Abstract
Objective
The purpose of this study was to investigate whether changes occurred in the clinical features of acute colonic diverticulitis (ACD) over a period of 10 years, to estimate the long-term probability of disease recurrence and to investigate whether it could be treated in an outpatient setting.
Methods
Between January 1998 and January 2009, 488 ACD patients were diagnosed and treated in Saiseikai Central Hospital, Tokyo. The diagnoses were made by ultrasonography (US) and/or CT. We investigated the time-dependent changes in the characteristics of patients with ACD, and we used the Kaplan-Meier method to estimate the cumulative probability of recurrence, based on information from a questionnaire.
Results
The percentage of patients who were diagnosed with left-sided ACD significantly increased over time in comparison to those with right-side disease (4% in 1998, 36% in 2009). Patients with left-sided ACD were significantly older and were diagnosed at a more advanced disease stage than those with right-sided ACD. Among the 212 ACD patients who responded to the questionnaire, the cumulative probability of recurrence in 125 patients with no history of ACD at 2.9, 5.9 and 10.1 years was 16.0%, 20.1% and 26.2%, respectively. The probability of recurrence in patients with right-sided and left-sided ACD did not differ to a statistically significant extent. In addition, outpatient treatability in patients with left-sided to right-sided ACD did not differ to a statistically significant extent (66.6% vs. 70.1%).
Conclusion
The ratio of left-sided to right-sided ACD was found to have increased over the past decade. Left-sided ACD patients were older and their incidence of complications was higher in comparison to right-sided patients; however, the rate of recurrence and outpatient treatability in patients with left-sided and right-sided ACD did not differ to a statistically significant extent.
Keywords: acute colonic diverticulitis, clinical features, conservative treatment, surgical treatment, recurrence
Introduction
The clinical features of ACD in Japanese patients have become similar to those in Western populations, with left-sided ACD becoming dominant and more severe. However, the outcome of uncomplicated ACD in the outpatient setting did not differ between patients with left-sided and right-sided disease, indicating that left-sided ACD is treatable in the outpatient setting. Thus, the treatment of uncomplicated ACD in an outpatient setting should be recommended more frequently in Japan, regardless of the location of ACD.
Diverticular disease of the colon is becoming widespread in Japan, in part due to the aging of the country's population and the adoption of Western eating habits (1,2). While most affected individuals are asymptomatic, some develop serious complications, such as acute colonic diverticulitis (ACD) and colonic diverticular bleeding (3,4). The clinical spectrum of ACD ranges from asymptomatic illness to symptomatic illness with potentially fatal complications (1).
There are differences in the clinical features of ACD in Asian and Western countries. One of the most striking discrepancies is in the location of ACD in the colon; while ACD on the left side of the colon is dominant in Western countries, right-sided ACD is dominant in Asia (5-7). Previous reports have shown that right-sided ACD tends to have a more benign clinical outcome than left-sided ACD (8).
A recent study reported that the clinical features of ACD worsen over time in patients with left-sided ACD (9). Meanwhile, Manabe et al. recently performed a cross-sectional study to investigate the population-level characteristics of ACD (10). Building on these studies, we hypothesized that the incidence of left-sided ACD is increasing in Japan. It is important to clarify whether left-sided ACD is increasing-similarly to Western countries- because we proposed treating mild-to-moderate ACD in an outpatient setting ACD (11) based on data from patients with right-sided ACD. Moreover, it is clinically important to determine whether the rate of recurrence differs between patients with left-sided and right-sided ACD.
In the present study, we retrospectively reviewed medical records to determine whether the ratio of left-sided to right-sided ACD changed at our hospital over a 10-year period. We also investigated the long-term recurrence of ACD and the treatability of left-sided ACD in the outpatient setting.
Materials and Methods
Ethical considerations
The study protocol was approved by the review board of Saiseikai Central Hospital and the study was performed in accordance with the Declaration of Helsinki.
Inclusion and exclusion criteria
All consecutive patients in our hospital who were given a final diagnosis of ACD between January 1998 and January 2009 were enrolled in the present study. ACD is suspected in patients with lower abdominal pain (typically in the right lower quadrant), abdominal tenderness on physical examination, and leukocytosis on laboratory testing. The diagnosis is usually confirmed by US and/or CT. The US criteria for the diagnosis of ACD include inflamed diverticula, as well as the presence of pericolitis, abscess formation, and/or free air. The CT criteria included localized thickening of the colon wall to ≥5 mm and signs of pericolic fat inflammation, with or without abscess formation and/or extraluminal air.
The exclusion criteria were as follows: patients in whom a differential diagnosis could not be made between appendicitis and right-sided diverticulitis, and patients with a history of colonic surgery or coexisting colon cancer.
Data collection
A retrospective case series study was conducted using medical records of patients who were treated at Saiseikai Central Hospital, Tokyo. We reviewed the medical records of 486 consecutive patients who were diagnosed with ACD and who were treated at Saiseikai Central Hospital, Tokyo from January 1998 to December 2009.
The demographic features included age, sex, ACD location, medical history of ACD comorbidities, status of complications and surgical status. The location of ACD was classified as follows: left-sided ACD involved the descending colon and/or sigmoid colon; right-sided ACD involved the cecum and/or ascending colon and/or hepatic flexure. In our study, the indications for surgery were as follows: perforation associated with generalized peritonitis, large abscesses, and a lack of response to conventional treatments and progression to peritonitis. Furthermore, complicated diverticulitis was defined based on the presence of an abscess of >2 cm in diameter, perforation, obstruction or fistula. ACD was classified according to a US-based classification system (11). Grade I is defined by an inflamed diverticulum without large (>2 cm) abscesses or perforations. Grade I is further classified into the following sub-grades are applied: Grade Ia, an inflamed diverticulum (in which the inflammation is limited to the diverticulum); Grade Ib, an inflamed diverticulum with pericolitis (the inflammation clearly extends to the pericolic tissue surrounding the diverticulum); and Grade Ic, an inflamed diverticulum with an abscess of ≤2 cm in diameter.
Grade II is defined by an inflamed diverticulum with an abscess of >2 cm in diameter, or perforation. Clinically, Grade I (Ia-c) corresponds to mild-to-moderate ACD, which can be treated on an outpatient basis, while Grade II corresponds to severe ACD, which requires inpatient care (11). Uncomplicated diverticulitis is defined as diverticulitis without any of the complications noted in the present report.
Patients who were considered to be treatable as outpatients (because US and/or CT indicated uncomplicated ACD) were treated according to a 10-day treatment protocol (11). Outpatients with any of the following conditions were excluded: complicated ACD, bacteremia, or any severe comorbidity (such as uncontrolled diabetes mellitus, heart failure, renal failure or end-stage cancer). In addition, patients who had undergone pre-treatment involving the use of broad-spectrum antibiotics (within 24 hours prior to presentation in the outpatient clinic) and those who were deemed unable to understand the protocol or manage self-care were excluded from the study.
Follow-up
In June 2013, all patients were contacted by mail, and data on recurrent ACD, the time of recurrence, the lesion site (if possible), and the type of therapy (conservative or surgery) were collected. Recurrence was defined as a new episode of ACD at least 30 days after initial successful conservative or surgical treatment.
In patients with recurrence, the ACD-free period was calculated from the date of the hospital visit to the date of ACD recurrence. In patients without recurrence, the ACD-free period was calculated from the date of the patient's first study-site hospitalization to the date on which the patient was contacted.
Statistical analysis
All statistical analyses were performed using the SPSS software program (version 22.0, IBM SPSS, Tokyo, Japan). Significant differences among the categorical data or between two groups were assessed using the chi-squared test or Student's t-test, respectively. The cumulative probability of recurrence was calculated by the Kaplan-Meier method, and significant differences between the two groups were determined using a generalized Wilcoxon test. p values of <0.05 were considered to indicate statistical significance.
Results
The changing colonic location of ACD and the clinical characteristics of left-sided ACD in Japan
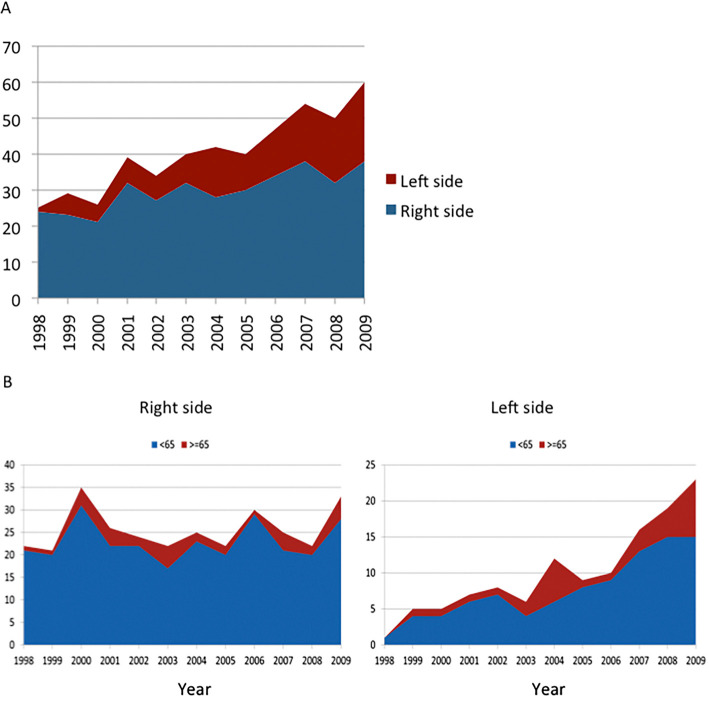
Fig. 1A shows the time-dependent changes in the ratio of left-sided ACD to right-sided ACD. The number of patients with ACD increased year by year. The proportion of patients who presented with left-sided ACD showed a significant increase (4% in 1998 vs. 36.7% in 2009, p<0.05). The trends in the first episode of ACD stratified by age (≥65 years and <65 years) are shown in Fig. 1B. The increase in left-sided ACD was predominantly observed in patients who were ≥65 years of age.
Figure 1.
The time-dependent changes in the clinical characteristics of ACD A). The time-dependent changes in the location of ACD. B) Trends in the first episode of ACD with stratification by age (≥65 years and <65 years).
Table 1 shows the characteristics of left-sided and right-sided ACD across all cases. The age of patients with left-sided disease was significantly higher (p<0.01) in comparison to patients with right-sided disease. Furthermore, the percentage of patients with a history of ACD (left-sided, 42.2% vs. right-sided, 19.2%) and a more severe grade of ACD (Grade II: 10.9% vs. 2.8%) was higher among patients with left-sided ACD. Among the 127 patients with left-sided ACD, the site of disease development was the descending colon in 70 patients, and the sigmoid colon in 57 patients. Among the 359 patients with right-sided ACD, the site of development was the ascending colon and/or cecum in 351 patients and the hepatic flexure in 8 patients.
Table 1.
Patient Characteristics of Acute Colonic Diverticulitis.
| Right side | Left side | |||
|---|---|---|---|---|
| (n=359) | (n=127) | p | ||
| Age: mean (SD) | 46.0 (13.7) | 54.9 (13.2) | <0.001 | |
| Sex : men:women (% of men) | 243:116 (67.7) | 83:44 (65.4) | ns | |
| WBC (/mm3) [mean(SD)] | 10,741 (3,356) | 10,5443 (3,917) | ns | |
| CRP (mg/dL) [median (IQR)] | 4.6 (7.7) | 4.3 (8.8) | ns | |
| Past history of ACD (%) | 69 (19.2) | 54 (42.2) | <0.001 | |
| Stage | Ia | 50 (13.9) | 22 (17.2) | |
| Ib | 262 (73.0) | 83 (64.8) | ||
| Ic | 37 (10.3) | 9 (7.0) | ||
| II | 10 (2.8) | 14 (10.9) | 0.002 | |
| Surgical treatment | 6 (1.7%) | 4 (3.1%) | ns |
WBC: white blood cell, CRP:C-reactive protein, ACD: acute colonic diverticulitis, SD: standard deviation, IQR: interquatar range
Complicated ACD and surgical and/or drainage therapies
Among the 359 cases of right-sided ACD and 127 cases of left-sided ACD, 24 patients with complicated ACD [right-sided ACD, n=10 (2.8%); left-sided ACD, n=14 (11.0%)] were treated as inpatients. Table 2 summarizes the patient characteristics. Among the 10 cases of complicated right-sided ACD, 6 cases involved small abscesses (size, <5 cm), and 3 involved large abscesses (size, ≥5 cm). In contrast, among the 14 cases of complicated left-sided ACD, 4 cases involved small abscesses (size, <5 cm), 2 cases involved large abscesses (size, ≥5), 3 cases involved perforation, and 1 case involved peritonitis. The right-sided cases were treated with antibiotics (n=7), percutaneous drainage under US guidance (n=2) or surgical resection (n=1). The left-sided cases were treated with antibiotics (n=8), percutaneous drainage under US guidance (n=2) or surgical resection (n=4). No ACD-related deaths occurred in either the left-sided or right-sided groups.
Table 2.
Patient Characteristics of Complicated Acute Colonic Diverticulitis.
| Right side | Left side | ||
|---|---|---|---|
| (n=10) | (n=14) | p | |
| Percentage of all ACD cases | 2.8% | 10.9% | <0.01 |
| Presenting features | |||
| Age: mean (SD) | 47.9 (11.4) | 53.6 (12.8) | ns |
| Sex : men:women (% of men) | 7:3 (70%) | 8:6 (57.1%) | ns |
| WBC (/mm3) [mean (SD)] | 12,900 (3,355) | 12,600 (3,833) | ns |
| CRP (mg/dL) [median (IQR)] | 7.8 (29.3) | 16.9 (19.2) | ns |
| Past history of ACD (%) | 2 (20) | 2 (14.3) | ns |
| Treatment | ns | ||
| Medical | 7 | 8 | |
| Percutaneous Drainage | 2 | 2 | |
| Surgical | 1 | 4 |
WBC: white blood cell, CRP:C-reactive protein, ACD: acute colonic diverticulitis, SD: standard deviation, IQR: interquatar range
Outpatient treatment
We tracked the results of the 464 patients with uncomplicated ACD who were treated as outpatients (right-sided/left-sided, 350/114). We diagnosed uncomplicated ACD according to the US (and/or CT)-based classification. Among the 350 patients with right-sided ACD, 233 (66.6%) were treated as outpatients. Among the 114 patients with left-sided ACD, 80 (70.1%) were treated as outpatients. There were no significant differences between the patients with right-sided and left-sided ACD in terms of the outpatient treatment outcomes.
Eighteen patients (5.7%) with right-sided ACD were unsuccessfully treated as outpatients and required hospitalization due to a worsening of their abdominal symptoms without obvious changes in their US results. These patients all showed mild C-reactive protein (CRP) elevation. Upon admission, they were treated with intravenous antibiotics; all of these patients improved. Four patients (5.0%) with left-sided ACD were unsuccessfully treated as outpatients, and showed an exacerbation of their abdominal symptoms without changes that were detectable by US, and with a mild CRP elevation. They were also treated in hospital with intravenous antibiotics. None of these patients required surgical treatment.
Follow-up
Two hundred twelve ACD patients (right-sided, n=156, left-sided, n=56) responded to the questionnaires (response rate, 43.6%). The patients' characteristics are summarized in Table 3. In this study population, the left-sided ACD patients were older in comparison to the right-sided patients. Among the 212 ACD patients who responded to the questionnaires, 53 (25%) reported having an additional episode of ACD. A greater proportion of right-sided patients experienced a second episode after treatment for ACD (right-sided, 42/156; 26.9% vs. left-sided, 11/53; 19.6%). The mean [standard deviation (SD)] observation period was 6.4 (4.0) years (range, 0.1-14.8). Using data from all patients, the cumulative probability of recurrence, as determined by a Kaplan-Meier analysis, at 5.2 and 10.1 years was 22.2% and 29.8%, respectively (Fig. 2A). There was no significant difference in the location of ACD in the recurrent cases (p=0.462; generalized Wilcoxon test) (Fig. 2B). Among the patients without a preceding episode of ACD, the cumulative probability of recurrence at 2.9, 4.2 and 10.1 years was 16%, 18.7% and 26.2%, respectively. Among the patients who had a preceding episode of ACD, the cumulative probability of recurrence at 1.6 and 4.3 years was 28.9% and 32.3%, respectively (p=0.085; generalized Wilcoxon test) (Fig. 2C).
Table 3.
Patient Characteristics of Acute Colonic Diverticulitis who Responded to the Questionneir.
| Right sider (n=156) |
Left side (n=56) |
p | |
|---|---|---|---|
| Response rate to the questionnaire survey | 43.6% | 43.8% | ns |
| Observation period year [mean (SD)] | 6.7 (4.2) | 5.4 (3.2) | <0.05 |
| Presenting features | |||
| Age: mean (SD) | 49.9 (13.6) | 62.2 (12.3) | <0.001 |
| Sex : men:women (% of men) | 112:44 (71.8) | 39:17 (69.6) | ns |
| WBC (/mm3) [mean(SD)] | 10,635 (3,206) | 10,181(4,001) | ns |
| CRP (mg/dL) [median (IQR)] | 4.6 (8.0) | 3.1 (4.4) | ns |
| Past history of ACD (%) | 25 (16.0) | 13 (23.2) | ns |
| Recurrence (%) | 42 (26.9) | 11 (19.6) | ns |
WBC: white blood cell, CRP:C-reactive protein, ACD: acute colonic diverticulitis, SD: standard deviation, IQR: interquatar range
Figure 2.
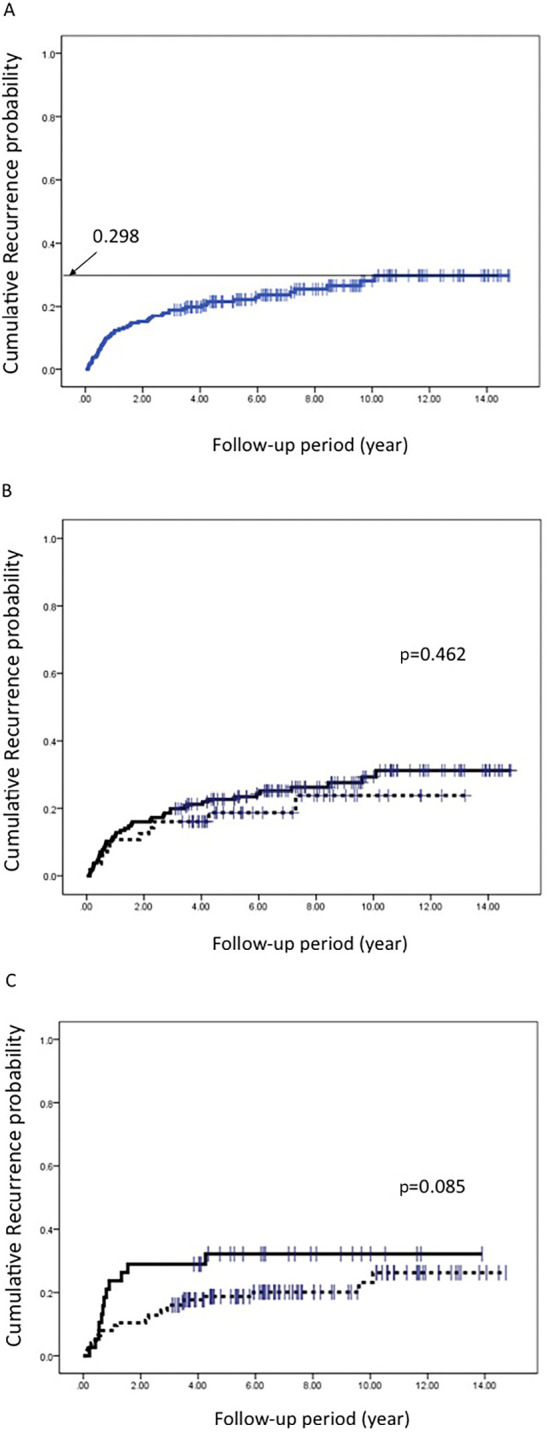
The cumulative probability of recurrence of ACD as estimated by the Kaplan-Meier method. A) Using the data from all ACD patients, B) Stratified based on a history of ACD. The solid line represents the ACD patients without a history of ACD. The broken line represents the ACD patients with a history of ACD. C) Stratification based on the location of ACD. The solid line represents right-sided ACD. The broken line represents left-sided ACD. | indicates censored cases.
Discussion
This retrospective study provides evidence of the recent trends in ACD in Japanese patients, and shows that the ratio of left-sided ACD to right-sided ACD has been increasing. The estimated probability of recurrence within 10 years was 20-30%, with no significant difference between right-sided and left-sided ACD. In addition, mild-to-moderate left-sided ACD could be treated on an outpatient basis, similarly to right-sided ACD; however, left-sided ACD patients were older and exhibited complications more frequently in comparison to patients with right-sided ACD.
The acquired form of diverticular disease is extremely common in Western societies, in which it affects approximately 5-10% of the population over 45 years of age and almost 80% of the population >85 years of age. Up to 20% of patients with ACD are <50 years of age (7). In Western societies, symptomatic ACD has been reported to account for approximately 20% of all ACD, with 15-24% of cases requiring surgical treatment (12,13). Although 85% of cases of diverticulitis in Caucasians occur in the sigmoid and descending colon, diverticula may be found throughout the colon (14,15). In contrast, right-sided diverticulitis is more common in Asians (16), including Japanese, and tends to follow a more benign course than left-sided ACD (10). The etiological and pathophysiological causes of this difference in the clinical features of colonic diverticulosis between Asians and Caucasians are largely unknown.
In Japan, the annual incidence of diverticulitis has been increasing rapidly, and the clinical features have been changing (10,17). Moreover, our present results and a previous report (11) demonstrate that ACD in Japanese patients increasingly tends to present on the left side of the colon. However, some clinical features of left-sided ACD in Japan are different from left-sided ACD in Caucasians. First, the present results and a previous study (10) show that the increase in left-sided ACD in Japan is not uniform across all ages; rather, it is predominant in older patients. Second, in Caucasians, ACD is more common in women (18-20), whereas men were more commonly affected in the Japanese population.
Conversely, Japanese and Caucasian patients share some similar features. The clinical course of ACD in left-sided cases is more severe than that in right-sided cases, and the incidence of surgery for complicated ACD is accordingly higher in left-sided ACD (7,18). This observation could be explained by colon anatomy. The ascending colon is fixed to the retroperitoneum; thus, inflammation may be restricted to a small area. In contrast, the sigmoid colon is not attached to the retroperitoneum, so inflammation may be more widespread.
With respect to the observed etiological differences, previous studies have shown primarily anatomical differences between right-sided and left-sided diverticula (21). Right-sided diverticula are congenitally formed by the outpouching of an entire layer of the weakened intestinal wall. In contrast, left-sided diverticula are acquired, possibly as a result of diet, habitual constipation, increased colonic pressure and aging (7); accordingly, left-sided diverticulitis is more common in elderly populations. This hypothesis is consistent with our present results and previous findings (10). Notably, the lifestyle changes in Japanese may predispose elderly people to left-sided ACD. In addition, complicated ACD was more often observed in left-sided ACD than in right-sided ACD, indicating that right-sided ACD tends to have a more benign clinical outcome than left-sided ACD. However, the rate of recurrence in right-sided ACD was not significantly different from that in left-sided ACD, and patients with mild-to-moderate left-sided ACD could be treated in an outpatient setting-similarly to patients with right-sided ACD.
A recent population-based study of ACD in Americans by Bharucha et al. (22) revealed that the incidence of recurrent ACD at 5 years was 17% among patients with a single prior episode of the disease. Moreover, the incidence of ACD in 2000-2007 was 50% higher than that in 1990-1999 (23). These findings are comparable to our results; however, a notable difference is that left-sided ACD was more prevalent in younger Caucasian populations (23), while left-sided ACD was more prevalent in the elderly Japanese population. Although we did not directly compare the clinical features of left-sided ACD between Japanese and Western patients, the authors hypothesized that the prevalence of potent risk factors for diverticulitis, namely a low dietary fiber intake and obesity, have markedly increased in younger Caucasian populations.
In the present study, left-sided ACD patients had second and third episodes of ACD more frequently than right-sided patients. In our follow-up analysis, however, the probability of recurrence in the right-sided and left-sided ACD cases (among the 212 patients who responded to the questionnaire) did not differ to a statistically significant extent. The ACD-free periods of the left-sided ACD cases were not significantly shorter in comparison to the right-sided cases. Thus, further large-scale follow-up studies are needed to evaluate the difference in the probability of recurrence between right-sided and left-sided ACD in Japan.
The present study is associated with several limitations. First, our study might have included a bias because it was a hospital-based observational study that was conducted in a single institution, and hence was not representative of ACD in the Japanese population as a whole. Second, information on recurrence was obtained from a questionnaire; thus, the definition of ACD was not clear, and an element of self-selection and a recall bias might have been involved. However, our study included a large number of ACD patients (approaching 500 cases), and our findings were consistent with previous studies that have evaluating the clinical features of left-sided ACD in Japanese patients (10).
Conclusion
The ratio of left-sided to right-sided ACD has been increasing over the past decade. Left-sided ACD patients were older and exhibited complications more frequently in comparison to patients with right-sided ACD; however, the rates of recurrence and outpatient-treatability in the two groups did not differ to a statistically significant extent.
The authors state that they have no Conflict of Interest (COI).
References
- 1.Stollman NH, Raskin JB. Diverticular disease of the colon. J Clin Gastroenterol 29: 241-252, 1999. [DOI] [PubMed] [Google Scholar]
- 2.Miura S, Kodaira S, Aoki H, Hosoda Y. Bilateral type diverticular disease of the colon. Int J Colorectal Dis 11: 71-75, 1996. [DOI] [PubMed] [Google Scholar]
- 3.Etzioni DA, Cannom RR, Ault GT, Beart RW Jr, Kaiser AM. Diverticulitis in California from 1995 to 2006: increased ratios of treatment for younger patients. Ann Surg 249: 210-217, 2009. [PubMed] [Google Scholar]
- 4.Etzioni DA, Mack TM, Beart RW Jr, Kaiser AM. Diverticulitis in the United States: 1998-2005: changing patterns of disease and treatment. Am Surg 75: 981-985, 2009. [DOI] [PubMed] [Google Scholar]
- 5.Chia JG, Wilde CC, Ngoi SS, Goh PM, Ong CL. Trends of diverticular disease of the large bowel in a newly developed country. Dis Colon Rectum 34: 498-501, 1991. [DOI] [PubMed] [Google Scholar]
- 6.Miura S, Kodaira S, Shatari T, Nishioka M, Hosoda Y, Hisa TK. Recent trends in diverticulosis of the right colon in Japan: retrospective review in a regional hospital. Dis Colon Rectum 43: 1383-1389, 2000. [DOI] [PubMed] [Google Scholar]
- 7.Stollman N, Raskin JB. Diverticlar disease of the colon. Lancet 363: 631-639, 2004. [DOI] [PubMed] [Google Scholar]
- 8.Markham NI, Li AK. Diverticulitis of the right colon-experience from Hong Kong. Gut 33: 547-549, 1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tarao K, Sekino Y, Nonaka T, et al. Recent trends in colonic diverticulosis in Yokohama city: a possibility of changing to a more western profile. Intern Med 54: 2545-2550, 2015. [DOI] [PubMed] [Google Scholar]
- 10.Manabe N, Haruma K, Nakajima A, et al. Characteristics of colonic diverticulitis and factors associated with complications: a Japanese multicenter, retrospective, cross-sectional study. Dis Colon Rectum 58: 1174-1181, 2015. [DOI] [PubMed] [Google Scholar]
- 11.Mizuki A, Nagata H, Tatemichi M, et al. The out-patient management of patients with acute mild-to-moderate colonic diverticulitis. Aliment Pharmacol Ther 21: 889-897, 2005. [DOI] [PubMed] [Google Scholar]
- 12.Ferzoco LB, Raptopoulos V, Silen W. Acute diverticulitis. N Engl J Med 338: 1521-1526, 1998. [DOI] [PubMed] [Google Scholar]
- 13.Anderson L. Acute diverticulitis of the cecum; study of 99 surgical cases. Surgery 22: 479-488, 1947. [PubMed] [Google Scholar]
- 14.Anscombe AR, Keddie NC, Schofield PF. Solitary ulcers and diverticulitis of the caecum. Br J Surg 54: 553-557, 1967. [DOI] [PubMed] [Google Scholar]
- 15.Chiu TC, Bailey HR, Hernandez AJ Jr. Diverticulitis of the midrectum. Dis Colon Rectum 26: 59-60, 1983. [DOI] [PubMed] [Google Scholar]
- 16.Lee YS. Diverticular disease of the large bowel in Singapore. An autopsy survey. Dis Colon Rectum 29: 330-335, 1986. [DOI] [PubMed] [Google Scholar]
- 17.Sugihara K, Muto T, Morioka Y, Asano A, Yamamoto T. Diverticular disease of the colon in Japan. A review of 615 cases. Dis Colon Rectum 27: 531-537, 1989. [DOI] [PubMed] [Google Scholar]
- 18.Levien DH, Mazier WP, Surrell JA, Raiman PJ. Safe resection for diverticular disease of the colon. Dis Colon Rectum 32: 30-32, 1989. [DOI] [PubMed] [Google Scholar]
- 19.Munson KD, Hensien MA, Jacob LN, Robinson AM, Liston WA. Diverticulitis. A comprehensive follow-up. Dis Colon Rectum 39: 318-322, 1996. [DOI] [PubMed] [Google Scholar]
- 20.Wedell J, Banzhaf G, Chaoui R, Fischer R, Reichmann J. Surgical management of complicated colonic diverticulitis. Br J Surg 84: 380-383, 1997. [PubMed] [Google Scholar]
- 21.Rodkey GV, Welch CE. Diverticulitis of the colon: evolution in concept and therapy. Surg Clin North Am 45: 1231-1434, 1965. [DOI] [PubMed] [Google Scholar]
- 22.Bharucha AE, Parthasarathy G, Ditah I, et al. Temporal trends in the incidence and natural history of diverticulitis: a population-based study. Am J Gastroenterol 110: 1589-1596, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sánchez-Velázquez P, Grande L, Pera M. Outpatient treatment of uncomplicated diverticulitis: a systematic review. Eur J Gastroenterol Hepatol 28: 622-627, 2016. [DOI] [PubMed] [Google Scholar]