, and the general population. Pediatr Blood Cancer. 2014;61(3):538–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Strauser DR, Jones A, Chiu C-Y, et al. Career development of young adult cancer survivors: a conceptual framework. J Vocat Rehabil. 2015;42(2):167–76 [Google Scholar]
- 11.Adhikari J, Sharma P, Bhatt VR. Risk of secondary solid malignancies after allogeneic hematopoietic stem cell transplantation and preventive strategies. Future Oncol. 2015;11(23):3175–85 [DOI] [PubMed] [Google Scholar]
- 12.Lowe T, Bhatia S, Somlo G. Second malignancies after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2007;13(10):1121–34 [DOI] [PubMed] [Google Scholar]
- 13.Syrjala KL, Martin P, Deeg J, Boeckh M. Medical and psychosocial issues in transplant survivors. In: Ganz PA. (Ed). Cancer survivorship today and tomorrow. New York: Springer; 2007, pp. 188–214 [Google Scholar]
- 14.Majhail NS, Rizzo JD. Surviving the cure: long term followup of hematopoietic cell transplant recipients. Bone Marrow Transplant. 2013;48(9):1145–51 [DOI] [PubMed] [Google Scholar]
- 15.Scherwath A, Schirmer LF, Kruse M, et al. Cognitive functioning in allogeneic hematopoietic stem cell transplantation recipients and its medical correlates: a prospective multicenter study. Psychooncology. 22(7):1509–16 [DOI] [PubMed] [Google Scholar]
- 16.Pidala J, Anasetti C, Jim H. Quality of life after allogeneic hematopoietic cell transplantation. Blood. 2009;114(1):7–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bieri S, Roosnek E, Helg C, et al. Quality of life and social integration after allogeneic hematopoietic SCT. Bone Marrow Transplant. 2008;42(12):819–27 [DOI] [PubMed] [Google Scholar]
- 18.Hacker ED, Fink AM, Peters T, et al. Persistent fatigue in hematopoietic stem cell transplantation survivors. Cancer Nurs. 2016;40(3):174–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yi JC, Syrjala KL. Sexuality after hematopoietic stem cell transplantation. Cancer J. 2009;15(1):57–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dyer G, Gilroy N, Bradford J, et al. A survey of fertility and sexual health following allogeneic haematopoietic stem cell transplantation in New South Wales, Australia. Br J Haematol. 2016;172(4):592–601 [DOI] [PubMed] [Google Scholar]
- 21.Lee HG, Park EY, Kim HM, et al. Sexuality and quality of life after hematopoietic stem cell transplantation. Korean J Intern Med. 2002;17(1):19–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Syrjala KL, Kurland BF, Abrams JR, et al. Sexual function changes during the 5 years after high-dose treatment and hematopoietic cell transplantation for malignancy, with case-matched controls at 5 years. Blood. 2008;111(3):989–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hefner J, Kapp M, Drebinger K, et al. High prevalence of distress in patients after allogeneic hematopoietic SCT: fear of progression is associated with a younger age. Bone Marrow Transplant. 2014;49(4):581–4 [DOI] [PubMed] [Google Scholar]
- 24.El-Jawahri AR, Vandusen HB, Traeger LN, et al. Quality of life and mood predict posttraumatic stress disorder after hematopoietic stem cell transplantation. Cancer. 2016;122(5):806–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mosher CE, Duhamel KN, Rini C, et al. Quality of life concerns and depression among hematopoietic stem cell transplant survivors. Support Care Cancer. 2011;19(9):1357–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bush NE, Donaldson GW, Haberman MH, et al. Conditional and unconditional estimation of multidimensional quality of life after hematopoietic stem cell transplantation: a longitudinal follow-up of 415 patients. Biol Blood Marrow Transplant. 2000;6(5A):576–91 [DOI] [PubMed] [Google Scholar]
- 27.Lee SJ, Fairclough D, Parsons SK, et al. Recovery after stem-cell transplantation for hematologic diseases. J Clin Oncol. 2001;19(1):242–52 [DOI] [PubMed] [Google Scholar]
- 28.Syrjala KL, Chapko MK, Vitaliano PP, et al. Recovery after allogeneic marrow transplantation: prospective study of predictors of long-term physical and psychosocial functioning. Bone Marrow Transplant. 1993;11(4):319–27 [PubMed] [Google Scholar]
- 29.Hamilton JG, Wu LM, Austin JE, et al. Economic survivorship stress is associated with poor health-related quality of life among distressed survivors of hematopoietic stem cell transplantation. Psychooncology. 2013;22(4):911–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Johansson E, Larsen J, Schempp T, et al. Patients' goals related to health and function in the first 13 months after allogeneic stem cell transplantation. Support Care Cancer. 2012;20(9):2025–32 [DOI] [PubMed] [Google Scholar]
- 31.Stepanikova I, Powroznik K, Cook KS, et al. Exploring long-term cancer survivors' experiences in the career and financial domains: interviews with hematopoietic stem cell transplantation recipients. J Psychosoc Oncol. 2016;34(1–2):2–27 [DOI] [PubMed] [Google Scholar]
- 32.Institute of Medicine. Identifying and addressing the needs of adolescents and young adults with cancer. Washington, DC: The National Academies Press; 2013 [PubMed] [Google Scholar]
- 33.Katz A. Meeting the need for psychosocial care in young adults with cancer. Pittsburgh, PA: Oncology Nursing Society; 2015 [Google Scholar]
- 34.Parsons HM, Harlan LC, Lynch CF, et al. Impact of cancer on work and education among adolescent and young adult cancer survivors. J Clin Oncol. 2012;30(19):2393–400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bukowinski AJ, Burns KC, Parsons K, et al. Toxicity of cancer therapy in adolescents and young adults (AYAs). Semin Oncol Nurs. 2015;31(3):216–26 [DOI] [PubMed] [Google Scholar]
- 36.Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London: Sage; 2014 [Google Scholar]
- 37.Corbin J, Strauss B. Basics of qualitative research: techniques & procedures for developing grounded theory. Thousand Oaks, CA: Sage; 2015 [Google Scholar]
- 38.ATLAS.ti Version 7.5.10. Berlin: Scientific Software Development; 2016 [Google Scholar]
- 39.Morrison EJ, Ehlers SL, Bronars CA, et al. Employment status as an indicator of recovery and function one year after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2016;22(9):1690–5 [DOI] [PubMed] [Google Scholar]
- 40.Parry C, Morningstar E, Kendall J, Coleman EA. Working without a net: leukemia and lymphoma survivors' perspectives on care delivery at end-of-treatment and beyond. J Psychosoc Oncol. 2011;29(2):175–98 [DOI] [PubMed] [Google Scholar]
- 41.Stergiou-Kita M, Pritlove C, Holness DL, et al. Am I ready to return to work? Assisting cancer survivors to determine work readiness. J Cancer Surviv. 2016;10(4):699–710 [DOI] [PubMed] [Google Scholar]
- 42.Harris MS. School reintegration for children and adolescents with cancer: the role of school psychologists. Psychol Sch. 2009;46(7):579–92 [Google Scholar]
- 43.Kirkpatrick KM. School issues and educational strategies for survivors of childhood cancer. New York: Springer Science+Business Media; 2015; pp. 347–65 [Google Scholar]
- 44.Soejima T, Sato I, Takita J, et al. Support for school reentry and relationships between children with cancer, peers, and teachers. Pediatr Int. 2015;57(6):1101–7 [DOI] [PubMed] [Google Scholar]
- 45.Prevatt FF, Heffer RW, Lowe PA. A review of school reintegration programs for children with cancer. J School Psychol. 2000;38(5):447–67 [Google Scholar]
- 46.Syrjala KL, Martin PJ, Lee SJ. Delivering care to long-term adult survivors of hematopoietic cell transplantation. J Clin Oncol. 2012;30(30):3746–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Masneri S, Bolis T. Late neurocognitive effects in children and adolescents who have undercone oncological treatment: a rehabilitation model. G Ital Med Lav Ergon. 2011;33(1 Suppl A):A37–A40 [PubMed] [Google Scholar]
- 48.Coccia PF, Altman J, Bhatia S, et al. Adolescent and young adult oncology. Clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2012;10(9):1112–50 [DOI] [PubMed] [Google Scholar]
- 49.Bower JE, Bak K, Berger A, et al. Screening, assessment, and management of fatigue in adult survivors of cancer: an American Society of Clinical oncology clinical practice guideline adaptation. J Clin Oncol. 2014;32(17):1840–50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Syrjala KL, Stover AC, Yi JC, et al. Development and implementation of an Internet-based survivorship care program for cancer survivors treated with hematopoietic stem cell transplantation. J Cancer Surviv. 2011;5(3):292–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wesley KM, Fizur PJ. A review of mobile applications to help adolescent and young adult cancer patients. Adolesc Health Med Ther. 2015;6:141–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Myneni S, Amith M, Geng Y, Tao C. Towards an ontology-driven framework to enable development of personalized mHealth solutions for cancer survivors' engagement in healthy living. Stud Health Technol Inform. 2015;216:113–117 [PMC free article] [PubMed] [Google Scholar]
- 53.Beale IL, Kato PM, Marin-Bowling VM, et al. Improvement in cancer-related knowledge following use of a psychoeducational video game for adolescents and young adults with cancer. J Adolesc Health. 2007;41(3):263–70 [DOI] [PubMed] [Google Scholar]
- 54.Smith AW, Seibel NL, Lewis DR, et al. Next steps for adolescent and young adult oncology workshop: an update on progress and recommendations for the future. Cancer. 2016;122(7):988–99 [DOI] [PMC free article] [PubMed] [Google Scholar]