Abstract
Purpose
The purpose of this study is to evaluate a surgical technique that aims to address the multi-planar deformities occurring in early onset Blount’s disease.
Methods
Seven patients (eight lower limbs) with early onset Blount’s disease were treated with a surgical technique that used an external fixator to simultaneously address all aspects of deformity. Presenting radiographic parameters including mechanical axis deviation (MAD), lateral distal femoral angle (LDFA), medial proximal tibial angle (MPTA) and medial plateau angle (MPA) were compared with final follow-up and the unaffected limb. Data was also collected on surgical complications and functional outcomes.
Results
After a mean interval of 4.6 years (2.2 to 9), the MAD of the affected limb improved from 4.85 cm to 1.88 cm, MPTA from 43.58° to 75.46° and MPA from 43.41° to 20.71°. The mean time in the external fixator was 5.6 months (3.5 to 10.4). Recurrence was noted in three patients; two had evidence of nerve injury and one patient had premature fibular consolidation.
Conclusion
The surgical technique described in this study has attempted to address the complex multiaxial deformity that is encountered in Blount’s disease. It identifies difficulties and limitations in developing a comprehensive surgical protocol and highlights complications associated with this approach.
Keywords: Blount’s disease, surgery, correction, definitive
Introduction
Tibia vara is a developmental condition characterised by disordered endochondral ossification of the medial part of the proximal tibial physis.1 The eponymous condition, described by Blount in 1937,2 implies only a frontal plane deformity. Authors have since noted multi-planar abnormalities consisting of tibia vara, procurvatum and internal rotation.1,3–5 These changes may lead to progressive limb-length discrepancies, gait abnormalities and premature osteoarthritis.6–8
The aim of treatment is to achieve early correction with conventional osteotomies, stabilised with a plate, Kirschner wires or plaster cast.9–11 In neglected or recurrent disease in older children, this approach is inadequate and a more complex method of deformity correction is required. This involves simultaneous tibial plateau elevation, correction of tibial metaphyseal deformity, lengthening and fibular epiphysiodesis.12–14 The aim of this report is to assess the application of this technique, and to identify and discuss its limitations and complications.
Patients and methods
Patient selection
Seven patients (eight limbs) with early onset Blount’s disease were managed between 2005 and 2010 in the Bristol Royal Hospital for Children. Medical records were interrogated to determine patient demographics, operative details, complications and functional outcomes. Radiographs were evaluated to determine the accuracy of correction using standard metrics.
Standard anterioposterior (AP) long leg radiographs were used to calculate the mechanical axis deviation (MAD), lateral distal femoral angle (LDFA), medial proximal tibial angle (MPTA) and medial plateau angle (MPA). Radiological data was extracted and compared from pre-operative radiographs and those done at most recent follow-up.
Surgical technique
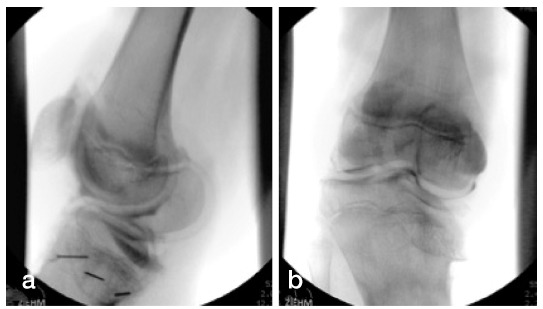
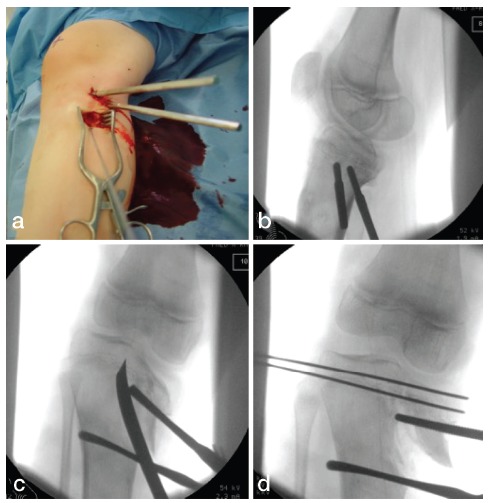
Clinical assessment and plain radiographs (AP, lateral and standing long leg alignment views) were obtained and used to determine the individual deformity characteristics (Fig. 1). Knee arthrography was initially performed to identify the orientation of the joint line in two planes and estimate the 3D deformity (Fig. 2).
Fig 1. Standing long leg alignment radiograph of child with left sided Blount’s disease (a) and post-operative radiograph (b).

Fig 2. Knee arthrogram to demonstrate posterior slope (a) and pathological varus joint line (b).
A proximal medial approach was used to conduct an osteotomy of the medial tibial plateau using a curved osteotome. The medial tibial plateau was elevated with a laminar spreader to reconstruct the joint line. The arthrogram demonstrated the extent of the cartilaginous anlage and the extent of elevation to produce a parallel joint line (Fig. 3).
Fig 3. Medial approach to proximal tibia (a,b); osteotomy performed with curved osteotome (c); acute hemi-plateau elevation initially stabilised with K-wires (d).
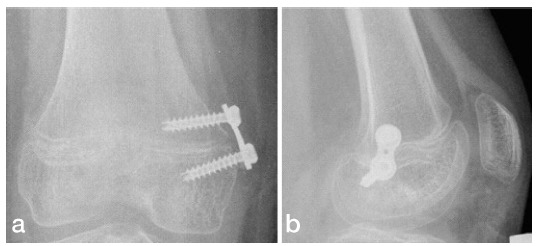
A proximal fixator ring was used to maintain the corrected joint line, initially with two 6 mm half pins, with a third pin inserted to stabilise the proximal segment. A low energy tibial metaphyseal osteotomy was then performed with multiple drill holes and osteotome using the same incision. A proximal third, fibular osteotomy was performed using a separate incision, with a sub-periosteal approach protecting the superficial peroneal nerve. The distal segment was stabilised with three 6 mm half pins and a distal fixator ring was applied (Fig. 4). A hexapod external fixator (Taylor Spatial Frame (TSF); Smith & Nephew, Memphis, Tennessee) was used to simultaneously correct alignment, rotation and length. In five cases, distal femoral valgus deformity was present and was addressed with a medial hemi-epiphyseal staple (8 Plate; Orthofix, Verona, Italy) (Fig. 5).
Fig 4. Definitive stabilisation of hemi-plateau with half pins (a); low energy tibial and fibular osteotomy (b).
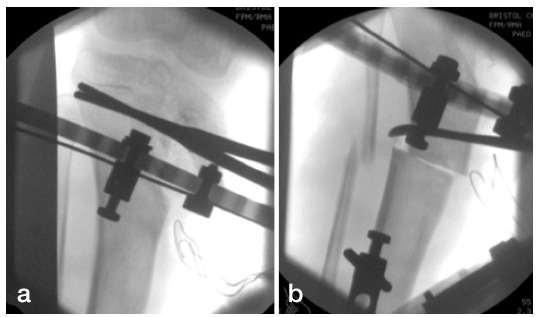
Fig 5. Anterioposterior (a) and lateral (b) radiographs of a right femur following insertion of 8 Plate staple. The posterior placement of the lateral staple is a technical error, but did not lead to clinical or radiological evidence of sagittal malalignment.
Results
Patient demographics
Seven patients were investigated with a mean follow-up period of 4.6 years (2.2 to 9.0). All were classified as Langenskiold stage VI.15 The average age at surgery was 9.5 years (6.6 to 10.6) and the average weight at the time of surgery was 45.5 kg (36 to 64). The mean time in external fixator was 5.6 months (3.5 to 10.4) (Table 1).
Table 1. Patient demographics.
| Patient | Affected limb | Gender | Age at surgery (yrs) | Weight at surgery (kg) | Langenskiold Classification | Follow-up (yrs) |
|---|---|---|---|---|---|---|
| 1 | Right | Female | 6.6 | 40.5 | VI | 9.0 |
| 2 | Right | Female | 10.5 | 36.0 | VI | 3.6 |
| 3 | Left | Female | 9.6 | 37.0 | VI | 4.6 |
| 4 | Left | Female | 9.4 | 64.0 | VI | 2.2 |
| 5 | Left | Male | 10.5 | 52.0 | VI | 5.0 |
| 6* | Right | Female | 10.4 | 36.0 | VI | 4.8 |
| 6* | Left | Female | 10.6 | 48.8 | VI | 4.6 |
| 7 | Left | Female | 8.3 | 49.4 | VI | 2.9 |
patient 6 had bilateral involvement
Deformity characteristics
Following the acute hemi-plateau elevation, the mean pre-operative MPA of 43.41° (24.00° to 56.80°; mean normal limb: 23.46°) was corrected to a mean of 20.71° (4.18° to 37.20°) at most recent review. The mean pre-operative MAD of the affected limbs was 4.85 cm (0.47 cm to 7.95 cm; mean normal limb: 0.5 mm) corrected to a mean 1.88 cm (0.00 cm to 4.55 cm) at most recent review. The mean pre-operative MPTA of the affected limbs was 43.58° (29.90° to 76.95°; mean normal limb: 77.08°) corrected to a mean 75.46° (67.50° to 81.90°) at most recent review. The mean pre-operative LDFA of the five affected limbs was 78.66° (75.75° to 84.50°; mean normal limb: 80.17°) corrected to a mean 82.01° (78.50° to 90.15°) at most recent review (Table 2).
Table 2. Normal, pre- and post-operative radiographic parameters.
| Patient | Parameter | Normal | Pre-operative | Post-operative |
|---|---|---|---|---|
| 1 | MAD (cm) | 0.32 | 5.21 | 4.55 |
| LDFA (°) | 81.25 | 84.50 | 90.15 | |
| MPTA (°) | 78.00 | 55.70 | 77.65 | |
| MPA (°) | 26.60 | 36.85 | 21.90 | |
| 2 | MAD (cm) | 0.14 | 0.47 | 0.40 |
| LDFA (°) | 81.10 | 79.10 | 80.05 | |
| MPTA (°) | 75.30 | 76.95 | 74.15 | |
| MPA (°) | 23.90 | 24.00 | 26.00 | |
| 3 | MAD (cm) | 0.56 | 7.95 | 0.55 |
| LDFA (°) | 80.70 | 77.50* | 82.25* | |
| MPTA (°) | 75.65 | 31.00 | 72.50 | |
| MPA (°) | 24.30 | 44.95 | 29.10 | |
| 4 | MAD (cm) | -2.67 | 7.01 | 0.00 |
| LDFA (°) | 77.75 | 75.75* | 78.50* | |
| MPTA (°) | 73.35 | 33.85 | 81.90 | |
| MPA (°) | 21.95 | 40.20 | 22.10 | |
| 5 | MAD (cm) | 0.16 | 3.15 | 3.51 |
| LDFA (°) | 79.55 | 78.50 | 79.75 | |
| MPTA (°) | 80.85 | 53.00 | 67.50 | |
| MPA (°) | 16.70 | 35.60 | 17.45 | |
| 6 (R) | MAD (cm) | n/a | 4.94 | 1.64 |
| LDFA (°) | n/a | 78.90* | 80.85* | |
| MPTA (°) | n/a | 33.10 | 77.00 | |
| MPA (°) | n/a | 52.85 | 4.18 | |
| 6 (L) | MAD (cm) | n/a | 4.15 | 3.13 |
| LDFA (°) | n/a | 83.65* | 82.80* | |
| MPTA (°) | n/a | 35.15 | 78.00 | |
| MPA (°) | n/a | 56.80 | 7.78 | |
| 7 | MAD (cm) | 1.18 | 5.94 | 1.27 |
| LDFA (°) | 82.05 | 77.50* | 85.65* | |
| MPTA (°) | 79.35 | 29.90 | 75.00 | |
| MPA (°) | 27.30 | 56.00 | 37.20 | |
| Mean | MAD (cm) | -0.05 | 4.85 | 1.88 |
| LDFA (°) | 80.40 | 79.43 | 82.50 | |
| MPTA (°) | 77.08 | 43.58 | 75.46 | |
| MPA (°) | 23.46 | 43.41 | 20.71 |
received distal femoral 8 Plate staple
MAD, mechanical axis deviation; LDFA, lateral distal femoral angle; MPTA, medial proximal tibial angle; MPA, medial plateau angle
Surgical complications
The operative technique was generally well tolerated. Table 3 details the complications and functional outcomes of each patient. Pin site infection occurred in four patients and three resolved with a single course of oral antibiotics. One patient developed recurrent infections and required a protracted course of oral antibiotics. One patient developed temporary paraesthesia over the anterior aspect of the proximal tibia. One patient developed a complete left peroneal nerve palsy, with complete recovery after 15 months. Premature consolidation of the fibular osteotomy was seen in one patient, one month after initial surgery. This required a course of physiotherapy and had recovered at most recent review.
Table 3. Clinical and functional outcomes following surgery.
| Patient | Time in frame (mths) | Infection | Nerve injury | RoM | Premature consolidation | Recurrence | Functional outcome |
|---|---|---|---|---|---|---|---|
| 1 | 3.5 | Pin site | No | Full | No | TSF reapplied twice | No deficit |
| 2 | 3.7 | Pin site | No | Full | No | No | No deficit |
| 3 | 5.7 | Pin site | No | Full | No | No | Playing sports |
| 4 | 7.1 | Pin site | Paraesthesia proximal tibia | Full | No | No | No deficit |
| 5 | 4.6 | No | No | Full | Premature fibular consolidation | No | Playing rugby and badminton |
| 6 (R) | 4.4 | No | No | Full | No | Tibia and fibula epiphysiodesis | No deficit |
| 6 (L) | 5.1 | No | Peroneal palsy | Full | No | Tibia and fibula epiphysiodesis. TSF reapplied | No deficit |
| 7 | 10.4 | No | No | Full | No | No | Occasionally uses crutches |
RoM, range of movement; TSF, Taylor Spatial Frame
Recurrence
Two patients (three limbs) developed recurrence of the original deformity. Patient 1 had persistent torsional asymmetry and required correction two years after the initial surgery with re-application of a hexapod external fixator for four months. This was due to failing to appreciate the extent of the pre-existing deformity and represents an error of pre-operative surgical planning. A further noticeable abnormality required the use of the TSF five years later, but this patient has since been stable.
Patient 6 required bilateral tibial and fibular epiphysiodesis two years after initial surgery. There was recurrence of the varus deformity in the left knee nine months after epiphysiodesis which was corrected with five months in a TSF.
One patient occasionally uses crutches to ease the pain in her left knee, the other six are enjoying various sporting activities without limitation. At most recent follow up, all patients had regained a full range of knee movement (Table 3).
Discussion
Recent studies have investigated individual aspects of the surgical management of Blount’s disease including closing wedge tibial osteotomies,16 fibular osteotomy,17 hemi-epiphyseal stapling18 and different types of external fixators.19 This study aimed to provide an evaluation of a technique required to simultaneously address all components of early onset Blount’s disease.
The classical radiographic changes seen in Blount’s disease are well known.1,5,20–22 However, plain radiographs have the potential to overestimate the apparent depression of the medial plateau.23,24 The proposed technique advocates the use of an intra-operative arthrogram which is useful in delineating the articular surface and provides information in two planes. The arthrography is performed as a precursor to the procedure under the same anaesthetic and provides information on the geometry of the articular correction.
The medial tibial plateau elevation is performed acutely and there is ongoing debate on the relative merits of iliac crest graft or gradual correction as an alternative. A prospective randomised clinical trial by Zorzi et al25 compared high tibial opening-wedge osteotomies with and without autologous iliac crest bone grafts. Blinded investigators concluded that all osteotomies had achieved bone union and that the difference in time to union was not statistically significant. The potential complications of bone grafting include infection, pain and failure.26,27 As patients requiring high degrees of correction often yield less than adequate bone,28 this method is not advocated.
Gradual correction has been reported to be a reliable and safe method of treating multi-planar deformities.29,30 Following a percutaneous osteotomy with progressive opening wedge correction using a modified Wagner monolateral fixator in ten patients (20 tibias) with late-onset Blount’s disease, de Pablos et al29 noted, apart from one case of under-correction, no major complications. Similar results were noted when Coogan et al30 reviewed their use of a circular external fixator in eight obese adolescents (12 tibias) undergoing gradual correction. A single case of premature consolidation was noted and this required a repeat osteotomy. The low incidence of neurovascular injury is likely to be due to the avoidance of acute intra-operative traction on the neurovascular structures.
Acute correction in Blount’s disease can be accomplished with a proximal tibial metaphyseal osteotomy.1 A variety of techniques have been suggested, including closing wedge,14 serrated,31 inclined,32 dome33 and as was done in this study, an opening wedge osteotomy34 (Fig. 3). We have used an acute opening wedge osteotomy without grafting and have observed uncomplicated union in all cases. Occasionally, like in Figure 3, this produced a medial metaphyseal prominence. This was not resected and it remodelled with time and did not produce a clinical or cosmetic abnormality.
Alternative methods of stabilisation have been reported and include smooth pins and wires,35 cast immobilisation,35 plates and screws,34 inter-fragmentary screws32 and external fixators (Fig. 4).36–38 Chotigavanichaya et al39 conducted a retrospective review of osteotomies performed for late-onset Blount’s disease. Of these, 34 were cross-pinned while 14 were held with an external fixator. At six years follow-up, the recurrence of varus deformity was 94% in those who were pinned and 72% in those with an external fixator. Following external fixator use in this study, three of eight (37.5%) limbs had recurrence after initial complete correction. This is due to the effect of residual growth in the proximal tibial physis and the procedure has been modified to include formal drill epiphysiodesis at the time of fixator removal. An alternative approach would involve physeal ablation at the time of initial surgery, but this would potentially compromise the stability and viability of the epimetaphyseal fragment and is considered unwise, from a theoretical perspective alone.
Regardless of the type of osteotomy and fixation device, there is a potential for serious adverse effects including compartment syndrome and focal neurological injury.40,35-37 In this report, one patient had mild paraesthesia lasting weeks, while one patient had a long episode of sensory and motor deficit of the peroneal nerve. A retrospective review of 116 children with 129 tibial osteotomies performed by Payman et al41 noted 35 cases of delayed union, two cases with transient peroneal nerve palsy, one case of nonunion and one case of malunion. More recently, Wilson et al42 reported a complication rate of 153% following 38 high tibial osteotomies with external fixation in patients with Blount’s disease; both studies highlighted Blount’s disease and obesity as factors increasing the complication rate.
The peroneal nerve is at risk at the time of fibular osteotomy and our recommendation is to perform the osteotomy through an incision that permits sub-periosteal exposure and osteotomy under direct vision. Paradoxically, this may increase the risk of neurapraxia due to a traction injury as seen in transient sensory loss in one patient. The site of the proximal fibular osteotomy is determined by the geometry of the tibial deformity and whilst a more distal division would be less likely to injure the peroneal nerve, it would produce a secondary fibular deformity that is frequently associated with local soft-tissue irritation. The fact that the complete peroneal nerve injury recovered without intervention indicates that this was also a traction injury, most likely at the time of fibular osteotomy.
Application of the TSF and a metaphyseal osteotomy allows six-axis deformity correction guided by a computer-generated schedule. Following TSF use in 14 obese children, Li et al43 noted an improved MAD from 90 mm to 10 mm 14 months post-application, a more pronounced improvement than the 30 mm seen in this study. Feldman et al44 noted 21 of 22 tibias being corrected to within 3° of normal. This is comparable with the average MPTA improvement in this study from 44° to 75°, with the average normal limb being 77°. The complications of TSF use include pin site infections,44 strut disengagement43 and in this series, one case of recurrent pin site infection and three transient superficial infections.
The purpose of this description is to demonstrate proof of principle and that failure of full correction is in part due to the simultaneous correction of all components. A retrospective review of 208 leg deformities corrected with either the TSF or Ilizarov ring was done by Manner et al45 In complex multidirectional deformities with four dimensions, correction was achieved in only 66.7% of patients following TSF use. The study demonstrates the difficulty in achieving full anatomical reconstruction in complex deformity and this is a shortcoming of this approach. There was, however, a useful improvement in alignment evidenced by the level of final function in the majority at most recent follow-up. Patient 7 had a poor outcome and it is important to highlight this in a candid manner. She occasionally uses crutches to ease hip and knee pain. Subsequent MRI scans have demonstrated no structural cause for her symptoms and she in engaging in a weight reduction programme and participating in swimming and field sports. The deformity is complex, and the potential for failure and the need for further procedures should be carefully discussed as part of the consenting process.
In this series, five patients required a distal femoral 8 Plate staple to address distal valgus deformity; this is a simple addition to the procedure and is recommended in cases with asymmetry of LDFA demonstrated in pre-operative standing alignment radiographs. The degree of deformity that mandates correction is controversial, and a pragmatic approach used in this series was to correct deformity > 5°. Castañeda et al46 conducted a retrospective case series studying hemiepiphysiodesis for correction of angular deformities about the knee caused by a variety of diseases. They noted an improvement of 3° in the patients with Blount’s disease, similar to the LDFA improvement seen in the five femurs that underwent stapling in this study. Disappointing results were seen in 2012 by Oto et al47 when tibial epiphysiodesis was used alone; the authors did not recommend this technique, highlighting the need for an all-inclusive surgical method.
Conclusion
Overall, the technique discussed is an effective way of improving the multi-dimensional deformity associated with early onset Blount’s disease. We have attempted to highlight the limitations of this surgical approach. Good functional outcomes and improved radiological measurements are produced in the majority but a significant incidence of recurrence and neurological complications have required further modifications of the surgical technique.
Compliance with Ethical Standards
Funding Statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Ethical Statement
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.Sabharwal S. Blount disease. J Bone Joint Surg [Am] 2009;91-A:1758-1776. [DOI] [PubMed] [Google Scholar]
- 2.Blount WP., vara Tibia. Osteochondrosis deformans tibiae. J Bone Joint Surg [Am] 1937;19-A:1-29. [Google Scholar]
- 3.Golding JSR, McNeil-Smith JDG. Observations on the etiology of tibia vara. J Bone Joint Surg [Br] 1963;45-B:320-325. [Google Scholar]
- 4.Sabharwal S, Lee J Jr, Zhao C.. Multiplanar deformity analysis of untreated Blount disease. J Pediatr Orthop 2007;27:260-265. [DOI] [PubMed] [Google Scholar]
- 5.Siffert RS, Katz JF.. The intra-articular deformity in osteochondrosis deformans tibiae. J Bone Joint Surg [Am] 1970;52-A:800-804. [PubMed] [Google Scholar]
- 6.Hofmann A, Jones RE, Herring JA.. Blount’s disease after skeletal maturity. J Bone Joint Surg [Am] 1982;64-A:1004-1009. [PubMed] [Google Scholar]
- 7.Ingvarsson T, Hägglund G, Ramgren B, Jonsson K, Zayer M.. Long-term results after adolescent Blount’s disease. J Pediatr Orthop B. 1997;6:153-156. [DOI] [PubMed] [Google Scholar]
- 8.Zayer M. Osteoarthritis following Blount’s disease. Int Orthop 1980;4:63-66. [DOI] [PubMed] [Google Scholar]
- 9.Doyle BS, Volk AG, Smith CF.. Infantile Blount disease: long-term follow-up of surgically treated patients at skeletal maturity. J Pediatr Orthop 1996;16:469-476. [DOI] [PubMed] [Google Scholar]
- 10.Ferriter P, Shapiro F.. Infantile tibia vara: factors affecting outcome following proximal tibial osteotomy. J Pediatr Orthop 1987;7:1-7. [PubMed] [Google Scholar]
- 11.Loder RT, Johnston CE II. Infantile tibia vara. J Pediatr Orthop 1987;7:639-646. [PubMed] [Google Scholar]
- 12.Accadbled F, Laville JM, Harper L.. One-step treatment for evolved Blount’s disease: four cases and review of the literature. J Pediatr Orthop 2003;23:747-752. [PubMed] [Google Scholar]
- 13.Bar-On E, Weigl DM, Becker T, Katz K.. Treatment of severe early onset Blount’s disease by an intra-articular and a metaphyseal osteotomy using the Taylor Spatial Frame. J Child Orthop 2008;2:457-461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schoenecker PL, Johnston R, Rich MM, Capelli AM.. Elevation of the medical plateau of the tibia in the treatment of Blount disease. J Bone Joint Surg [Am] 1992;74-A:351-358. [PubMed] [Google Scholar]
- 15.Langenskiöld A. Tibia vara. A critical review. Clin Orthop Relat Res 1989;195-207. [PubMed] [Google Scholar]
- 16.Burton A, Hennrikus W.. Complete closing wedge osteotomy for correction of blount disease (tibia vara): A Technique. Am J Orthop 2016;45:16-18. [PubMed] [Google Scholar]
- 17.Sachs O, Katzman A, Abu-Johar E, Eidelman M.. Treatment of adolescent Blount disease using Taylor Spatial Frame with and without fibular osteotomy: Is there any difference? J Pediatr Orthop 2015;35:501-506. [DOI] [PubMed] [Google Scholar]
- 18.Schroerlucke S, Bertrand S, Clapp J, Bundy J, Gregg FO.. Failure of Orthofix eight-Plate for the treatment of Blount disease. J Pediatr Orthop 2009;29:57-60. [DOI] [PubMed] [Google Scholar]
- 19.Mayer SW, Hubbard EW, Sun D, Lark RK, Fitch RD.. Gradual Deformity Correction in Blount Disease. J Pediatr Orthop 2016;December 23; Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 20.Thompson GH, Carter JR.. Late-onset tibia vara (Blount’s disease). Current concepts. Clin Orthop Relat Res 1990;255:24-35. [PubMed] [Google Scholar]
- 21.Sabharwal S, Zhao C, McClemens E.. Correlation of body mass index and radiographic deformities in children with Blount disease. J Bone Joint Surg [Am] 2007;89-A:1275-1283. [DOI] [PubMed] [Google Scholar]
- 22.Johnston CE., II Infantile tibia vara. Clin Orthop Relat Res 1990;255:13-23. [PubMed] [Google Scholar]
- 23.Craig JG, van Holsbeeck M, Zaltz I.. The utility of MR in assessing Blount disease. Skeletal Radiol 2002;31:208-213. [DOI] [PubMed] [Google Scholar]
- 24.Stanitski DF, Stanitski CL, Trumble S.. Depression of the medial tibial plateau in early-onset Blount disease: myth or reality? J Pediatr Orthop 1999;19:265-269. [DOI] [PubMed] [Google Scholar]
- 25.Zorzi AR, da Silva HG, Muszkat C, et al. Opening-wedge high tibial osteotomy with and without bone graft. Artif Organs 2011;35:301-307. [DOI] [PubMed] [Google Scholar]
- 26.Arrington ED, Smith WJ, Chambers HG, Bucknell AL, Davino NA.. Complications of iliac crest bone graft harvesting. Clin Orthop Relat Res 1996;329:300-309. [DOI] [PubMed] [Google Scholar]
- 27.Goulet JA, Senunas LE, DeSilva GL, Greenfield ML.. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop Relat Res 1997;339:76-81. [DOI] [PubMed] [Google Scholar]
- 28.Seagrave RA, Sojka J, Goodyear A, Munns SW.. Utilizing reamer irrigator aspirator (RIA) autograft for opening wedge high tibial osteotomy: A new surgical technique and report of three cases. Int J Surg Case Rep 2014;5:37-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Pablos J, Azcárate J, Barrios C.. Progressive opening-wedge osteotomy for angular long-bone deformities in adolescents. J Bone Joint Surg [Br] 1995;77-B:387-391. [PubMed] [Google Scholar]
- 30.Coogan PG, Fox JA, Fitch RD.. Treatment of adolescent Blount disease with the circular external fixation device and distraction osteogenesis. J Pediatr Orthop 1996;16:450-454. [DOI] [PubMed] [Google Scholar]
- 31.Hayek S, Segev E, Ezra E, Lokiec F, Wientroub S.. Serrated W/M osteotomy. Results using a new technique for the correction of infantile tibia vara. J Bone Joint Surg (Br) 2000;82:1026-1029. [DOI] [PubMed] [Google Scholar]
- 32.Rab GT. Oblique tibial osteotomy for Blount’s disease (tibia vara). J Pediatr Orthop 1988;8:715-720. [DOI] [PubMed] [Google Scholar]
- 33.Miller S, Radomisli T, Ulin R.. Inverted arcuate osteotomy and external fixation for adolescent tibia vara. J Pediatr Orthop 2000;20:450-454. [PubMed] [Google Scholar]
- 34.Martin SD, Moran MC, Martin TL, Burke SW.. Proximal tibial osteotomy with compression plate fixation for tibia vara. J Pediatr Orthop 1994;14:619-622. [DOI] [PubMed] [Google Scholar]
- 35.Ferriter P, Shapiro F.. Infantile tibia vara: factors affecting outcome following proximal tibial osteotomy. J Pediatr Orthop 1987;7:1-7. [PubMed] [Google Scholar]
- 36.Price CT, Scott DS, Greenberg DA.. Dynamic axial external fixation in the surgical treatment of tibia vara. J Pediatr Orthop 1995;15:236-243. [PubMed] [Google Scholar]
- 37.Smith SL, Beckish ML, Winters SC, Pugh LI, Bray EW.. Treatment of late-onset tibia vara using afghan percutaneous osteotomy and orthofix external fixation. J Pediatr Orthop 2000;20:606-610. [DOI] [PubMed] [Google Scholar]
- 38.Stanitski DF, Srivastava P, Stanitski CL.. Correction of proximal tibial deformities in adolescents with the T-Garches external fixator. J Pediatr Orthop 1998;18: 512-517. [PubMed] [Google Scholar]
- 39.Chotigavanichaya C, Salinas G, Green T, Moseley CF, Otsuka NY.. Recurrence of varus deformity after proximal tibial osteotomy in Blount disease: long-term follow-up. J Pediatr Orthop 2002;22:638-641. [PubMed] [Google Scholar]
- 40.Loder RT, Johnston CE II. Infantile tibia vara. J Pediatr Orthop 1987;7: 639-646. [PubMed] [Google Scholar]
- 41.Payman KR, Patenall V, Borden P, Green T, Otsuka NY.. Complications of tibial osteotomies in children with comorbidities. J Pediatr Orthop 2002;22: 642-644. [PubMed] [Google Scholar]
- 42.Wilson NA, Scherl SA, Cramer KE.. Complications of high tibial osteotomy with external fixation in adolescent Blount’s disease. Orthopedics 2007;30: 848-852. [DOI] [PubMed] [Google Scholar]
- 43.Li Y, Spencer SA, Hedequist D.. Proximal tibial osteotomy and Taylor Spatial Frame application for correction of tibia vara in morbidly obese adolescents. J Pediatr Orthop 2013;33:276-281. [DOI] [PubMed] [Google Scholar]
- 44.Feldman DS, Madan SS, Koval KJ, et al. Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J Pediatr Orthop 2003;23:387-391. [PubMed] [Google Scholar]
- 45.Manner HM, Huebl M, Radler C, et al. Accuracy of complex lower-limb deformity correction with external fixation: a comparison of the Taylor Spatial Frame with the Ilizarov ring fixator. J Child Orthop 2007;1:55-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Castañeda P, Urquhart B, Sullivan E, Haynes RJ.. Hemiepiphysiodesis for the correction of angular deformity about the knee. J Pediatr Orthop 2008;28:188-191. [DOI] [PubMed] [Google Scholar]
- 47.Oto M, Yilmaz G, Bowen JR, Thacker M, Kruse R.. Adolescent Blount disease in obese children treated by eight-plate hemiepiphysiodesis. Eklem Hastalik Cerrahisi 2012;23:20-24. [PubMed] [Google Scholar]


