Abstract
Atrial fibrosis appears to be a key factor in the genesis and/or perpetuation of atrial fibrillation (AF). The pathological distribution of atrial fibrosis is geographically consistent with the attachments between the posterior left atrium and the pericardium along the reflections where wall stiffness is increased and structural changes are found. While there is a wide range of complex etiological factors and electrophysiological mechanisms in AF, there is evidence for a common pathophysiological pathway that could account for deliberate substrate formation and progression of AF. Anatomical stresses along the atrium, mediated by the elastic modulus mismatch between atrial tissue and the pericardium, result in inflammatory and fibrotic changes which create the substrate for atrial fibrillation. This may explain the anatomical predominance of pulmonary vein triggers earlier in the development of atrial fibrillation and the increasing involvement of the atrium as the disease progresses. Ablative treatments that address the progressive nature of atrial fibrillation and fibrosis may yield improved success rates.
Keywords: Atrial Fibrillation, Ablation, Fibrosis
Introduction
Atrial Fibrillation (AF) is the most commonly encountered clinical arrhythmia requiring treatment, and results in multiple adverse sequelae including stroke, heart failure, cognitive decline, dementia, diminished quality of life and a rising incidence of death. [1], [2] With increasing life expectancy and the upsurge of underlying factors that affect progressive atrial remodeling, AF has become a global pandemic, evidenced by a worldwide prevalence of 33.5 million and 5 million new cases annually. [3]
The mechanisms for development of persistent atrial fibrillation are not known, although conjecture is widespread. [4] While many viable theories to account for the development and occurrence of atrial fibrillation (AF) have been suggested, a unifying explanation that puts all of the acknowledged pathological explanations into perspective is lacking. Dominant theories revolve around ganglionated plexi, ectopic foci, rotors, and macro re-entrant circuits that enable arrhythmogenic wavefronts. [5] Curiously, none of these explanations focus on the consistent geographic distribution of substrates responsible for AF.
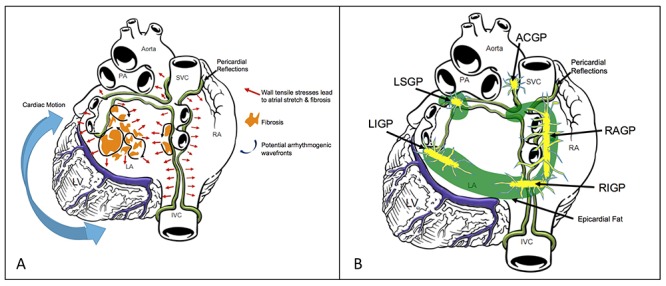
Computational models, real time voltage mapping and advanced imaging studies have consistently demonstrated geographically similar atrial remodeling in progressive patterns. [6] This atrial remodeling emanates from proposed high stress regions where the pericardium secures the posterior left atrium. The progression of atrial fibrosis relative to the pericardial reflections and stress points about the posterior left atrium, as depicted in [Figure 1], appears clinically significant and may offer clues to underlying mechanisms in AF. Understanding the role played by the pericardial reflections in the genesis of AF may unlock additional treatment considerations and clinical algorithms.
Figure 1. Panel A: Schematic of progressive atrial remodeling. Pericardial reflections (green lines), their attachments to the posterior left atrium, and their relation to proposed high stress regions. Panel B: Ganglionated plexi (yellow) and epicardial fat (green). Left superior ganglionated plexi (LSGP), left inferior ganglionated plexi (LIGP), right anterior ganglionated plexi (RAGP), right inferior ganglionated plexi (RIGP), aortocaval ganglionated plexi (ACGP).
Treatment of atrial fibrillation: A changing target
Endocardial catheter ablation has become a primary treatment modality for drug resistant, symptomatic paroxysmal AF (PAF), but has demonstrated a limited, temporally related efficacy in non-paroxysmal atrial fibrillation (NPAF) patients. [7] The 3 year arrhythmia-free survival in NPAF for a single endocardial catheter ablation procedure has been reported at 28.4% with the efficacy after multiple procedures at 51.1%. [8] The Hamburg sequential ablation strategy of PVI plus linear lesions and SVC isolation for long-standing persistent AF patients yielded 5-year single and multiple procedure success rates of 20% and 45% respectively. [9] Recently, the StarAF II study demonstrated that PVI only ablation in patients with persistent AF resulted in a single-procedure 49% freedom from atrial tachyarrhythmias off antiarrhythmics at 18 months. The addition of CFAE or linear lesions actually yielded an even lower ~30% freedom from atrial tachyarrhythmias. Additional ablations and antiarrhythmic therapy increased the success rate to only ~60%. Even an open surgical approach has not yielded much higher success. A recent study by Gillinov et al. examined the outcomes of surgical atrial fibrillation ablation in patients with persistent AF undergoing mitral-valve surgery. Biatrial maze resulted in only a 66% freedom from AF at 1 year. [10]
Detailed investigation into potential explanations for the failure of AF ablation frequently indicts reconnections of pulmonary vein tissue and substrates along the posterior left atrium. Fibrosis progresses predictably from the heavily invested pulmonary veins to the posterior left atrium, evolving additional AF substrates [Figure 1]. Attempts to ablate localized rotors or complex fractionated atrial electrograms may actually create patchy, heterogeneous fibrosis capable of initiating or sustaining arrhythmogenic circuits as illustrated. A better understanding of the mechanisms for AF is needed to tailor a more effective treatment.
Pulmonary Vein Triggers of Atrial Fibrillation
The atrial muscle sleeves at the pulmonary vein-left atrial junction are the most common source of focal triggers for atrial fibrillation. [11] There is a predominance of pulmonary vein ectopy in the superior veins versus the inferior veins and the left superior vein was noted to have the highest frequency of ectopy. There may be an anatomical reason for this unequal distribution of PV ectopy. Anatomically, the superior veins are better developed and longer than the inferior veins. The longest sleeve is usually the left superior vein. [12] Histologically, patients with atrial fibrillation have a significantly increased presence of atrial myocardial extension into the pulmonary veins. In addition, patients with AF also have a higher frequency of discontinuity, hypertrophy, and fibrosis of these extensions. [13] Fibrosis was more prominent in the periphery of the sleeves and often are completely sclerotic distally. This may be due to chronic hypoxia at these distal sleeves since they are at the periphery of the coronary circulation. Development of extensive collagenous septa may create nonuniform anisotropic electrical propagation that could result in micro re-entry and automaticity. [14] Since the left superior pulmonary vein frequently has the longest atrial myocardial extension, placing it at the highest risk for tissue hypoxia, this may explain the increased propensity for LSPV ectopy. Additionally, since the atrial and pulmonary veins are autonomically innervated, sympathovagal imbalance can cause additional anisotropic changes in the action potential duration and PV myocyte refractory periods, increasing the potential for re-entry. [15]
Persistent Atrial Fibrillation and Non-Pulmonary Vein Atrial Fibrillation Substrate
As atrial fibrillation increases in chronicity, so does the proportion of the patients who have non-pulmonary vein substrate. The posterior left atrium is the most anatomically concentrated location of arrhythmogenic mechanisms that are consistently demonstrated with nonparoxysmal AF. [16] Kalifa et al. demonstrated that, in an ovine model, the posterior left atrium frequently contains sites of fast-organized activity with the highest dominant frequency. [17] Patients with AF demonstrated a significantly greater anatomic distribution and degree of conduction slowing, heterogeneity, and anisotropy in the posterior left atrium, culminating in circuitous patterns of propagation. [18]
Atrial Fibrosis/ Tailored Atrial substrate modification
There is increasing data that point to the development of atrial fibrosis in the progression of atrial fibrillation. An underlying cardiac abnormality or metabolic disorder associated with atrial fibrosis and atrial enlargement can be found in approximately 85% of patients with atrial fibrillation. [19] Atrial fibrosis usually extends beyond the pulmonary veins and appears to be a significant reason why simple pulmonary vein isolation is not adequate in treating the majority of persistent atrial fibrillation patients.
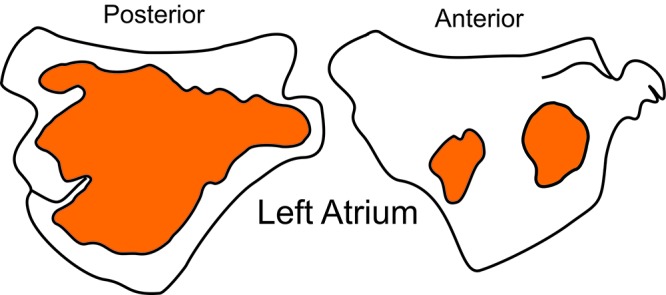
Despite the current limitations in spatial resolution with cardiac MRI, there appears to be a pattern of atrial fibrosis in patients with atrial fibrillation. Cochet et al. elegantly described the distribution of atrial fibrosis in patients with and without atrial fibrillation. [20] The predominant location of fibrosis was noted to be in the posterior LA wall rather than the septal, anterior, and lateral segments. More specifically, delayed-enhancement likelihood maps showed that the region around the left inferior pulmonary vein ostium was most frequently to have fibrosis. [Figure 2] There was a lesser degree of fibrosis at the right veins ostia. Fibrosis in the anterior wall was less common but when present was more often found in the septum below and anterior to the right pulmonary veins.
Figure 2. Common regions of fibrosis Adapted from Cochet et al. J Cardiovasc Electrophysiol 2015; 26: 489.
Treatment strategies which isolate a larger area of the posterior wall appear to have increased rates of success. [21], [22] This is the theory of why a wide antral circumferential ablation has been more successful than ostial pulmonary vein isolation. Posterior wall isolation via the creation of a roof line and posterior box line to the usual PVI circles has also been demonstrated to have better long term outcomes than PVI alone for persistent AF. Unfortunately, isolation of the posterior left atrium is frequently challenging with endocardial catheter ablation alone since a breakdown in the PVI or either linear line may be arrhythmogenic and can result in recurrence. [23] Additionally, even if durable lines are created, some arrhythmogenic areas of fibrosis may be missed by empiric anatomical lines. As a result, there has been recent interest in developing an individualized strategy for ablating atrial fibrillation. [24] In this strategy, a pre-procedural MRI is performed to delineate the atrial scar substrate and ablation to box these additional regions is performed. This strategy has been termed Box Isolation of Fibrotic Areas (BIFA).
The Stretch-Inflammation-Fibrosis-Fibrillation (StIFF) Axis
Anatomical Stress mediated by the Pericardial Reflections
Interestingly the common sites of atrial fibrosis appears to be centered around regions of high stress. There appears to be an anatomical reason for this. The pericardium supports the heart against gravity and is attached to the posterior left atrium, inferior vena cava, superior vena cava, and pulmonary veins, as shown in [Figure 1]. These reflections secure the heart to the chest wall and vertebral column and confer specific plasticity and elasticity that allow cardiac excursion during acceleration and deceleration. The reflections anchor the heart and limit translational and rotational excursion of the heart with activity.
The pericardium is a strong, dense, fibrotic layer that blends with the adventitia of the roots of the great vessels and the central tendon of the diaphragm. [25]The pericardial reflections of the human heart derive from the same mesodermal fetal tissue as functional cardiac tissue. Histologically, however, the pericardium contains more abundant fibroblasts and has a higher modulus of elasticity than adjoining atrial and venous tissue, resulting in a material mismatch. Because of the tethering of the pericardium, motion of the heart is limited and high stresses at the pericardial attachment points lead to reactive fibrosis adjacent to these regions [Figure 2]. To compound the stress issue, the posterior left atrium and the pulmonary veins are substantially thinner than the left atrial roof, the ridge, or the lateral left atrium. [26] [Table 1] Laplace’s law reasons that these regions would experience the highest pressure and stress. This may explain why dense fibrosis appears to be more common within the oblique sinus rather than on the other side of the pericardial reflection (ie in the borderzone of the transverse sinus, Waterston’s sulcus anteriorly, and the posterior left atrial appendage). Additionally, the pericardial attachment points may also explain why fibrosis around the region of the sinus node and thus sinus node dysfunction coexist with atrial fibrillation. It may also explain why the SVC frequently harbors sites of AF triggers. Although the pericardial reflections are frequently found near fibrosis prone regions, fibrosis may also be located at other regions due to regional pressure, stretch, and stress.
Table 1. Left atrial wall thickness and fat thickness.
| Left atrial wall thickness (mm) | Left atrial fat thickness (mm) | |
|---|---|---|
| LAA | 2.2±0.6 | 4.3±1.8 |
| Roof | 2.0±0.6 | 4.3±2.1 |
| Anterior Wall | 1.8±0.3 | 1.3±0.7 |
| Posterior Wall | 1.7±0.3 | 3.6±2.0 |
| Floor | 1.7±0.3 | 9.6±3.9 |
| Lateral Wall | 1.8±0.4 | 6.3±3.1 |
| Septum | 2.4±0.8 | |
| Adapted from Park et al. Int J Cardiol 2014; 172(3):e411-3. |
Cardiac Motion
Since DE-MRI data indicate that the region outside the left inferior pulmonary veins are most frequently associated with fibrosis, perhaps there is an anatomic reason for this region being statistically problematic. Since the pericardial reflections at the inferior pulmonary veins help tether the heart in place, cardiac motion may place significant strain at these regions. The base of the left ventricle twists in a counterclockwise motion. The heart’s rotational motion during systole as well as the longitudinal and translational motion may put particular strain on the left inferior antrum. Anteriorly, this may translate to annular fibrosis and coronary sinus substrate as there is also a material mismatch of atrial and ventricular tissue at the annulus.
Regional atrial wall stresses
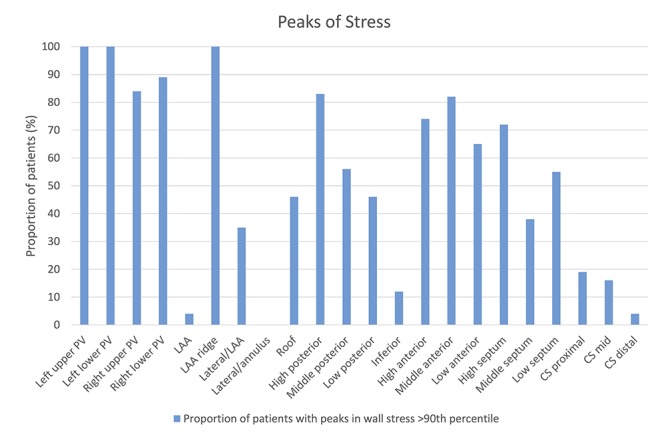
Finite element analysis has been used to predict wall stress distribution based on left atrial geometry from CT. Peaks in walls stress were concentrated at the pulmonary venous ostia, the appendage ridge, the high posterior wall and septal regions. [Figure 3] Peaks in wall stress were consistent with low voltage areas suggestive of focal remodeling and fibrosis. [27] These high stress regions correlate with locations of the pericardial reflections. The pericardial reflections outlined in green in [Figure 1] extend along the right heart from the SVC to the right pulmonary vein ostia to the IVC, across the high posterior roof from the superior aspect of the RPV ostium to the superior aspect of the left pulmonary veins, and incorporate the LPV ostium. Delayed-Enhancement Magnetic Resonance Imaging (DE-MRI) has illustrated progressive fibrosis formation in the same regions of finite element analysis documented increased wall stress suggesting a correlation [Figure 2].
Figure 3. Peaks of atrial wall stress Adapted from Hunter et al. Circ Arrhythm Electrophysiol. 2012;5(2):354.
Stretch, Inflammation and fibrosis
In preclinical animal models, atrial stretch induces increased atrial fibrosis that causes regional remodeling and conduction slowing. Atrial stretch causes release of ANP, calcium overload, calcineurin activation, engagement of the AT1 receptor and alterations in MMP and TIMP levels, which are implicated in tissue turnover and remodeling. [28] Importantly, atrial stretch results in inflammation that contribute to fibroblast proliferation, collagen elaboration and scar formation. [29] Structural remodeling is ongoing with AF and thought to be partially mediated by transforming growth factor β1 (TGF-β1), which is a potent stimulator of collagen-producing cardiac fibroblasts. [30]
Atrial structural changes observed in animal models of AF include atrial enlargement, cellular hypertrophy, dedifferentiation, fibrosis, apoptosis, loss of contractile apparatus (myolysis), changes in size and shape of the mitochondria, disruption of the sarcoplasmatic reticulum, and homogeneous distribution of nuclear heterochromatin. [31] The changes in structural, contractile, and electrical properties disrupt interconnections between cardiac muscle bundles produces anisotropy that causes micro-reentry circuits. The resulting electrophysiological substrate is characterized by shortening of atrial refractoriness and reentrant wavelength or by local conduction heterogeneities caused by disruption of electrical interconnections between muscle bundles, which predisposes patients to develop AF. [32], [33] [16] [34]
Anatomical Enhancers of Atrial Fibrillation substrate
Ganglionated plexi
Epicardial fat also contains a rich supply of autonomic ganglionated plexi (GP), which has gained attention in the creation of AF substrate. GPs are found embedded along the ligament of Marshall, along the great vessels, at the right superior PV-atrial junction, at the left superior PV-atrial junction, at the left inferior PV-atrial junction, and at the junction of the inferior vena cava and both atria. [35], [36] [Figure 1] GP stimulation by the autonomic nervous system has been hypothesized to release neurotransmitters that increase PV ectopy [37], reduce PV sleeve action potential duration [38], and shorten the fibrillation cycle length.[39] These factors appear to stimulate triggers and enable the perpetuation of AF. [40] The ablation of GP in addition to PVI may result in higher success rates in patients with paroxysmal and persistent AF. [41] Neural remodeling may allow for regrowth of ganglionated plexi [42], however even temporary suppression of ganglionated plexi may have long-term effects in suppressing of AF by breaking the cyclical progression of AF. [43]
Epicardial fat
Recent studies have also implicated epicardial fat in the creation of AF substrate. [44] Adipose tissue is frequently found in the atrioventricular and interventricular grooves extending to the apex of the heart. There are also minor regions of fat that are located subepicardially around the 2 appendages and in the free walls of the atria. [Figure 1] Epicardial fat may have direct electrophysiologic effects as well as possible paracrine effects by cytokines or other signaling molecules. [45] Epicardial adipose tissue express a wide range of inflammatory mediators and demonstrate increased activity of matrix metalloproteinases which likely contribute to interstitial fibrosis, [46] Since epicardial fat is often associated with fatty infiltration deep into the myocardial tissue, this disorganized tissue may contribute to local arrhythmogenic substrate.
Contribution of Comorbidities and Environmental Factors towards the Development of Atrial Fibrillation: Accelerators of Fibrosis
Hypertension
Stress from any source, whether endocardial or epicardial, applied to the left atrium leads to tissue remodeling and fibrogenesis. [47] The most common stressor is hypertension. In the DECAAF trial, hypertension was the only predictor of the degree of atrial fibrosis in patients with atrial fibrillation. [6] As an independent predictor of AF, hypertension causes remodeling of small and large vessels where low-grade inflammation and associated elaboration of C-Reactive Protein are thought to play important roles in triggering fibrosis. A chronic increase in internal atrial pressure also causes atrial stretch that has been implicated in inflammation, apoptosis and atrial remodeling.
Pressure induced fibrosis has been studied in an experimental porcine animal model. Ventricular tachypacing resulted in an increase in atrial volume of 60%, a two-fold rise in pressure and a complex pattern of local mechanical, histological and biochemical changes including fibrosis. The authors used a comparison of the stress distribution in healthy versus ventricular tachypacing cases to determine how volume overload and stress affects and modifies left atrial mechanics. The largest areas of stretch-induced changes were around the lower pulmonary veins and the appendage boundaries. [48] Similar to the pressure overload of hypertension, the pressure and volume overload of mitral regurgitation and mitral stenosis, sleep apnea, or congestive heart failure creates stress in the atria that predispose patients to atrial remodeling, fibrosis, and atrial fibrillation.
Obesity
Obesity as a risk factor for AF has been documented with a two-fold increase in AF compared to age- and sex-matched individuals having a normal weight; this risk of developing AF increases progressively with rising Body Mass Index. [49] With a 2.4 fold increased risk of left atrial enlargement, obesity has the potential to cause stress-mediated progressive atrial remodeling that produces substrates known to initiate or maintain AF. [50] The hemodynamic alterations in obesity such as increased intravascular volume and increased cardiac output may lead to LA volume overload, stress and LA dilatation. Interstitial and epicardial fat may accumulate and contribute to atrial fibrosis enhanced by paracrine effects. Studies have shown that the expansion of adipose tissue with obesity are accompanied by inadequate capillarization, resulting in hypoxia. [51] The increased leptin and reduced adiponectin levels of obesity may contribute to the adverse atrial remodeling. [52] Obesity is also associated with a proinflammatory state and oxidative stress, as evidenced by increased CRP, IL-6, and TNF-α. Finally, the autonomic dysfunction of obesity (increased sympathetic activity and decreased vagal tone) may also contribute to AF inducibility. [53], [54]
AF in Endurance Athletes
In endurance athletes, atrial fibrillation is more common than their age, sex and activity matched peers. The increased left atrial pressure loading and constant supra-physiologic acceleration/deceleration movements placed on the cardiac reflections may cause acute stretch induced electrical changes, fibrosis, and AF. [55] Deconditioning reverses expression of cardiac fibrosis markers in animal models of endurance suggesting that once training is halted and load is removed from the pericardial attachments, the fibrotic process is retarded. [56]
Treatment of Progressive Atrial fibrillation
Current therapies in the ablation of atrial fibrillation focus on the creation of durable lesions (contact force catheters, laser balloon, cryoballoon, nMarq ablation catheter) and the assessment of real-time arrhythmogenic substrate (CFAE and rotor mapping). In centers with expertise in cardiac MRI, pre-ablation substrate assessment and tailored ablation isolating regions of fibrosis shows an appreciation for atrial fibrotic substrate. However all of these therapies generally deal with a patient’s atrial fibrillation at its present state of substrate. As long as the causative factors for atrial stress continue to exist, it would not be surprising that atrial fibrosis would progress, exposing the patient to continued risk for developing atrial fibrillation. Certainly patients with sleep apnea, obesity, and hypertension need to be treated, however complete control of AF risk factors is usually impossible.
Patients with enlarged atrial and heterogeneous AF substrate will likely have more than just focal pulmonary vein triggers as the driver for their disease. This is the reason why more extensive ablation is usually required to treat these patients. Using an endocardial approach only, creation of additional lines to isolate the posterior wall and prevent mitral annular, septal, or right atrial substrate can better address the non-PV substrate of AF, however it is currently limited by issues inherent in the creation of lines using a point-by-point technique. Additionally, an endocardial approach may not address GP, epicardial fat, and other non-PV substrate as thoroughly or as easily as an epicardial approach.
Hybrid procedures have been utilized to treat patients with difficult AF substrate.
The Convergent atrial fibrillation procedure treats a high proportion of left atrial territory that is at high risk for fibrosis and addresses multiple non-PV mechanisms of AF. [57] The Convergent multidisciplinary procedure applies closed chest epicardial ablation of the posterior left atrium via a subxiphoid approach in combination with standard endocardial catheter ablation. This multidisciplinary procedure allows for electrosilencing the posterior wall using epicardial ablation at relevant points juxtaposing the pericardial reflections at their attachments to the left atrium. [Figure 4] The homogenization of the posterior and inferior wall tissue should theoretically prevent further progression of arrhythmogenic patchy atrial fibrosis. Fortunately, ablation of the posterior wall appears to have a minimal impact on left atrial function since the posterior wall contributes less to the left atrial ejection fraction than the anterior, septal and lateral walls.
Figure 4. Panel A: Schematic of the Convergent procedure lesion pattern relative to the high stress regions. Panel B: Thoracoscopic hybrid AF ablation lesion set. Hybrid AF ablation utilizing a thoracoscopic approach commonly involves pulmonary vein isolation, a roof line, posterior box line, exclusion of the left atrial appendage (blue lines). Endocardial ablation is performed to confirm bi-directional block across the lines and create a cavotricuspid isthmus line (red dotted line). Additional ablation may be performed to create an intercaval line, mitral line, and at ganglionated plexi.
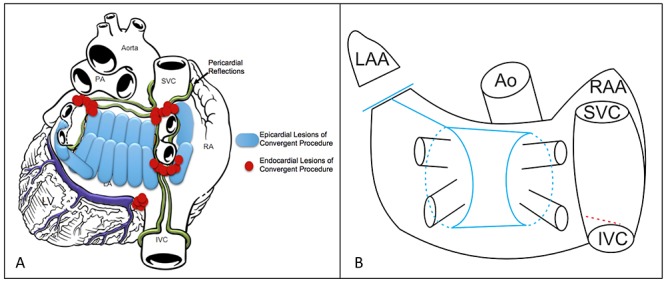
The promising clinical results utilizing this more comprehensive lesion set may lead credence to the role of ablating a wider territory of the left atrium. [58]-[62] Despite the fact that many patients had complex disease and frequently failed prior ablations, operators have reproducibly been reporting success rates in the 73% to 95% range on or off antiarrhythmic therapy at 1-year follow up amongst a mixed population of paroxysmal and persistent AF patients. [63] Although long-term data is pending, homogenization of the posterior wall should prevent posterior wall substrate development. Additionally, epicardial ablation of ganglionated plexi and epicardial fat may aid in the current treatment of and further progression of AF substrate.
Similar to the Convergent procedure, hybrid procedures utilizing a thoracoscopic approach also seek to provide durable isolation of the pulmonary veins and posterior wall. [Figure 4] The ligament of Marshall is easily dissected from a thoracoscopic approach and ligation of the left atrial appendage may yield anti-arrhythmic benefit as well as reducing stroke risk. Additionally, ganglionated plexi may be more readily targeted, and additional linear lesions may also be created and verified across the mitral isthmus and cavotricuspid isthmus. Success rates utilizing a hybrid thoracoscopic technique have also been very favorable in the 84% to 94% range on or off antiarrhythmic therapy at 1-year follow up amonst a mixed population of paroxysmal and persistent AF patients. [64]
Conclusions
In contrast to other organized arrhythmias, atrial fibrillation is an electrically disorganized arrhythmia that is frequently the end product of unfavorable atrial remodeling. Ablative therapy initially began targeting triggers which were frequently found in the pulmonary veins however we have subsequently learned that atrial fibrillation involves much more of the atrium and attention has expanded to additional mechanisms of atrial fibrillation genesis and perpetuation. Recent focus has been on the targeting of functional mechanisms of AF however it remains to be seen if these interventions will result in long-term arrhythmia-free success.
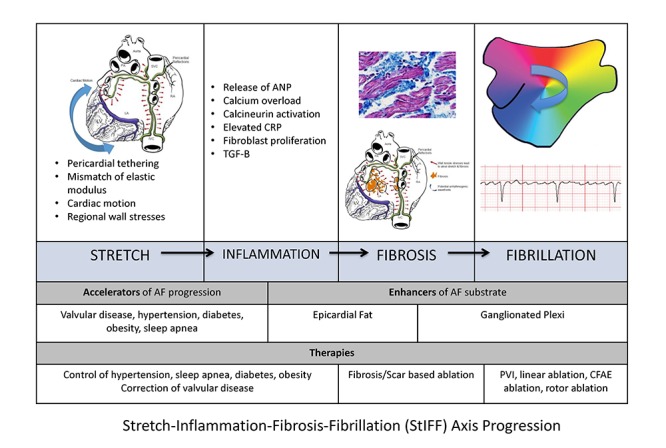
There appears to be a plausible anatomical mechanism for the progression of atrial fibrillation. Mechanical stress placed on the atrium due to its pericardial tethers and repetitive cardiac motion appear to cause stress induced inflammatory changes and fibrosis. These fibrotic changes predispose the atrium to fibrillate. [Figure 5] The failure of current ablative strategies particularly to treat persistent atrial fibrillation may be due to the fact that PVI, linear ablation, CFAE ablation, and rotor ablation probably does not reduce the mechanical nor inflammatory stresses upon the remodeling atrium, and thus does not halt the anatomical progression of atrial fibrillation. This enforces the importance of risk factor reduction: control of hypertension, obesity, sleep apnea. However it also brings to question if there is an anatomic method to reduce the mechanical stresses upon the atrium or pre-treat the areas of atrium most prone to anisotropic fibrosis and AF substrate formation. Since AF is recognized as a progressive disease, treatments that target the progressive nature of fibrosis may result in improved outcomes. Scar-based, or empiric ablation to cover regions of fibrosis prone areas such as BIFA ablation or the homogenization or durable isolation of the posterior wall through a hybrid ablation procedure may better address the progressive nature of AF. Additionally, ablative strategies that target ganglionated plexi and epicardial fat may adjunctively treat and prevent the progression of AF.
Figure 5. Stretch-Inflammation-Fibrosis-Fibrillation (StiFF) Axis.
Disclosures
None.
References
- 1.Lloyd-Jones Donald, Adams Robert J, Brown Todd M, Carnethon Mercedes, Dai Shifan, De Simone Giovanni, Ferguson T Bruce, Ford Earl, Furie Karen, Gillespie Cathleen, Go Alan, Greenlund Kurt, Haase Nancy, Hailpern Susan, Ho P Michael, Howard Virginia, Kissela Brett, Kittner Steven, Lackland Daniel, Lisabeth Lynda, Marelli Ariane, McDermott Mary M, Meigs James, Mozaffarian Dariush, Mussolino Michael, Nichol Graham, Roger Véronique L, Rosamond Wayne, Sacco Ralph, Sorlie Paul, Stafford Randall, Thom Thomas, Wasserthiel-Smoller Sylvia, Wong Nathan D, Wylie-Rosett Judith. Executive summary: heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010 Feb 23;121 (7):948–54. doi: 10.1161/CIRCULATIONAHA.109.192666. [DOI] [PubMed] [Google Scholar]
- 2.Fuster Valentin, Rydén Lars E, Cannom Davis S, Crijns Harry J, Curtis Anne B, Ellenbogen Kenneth A, Halperin Jonathan L, Kay G Neal, Le Huezey Jean-Yves, Lowe James E, Olsson S Bertil, Prystowsky Eric N, Tamargo Juan Luis, Wann L Samuel, Smith Sidney C, Priori Silvia G, Estes N A Mark, Ezekowitz Michael D, Jackman Warren M, January Craig T, Lowe James E, Page Richard L, Slotwiner David J, Stevenson William G, Tracy Cynthia M, Jacobs Alice K, Anderson Jeffrey L, Albert Nancy, Buller Christopher E, Creager Mark A, Ettinger Steven M, Guyton Robert A, Halperin Jonathan L, Hochman Judith S, Kushner Frederick G, Ohman Erik Magnus, Stevenson William G, Tarkington Lynn G, Yancy Clyde W. 2011 ACCF/AHA/HRS focused updates incorporated into the ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011 Mar 15;123 (10):e269–367. doi: 10.1161/CIR.0b013e318214876d. [DOI] [PubMed] [Google Scholar]
- 3.Chugh Sumeet S, Havmoeller Rasmus, Narayanan Kumar, Singh David, Rienstra Michiel, Benjamin Emelia J, Gillum Richard F, Kim Young-Hoon, McAnulty John H, Zheng Zhi-Jie, Forouzanfar Mohammad H, Naghavi Mohsen, Mensah George A, Ezzati Majid, Murray Christopher J L. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014 Feb 25;129 (8):837–47. doi: 10.1161/CIRCULATIONAHA.113.005119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Calkins Hugh, Kuck Karl Heinz, Cappato Riccardo, Brugada Josep, Camm A John, Chen Shih-Ann, Crijns Harry J G, Damiano Ralph J, Davies D Wyn, DiMarco John, Edgerton James, Ellenbogen Kenneth, Ezekowitz Michael D, Haines David E, Haissaguerre Michel, Hindricks Gerhard, Iesaka Yoshito, Jackman Warren, Jalife Jose, Jais Pierre, Kalman Jonathan, Keane David, Kim Young-Hoon, Kirchhof Paulus, Klein George, Kottkamp Hans, Kumagai Koichiro, Lindsay Bruce D, Mansour Moussa, Marchlinski Francis E, McCarthy Patrick M, Mont J Lluis, Morady Fred, Nademanee Koonlawee, Nakagawa Hiroshi, Natale Andrea, Nattel Stanley, Packer Douglas L, Pappone Carlo, Prystowsky Eric, Raviele Antonio, Reddy Vivek, Ruskin Jeremy N, Shemin Richard J, Tsao Hsuan-Ming, Wilber David. 2012 HRS/EHRA/ECAS Expert Consensus Statement on Catheter and Surgical Ablation of Atrial Fibrillation: recommendations for patient selection, procedural techniques, patient management and follow-up, definitions, endpoints, and research trial design. Europace. 2012 Apr;14 (4):528–606. doi: 10.1093/europace/eus027. [DOI] [PubMed] [Google Scholar]
- 5.Marrouche Nassir F, Wilber David, Hindricks Gerhard, Jais Pierre, Akoum Nazem, Marchlinski Francis, Kholmovski Eugene, Burgon Nathan, Hu Nan, Mont Lluis, Deneke Thomas, Duytschaever Mattias, Neumann Thomas, Mansour Moussa, Mahnkopf Christian, Herweg Bengt, Daoud Emile, Wissner Erik, Bansmann Paul, Brachmann Johannes. Association of atrial tissue fibrosis identified by delayed enhancement MRI and atrial fibrillation catheter ablation: the DECAAF study. JAMA. 2014 Feb 05;311 (5):498–506. doi: 10.1001/jama.2014.3. [DOI] [PubMed] [Google Scholar]
- 6.Weerasooriya Rukshen, Khairy Paul, Litalien Jean, Macle Laurent, Hocini Meleze, Sacher Frederic, Lellouche Nicolas, Knecht Sebastien, Wright Matthew, Nault Isabelle, Miyazaki Shinsuke, Scavee Christophe, Clementy Jacques, Haissaguerre Michel, Jais Pierre. Catheter ablation for atrial fibrillation: are results maintained at 5 years of follow-up? J. Am. Coll. Cardiol. 2011 Jan 11;57 (2):160–6. doi: 10.1016/j.jacc.2010.05.061. [DOI] [PubMed] [Google Scholar]
- 7.Chao Tze-Fan, Tsao Hsuan-Ming, Lin Yenn-Jiang, Tsai Chin-Feng, Lin Wei-Shiang, Chang Shih-Lin, Lo Li-Wei, Hu Yu-Feng, Tuan Ta-Chuan, Suenari Kazuyoshi, Li Cheng-Hung, Hartono Beny, Chang Hung-Yu, Ambrose Kibos, Wu Tsu-Juey, Chen Shih-Ann. Clinical outcome of catheter ablation in patients with nonparoxysmal atrial fibrillation: results of 3-year follow-up. Circ Arrhythm Electrophysiol. 2012 Jun 01;5 (3):514–20. doi: 10.1161/CIRCEP.111.968032. [DOI] [PubMed] [Google Scholar]
- 8.Chao Tze-Fan, Tsao Hsuan-Ming, Lin Yenn-Jiang, Tsai Chin-Feng, Lin Wei-Shiang, Chang Shih-Lin, Lo Li-Wei, Hu Yu-Feng, Tuan Ta-Chuan, Suenari Kazuyoshi, Li Cheng-Hung, Hartono Beny, Chang Hung-Yu, Ambrose Kibos, Wu Tsu-Juey, Chen Shih-Ann. Clinical outcome of catheter ablation in patients with nonparoxysmal atrial fibrillation: results of 3-year follow-up. Circ Arrhythm Electrophysiol. 2012 Jun 01;5 (3):514–20. doi: 10.1161/CIRCEP.111.968032. [DOI] [PubMed] [Google Scholar]
- 9.Gillinov A Marc, Gelijns Annetine C, Parides Michael K, DeRose Joseph J, Moskowitz Alan J, Voisine Pierre, Ailawadi Gorav, Bouchard Denis, Smith Peter K, Mack Michael J, Acker Michael A, Mullen John C, Rose Eric A, Chang Helena L, Puskas John D, Couderc Jean-Philippe, Gardner Timothy J, Varghese Robin, Horvath Keith A, Bolling Steven F, Michler Robert E, Geller Nancy L, Ascheim Deborah D, Miller Marissa A, Bagiella Emilia, Moquete Ellen G, Williams Paula, Taddei-Peters Wendy C, O'Gara Patrick T, Blackstone Eugene H, Argenziano Michael. Surgical ablation of atrial fibrillation during mitral-valve surgery. N. Engl. J. Med. 2015 Apr 09;372 (15):1399–409. doi: 10.1056/NEJMoa1500528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tilz Roland Richard, Rillig Andreas, Thum Anna-Maria, Arya Anita, Wohlmuth Peter, Metzner Andreas, Mathew Shibu, Yoshiga Yasuhiro, Wissner Erik, Kuck Karl-Heinz, Ouyang Feifan. Catheter ablation of long-standing persistent atrial fibrillation: 5-year outcomes of the Hamburg Sequential Ablation Strategy. J. Am. Coll. Cardiol. 2012 Nov 06;60 (19):1921–9. doi: 10.1016/j.jacc.2012.04.060. [DOI] [PubMed] [Google Scholar]
- 11.Haïssaguerre M, Jaïs P, Shah D C, Takahashi A, Hocini M, Quiniou G, Garrigue S, Le Mouroux A, Le Métayer P, Clémenty J. Spontaneous initiation of atrial fibrillation by ectopic beats originating in the pulmonary veins. N. Engl. J. Med. 1998 Sep 03;339 (10):659–66. doi: 10.1056/NEJM199809033391003. [DOI] [PubMed] [Google Scholar]
- 12.Ho S Y, Sanchez-Quintana D, Cabrera J A, Anderson R H. Anatomy of the left atrium: implications for radiofrequency ablation of atrial fibrillation. J. Cardiovasc. Electrophysiol. 1999 Nov;10 (11):1525–33. doi: 10.1111/j.1540-8167.1999.tb00211.x. [DOI] [PubMed] [Google Scholar]
- 13.Hassink Rutger J, Aretz H Thomas, Ruskin Jeremy, Keane David. Morphology of atrial myocardium in human pulmonary veins: a postmortem analysis in patients with and without atrial fibrillation. J. Am. Coll. Cardiol. 2003 Sep 17;42 (6):1108–14. doi: 10.1016/s0735-1097(03)00918-5. [DOI] [PubMed] [Google Scholar]
- 14.Spach M S, Boineau J P. Microfibrosis produces electrical load variations due to loss of side-to-side cell connections: a major mechanism of structural heart disease arrhythmias. Pacing Clin Electrophysiol. 1997 Feb;20 (2 Pt 2):397–413. doi: 10.1111/j.1540-8159.1997.tb06199.x. [DOI] [PubMed] [Google Scholar]
- 15.Ogawa Masahiro, Zhou Shengmei, Tan Alex Y, Song Juan, Gholmieh Ghassan, Fishbein Michael C, Luo Huai, Siegel Robert J, Karagueuzian Hrayr S, Chen Lan S, Lin Shien-Fong, Chen Peng-Sheng. Left stellate ganglion and vagal nerve activity and cardiac arrhythmias in ambulatory dogs with pacing-induced congestive heart failure. J. Am. Coll. Cardiol. 2007 Jul 24;50 (4):335–43. doi: 10.1016/j.jacc.2007.03.045. [DOI] [PubMed] [Google Scholar]
- 16.Allessie Maurits, Ausma Jannie, Schotten Ulrich. Electrical, contractile and structural remodeling during atrial fibrillation. Cardiovasc. Res. 2002 May;54 (2):230–46. doi: 10.1016/s0008-6363(02)00258-4. [DOI] [PubMed] [Google Scholar]
- 17.Kalifa Jérôme, Tanaka Kazuhiko, Zaitsev Alexey V, Warren Mark, Vaidyanathan Ravi, Auerbach David, Pandit Sandeep, Vikstrom Karen L, Ploutz-Snyder Robert, Talkachou Arkadzi, Atienza Felipe, Guiraudon Gérard, Jalife José, Berenfeld Omer. Mechanisms of wave fractionation at boundaries of high-frequency excitation in the posterior left atrium of the isolated sheep heart during atrial fibrillation. Circulation. 2006 Feb 07;113 (5):626–33. doi: 10.1161/CIRCULATIONAHA.105.575340. [DOI] [PubMed] [Google Scholar]
- 18.Roberts-Thomson Kurt C, Stevenson Irene, Kistler Peter M, Haqqani Haris M, Spence Steven J, Goldblatt John C, Sanders Prashanthan, Kalman Jonathan M. The role of chronic atrial stretch and atrial fibrillation on posterior left atrial wall conduction. Heart Rhythm. 2009 Aug;6 (8):1109–17. doi: 10.1016/j.hrthm.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Janse M J. Why does atrial fibrillation occur? Eur. Heart J. 1997 May;18 Suppl C ():C12–8. doi: 10.1093/eurheartj/18.suppl_c.12. [DOI] [PubMed] [Google Scholar]
- 20.Cochet Hubert, Mouries Amaury, Nivet Hubert, Sacher Frederic, Derval Nicolas, Denis Arnaud, Merle Mathilde, Relan Jatin, Hocini Mélèze, Haïssaguerre Michel, Laurent François, Montaudon Michel, Jaïs Pierre. Age, atrial fibrillation, and structural heart disease are the main determinants of left atrial fibrosis detected by delayed-enhanced magnetic resonance imaging in a general cardiology population. J. Cardiovasc. Electrophysiol. 2015 May;26 (5):484–92. doi: 10.1111/jce.12651. [DOI] [PubMed] [Google Scholar]
- 21.Ouyang Feifan, Bänsch Dietmar, Ernst Sabine, Schaumann Anselm, Hachiya Hitoshi, Chen Minglong, Chun Julian, Falk Peter, Khanedani Afsaneh, Antz Matthias, Kuck Karl-Heinz. Complete isolation of left atrium surrounding the pulmonary veins: new insights from the double-Lasso technique in paroxysmal atrial fibrillation. Circulation. 2004 Oct 12;110 (15):2090–6. doi: 10.1161/01.CIR.0000144459.37455.EE. [DOI] [PubMed] [Google Scholar]
- 22.Verma Atul, Marrouche Nassir F, Natale Andrea. Pulmonary vein antrum isolation: intracardiac echocardiography-guided technique. J. Cardiovasc. Electrophysiol. 2004 Nov;15 (11):1335–40. doi: 10.1046/j.1540-8167.2004.04428.x. [DOI] [PubMed] [Google Scholar]
- 23.Chilukuri Karuna, Scherr Daniel, Dalal Darshan, Cheng Alan, Spragg David, Nazarian Saman, Barcelon Bernadette D, Marine Joseph E, Calkins Hugh, Henrikson Charles A. Conventional pulmonary vein isolation compared with the "box isolation" method: a randomized clinical trial. J Interv Card Electrophysiol. 2011 Nov;32 (2):137–46. doi: 10.1007/s10840-011-9587-8. [DOI] [PubMed] [Google Scholar]
- 24.Kottkamp Hans, Bender Roderich, Berg Jan. Catheter ablation of atrial fibrillation: how to modify the substrate? J. Am. Coll. Cardiol. 2015 Jan 20;65 (2):196–206. doi: 10.1016/j.jacc.2014.10.034. [DOI] [PubMed] [Google Scholar]
- 25.Laizzo P. Handbook of Cardiac Anatomy, Physiology, and Devices. 2nd Edition ed. Humana Press. 2009;0:0–0. [Google Scholar]
- 26.Suenari Kazuyoshi, Nakano Yukiko, Hirai Yukoh, Ogi Hiroshi, Oda Noboru, Makita Yuko, Ueda Shigeyuki, Kajihara Kenta, Tokuyama Takehito, Motoda Chikaaki, Fujiwara Mai, Chayama Kazuaki, Kihara Yasuki. Left atrial thickness under the catheter ablation lines in patients with paroxysmal atrial fibrillation: insights from 64-slice multidetector computed tomography. Heart Vessels. 2013 May;28 (3):360–8. doi: 10.1007/s00380-012-0253-6. [DOI] [PubMed] [Google Scholar]
- 27.Hunter Ross J, Liu Yankai, Lu Yiling, Wang Wen, Schilling Richard J. Left atrial wall stress distribution and its relationship to electrophysiologic remodeling in persistent atrial fibrillation. Circ Arrhythm Electrophysiol. 2012 Apr;5 (2):351–60. doi: 10.1161/CIRCEP.111.965541. [DOI] [PubMed] [Google Scholar]
- 28.Saygili Erol, Rana Obaida R, Meyer Christian, Gemein Christopher, Andrzejewski Michael G, Ludwig Andreas, Weber Christian, Schotten Ulrich, Krüttgen Alexander, Weis Joachim, Schwinger Robert H G, Mischke Karl, Rassaf Tienush, Kelm Malte, Schauerte Patrick. The angiotensin-calcineurin-NFAT pathway mediates stretch-induced up-regulation of matrix metalloproteinases-2/-9 in atrial myocytes. Basic Res. Cardiol. 2009 Jul;104 (4):435–48. doi: 10.1007/s00395-008-0772-6. [DOI] [PubMed] [Google Scholar]
- 29.Schotten Ulrich, Duytschaever Mattias, Ausma Jannie, Eijsbouts Sabine, Neuberger Hans-Ruprecht, Allessie Maurits. Electrical and contractile remodeling during the first days of atrial fibrillation go hand in hand. Circulation. 2003 Mar 18;107 (10):1433–9. doi: 10.1161/01.cir.0000055314.10801.4f. [DOI] [PubMed] [Google Scholar]
- 30.Khan Razi, Sheppard Richard. Fibrosis in heart disease: understanding the role of transforming growth factor-beta in cardiomyopathy, valvular disease and arrhythmia. Immunology. 2006 May;118 (1):10–24. doi: 10.1111/j.1365-2567.2006.02336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schotten Ulrich, Verheule Sander, Kirchhof Paulus, Goette Andreas. Pathophysiological mechanisms of atrial fibrillation: a translational appraisal. Physiol. Rev. 2011 Jan;91 (1):265–325. doi: 10.1152/physrev.00031.2009. [DOI] [PubMed] [Google Scholar]
- 32.Verheule Sander, Wilson Emily, Banthia Smriti, Everett Thomas H, Shanbhag Sujata, Sih Haris J, Olgin Jeffrey. Direction-dependent conduction abnormalities in a canine model of atrial fibrillation due to chronic atrial dilatation. Am. J. Physiol. Heart Circ. Physiol. 2004 Aug;287 (2):H634–44. doi: 10.1152/ajpheart.00014.2004. [DOI] [PubMed] [Google Scholar]
- 33.Verheule Sander, Wilson Emily, Everett Thomas, Shanbhag Sujata, Golden Catherine, Olgin Jeffrey. Alterations in atrial electrophysiology and tissue structure in a canine model of chronic atrial dilatation due to mitral regurgitation. Circulation. 2003 May 27;107 (20):2615–22. doi: 10.1161/01.CIR.0000066915.15187.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Casaclang-Verzosa Grace, Gersh Bernard J, Tsang Teresa S M. Structural and functional remodeling of the left atrium: clinical and therapeutic implications for atrial fibrillation. J. Am. Coll. Cardiol. 2008 Jan 01;51 (1):1–11. doi: 10.1016/j.jacc.2007.09.026. [DOI] [PubMed] [Google Scholar]
- 35.Chevalier Philippe, Tabib Alain, Meyronnet David, Chalabreysse Lara, Restier Lioara, Ludman Valérie, Aliès Alexandre, Adeleine Patrice, Thivolet Françoise, Burri Haran, Loire Robert, François Laurent, Fanton Laurent. Quantitative study of nerves of the human left atrium. Heart Rhythm. 2005 May;2 (5):518–22. doi: 10.1016/j.hrthm.2005.01.022. [DOI] [PubMed] [Google Scholar]
- 36.Tan Alex Y, Li Hongmei, Wachsmann-Hogiu Sebastian, Chen Lan S, Chen Peng-Sheng, Fishbein Michael C. Autonomic innervation and segmental muscular disconnections at the human pulmonary vein-atrial junction: implications for catheter ablation of atrial-pulmonary vein junction. J. Am. Coll. Cardiol. 2006 Jul 04;48 (1):132–43. doi: 10.1016/j.jacc.2006.02.054. [DOI] [PubMed] [Google Scholar]
- 37.Zhou Jing, Scherlag Benjamin J, Edwards Jeffery, Jackman Warren M, Lazzara Ralph, Po Sunny S. Gradients of atrial refractoriness and inducibility of atrial fibrillation due to stimulation of ganglionated plexi. J. Cardiovasc. Electrophysiol. 2007 Jan;18 (1):83–90. doi: 10.1111/j.1540-8167.2006.00679.x. [DOI] [PubMed] [Google Scholar]
- 38.Patterson Eugene, Po Sunny S, Scherlag Benjamin J, Lazzara Ralph. Triggered firing in pulmonary veins initiated by in vitro autonomic nerve stimulation. Heart Rhythm. 2005 Jun;2 (6):624–31. doi: 10.1016/j.hrthm.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 39.Scherlag Benjamin J, Nakagawa Hiroshi, Jackman Warren M, Yamanashi William S, Patterson Eugene, Po Sunny, Lazzara Ralph. Electrical stimulation to identify neural elements on the heart: their role in atrial fibrillation. J Interv Card Electrophysiol. 2005 Aug;13 Suppl 1 ():37–42. doi: 10.1007/s10840-005-2492-2. [DOI] [PubMed] [Google Scholar]
- 40.Jiang Ru-Hong, Jiang Chen-Yang, Sheng Xia, Zhang Zu-Wen, Sun Ya-Xun, Liu Qiang, Fu Guo-Sheng, Po Sunny S. Marked suppression of pulmonary vein firing after circumferential pulmonary vein isolation in patients with paroxysmal atrial fibrillation: is pulmonary vein firing an epiphenomenon? J. Cardiovasc. Electrophysiol. 2014 Feb;25 (2):111–8. doi: 10.1111/jce.12288. [DOI] [PubMed] [Google Scholar]
- 41.Katritsis Demosthenes G, Pokushalov Evgeny, Romanov Alexander, Giazitzoglou Eleftherios, Siontis George C M, Po Sunny S, Camm A John, Ioannidis John P A. Autonomic denervation added to pulmonary vein isolation for paroxysmal atrial fibrillation: a randomized clinical trial. J. Am. Coll. Cardiol. 2013 Dec 17;62 (24):2318–25. doi: 10.1016/j.jacc.2013.06.053. [DOI] [PubMed] [Google Scholar]
- 42.Wang Ximin, Zhang Ming, Zhang Yujiao, Xie Xinxing, Wang Weizong, Li Zhan, Gao Mei, Wang Zhongsu, Hou Yinglong. Long-Term Effects of Ganglionated Plexi Ablation on Electrophysiological Characteristics and Neuron Remodeling in Target Atrial Tissues in a Canine Model. Circ Arrhythm Electrophysiol. 2015 Oct;8 (5):1276–83. doi: 10.1161/CIRCEP.114.002554. [DOI] [PubMed] [Google Scholar]
- 43.Lo Li-Wei, Chang Hung-Yu, Scherlag Benjamin J, Lin Yenn-Jiang, Chou Yu-Hui, Lin Wei-Lun, Chen Shih-Ann, Po Sunny S. Temporary Suppression of Cardiac Ganglionated Plexi Leads to Long-Term Suppression of Atrial Fibrillation: Evidence of Early Autonomic Intervention to Break the Vicious Cycle of "AF Begets AF". J Am Heart Assoc. 2016 Jul 05;5 (7) doi: 10.1161/JAHA.116.003309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hatem Stéphane N, Redheuil Alban, Gandjbakhch Estelle. Cardiac adipose tissue and atrial fibrillation: the perils of adiposity. Cardiovasc. Res. 2016 Apr 01;109 (4):502–9. doi: 10.1093/cvr/cvw001. [DOI] [PubMed] [Google Scholar]
- 45.Hatem Stéphane N, Sanders Prashanthan. Epicardial adipose tissue and atrial fibrillation. Cardiovasc. Res. 2014 May 01;102 (2):205–13. doi: 10.1093/cvr/cvu045. [DOI] [PubMed] [Google Scholar]
- 46.Mazurek Tomasz, Zhang LiFeng, Zalewski Andrew, Mannion John D, Diehl James T, Arafat Hwyda, Sarov-Blat Lea, O'Brien Shawn, Keiper Elizabeth A, Johnson Anthony G, Martin Jack, Goldstein Barry J, Shi Yi. Human epicardial adipose tissue is a source of inflammatory mediators. Circulation. 2003 Nov 18;108 (20):2460–6. doi: 10.1161/01.CIR.0000099542.57313.C5. [DOI] [PubMed] [Google Scholar]
- 47.Everett Thomas H, Olgin Jeffrey E. Atrial fibrosis and the mechanisms of atrial fibrillation. Heart Rhythm. 2007 Mar;4 (3 Suppl):S24–7. doi: 10.1016/j.hrthm.2006.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Di Martino Elena S, Bellini Chiara, Schwartzman David S. In vivo porcine left atrial wall stress: Effect of ventricular tachypacing on spatial and temporal stress distribution. J Biomech. 2011 Nov 10;44 (16):2755–60. doi: 10.1016/j.jbiomech.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 49.Frost Lars, Hune Lone Juul, Vestergaard Peter. Overweight and obesity as risk factors for atrial fibrillation or flutter: the Danish Diet, Cancer, and Health Study. Am. J. Med. 2005 May;118 (5):489–95. doi: 10.1016/j.amjmed.2005.01.031. [DOI] [PubMed] [Google Scholar]
- 50.Stritzke Jan, Markus Marcello Ricardo Paulista, Duderstadt Stefanie, Lieb Wolfgang, Luchner Andreas, Döring Angela, Keil Ulrich, Hense Hans-Werner, Schunkert Heribert. The aging process of the heart: obesity is the main risk factor for left atrial enlargement during aging the MONICA/KORA (monitoring of trends and determinations in cardiovascular disease/cooperative research in the region of Augsburg) study. J. Am. Coll. Cardiol. 2009 Nov 17;54 (21):1982–9. doi: 10.1016/j.jacc.2009.07.034. [DOI] [PubMed] [Google Scholar]
- 51.Ye Jianping, Gao Zhanguo, Yin Jun, He Qing. Hypoxia is a potential risk factor for chronic inflammation and adiponectin reduction in adipose tissue of ob/ob and dietary obese mice. Am. J. Physiol. Endocrinol. Metab. 2007 Oct;293 (4):E1118–28. doi: 10.1152/ajpendo.00435.2007. [DOI] [PubMed] [Google Scholar]
- 52.Ochiai Hirotaka, Shirasawa Takako, Nishimura Rimei, Nanri Hinako, Ohtsu Tadahiro, Hoshino Hiromi, Tajima Naoko, Kokaze Akatsuki. Abdominal obesity and serum adiponectin complexes among population-based elementary school children in Japan: a cross-sectional study. BMC Pediatr. 2014 Mar 26;14 () doi: 10.1186/1471-2431-14-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Musaad Salma, Haynes Erin N. Biomarkers of obesity and subsequent cardiovascular events. Epidemiol Rev. 2007;29 ():98–114. doi: 10.1093/epirev/mxm005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Karason K, Mølgaard H, Wikstrand J, Sjöström L. Heart rate variability in obesity and the effect of weight loss. Am. J. Cardiol. 1999 Apr 15;83 (8):1242–7. doi: 10.1016/s0002-9149(99)00066-1. [DOI] [PubMed] [Google Scholar]
- 55.Hoogsteen Jan, Schep Goof, Van Hemel Norbert M, Van Der Wall Ernst E. Paroxysmal atrial fibrillation in male endurance athletes. A 9-year follow up. Europace. 2004 May;6 (3):222–8. doi: 10.1016/j.eupc.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 56.Benito Begoña, Gay-Jordi Gemma, Serrano-Mollar Anna, Guasch Eduard, Shi Yanfen, Tardif Jean-Claude, Brugada Josep, Nattel Stanley, Mont Lluis. Cardiac arrhythmogenic remodeling in a rat model of long-term intensive exercise training. Circulation. 2011 Jan 04;123 (1):13–22. doi: 10.1161/CIRCULATIONAHA.110.938282. [DOI] [PubMed] [Google Scholar]
- 57.Geršak Borut, Zembala Michael O, Müller Dirk, Folliguet Thierry, Jan Matevz, Kowalski Oskar, Erler Stefan, Bars Clement, Robic Boris, Filipiak Krzysztof, Wimmer-Greinecker Gerhard. European experience of the convergent atrial fibrillation procedure: multicenter outcomes in consecutive patients. J. Thorac. Cardiovasc. Surg. 2014 Apr;147 (4):1411–6. doi: 10.1016/j.jtcvs.2013.06.057. [DOI] [PubMed] [Google Scholar]
- 58.Gersak Borut, Pernat Andrej, Robic Boris, Sinkovec Matjaz. Low rate of atrial fibrillation recurrence verified by implantable loop recorder monitoring following a convergent epicardial and endocardial ablation of atrial fibrillation. J. Cardiovasc. Electrophysiol. 2012 Oct;23 (10):1059–66. doi: 10.1111/j.1540-8167.2012.02355.x. [DOI] [PubMed] [Google Scholar]
- 59.KC Civello, CA Smith, Boedefeld W. Combined endocardial and epicardial ablation for symptomatic atrial fibrillation: single center experience in 100+ consecutive patients. J Innov Cardiac Rhythm Mgmt. 2013;0:1–7. [Google Scholar]
- 60.DM Gilligan, CA Joyner, GM Gundy. Multidisciplinary collaboration for the treatment of atrial fibrillation: Convergent procedure outcomes from a single center. J Innov Cardiac Rhythm Mgmt. 2013;0:1–8. [Google Scholar]
- 61.Thosani Amit J, Gerczuk Paul, Liu Emerson, Belden William, Moraca Robert. Closed Chest Convergent Epicardial-Endocardial Ablation of Non-paroxysmal Atrial Fibrillation - A Case Series and Literature Review. Arrhythm Electrophysiol Rev. 2013 Apr;2 (1):65–8. doi: 10.15420/aer.2013.2.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Zembala Michal, Filipiak Krzysztof, Kowalski Oskar, Buchta Piotr, Niklewski Tomasz, Nadziakiewicz Pawel, Koba Rafał, Gąsior Mariusz, Kalarus Zbigniew, Zembala Marian. Staged hybrid ablation for persistent and longstanding persistent atrial fibrillation effectively restores sinus rhythm in long-term observation. Arch Med Sci. 2017 Feb 01;13 (1):109–117. doi: 10.5114/aoms.2015.53960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zembala Michael O, Suwalski Piotr. Minimally invasive surgery for atrial fibrillation. J Thorac Dis. 2013 Nov;5 Suppl 6 ():S704–12. doi: 10.3978/j.issn.2072-1439.2013.10.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kumar Prabhat, Kiser Andy C, Gehi Anil K. Hybrid treatment of atrial fibrillation. Prog Cardiovasc Dis. 2015 Aug 15;58 (2):213–20. doi: 10.1016/j.pcad.2015.08.001. [DOI] [PubMed] [Google Scholar]


