Abstract
Dramatic differences in health are closely related to degrees of social and economic disadvantage. Poverty-induced hardships such as food insecurity, utility shut-offs and substandard housing all have the potential to negatively impact the health of families. In an effort to better address social determinants of health in pediatric primary health care settings using the Medical Legal Partnership model of health care delivery, a multi-disciplinary team of investigators came together to design an innovative process for using computerized clinical decision support to identify health-harming legal and social needs, improve the delivery of appropriate physician counseling and streamline access to legal and social service professionals when non-medical remedies are required. This article describes the multidisciplinary nature of the MLP model itself, illustrates the work that was done to craft this innovative health informatics approach to implementing MLP, and demonstrates how pediatricians, social workers and attorneys may work together to improve child health outcomes.
Introduction
The National Center for Medical Legal Partnership (MLP) defines MLP as an innovative health care delivery model that fully engages the expertise of a multidisciplinary team of professionals to improve the health and wellbeing of low-income and other vulnerable populations by addressing unmet legal needs and removing legal barriers that impede access to care (National Center for Medical Legal Partnership, 2014). This model focuses specifically on social determinants of health, described by the U.S. Centers for Disease Control and Prevention as the circumstances into which people are born, live, and work; and the systems that are put in place to deal with illness and disability. These circumstances are shaped by economics, social policies and politics (U.S. Centers for Disease Control and Prevention, 2014). In contrast, traditional health care delivery models generally overlook non-medical determinants of health – focusing exclusively on biomedical determinants.
In recent years, research has increasingly considered the impact that social determinants have on individual health (Bravemen, Egerter & Mockenhaupt, 2011). Health economists have estimated that medical care accounts for only 10% of overall health, with social, environmental and behavioral factors accounting for the remaining 90% (Asch & Volpp, 2012). The health of children, in particular, may be adversely affected by poor social conditions because they have so little control over the factors contributing to those conditions, and improving the health of a child has the likely long-term effect of improving the health of the adult that child will become. The national MLP movement arose in response to the realization that upstream interventions to address social determinants of health using non-traditional, multidisciplinary teams of helping professionals would likely have the downstream effect of improving health outcomes for disadvantaged individuals and communities.
In an effort to expand the MLP concept to better address social determinants of health in clinical primary health care settings, and help mitigate adverse health outcomes among children using health information technology, investigators with expertise in the fields of law, medicine, public health and informatics came together at the Indiana University School of Medicine to try something new. Together, they designed an innovative process for using computerized clinical decision support to identify health-harming legal and social needs, improve the delivery of appropriate physician counseling, and streamline access to legal and social service professionals when non-medical remedies are required. In this article, we first describe the multidisciplinary nature of the MLP model. We then illustrate the work of the interprofessional team that came together at Indiana University to design, launch and evaluate an innovative health informatics approach to implementing MLP. Lastly, we explain how the Child Health Improvement through Computer Automation, Medical Legal Partnership (CHICA MLP) module actually operates, and demonstrate how it facilitates pediatricians, social workers and attorneys working together to address social determinants of health that may adversely impact child health outcomes.
Medical Legal Partnership: A Model of Interprofessional Practice
It has been well established that health outcomes are closely related to degrees of social and economic disadvantage, and that interventions addressing social determinants of health can help reduce disparities (Williams, Costa, et al., 2008). Consider, for example, poverty-induced hardships such as food insecurity, utility shut-offs and substandard housing or homelessness - all of which clearly have the potential to negatively impact a family’s health. In the United States, there exist a variety of public health protections designed to help address such issues, and legal remedies for these problems are frequently available to those who know how to access them. Much like access to nutritious food, however, access to legal assistance is often limited by social and economic disadvantage. Fewer than one in five legal problems experienced by low-income individuals are addressed with the help of an attorney who understands how to successfully navigate the legal system (Legal Services Corporation, 2007).
To further illustrate how the health status of a child living in poverty may be negatively affected when he or she does not receive the benefit of public health laws designed to help address common social determinants of health, consider the following. A substandard rental home environment may lead to an increased risk of preventable injury or, in the case of dangerous molds, asthma. An excessively cold environment brought on by a utility shut-off may also trigger childhood asthma, or result in a family’s decision to trade-off food for heat. Poor nutrition due to a wrongful denial of federal Supplemental Nutrition Assistance Program benefits may contribute to any number of deficiencies impacting a child’s health. Policies that directly address these issues include state and local laws requiring landlords to mitigate dangerous rental home conditions, state energy assistance programs that improve access to utilities for low-income individuals, and administrative appeals processes for inappropriate denials of state and federal food benefit programs to financially eligible recipients.
To help address these issues, the MLP model was developed in 1993 by innovators at the Boston Medical Center Department of Pediatrics and the Boston University School of Medicine. The model brings medical, legal and public health professionals together in the healthcare setting to: (1) provide direct legal advice and assistance to patients; (2) improve health care delivery by providing training and creating internal systems for identifying and managing patients’ health-harming legal needs; and (3) collectively promote policy change on a broad scale to improve the health and wellbeing of vulnerable populations (Tyler, Lawton, et al., 2011). In more concrete terms, MLP-affiliated clinicians are trained to identify health-harming legal needs in the exam room, which are then directly communicated to a legal partner via a structured referral system. Participating attorneys generally provide an initial consultation and then engage in full representation as needed to help ensure that the patients’ legal rights are appropriately enforced. The provision of legal care via MLP may be documented in a patient’s medical record with his or her consent, and patterns of unmet need within broader patient populations have been identified in this manner. In addition to informing internal quality improvement efforts, such patterns have also been used to advocate for policy change on a broader scale and secure institutional financing of MLP services (Tyler & Lawton, 2011).
On a national scale, the MLP movement is gaining momentum and attracting the attention of policy makers. The National Center for Medical Legal Partnership asserts that established MLPs in the United States address the needs of approximately 54,000 children, elders, veterans and patients with chronic illness per year thanks to the coordinated efforts of hundreds of hospitals, health centers and legal institutions (National Center for Medical Legal Partnership, 2014b). Resolutions in support of MLP have been passed by both the American Medical Association and the American Bar Association, among others, and preliminary evidence of its effectiveness is apparent in the published findings of several pilot studies. In a 2013 review of the literature, Beeson, McAllister & Regenstein (2013) highlighted the work of several small studies demonstrating the positive impact that MLPs had on the financial status of certain MLP partners and patients, the health and wellbeing of patients, and the knowledge and training of health care providers. Clear gaps in the literature exist, however, and now is an ideal time to evaluate the full potential of MLP on a large scale as the country focuses on health care financing and delivery pursuant to the Patient Protection and Affordable Care Act of 2010.
One powerful example of our nation’s willingness to consider novel interprofessional solutions to improve health care delivery is a recent report generated by the Robert Wood Johnson Foundation’s Commission to Build a Healthier America (2014). This report focused specifically on broadening the health care delivery model to include concepts that are decidedly reminiscent of the MLP model. Recommendation #3 of this report, for example, specifically calls the nation to “[b]roaden the mindset, mission, and incentives for health professionals and health care institutions beyond treating illness to helping people lead healthy lives” by expanding the healthcare team to include other helping professionals, adopting new health “vital signs” to assess non-medical determinants of health, creating incentives tied to reimbursement to address these determinants, and incorporating non-medical measures into community health needs assessments so that multidisciplinary solutions can be identified.
Doctors, Lawyers, Researchers and Patients Working Together to Build Innovation
Investigators
It is against this backdrop of a changing health care delivery zeitgeist that a group of multidisciplinary researchers at the Indiana University School of Medicine came together to design and study a system that automates the identification of health-harming legal needs in clinical primary health care settings and helps pediatricians mitigate adverse health outcomes using health information technology. Funding for this research project, entitled Computer-Supported Management of Medical Legal Issues Impacting Child Health, was awarded by the federal Agency for Healthcare Research and Quality in 2012.
The impetus for this effort was a conversation between two health services researchers from different disciplines and backgrounds about the emerging MLP model and its suitability for busy pediatric practices. Amy Lewis Gilbert, Assistant Professor of Pediatrics at the Indiana University School of Medicine, is an attorney and health services researcher with specific training in health law and public health, and a history of engagement with the MLP community on both a local and national scale. Pediatrician and health services researcher Stephen Downs, Professor of Pediatrics at the Indiana University School of Medicine and Director of the Department of Children’s Health Services Research, is a medical informatician and the originator of the Child Health Improvement through Computer Automation (CHICA) system. Their conversation focused on the reality that while pediatricians are ideally situated to identify medical legal issues, both because they generally receive some amount of professional training regarding non-medical determinants of health and because national guidelines dictate frequent well child visits in the first three years of life, they often don’t have the specific knowledge, resources or time required to systematically screen patients for such issues or effectively intervene when they do recognize them (Lawton, 2007). Moreover, pediatricians are faced with a dizzying array of guidelines and interventions that they are expected to address in one brief office visit (Belamarich, Gandica, et al., 2006). As a result, fewer than 50% of ambulatory services recommended for children are actually provided in the United States (Mangione-Smith, DeCristofaro, et al., 2007). Furthermore, pediatricians are rarely provided with guidance as to how such services should be prioritized, so they frequently make prioritization decisions based on previous experience alone.
In response to these issues, computerized clinical decision support systems have emerged as an effective way of empowering physicians to provide relevant and appropriate care in a variety of contexts. These systems help physicians identify and prioritize the most appropriate interventions for specific patients in a world in which the expanse of potential subject matter to be covered during an office visit, coupled with an absence of guidance regarding how best to approach it, often results in information overload (Hunt, Haynes & Hanna, 1998; Johnston, Langton, et al., 1994; Biondich, Downs, et al., 2005). Ideally, such systems automate the assessment of a child’s risks and help the physician prioritize interventions so as to maximize the benefit to the child without overburdening the system. The CHICA system, developed in 2004, was specifically designed to help support the appropriate and efficient implementation of multiple pediatric guidelines in busy primary care practices.
In the end, this multidisciplinary team of researchers at Indiana University decided to expand and modify the CHICA system to assist pediatricians with the identification and management of four common medical-legal problems. Their goal was to integrate support for MLP into the existing primary care system so that screening for, and responding to, unmet legal needs would become a routine part of primary care. Proposed evaluation measures for this randomized controlled study of the CHICA MLP intervention include changes in the rate of MLP issue identification, actions taken by caregivers and physicians to mitigate identified issues, caregiver and physician satisfaction with the CHICA MLP module and the downstream impact of the module on healthcare utilization. Pediatrician and data management expert Marc Rosenman, Associate Professor of Pediatrics and Director of the Health Data and Epidemiology Section at the Regenstrief Institute, Inc. was the final researcher to join the team for the purpose of assisting with the proposed healthcare utilization analysis. All analyses are on schedule to be completed and published at the end of the study period in 2015.
Advisory Panel
A critical component of the CHICA MLP project has been its advisory panel of multidisciplinary experts, a group convened to help design the module and address any clinical, legal or ethical issues that might arise. In addition to the investigators named previously, this group includes Dr. Barry Zuckerman, Chief of Pediatrics at Boston Medical Center and Founding Director of the National Center for Medical Legal Partnership; Dr. Suzanne Cashman, Professor of Family Medicine and Community Health at the University of Massachusetts Medical School, who previously helped develop and validate a well-known medical legal issue screening tool; attorney Anna Kirkman, Director of the Eskenazi Health Medical Legal Partnership, a local MLP that serves the project’s target population; and Dr. Deanna Reinoso, a pediatrician that delivers care in one of 5 primary care practices targeted by the project.
The value of designing the CHICA MLP module under the advisement of such a rich and varied group of professionals has been immeasurable. For example, at the prompting of national MLP expert Dr. Barry Zuckerman, the screening questions were refined to mirror new, recently validated tools in the field. These questions were further revised by the panel’s medical practitioners to be more clinically relevant, and its attorney members to reflect local law. Another proposal made by the panel was to incorporate emergency bypass algorithms (e.g., fast-track access to attorneys) for patients who indicate that they have received a recent notice of imminent eviction or unjustified denial of food program benefits, as the availability of legal remedies for these situations is highly time sensitive. One other suggestion generated by this group was the development of an electronic flagging strategy for patients who endorse medical legal issues, but are then lost to follow-up. Both the clinical and legal importance of prompting further action in such situations was discussed at length, and the quality of care delivered by the CHICA MLP module stands to benefit substantially from this modification.
Community Focus Groups
Recognizing the importance of community engagement in research design and implementation, the advisory panel also recommended convening at least one focus group of community members to help refine the screening tool and proposed intervention. In all, five families spent approximately one hour with investigators reviewing the specific wording and subject matter of all intervention-specific documents, and discussing the acceptability of the intervention in general. This process resulted in screening questions and patient handouts that were more culturally sensitive and understandable to the target population, and the development of additional resources that directly addressed focus group concerns about public benefit eligibility and implications for both documented and undocumented immigrant populations.
Promoting Interprofessional Practice with Health Information Technology
Although pediatricians are increasingly familiar with the MLP concept, few have successfully incorporated medical-legal issue screening, assessment, intervention and referral into their routine practice for the reasons articulated above. Previous studies of CHICA have shown that it is a powerful tool for integrating recommended care into clinical practice because it is both comprehensive and universally used, providing screening and management support to nearly all of the patients in the clinics that use it. So the team at Indiana University set out to build a new CHICA module that would integrate guidelines specific to social determinants of health by automating the identification and management of medical-legal issues (Carroll, Biondich, et al., 2011; Carroll, Anand, et al., 2012; Carroll, Bauer, et al., 2013), and implementing electronic processes to help facilitate interprofessional collaborative care.
The CHICA MLP Module
Part of what makes CHICA innovative is that it collects data directly from families in the waiting room using a tailored paper or electronic form, and then combines this information with individualized electronic medical record data to provide targeted decision support to physicians at the point of care. Unlike other systems that collect data directly from patients, CHICA selects which questions to ask from hundreds of options based on the patient’s history, age and a unique expected value prioritization scheme. (Downs & Uner, 2002) The system prioritizes patient responses to assure that the most important issues are highlighted in the physician guidance so he or she may address the most critical issues in the limited amount of time available. For example, if a patient caregiver were to endorse a domestic violence question on the PSF, the corresponding physician alert would have a higher priority than an MLP issue. However, an MLP issue would take priority over an infant sleep issue. Although a physician may not modify CHICA’s automated prioritization scheme, he or she has final discretion regarding which issues to address and may ultimately decide to focus on different issues entirely.
CHICA is currently used in 5 inner-city pediatric health centers affiliated with Eskenazi Health and the Indiana University School of Medicine, where it acts as a front end to the health centers’ electronic medical record system. When a family checks a pediatric patient into a participating clinic, the registration system sends a message to CHICA. In response to this trigger, CHICA queries the electronic medical record for all of the patient’s clinical data. Upon receipt and parsing of these data, CHICA generates a highly tailored paper or electronic (for use on tablet devices) Pre-screener Form (PSF). The top portion of the form, to be completed by the nursing staff, contains a structured template for recording height and weight measurements, vital signs and screening test results. The bottom portion includes 20 “Yes/No” health assessment questions that the system identifies as being the most important for the particular patient at the particular visit. All paper PSFs are printed in English on one side and Spanish on the other, and electronic versions allow users to toggle back and forth between languages. For the purpose of this project, screening questions assessing 4 health-harming medical-legal issues (pertaining to housing insecurity, substandard rental home conditions, energy/utility insecurity and food insecurity) were developed and implemented for all eligible patients ≤3 years of age. These questions are completed by families in the waiting room, and then scanned or uploaded to the CHICA system by clinical staff prior to the physician encounter.
Data derived from responses to the PSF are analyzed along with previously existing medical record data by the CHICA library of Arden Syntax rules to generate the content for a Physician Worksheet (PWS) (Downs, Biondich, et al., 2006). CHICA employs a global prioritization scheme (Downs & Uner, 2002) to restrict the printed content so as to appropriately limit the number of topics addressed in a single visit. Certain areas on the PWS are designated for a handwritten history, physical examination, impression and plan, and others provide CHICA-generated prompts with reminders. Each prompt on a PWS explains the reason for the prompt and recommends a course of action. This is followed by up to 6 check-box responses, which the physician may use to notate the results of an assessment made, treatment initiated or referral generated. Positive responses to the medical-legal issue screening questions on the PSF trigger physician prompts on the PWS that ask the pediatrician to confirm the existence of the medical-legal issue, and advise him or her about how to proceed if the issue is confirmed.
CHICA also produces Just-in-Time (JIT) handouts designed to support the physician’s counseling effort. These paper forms, which are tailored to the patient’s specific needs, are printed at the same time as the PWS. JITs are generally designed to provide additional physician guidance or take-home information for the patient’s family. Like the PSF, JITs are printed in English on one side and Spanish on the other. If medical-legal issues are identified on the PSF, CHICA generates JIT handouts tailored to the specific issues found. For example, if food insecurity is identified on the PSF, then a JIT including food benefit program information is generated. If the issue identified is a substandard rental property, then the JIT includes a detailed letter to the landlord specifying the landlord’s legal responsibility to mitigate the problem. In all cases, the pediatrician is directed (via the PWS) to advise the caregiver about actions that can be taken with the JITs provided (e.g., “you can get information about eligibility for food benefit programs by calling this number,” or “this letter should be delivered to your landlord within 48 hours”).
Once a physician completes a PWS form, he or she scans it back into the CHICA system, which then records the data (along with an electronic image of the form) into the electronic medical record system. If no medical-legal issues are confirmed by the physician on the PWS, the intervention for that visit is considered to be complete.
When a patient returns to the clinic after a medical-legal issue has been identified, the PSF form inquires as to whether the previously identified issued has been resolved. If the caregiver answers in the negative, and the issue pertains to unsafe rental property conditions, a legal referral JIT is printed out with detailed instructions for the physician to complete the form and fax it to the Director of the Eskenazi Health Medical Legal Partnership so a legal consultation may be arranged. In addition, a JIT describing the legal referral process and specifying the documentation required for the legal consultation is generated for the family. If the issue pertains to housing insecurity, energy/utility insecurity or food insecurity, a social work referral JIT is generated with detailed instructions for the physician to complete and deliver it to the co-located social worker for that clinic. In addition, JITs are generated for the family that again include information about available resources and, for Spanish-speakers, also provide “myths and facts” information about public benefits and immigration status. If the social worker determines that legal intervention is required (e.g., a food benefit application has been unlawfully denied), then a referral to the Eskenazi Health Medical Legal Partnership is made. At the following clinic visit, the PSF form again inquires whether the medical-legal issue has been resolved, and if it has not been resolved, the physician is prompted one last time to intervene.
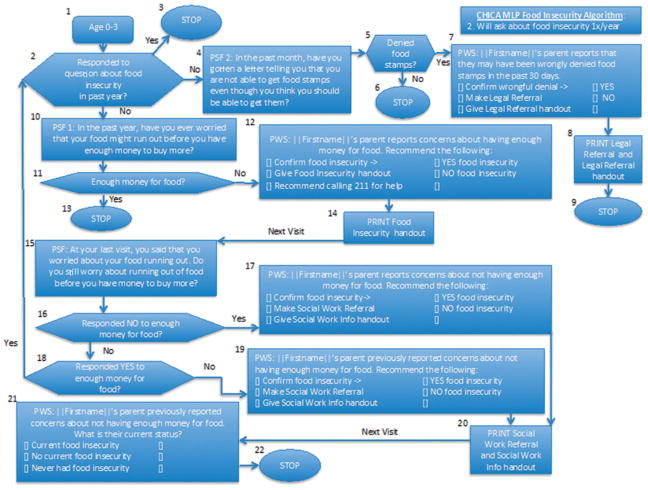
The first step in implementing a new module in CHICA is to develop a formal clinical algorithm (Society for Medical Decision Making Committee on Standardization of Clinical Algorithms, 1992). To follow the entire algorithm from initial PSF query regarding a single medical-legal issue to the conclusion of the intervention for that specific issue, see Figure 1. Of note, this algorithm includes an emergency bypass pathway that diverges from the normal intervention pathway in cases where the family reports on the PSF that they have received notice of denial of Supplemental Nutrition Assistance Program (SNAP) benefits in the past two weeks. The rationale behind this divergence is that the administrative window of opportunity for appealing a denial of food stamps is very limited, and a legal referral needs to be generated immediately so that an attorney can determine whether the facts of the case support an appeal.
Figure 1.
CHICA MLP food insecurity MDM algorithm.
CHICA Technical Description
CHICA has a modular architecture and is built upon the OpenMRS® (http://www.openmrs.org) system. OpenMRS® is a community-developed, open-source, enterprise electronic medical record framework for actively building and managing health systems. The OpenMRS® core data model and application programming interface (API) are extensible, and CHICA adds modules to support Adaptive Turnaround Document technology, Decision Support Services that use industry standard Arden Syntax decision rules, and the Health Level 7 standard for information exchange. CHICA 2.0 is implemented in Java and uses the OpenMRS® API to connect to the underlying data repository, which runs on the open source database engine, MySQL. The CHICA application runs as a web application under the open source Apache Tomcat servlet engine and is accessed via a Secure Socket Layer data exchange protocol.
To summarize the Arden Syntax and global prioritization processes described above, CHICA rules query the medical record and conclude with either a question for the family or an alert for the physician. Each rule in CHICA has an age range and a priority score. In order to produce a PSF, CHICA creates a list of all rules that include the patient’s age and orders it by priority. If the highest rule’s criteria are met, the question associated with that rule is added to the list. CHICA then moves on to the rule with the next highest priority. This process is repeated until 20 questions have been selected. The same approach is used to generate the six physician alerts on the PWS.
Conclusion
Interprofessional collaboration is essential to successful implementation of the MLP model of health care delivery, which seeks to improve the health and wellbeing of vulnerable populations by addressing unmet, health-harming legal needs and removing barriers that negatively impact access to care. Designing and testing a new MLP likewise requires the engaged participation of a multidisciplinary team of invested stakeholders, including physicians, lawyers, social workers, researchers or evaluators and other members of the community. In the case of the CHICA MLP, which has been developed to integrate social determinants of health guidelines into pediatric primary care by automating the identification and management of medical-legal issues via computerized clinical decision support, the participation of data managers and medical informaticians is also of critical importance. Outcomes from the Computer-Supported Management of Medical Legal Issues Impacting Child Health study will be available in 2015, and findings relative to the intervention’s impact on rates of identification of health-harming legal needs, actions taken by caregivers and physicians to mitigate identified MLP issues, caregiver and physician satisfaction with the CHICA MLP module and the downstream impact of the intervention on healthcare utilization will hopefully inspire other communities to broaden their understanding of effective health care delivery and welcome new professionals into the fold.
Acknowledgments
Funding Source: This work was supported by a grant from the Agency for Healthcare Research and Quality [R01HS020640].
Footnotes
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
Potential Conflicts of Interest: The authors have no conflicts of interest relevant to this article to disclose.
Declaration of Interest
The authors report that the research activities described in this manuscript are supported by the U.S. Department of Health and Human Services’ Agency for Healthcare Research and Quality, grant number R01HS020640.
References
- 1.American Bar Association. [Last accessed, January 30, 2014];Health Law Section Report to the House of Delegates #120A. 2007 http://www.americanbar.org/directories/policy.html.
- 2.American Medical Association. [Last accessed, January 30, 2014];AMA adopts new policies during final day of annual meeting. 2010 http://www.ama-assn.org/ama/pub/news/news/2010-new-policies.page.
- 3.Asch DA, Volpp KG. What business are we in? The emergence of health as the business of health care. N Engl J Med. 2012;367:888–889. doi: 10.1056/NEJMp1206862. [DOI] [PubMed] [Google Scholar]
- 4.Beeson T, McAllister BD, Regenstein M. Making the case for medical-legal partnerships: A review of the evidence. National Center for Medical Legal Partnership, George Washington University; 2013. [Last accessed, January 30, 2014]. http://legalaidresearch.files.wordpress.com/2013/04/medical-legal-partnership-literature-review-february-2013.pdf. [Google Scholar]
- 5.Belamarich PF, Gandica R, Stein RE, Racine AD. Drowning in a sea of advice: Pediatricians and American Academy of Pediatrics Policy Statements. Pediatrics. 2006;118:e964–e978. doi: 10.1542/peds.2006-0652. [DOI] [PubMed] [Google Scholar]
- 6.Biondich PG, Downs SM, Anand V, Carroll AE. Automating the recognition and prioritization of needed preventive services: Early results from the CHICA system. 2005 Annual Symposium Proceedings, American Medical Informatics Association Symposium; 2005. pp. 51–55. [PMC free article] [PubMed] [Google Scholar]
- 7.Braveman PA, Egerter SA, Mockenhaupt RE. Broadening the focus: The need to address the social determinants of health. Am J Prev Med. 2011;40(1S1):S4–S18. doi: 10.1016/j.amepre.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Carroll AE, Biondich PG, Anand V, Dugan TM, Sheley ME, Xu SZ. Targeted screening for pediatric conditions with the CHICA system. J Am Med Inform Assoc. 2011;18(4):485–490. doi: 10.1136/amiajnl-2011-000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carroll AE, Anand V, Dugan DM, Sheley ME, Xu SZ, Downs SM. Increased physician diagnosis of asthma with the Child Health Improvement through Computer Automation decision support system. Pediatr Allergy Immunol Pulmonol. 2012 Sep;:168–171. [Google Scholar]
- 10.Carroll AE, Bauer NS, Dugan TM, Anand V, Saha C, Downs SM. Use of a computerized decision aid for ADHD diagnosis: a randomized controlled trial. Pediatrics. 2013;132(3):e623–629. doi: 10.1542/peds.2013-0933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Downs SM, Uner H. Expected value prioritization of prompts and reminders. Proceedings/AMIA, 2002 Annual Symposium; 2002. pp. 215–219. [PMC free article] [PubMed] [Google Scholar]
- 12.Downs SM, Biondich PG, Anand V, et al. Using Arden Syntax and adaptive turnaround documents to evaluate clinical guidelines. AMIA, Annual Symposium Proceedings/AMIA Symposium; 2006. pp. 214–218. [PMC free article] [PubMed] [Google Scholar]
- 13.Hunt DL, Haynes RB, Hanna SE. Effects of computer-based clinical decision support systems on physician performance and patient outcomes: a systematic review. JAMA. 1998;280(15):1339–1346. doi: 10.1001/jama.280.15.1339. [DOI] [PubMed] [Google Scholar]
- 14.Johnston ME, Langton KB, Haynes RB, Mathieu A. Effects of computer-based clinical decision support systems on clinician performance and patient outcomes: a critical appraisal of research. Ann Intern Med. 1994;120(2):266–269. doi: 10.7326/0003-4819-120-2-199401150-00007. [DOI] [PubMed] [Google Scholar]
- 15.Lawton EM. Medical-legal partnerships: From surgery to prevention? Management Information Exchange Journal. 2007;(Spring Issue):37–42. 53. [Google Scholar]
- 16.Legal Services Corporation. Documenting the justice gap in America: The current unmet civil legal needs of low-income Americans. Washington, DC: The Corporation; 2009. [Last accessed, January 16, 2014]. http://www.lsc.gov/justicegap.pdf. [Google Scholar]
- 17.Mangione-Smith R, DeCristofaro AH, Setodji CM, Keesey J, Klein DJ, Adams JL, et al. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007;357:1515–1523. doi: 10.1056/NEJMsa064637. [DOI] [PubMed] [Google Scholar]
- 18.National Center for Medical Legal Partnership. [Last accessed, January 10, 2014];The model: 50 million people need legal care to be healthy. http://www.medical-legalpartnership.org/model.
- 19.National Center for Medical Legal Partnership. [Last accessed, January 16, 2014];The movement. http://www.medical-legalpartnership.org/movement.
- 20.Robert Wood Johnson Foundation Commission to Build a Healthier America. [Last accessed, January 30, 2014];Time to act: Investing in the health of our children and communities. 2014 http://www.rwjf.org/en/research-publications/find-rwjf-research/2014/01/recommendations-from-the-rwjf-commission-to-build-a-healthier-am.html.
- 21.Society for Medical Decision Making Committee on Standardization of Clinical Algorithms. Proposal for clinical algorithm standards. Medical Decision Making. 1992;12(2):149–154. [PubMed] [Google Scholar]
- 22.Tyler TB, Lawton E, Conroy K, Sandel M, Zuckerman B, editors. Poverty, health and law: Readings and cases for medical-legal partnership. Durham, NC: Carolina Academic Press; 2011. [Google Scholar]
- 23.U.S. Centers for Disease Control and Prevention. [Last accessed, January 15, 2014];Social Determinants of Health. http://www.cdc.gov/socialdeterminants/Index.html.
- 24.Williams DR, Costa MV, Odunlami AO, Mohammed SA. Moving upstream: How interventions that address the social determinants of health can improve health and reduce disparities. J Public Health Manag Pract. 2008;14(Suppl):S8–S17. doi: 10.1097/01.PHH.0000338382.36695.42. [DOI] [PMC free article] [PubMed] [Google Scholar]