Abstract
Purpose
This study aims to review the results of sclerotherapy using Surgiflo in addition to alcohol in primary aneurysmal bone cysts (ABC).
Methods
A total of 16 consecutive patients with histologically confirmed diagnosis of primary ABC were treated by percutaneous Surgiflo and alcohol injection at our institution. Clinical follow-up included the assessment of pain, swelling, limping and functional impairment. Radiological parameters included tumour volume, physis-cyst distance, thickness of cyst cortex, and presence of intracystic septations. Mean follow-up was 35,6 months (24–71 months). Treatment was considered successful when the cyst volume decreased by a minimum of 10%, the bone cortex became thicker, and the distance to physis increased.
Results
Mean age at presentation was 9.5 years (5.16–13.84 years). All ABC’s were primary and all patients underwent a single Surgiflo and alcohol session except for two (12.5%) who required a second session. All patients had a good clinical result at final follow-up. Satisfactory cyst healing was achieved in 11 cases according to radiological parameters. Tumour volume decreased from a mean of 122 cm3 (111 to 133) before injection to 86 cm3 (76 to 96) at last follow-up (p < 0.01). Physis-cyst distance increased from a mean of 1 cm (0.1 to 2) to 2.1 cm (0.5 to 4) at last follow-up (p < 0.01). Cortical thickness improved from 1 mm (0.5 to 1.5) to 2 mm (1 to 3.5) at last follow-up (p < 0.01).
There were no treatment related complications. Surgery was performed in one patient having a C3 vertebra ABC after developing quadriparesis due to tumour progression.
Conclusion
Sclerotherapy using Surgiflo and alcohol may be used as an efficient, safe and minimally invasive alternative for the treatment of primary ABCs.
Keywords: aneurysmal bone cyst, benign bone tumour, percutaneous treatment, Surgiflo, sclerotherapy
Introduction
Aneurysmal bone cyst (ABC) is a rare, rapidly growing, expansile and destructive tumour-like lesion, commonly occurring around the knee and in the humerus.1 It was first described as a distinct entity in 1942 by Jaffe and Lichtenstein.1,2,3 One theory holds that the ABC is a non-neoplastic reactive condition, which is aggressive in its ability to destroy and expand bone.3 Another theory confirms the neoplastic nature of this lesion with a recurrent translocation of the USP6 gene.4 In about 70% of cases, it arises as a primary tumour without any recognised precursor bone lesion. In the remaining 30% of cases, it arises as a secondary lesion when a preexisting osseous lesion can be identified such as giant cell tumour, chondroblastoma, chondromyxoid fibroma, fibrous dysplasia or even malignant tumour.5-7
ABC has been treated by several methods. Inactive lesions can simply be monitored without any treatment, whereas active or aggressive lesions are classically treated by surgery (curettage or excision).8 The position of the cyst, however, limits the indications: it is not always easy in long bones, when the tumour is juxtaposed to the growth plate.9,10 Surgery is also difficult in the pelvis when the lesion is not peripheral and hazardous in the spine.6,11 Surgical treatment for ABCs has primarily been intra-lesional curettage that can be supplemented with various adjuvants to achieve higher healing rates and reduce recurrences.1 Limitations with the use of surgical treatment have been hospitalisation, immobilisation of the part, intra-operative blood loss and the potential of physeal damage associated with curettage.1,9
A percutaneous intracystic Ethibloc (Ethicon, West Somerville, New Jersey) injection was introduced several years ago as an alternative less aggressive method to treat ABC.12 Evidence from the literature shows that sclerotherapy using Ethibloc is at least as effective as surgery in treatment of ABC in terms of healing rates, pain and complications, which made it an effective primary treatment of this condition.13 However, Topouchian et al14 showed a high rate of local complications and one case of pulmonary embolism caused by Ethibloc. Some fatalities were also reported.15 This led the authors to abandon this technique and thereafter led to withdrawal of the product from the pharmaceutical market.14
Surgiflo (Ethicon, New Brunswick, New Jersey) is a hemostatic matrix that is used to stop severe surgical bleeding especially in spine surgery.16 It has been used lately by interventional radiologists as a fibrosing agent for hemostatic purposes in the treatment of arteriovenous malformations of head and neck, to decrease bleeding during resection.16
Since there have been no major complications reported with its use, we extended its indications to the treatment of ABC.
The purpose of this study was to report the preliminary results of Surgiflo as a first line treatment of ABC.
Material and Methods
Between June 2008 and June 2013, 16 patients with radiological, MRI and histological diagnosis of active or aggressive primary ABC were treated by percutaneous Surgiflo injection at our institution.
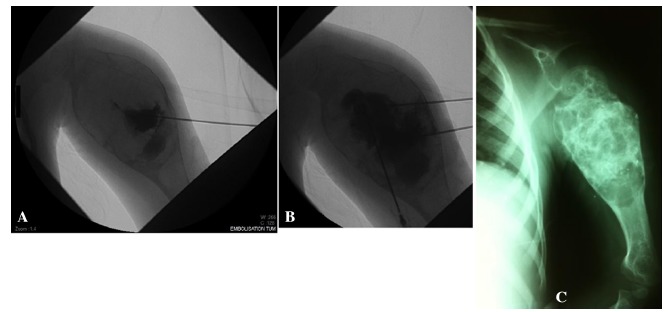
Surgiflo injection is performed under local, spinal or general anesthesia depending on the cyst location and the patient’s age. In radiologically aggressive ABCs previous open histological confirmation is obtained before the patient is scheduled for Surgiflo injection. In active lesions the procedure begins with percutaneous biopsy and culture under image guidance using a 12 Gauge to 16 Gauge biopsy needle. A frozen section is obtained for histology and is immediately followed by an intracystic contrast medium (lipiodol) injection with care taken to opacify all possible cyst cavities (cystography) (Fig. 1). Two, three or four needles were required in each case, depending on the size and the cavitation of the tumour. This is also useful to detect any possible major venous opacification that may contradict the use of Surgiflo. Next, using the syringes available in the Surgiflo kit, 6 mL of Surgiflo is mixed with 6 mL of extra pure ethanol and 2 mL of lipiodol. Then, the mixture is slowly injected with minimal pressure in all existing cavities, under fluoroscopic or CT guidance. Alcohol will improve Surgiflo’s fixation to the cyst walls in addition to its efficacy in ABC treatment. Furthermore, the elevated viscosity of Surgiflo will reduce the risk of alcohol leak into venous drainage and alcohol extravasation into surrounding tissues. Injection is discontinued when resistance is felt or in cases of major venous opacification or major leakage into the surrounding soft tissues. Each cyst is injected with around one-third of its volume. We did not have any cases of major venous opacification or major leakage into surrounding tissues. Following the procedure, the patients are given analgesics and/or non-steroidal anti-inflammatory drugs for a few days, to minimise pain and local inflammatory reaction that usually follows the injection. Patients were instructed to have 24 hours of restriction of physical activities and to get back to their normal activity thereafter.
Fig. 1. Aneurysmal bone cyst of the left proximal humerus (patient 4): (a) and (b) percutaneous cystography using many needles making sure all cavities are identified prior to Surgiflo administration; (c) radiograph one year following the procedure.
All patients were checked every six months clinically and radiologically. All pre- and post-injection radiographs were performed in the same radiology department and interpreted by the same radiologist. The mean follow-up was 35.6 months (24 to 71) except for one case of cervical spine ABC who developed quadriparesis three months following Surgiflo injection. Clinical follow-up included the assessment of pain, swelling, limping and functional impairment. Radiological parameters included overall tumour volume, distance between cyst and physis, thickness of cyst cortex and presence and density of intracystic septations. Tumour volume was measured using anteroposterior (AP) and lateral radiographs or CT scans and by multiplying maximum length, width and depth. Cortical thickness was defined as the thickness of the thinnest cortical bone surrounding the tumour whether on the AP, lateral or oblique radiograph. All images were interpreted by two independent observers (a radiologist (SS) and an orthopaedic surgeon (IG)) taking into account magnification and standard measurement error for digital radiographs. The observers were blinded to the dates on which the images were taken and to each other’s findings. The treatment was considered successful (in terms of cyst involution and lack of compromise of surrounding growth plate) when the following three parameters existed together: the cyst volume decreased by a minimum of 10%, the bone cortex became thicker and the distance to physis increased.
Student’s paired t-test was used for statistical analysis; it was used to study the success of treatment according to different parameters such as gender, tumour location, initial clinical presentation, previous treatment, number of sclerotherapy sessions, onset of complications and recurrence rate. A difference between the pre- and post-operative situation was considered significant for p-values < 0.05.
All patients were informed about the procedure, the potential outcomes and complications, and alternative treatments including surgical options as well as the natural history of the disease without treatment. Written informed consent was obtained before the inclusion of the patients in our study.
Results
Patient characteristics
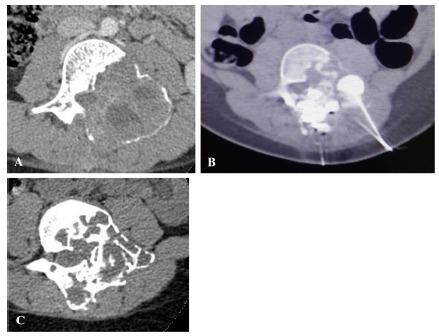
There were ten male (62.5%) and six female (37.5%) patients, with a mean age at presentation of 9.5 years (5.16 to 13.84). All ABCs were primary. The most common tumour location was the proximal humerus (six patients, 37.5%), followed by the tibia (three patients, 18.8%), femur (three patients, 18.8%), iliac bone (two patients, 12.5%), L3 vertebra (Fig. 2) (one patient, 6.25%) and the cervical spine (one patient, 6.25%). The most common clinical presentation was pain and swelling in eight patients (50%), followed by pathological fracture in six patients (37.5%) including one vertebral compression fracture of C3 with subsequent spinal cord compression. Two patients (12.5%) with lower limb ABCs presented with a painful limp. Half of the patients had already been treated either by curettage, internal fixation or embolisation a mean 10.4 months (9.2 to 11.5) prior to Surgiflo administration. The patients who underwent a previous treatment did not experience clinical improvement, with persistence of clinical and radiological symptoms and signs in six patients and recurrence in two patients (patients 7 and 15).
Fig. 2. Aneurysmal bone cyst of L3 (patient 6): (a) initial CT-scan before treatment; (b) percutaneous Surgiflo administration under CT guidance; (c) CT-scan 20 months following treatment shows increased septations. The patient is asymptomatic.
Number of required sessions
All patients underwent a single Surgiflo session except for two patients (12.5%) who had persistent symptoms following the first injection, therefore requiring a second session. The first patient was a two-year-old girl with persistent pain and swelling of the left proximal humerus. Radiographs showed cyst progression eight months after the first Surgiflo session. Therefore, this cyst required a second Surgiflo session. The patient showed clinical improvement after 12 months and radiographs show cortical thickening and cyst sclerosis. The second patient was a ten-year-old boy with an ABC that involved all of the right iliac bone. He underwent a second sclerotherapy session two years after the first session for mild inflammatory pain. At 36 months the patient is pain free and radiographs show regression of the cystic cavity and thickened bone cortex.
Clinical results at final follow-up
At final follow-up, all patients were pain free, with full range of movement in the affected limb, and no swelling or redness. None of them had any pathological fracture during the post-operative course till last follow-up. The only exception was a patient who developed quadriparesis (patient 14) three months after Surgiflo session; the neurological symptoms resulted from tumour progression and not from a direct complication from sclerotherapy. The patient was treated by posterior cervical decompression and fusion, with complete neurological recovery two months post-operatively. The patient was pain and symptom free at 26-month follow-up. Three other patients (patients 3, 9 and 12) experienced mild limb shortening without any negative impact on their daily life activities; all of them had a cyst that was touching the physis before any Surgiflo administration. Radiographic images of patients 3 and 12 at final follow-up showed intact physis, while those of patient 9 showed a partial damage of proximal humeral physis without any clinical or functional impact.
Table 1 summarises patients’ characteristics, number of sessions and clinical results at the last follow-up.
Table 1. Patient characteristics, number of sessions and clinical results at the last follow-up.
| Age (yrs)/gender | Site | Clinical presentation | Previous treatment | Follow-up (mths) | Clinical results | Further treatment | |
|---|---|---|---|---|---|---|---|
| 1 | 10/M | Proximal tibia | Pain | Cyst curettage + bone grafting | 32 | Successful | No |
| 2 | 8/M | Proximal humerus | Pathological fracture | Cyst curettage + bone grafting + osteosynthesis | 36 | Successful | No |
| 3 | 7/F | Proximal tibia | Accidental discovery | No remarks | 31 | Limb shortening | No |
| 4 | 2/F | Proximal humerus | Pathological fracture | Embolization | 29 | Successful | No |
| 5 | 19/M | Iliopubic ramus | Pain | No remarks | 44 | Successful | No |
| 6 | 10/F | L3 vertebra | Lumbar pain | Cyst curettage + osteosynthesis | 30 | Successful | No |
| 7 | 3/F | Proximal tibia | Painful limp | Cyst curettage + bone grafting | 52 | Successful | No |
| 8 | 13/M | Distal femur | Pain | No remarks | 34 | Successful | No |
| 9 | 5/F | Proximal humerus | Pathological fracture | No remarks | 34 | Limb shortening | No |
| 10 | 10/M | Iliac bone | Pain | No remarks | 71 | Successful | No |
| 11 | 10/M | Distal femur | Pain | Cyst curettage + bone grafting | 38 | Successful | No |
| 12 | 7/M | Proximal humerus | Pathological fracture | No remarks | 34 | Limb shortening | No |
| 13 | 4/M | Proximal humerus | Pathological fracture | No remarks | 27 | Successful | No |
| 14 | 13/M | C4 vertebra | Vertebral compression fracture | No remarks | 26 | Quadriparesis | Laminectomy + synthesis |
| 15 | 13/M | Proximal femur | Painful limp | Cyst curettage + bone grafting | 27 | Successful | No |
| 16 | 9/F | Humeral diaphysis | pain | Cyst curettage + bone grafting | 25 | Successful | No |
Radiologic characteristics at final follow-up
Tumour volume decreased from a mean of 122 cm3 (111 to 133) before injection to 86 cm3 (76 to 96) at final follow-up (p < 0.01). Physis-cyst distance increased from a mean of 1 cm (0.1 to 2) to 2.1 cm (0.5 to 4) at final follow-up (p < 0.01) (Fig. 3). Cortical thickness improved from a mean of 1 mm (0.5 to 1.5) to 2 mm (1 to 3.5) at final follow-up (p < 0.01). Intracystic septations were present in 12 cases (75%) at initial presentation, and in 15 cases (93.8%) at final follow-up (p =0. 55) (Fig. 4).
Fig. 3. (a) Aneurysmal bone cyst of proximal tibia (patient 1); (b) radiographs 3.5 years after injection shows complete ossification. Note the increase of the physis-cyst distance.
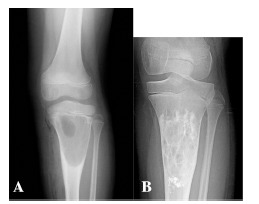
Fig. 4. (a) and (b) Aneurysmal bone cyst of proximal tibia immediately after Surgiflo injection (patient 7); (c) and (d) radiograph at 25 months showing partial ossification.

According to our radiological criteria, our results were considered successful in 11 patients (68.8%) after a minimum two-year follow-up.
Treatment success was not related to gender (p = 0.889), tumour location (p = 0.465), initial clinical presentation (p = 0.541), previous treatment (p = 0.59), number of sclerotherapy sessions (p = 0.541), onset of complications (p = 0.35) or recurrence rate (p = 0.126).
Discussion
Surgiflo is a hemostatic matrix used to stop severe surgical bleeding especially in spine surgery. Interventional radiologists have used it lately as a fibrosing agent for hemostatic purposes in the treatment of arteriovenous malformations of head and neck to decrease bleeding during resection.16 It has been shown to be a safe and effective alternative for the treatment of ABC. In the majority of cases, it halts tumour progression and decreases its size and the risk of pathological fracture.
Percutaneous injection of fibrosing agent was first proposed for the treatment of ABC by Adamsbaum et al in 1993.17 Fibrosis is induced by alcohol and/or an inflammatory foreign body reaction.
In 2003, Adamsbaum et al18 reported the results of 17 patients treated with sclerotherapy with Ethibloc, a fibrogenic and thrombogenic agent, as an alternative for more invasive procedures. In this study, 75% of the patients received one injection, all but one patient developed local and/or general inflammatory reactions a few days after treatment, and three patients had cutaneous fistulas at the site of injection with spontaneous resolution. Three patients had recurrence (18%), after a mean follow-up of five years; all were treated with surgical resection and bone grafting.18
Varshney et al 19 published a randomised study in 2010, in which they used polidocanol (Aetoxisclerol) for intracystic injection of ABC. They found that healing rates were similar comparing sclerotherapy with curettage and grafting, after a minimum of 3.2 years of follow-up, with lower rates of complications in the polidocanol group.19 A weak point of this study, however, was that the patients required repetitive injections to achieve the desired outcome with a mean of three injections per patient.19
In our series, only two patients (12.5%) had two injections of Surgiflo, the first was an iliac bone cyst that responded well to treatment, the second was an aggressive proximal humerus ABC with a less optimal response. This gives an advantage over sclerotherapy with polidicanol and makes the treatment with Surgiflo more cost-effective.
In their series, Adamsbaum et al18 reported a high rate of immediate post-operative inflammatory response, which required hospitalisation for a few days after the procedure. We had a smooth immediate post-operative follow-up in all patients, with minimal local and/or general inflammatory responses that required no increase in hospital stay; all our patients stayed up to 24 hours post-operatively.
In 2004, Topouchian et al14 reported their experience after sclerotherapy with Ethibloc; they had one case of pulmonary Ethibloc embolism that occurred after the third injection in a patient with iliac ABC who required a seven-day stay in the intensive care unit. They also reported four cases of cutaneous fistulisation (26%) at the injection site that required repetitive surgical debridement as well as curettage of the cyst and excision of any Ethibloc residues.14 This high complication rate led to Ethibloc withdrawal from the pharmaceutical market worldwide. In this preliminary study we did not encounter any major complications with Surgiflo, which makes it a safer sclerotherapy agent than Ethibloc to use for the minimally invasive treatment of ABC. We had one case of quadriparesis that was caused by tumour progression in the cervical spine, and it was treated by excision and posterior fusion with good neurological recovery with time. This complication is not caused by Surgiflo itself and may be related to the fact that fibrosing agents in general, including Surgiflo, freeze new bone formation during the first weeks following the injection, therefore allowing the weakened vertebra to collapse before osteogenesis becomes strong enough to improve mechanical strength.
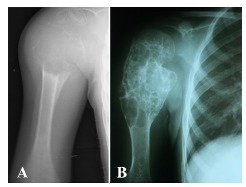
Tolerable limb shortening was found in three of 16 patients, in whom the cyst was touching the physis (Fig. 5). It is not clear whether this was due to Surgiflo, or if it was a complication of the cyst itself.
Fig 5. (a) Aggressive ABC of left proximal humerus (patient 9); (b) satisfactory ossification 2.5 years following Surgiflo administration with lateral spontaneous growth arrest.
Radiographic follow-up showed a success rate of 68.8%. Total cyst disappearance did not happen in any case following treatment even in cases with the longest follow-up, but all our patients were clinically asymptomatic and none of them have experienced any pathological fracture since the procedure. Success rates are comparable with those observed with surgical curettage alone (68%),5 and Ethibloc injections (82%),18 but with less surgical site morbidity and/or severe complications.
We have no exact idea about the pathogenesis of bone response to Surgiflo, since we did not undertake any histological studies on the cyst during the post-operative course of Surgiflo injection. However, we believe that it could be similar to that reported with Ethibloc.20
Conclusion
ABC is a benign locally aggressive tumour-like lesion which can be treated with open surgery or percutaneous sclerotherapy. Direct Surgiflo injection appears to be an effective and minimally invasive treatment of ABC with a low rate of major complications or surgical site morbidity. It can be recommended as an alternative to surgery and a first line treatment of ABCs.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Statement
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was not required for this work.
References
- 1.Mascard E, Gomez-Brouchet A, Lambot K.. Bone cysts: unicameral and aneurysmal bone cyst. Orthop Traumatol Surg Res 2015;101:S119-S127. [DOI] [PubMed] [Google Scholar]
- 2.Jaffe HL, Lichtenstein L.. Solitary unicameral bone cyst: with emphasis on the Roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg 1942;44:1004–1025. [Google Scholar]
- 3.Rădulescu R, Bădilă A, Manolescu R, Sajin M, Japie I.. Aneurysmal bone cyst--clinical and morphological aspects. Rom J Morphol Embryol 2014;55:977–981. [PubMed] [Google Scholar]
- 4.Oliveira AM, Chou MM, Perez-Atayde AR, Rosenberg AE.. Aneurysmal bone cyst: a neoplasm driven by upregulation of the USP6 oncogene. J Clin Oncol 2006;24:e1; author reply e2. [DOI] [PubMed] [Google Scholar]
- 5.Cottalorda J, Bourelle S.. Modern concepts of primary aneurysmal bone cyst. Arch Orthop Trauma Surg 2007;127:105–114. [DOI] [PubMed] [Google Scholar]
- 6.Zileli M, Isik HS, Ogut FE, et al. Aneurysmal bone cysts of the spine. Eur Spine J 2013;22:593–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leithner A, Windhager R, Lang S, et al.. Aneurysmal bone cyst. A population based epidemiologic study and literature review. Clin Orthop Relat Res 1999;363:176–179. [PubMed] [Google Scholar]
- 8.Cottalorda J, Bourelle S.. Current treatments of primary aneurysmal bone cysts. J Pediatr Orthop B 2006;15:155–167. [DOI] [PubMed] [Google Scholar]
- 9.Tsagozis P, Brosjö O.. Current strategies for the treatment of aneurysmal bone cysts. Orthop Rev (Pavia) 2015;7:6182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN.. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag 2014;10:937–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bollini G, Jouve JL, Cottalorda J, et al.. Aneurysmal bone cyst in children: analysis of twenty-seven patients. J Pediatr Orthop B 1998;7:274–285. [DOI] [PubMed] [Google Scholar]
- 12.de Gauzy JS, Abid A, Accadbled F, et al.. Percutaneous Ethibloc injection in the treatment of primary aneurysmal bone cysts. J Pediatr Orthop B 2005;14:367–370. [DOI] [PubMed] [Google Scholar]
- 13.Rapp TB, Ward JP, Alaia MJ.. Aneurysmal bone cyst. J Am Acad Orthop Surg 2012;20:233–241. [DOI] [PubMed] [Google Scholar]
- 14.Topouchian V, Mazda K, Hamze B, Laredo J-D, Penneçot G-F.. Aneurysmal bone cysts in children: complications of fibrosing agent injection. Radiology 2004;232:522–526. [DOI] [PubMed] [Google Scholar]
- 15.Peraud A, Drake JM, Armstrong D, et al.. Fatal ethibloc embolization of vertebrobasilar system following percutaneous injection into aneurysmal bone cyst of the second cervical vertebra. AJNR Am J Neuroradiol 2004;25:1116–1120. [PMC free article] [PubMed] [Google Scholar]
- 16.Karim AB, Lindsey S, Bovino B, Berenstein A.. Oral surgical procedures performed safely in patients with head and neck arteriovenous malformations: a retrospective case series of 12 patients. J Oral Maxillofac Surg 2016;74:255.e1-255.e8. [DOI] [PubMed] [Google Scholar]
- 17.Adamsbaum C, Kalifa G, Seringe R, Dubousset J.. Direct Ethibloc injection in benign bone cysts: preliminary report on four patients. Skeletal Radiol 1993;22:317–320. [DOI] [PubMed] [Google Scholar]
- 18.Adamsbaum C, Mascard E, Guinebretière JM, Kalifa G, Dubousset J.. Intralesional Ethibloc injections in primary aneurysmal bone cysts: an efficient and safe treatment. Skeletal Radiol 2003;32:559–566. [DOI] [PubMed] [Google Scholar]
- 19.Varshney MK, Rastogi S, Khan SA, Trikha V.. Is sclerotherapy better than intralesional excision for treating aneurysmal bone cysts? Clin Orthop Relat Res 2010;468:1649–1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.George HL, Unnikrishnan PN, Garg NK, et al.. Long-term follow-up of Ethibloc injection in aneurysmal bone cysts. J Pediatr Orthop B 2009;18:375–380. [DOI] [PubMed] [Google Scholar]


