Abstract
Research suggests that Mexican immigrants arrive in the United States with equivalent or better health than native-born whites but lose their advantage over time. We seek to examine systematically how well the patterns of initial advantage and deteriorating health apply to immigrants originating from other regions of the world – regions that represent a growing proportion of U.S. immigrants. We begin by identifying which of the groups in our study have a health advantage compared to U.S.-born whites and to Mexican immigrants. We then we assess changes in health over time, controlling for variation in the health profiles of cohorts upon arrival. We use logistic regression of self-rated health and heart conditions with data from the 2004–2013 National Health Interview Survey. The results reveal diversity and similarity in health outcomes across world regions of origin, both on arrival and over time. By comparing and contrasting cases previously examined in isolation, we clarify and qualify theories of the immigrant health paradox and health deterioration.
Keywords: Nativity, Self-rated health, Heart condition, Latino paradox, Synthetic cohort, Logistic regression, National Health Interview Survey
1. Introduction
Research on immigrant health has grown rapidly in response to changes in the demographic composition of the U.S. population. In 2013, immigrants comprised fourteen percent of the U.S. population, up from only five percent in 1970 (U.S. Bureau of Census, 2013). The overwhelming majority of U.S.-based studies have focused on the largest group, Latino immigrants (Van Hook et al., 2014). The unusual combination of good health and low socioeconomic status upon arrival (i.e., Hispanic health paradox) has drawn considerable attention, as has the fact that the health of Latino immigrants tends to decline as they spend more time in the U.S. (Antecol and Bedard, 2006; Powers, 2013; Riosmena et al., 2013). Findings from these studies have so dominated the immigrant health literature that the term “Hispanic health paradox” has been expanded to that of “immigrant health paradox” or the “healthy migrant hypothesis” (Gubernskaya, 2015; Richardson et al., 2013; Wingate and Alexander, 2006).
This expansion of terminology potentially conceals diversity in health outcomes among immigrant subpopulations from other world regions of origin (Cunningham et al., 2008). For example, a number of studies focusing on the health and well-being of immigrants from Asia, (Frisbie et al., 2001; Lee et al., 2013; Son, 2013), Africa (Hamilton and Hummer, 2011; Hendi et al., 2015; Read and Emerson, 2005), and the Middle East (Dallo and Borell, 2006; Read and Reynolds, 2012; Read et al., 2005) find both similarities to and differences from the Mexican case.
Relative to studies focused strictly on the Mexican case, few studies have examined immigrants originating from multiple regions of the world simultaneously within the same analytic framework. Thus, the degree to which immigrants from other regions resemble the Mexican case remains unclear. The evidence is also mixed regarding the appropriate reference category when assessing immigrant health. Immigrants may fare better than U.S.-born whites but how well do they fare relative to other immigrant populations? This is an important question because the number of immigrants from Mexico is on the decline, while populations from Asia, Africa and other regions of the world are on the rise (Whatley and Batalova, 2013). Current estimates indicate that the three largest immigrant groups after Mexican-Americans are sizable and growing: Chinese (2.2 million), Indian (1.9 million), and Philippino (1.8 million) (Grieco et al., 2012). Determining the applicability of knowledge gleaned from Mexican immigrants to groups from other world regions will be paramount for informing policies aimed at improving population health. Accordingly, this paper uses nationally representative data to compare the health of immigrants from multiple regions of origin to that of U.S.-born whites and Mexican immigrants.
2. Background
2.1. The health paradox and health deterioration hypotheses
The term “Hispanic health paradox” refers to an unusual combination of low socioeconomic status and good health outcomes observed in immigrant Latino populations. The phenomenon was originally documented by Markides and Coreil (1986), and subsequent studies on Latino immigrant health have consistently replicated this finding. Advantages are observed for mortality (Palloni and Arias, 2004), pregnancy outcomes (Hessol and Fuentes-Afflick, 2000; Hummer et al., 2007), self-rated health (Antecol and Bedard, 2006), activity limitations (Bostean, 2013), heart disease (Singh and Siahpush, 2001) and various mental health conditions (Alegría et al., 2008). Yet, Latinos do not appear to have an advantage over native-born whites on a range of other health conditions, including diabetes (Scheder, 1988), old-age disability (Hayward et al., 2014) and occupational injuries (Pransky et al., 2002), owing largely to the riskier nature of the jobs into which they are sorted (Orrenius and Zavodny, 2009).
One major family of explanations for the initial advantaged health status of immigrants centers around the selective nature of migration. In the case of positive selection, healthier individuals migrate into the U.S. (Jasso et al., 2004; Martinez et al., 2014), while less healthy individuals migrate out, returning to the country of origin (Ceballos, 2011; Hummer et al., 2007). Other explanations relate to differences in lifestyle in host versus receiving countries (Frank and Akresh, 2013; Powers, 2013; Rosenthal, 2014; Singh and Siahpush, 2002). If immigrant health worsens with the adoption of lifestyles more similar to native-born Americans, then perhaps the lifestyles in the countries of origin and on initial arrival in the U.S. have certain health-protective characteristics. Not all culturally-defined lifestyles, however, appear to be healthier than America’s. For example, in the former Soviet Union and throughout Eastern Europe, rates of heavy alcohol consumption and smoking are notably high (Cockerham, 2000). For these groups, health behaviors are a less likely source of any health advantage.
2.2. Generalizing beyond the Mexican case
Although the “Hispanic health paradox” has been expanded to encompass other immigrant groups, the evidence has been less than conclusive. Several studies have shown that even in the face of some similarities with Mexican immigrants, idiosyncratic health and disease patterns are observed among immigrants from different regions of the world (Akresh, 2007; Dallo and Borrell, 2006; David and Collins, 1997; Read and Emerson, 2005). Moreover, many immigrant populations come from regions that have very little in common with Central America or Mexico, in terms of proximity to the U.S. and socio-demographic and cultural characteristics. For these reasons, explanations based on the experiences of Mexicans may be less appropriate for understanding the experiences of other groups.
Possible explanations for the divergent patterns of health among immigrant groups relate to the context and history of out-and in-migration. Those who migrate largely due to push-factors in the country or region of origin, such as natural disasters or political unrest, may not be selected in the same way as those who migrate primarily for economic reasons. In addition, historical differences in relations between the U.S. and other regions of the world have resulted in very different migration patterns from Africa and Asia than from Europe and Mexico, which have, in turn, shaped the social and demographic profile of these groups. The nature of migration streams can affect the extent to which migrants are selected on multiple factors, including health (Lindstrom and Ramirez, 2010). In terms of the context of reception, the existence of co-ethnic communities (Viruell-Fuentes, 2007) as well as the ability to maintain transnational social ties with the sending community (Alcántara et al., 2015) can also influence the health of the migrants in the long term. For non-white immigrants, experiences of racial and ethnic discrimination upon arrival to the U.S. can become particularly salient factors in shaping their health (Ryan et al., 2006).
Much like the case of health upon arrival, the typical pattern of declining health with increased duration found among Mexican immigrants is inconsistent for other immigrant groups (Dallo and Borrell, 2006; Read and Emerson, 2005). Even where an initial advantage is observed, specific patterns of health within certain groups cannot be explained in quite the same way. For example, Dallo and James (2000) found lower levels of acculturation to be associated with increased risk for hypertension among Arab women in Detroit. Moreover, recent research shows a larger effect of time spent in the U.S. on health among those who emigrated at a young versus older age (Holmes et al., 2015) and null effects of acculturation among elderly Latinos (Lopez et al., 2014). This research suggests non-uniform effects of exposure depending on individual characteristics.
2.3. Expectations and research questions
The above literature suggests that the size and scope of the initial immigrant health advantage, as well as trends in health-related outcomes over time, may well vary by region of origin. Yet, compared to work focused on a single (often Latino) immigrant group, prior research has rarely examined immigrants from multiple regions of origin simultaneously within the same analytic framework (for exceptions, see the well-developed literature on pregnancy outcomes exemplified by Acevedo-Garcia et al. (2005), Fuentes-Afflick et al. (1998), Forna et al. (2003), Janevic et al. (2011), Korenbrot et al. (2000) and Qin and Gould (2010) as well as research on obesity and diabetes by Oza-Frank and Narayan (2010) and Singh and Lin (2013a,b)). Further, extant literature has not systematically compared the health of immigrants originating outside of Mexico to that of Mexican immigrants, the case that has anchored conclusions about immigrant health for decades. We attempt to address these shortcomings by examining the health of multiple large and/or growing U.S. immigrant groups within the same analysis and by comparing their outcomes to both U.S.-born whites and the Mexican-born. Specifically, we assess: 1) whether groups originating outside of Mexico arrive in better health than U.S.-born whites, as predicted by the health paradox literature; 2) the extent to which various groups originating outside of Mexico have health profiles similar to those originating from within Mexico; and 3) how applicable the health deterioration hypothesis is for each group.
3. Data and methods
3.1. Data
To examine these questions, we draw on ten waves of merged data from the 2004–2013 National Health Interview Survey (NHIS), an annual multi-purpose health survey conducted by the National Center for Health Statistics and Centers for Disease Control and Prevention and administered by the U.S. Census Bureau. NHIS uses a multi-stage, stratified, cluster design to oversample the black and Latino populations and to obtain a nationally representative sample of the non-institutionalized civilian population. The U.S. Census Bureau conducts face-to-face interviews, collecting information about the health and other characteristics of each member of the household.
The analyses are based on U.S.-born whites (n = 183,795), and foreign-born respondents born in Mexico (n = 27,816), Europe (n = 4706), Russia (n = 779), Africa (n = 1899), the Middle-East (n = 986), Indian subcontinent (hereafter referred to as India; n = 2763), Asia (n = 3802) and Southeast Asia (n = 5058) who are age 18 and older.
3.2. Measures
The dependent variables include one subjective and one objective measure of health. First, self-rated health is assessed with the question, “Would you say that [person’s] health in general is excellent, very good, good, fair, or poor?” Research has demonstrated that self-rated health is a valid predictor of morbidity (Ferraro et al., 1997), morbidity-related disability (Idler and Kasl, 1995) and mortality (Idler and Benyamini, 1999). Moreover, by relying on a subjective measure of health, measurement error associated with variations in medical documentation of illness across social groups is minimized. We have dichotomized this variable into excellent/very good/good health and fair/poor health. Odds of the latter are modeled throughout.
Because subjective assessments of health likely vary cross-culturally, we also include an objective indicator for heart condition, where ‘1’ indicates that the respondent reported that they had once been told by a doctor or other health professional that they had heart disease. We selected this outcome because cardiovascular disease is the leading cause of death in the U.S. and a commonly used measure in studies on population health (Centers for Disease Control, 2015). We model the odds of having been diagnosed with heart disease, setting those who are free of such health concerns as a reference group.
Our key independent variable is region of origin, based on the respondent’s region of birth: Mexico, Europe, Russia, Africa, Middle-East, India, Asia or Southeast Asia. We also use duration of stay in the U.S. as an independent variable in the second part of the analysis. The original categorical variable is coded so that higher values correspond with longer duration of stay in the U.S. We control for several factors known to be associated with health, including gender, age, and socioeconomic status (educational attainment and income). Educational attainment is coded into four categories: less than high school (reference), high school graduate, some college and bachelor’s degree or more. Household income is categorized as low (up to $24,999), middle (between $25,000 and $74,999) and high ($75,000 or more). Gender is coded ‘1’ for female, with male set as the reference category. We include age in all models as well as age-squared, in recognition of the trend in declining health across the life course and the increase in the rate of this decline in later life. We include a variable specifying which of the four census regions the respondents resided in: Northeast (reference category), Midwest, South and West. Finally, we add dummy variables representing the survey year. In sensitivity analyses, we also include indicators for ‘seen doctor’ (“During the past twelve months, have you seen or talked to a general doctor who treats a variety of illnesses about your own health?”) and ‘usual place’ (“Is there a place that you usually go to when you are sick or need advice about your health?”). Although the inclusion of these variables do narrow gaps between groups, they do not alter the pattern or significance of our results.
3.3. Analysis
We begin by presenting descriptive statistics for each of the groups of origin (Table 1). We provide information about statistically significant differences between each group and Mexican immigrants. (The large sample size of U.S.-born whites produces uniformly significant results, rendering significance tests uninformative.) Next, we address the question of whether immigrants from all regions of origin experience a health advantage (Figs. 1 and 2). First, we conduct a series of bivariate binomial logistic regressions predicting the odds of fair or poor self-rated health and heart condition for immigrants from each region of origin relative to U.S.-born whites. In the face of unequal variance across comparison groups, not only standard errors but parameters can also be biased in unpredictable ways. Thus, conclusions based on odds ratios alone should be drawn cautiously. For this reason, we present predicted probabilities and marginal effects in later analysis where comparisons between groups are a central part of the investigation. These models include all control variables described above. Next we replicate this analysis, setting Mexican-born immigrants as the reference group. Throughout this, and subsequent analysis, we apply appropriate sampling weights and variance estimation techniques to address the NHIS’ complex sampling design.
Table 1.
Distribution of select characteristics by region of origin, NHIS 2004–2013.a
| White (US) | Mexico | Europe | Russia | Africa | Middle East | India | Asia | Southeast Asia | |
|---|---|---|---|---|---|---|---|---|---|
| Heart disease | 12.9 | 5.7 | 11.48** | 10.5** | 3.7** | 6.9** | 4.3** | 5.2** | 6.0 |
| Poor self-rated health | 12.1 | 15.3 | 10.4** | 17.3** | 7.2** | 12.1** | 6.2** | 9.4** | 11.0** |
| Female | 51.3 | 47.2 | 53.6** | 53.3** | 44.8** | 45.7** | 43.9** | 57.5** | 55.0** |
| Average age | 48.61 | 42.89 [15.50] | 51.35** [18.48] | 48.20** [19.50] | 39.88** [13.29] | 44.73** [17.07] | 38.84** [13.79] | 46.71** [18.15] | 46.39** [15.62] |
| Less than HS | 11.1 | 55.1 | 10.8** | 10.5** | 9.1** | 13.6** | 7.3** | 11.1** | 13.3** |
| High school | 28.3 | 22.9 | 24.8** | 13.7** | 18.1** | 20.1** | 9.8 | 17.4** | 17.5** |
| College | 60.6 | 22.0 | 64.5** | 75.8** | 72.8** | 66.2** | 82.9** | 71.6** | 69.2** |
| Low income | 30.6 | 55.9 | 30.7** | 38.9** | 40.0** | 41.8** | 24.3** | 34.7** | 25.3** |
| Middle income | 33.5 | 32.2 | 30.0** | 30.3 | 33.3** | 26.5 | 28.4* | 28.0 | 34.4** |
| High income | 35.9 | 11.9 | 39.4** | 30.7** | 26.7** | 31.6** | 47.3** | 37.3** | 40.3** |
| Up to four years | – | 9.7 | 6.4** | 11.6 | 19.3** | 15.6** | 23.7** | 14.8** | 8.7 |
| Five to nine years | – | 16.2 | 8.3** | 19.3** | 24.1** | 13.6* | 21.0** | 13.3** | 10.6** |
| Ten to fourteen years | – | 16.6 | 9.0** | 24.4** | 19.8** | 13.2** | 18.2 | 12.7** | 11.9** |
| Fifteen or more years | – | 57.4 | 76.3** | 44.7** | 36.8** | 57.5 | 37.1** | 59.2** | 68.8** |
| Observations | 183,795 | 25,135 | 4091 | 706 | 1744 | 874 | 2464 | 3366 | 4516 |
p ≤ 0.05
p ≤ 0.10.
Notes: The large sample size of U.S.-born whites produces uniformly significant results, rendering significance tests uninformative.
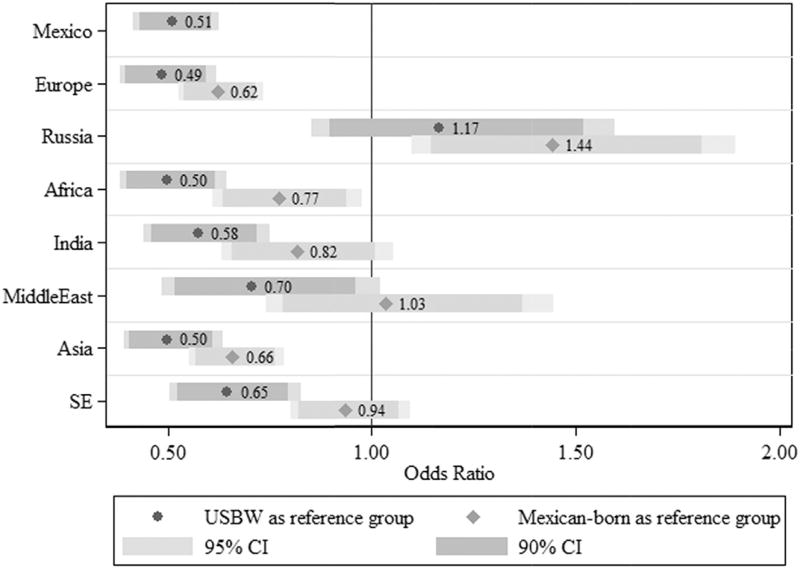
Fig. 1.
Odds ratios with 90% and 95% confidence intervals from logistic regression models predicting nativity gap in poor self-rated health, NHIS 2004–2013.
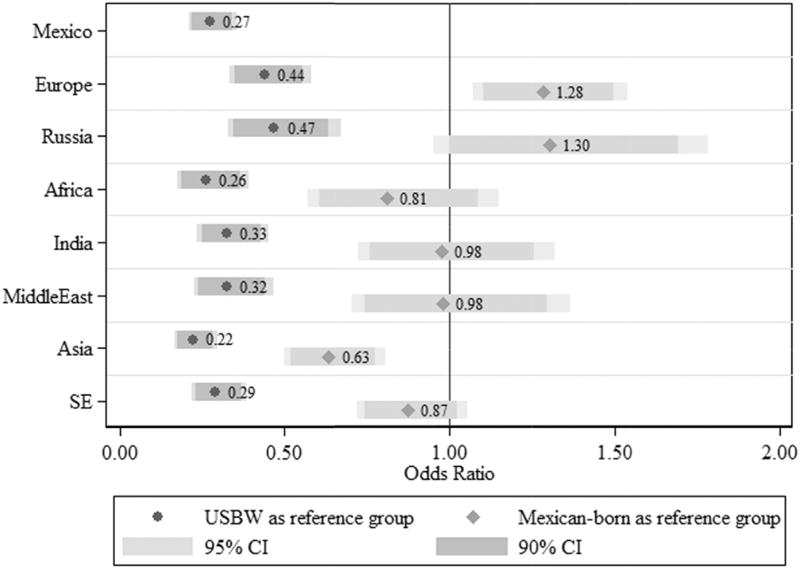
Fig. 2.
Odds ratios with 90% and 95% confidence intervals from logistic regression models predicting nativity gap in heart conditions, NHIS 2004–2013.
Our second series of analyses address the health deterioration hypothesis among a subset of the regions of origin (Table 2). Doing so poses special challenges with the use of cross-sectional data. This is because of the possibility that cohort variations are behind any findings of change over time. In other words, if we observe that the risk of heart disease is higher among immigrants who have been in the U.S. for fifteen years than it is among immigrants who have been here for only five, that could mean one of two things. The first, in keeping with the health deterioration hypotheses, is that, for any given immigrant, the risk of heart disease increases the longer they stay in the U.S. Alternatively, it could mean that the immigrants who immigrated fifteen years ago arrived in worse health than those who migrated five years ago. Recent research accounting for both arrival-cohort and duration suggests that the effect of cohort arrival significantly biases estimates of health trajectories (Hamilton et al., 2015).
Table 2.
Marginal effects of discrete change from U.S. born (“cohort effects”) and from 0 to 4 years (“duration effects”) by region of origin, NHIS 2004–2013.
| Variable | Mexican
|
Russian
|
African
|
Southeast Asian
|
||||
|---|---|---|---|---|---|---|---|---|
| Poor health | Heart condition | Poor health | Heart condition | Poor health | Heart condition | Poor health | Heart condition | |
| Cohort effects | ||||||||
| Immigrated in 1997 or before | −0.057** | −0.068** | 0.011 (0.13) | 0.154 (1.30) | −0.079** | −0.131** | 0.002 (0.05) | 0.006 (0.09) |
| (−5.19) | (−4.63) | (−2.54) | (−10.35) | |||||
| Immigrated in 1998–2002 | −0.075** | −0.079** | −0.057 | 0.132 (1.47) | −0.063** | –0.087** (–2.82) | –0.023 (–0.65) | –0.051 (–1.42) |
| (−9.17) | (−7.39) | (−1.21) | (−2.13) | |||||
| Immigrated in 2003–2007 | −0.059** | −0.071** | −0.008 | –0.009 (–0.12) | −0.055** | –0.083** (–3.05) | −0.064** | −0.066** |
| (−7.29) | (−6.93) | (−0.13) | (−2.32) | (−3.03) | (−2.51) | |||
| Immigrated in 2008–2013 | −0.032** | −0.078** | −0.009 | 0.005 (0.07) | −0.111** | –0.084** (–3.26) | −0.061** | −0.074** |
| (−2.73) | (−6.29) | (−0.15) | (−8.02) | (−3.33) | (−3.37) | |||
| Duration effects | ||||||||
| 5–9 years since arrival | 0.005 (0.39) | −0.010 (−0.56) | 0.107 (1.02) | –0.072* (–1.86) | −0.045 (−1.41) | 0.053 (0.68) | −0.014 (−0.38) | −0.030 (−0.70) |
| 10–14 years since arrival | 0.005 (0.37) | −0.005 (−0.26) | 0.028 (0.31) | −0.095** | 0.038 (0.59) | 0.011 (0.13) | −0.003 (−0.08) | −0.090** |
| (−3.49) | (−3.21) | |||||||
| 15+ years since arrival | 0.064** (3.53) | 0.018 (0.74) | 0.0977 (0.86) | −0.093** | 0.117 (1.21) | 0.312 (1.31) | 0.010 (0.19) | –0.061 (–1.42) |
| (−3.03) | ||||||||
| Observations | 188,133 | 188,002 | 164,669 | 164,562 | 165,709 | 165,605 | 168,394 | 168,282 |
Notes: p ≤ 0.05
p ≤ 0.10.
z-scores in parentheses.
All models include full set of covariates and NHIS sample weights.
Examining how health changes over time for each non-native respondent would allow us to determine what contribution each of these processes makes to observed duration effects. However, the cross-sectional nature of the NHIS data limits possibilities for such analysis. To address this shortcoming, we borrow the method devised by Borjas (1985) and fruitfully applied by Antecol and Bedard (2006) to the subject of immigrant health. This entails the creation of synthetic cohorts, assigning each respondent to one of four multi-year arrival cohorts based on the survey year and length of time in residence: prior to 1997, between 1998 and 2002, 2003–2007 and 2008–2013.
Models of this sort would normally not be identified given the well-known linear dependence problem (whereby age = period -cohort). We enable the inclusion of survey year, cohort and duration in the models simultaneously by setting the native-born as the reference for the cohort variable and estimating the period effect among this group for whom the linear dependency does not obtain. This constrains the period effect to be equal among all sample respondents (i.e. - no year-by-cohort interaction terms are estimated) but this assumption is not implausible. The resulting analysis provides estimates of the difference in health between each immigrant cohort and U.S.-born whites, as well as between each length of stay in the U.S. and 0–4 years, accounting for potential differences in health profiles across immigrant cohorts. The resulting model can be expressed as follows:
where i represents individuals, X the potential confounders described above, A duration of stay, C arrival cohort, ∞ the dependent variable, T survey year, ∏ the period effect and ε the stochastic component.
We generate predicted probabilities based on the above equation, computing the likelihood of each health outcome occurring for immigrants from each region of origin assuming a given set of values for the independent variables. The predictions are calculated as adjusted average predictions rather than adjusted predictions at the mean. This means that rather than generating a prediction using the “mean” value for all control variables, we generate a predicted probability for each case using the observed values of the co-variates and then average those predictions across members of a given region of origin. Marginal effects are then calculated for each group, indicating the effect on health of a discrete change from the base to a given category.
4. Results
4.1. Sample characteristics
Table 1 describes the characteristics of immigrants from the various regions of origin included in our sample. To conserve space, and because its substantive relevance is minimal, we have excluded the breakdown on marital status and region of U.S. residence. The top two rows describe the distribution of the health outcomes across regions of origin. Overall, we see a lot of variability across regions of origin. In the case of heart disease, the U.S.-, European-and Russian-born have the highest rates of over 10%, while the prevalence rates of heart conditions among immigrants born in Africa, India and Asia are less than half that. We see similar variability when looking at self-rated health. The U.S.-, European, Middle-Eastern-, Asian and Southeast Asian-born groups range between 9 and 12% reporting poor self-rated health, but Mexicans and especially Russians show much higher rates (15% and 17% respectively), and the African and Indian group much lower rates (7% and 6% respectively).
European, Russian, Asian and Southeast Asian women outnumber men, whereas the opposite is true among the African, Middle-Eastern and Indian immigrants. In terms of education, we see that a much greater proportion of Mexicans have less than a high school education and that the remaining groups are well-educated, having higher rates of college completion than U.S.-born whites. This is less true of European and Middle-Eastern immigrants and especially true of Indians. Between 30 and 40% of each immigrant sample has income in the highest category, with two deviations – Mexicans and Indians – well-predicted by the education measure.
4.2. Comparisons to U.S.-born whites and Mexican immigrants
Figs. 1 and 2 display the odds ratios for immigrants from each region of origin relative to the U.S.-born whites and Mexican immigrants. These figures are designed to shed light on the first two of our research questions: 1) whether immigrants originating outside of Mexico arrive in better health than U.S.-born whites, as predicted by the immigrant health paradox literature; and 2) the extent to which immigrants from various regions of origin maintain health profiles similar to Mexican-born immigrants. Fig. 1 displays these results for self-rated health with comparisons to U.S.-born whites in blue and to Mexican immigrants in red. Fig. 2 displays the results for heart conditions in the same fashion. We display the 90 and 95% confidence intervals around point estimates in both figures.
In comparing the self-rated health of the foreign to native-born in Fig. 1, we find that Mexican, European, African, Indian and Asian and Southeast Asian immigrants have significantly lower odds of having poor self-rated health. Middle-Eastern immigrants also have lower odds of having poor self-rated health, although this is only significant at the p ≤ 0.1 level. Russian immigrants do not have statistically different odds of poor self-rated health compared to the U.S.-born whites. When examining the comparisons against the Mexican-born as the base category, for self-rated health, Europeans, Africans and Asians have significantly lower odds relative to the Mexican-born and Russians significantly higher odds. Middle-Eastern, Indian and Southeast Asian immigrants do not have statistically different odds of poor self-rated health than do Mexican immigrants.
In Fig. 2, we find that all groups have significantly lower odds of having been diagnosed with a heart condition relative to the U.S-born. With Mexican-born as the base, Asians have significantly lower odds. European and Russian immigrants, on the other hand, have higher odds of having been diagnosed with a heart condition. Among remaining groups, none are statistically different from Mexican immigrants.
4.3. Cohort effects & health deterioration
In order to better understand the findings for groups exhibiting the most divergent patterns in Figs. 1 and 2, Table 2 displays the marginal cohort (top panel) and duration (bottom panel) effects for our immigrant groups. Due to space limitations, we have elected to present the findings for only four of our seven groups (Mexican, Russian, African, Southeast Asian). We have selected these groups as the first represents the most-studied and the latter three represent some of the least-studied groups in our sample; results for these groups should be particularly illuminating. Results for self-rated health are displayed in the first column and heart disease is displayed in the second. For each group, the marginal effects indicate the change in the adjusted average predicted probability of a specific outcome due to a shift from the base to a given category. In the case of cohort effects, this represents the shift from U.S.-born to 0–4 years in residence as an immigrant. In the case of duration effects, it represents the shift from 0 to 4 years to one of three longer residency intervals (5–9 years, 10–14 years and 15 or more years). The pattern of results allows us to investigate the third research question: how applicable is the health deterioration hypothesis for each group? Fitting these duration models while simultaneously estimating cohort effects allows us to test for differences in incoming waves of immigrants relative to the native-born population. Moreover, it permits us to interpret the duration effects net of the influence of any differences in the health of immigrant cohorts upon arrival.
4.4. Cohort effects
We begin by describing the results of the cohort analysis of self-rated health. For self-rated health, the cohort effects are negative in at least one cohort for each immigrant group. These negative effects are significant for all Mexican cohorts as well as the most recent two African and Southeast Asian cohorts. They are not significant for Russians in the second and fourth cohorts, Africans in the first and second cohort or Southeast Asians in the second cohorts. The effects are positive for Russians in the first and third cohorts and Southeast Asians in the first cohort, but none of these coefficients reach statistical significance. Now we turn to the results of the cohort analysis of heart conditions. The effects are again negative for all groups in at least one cohort. The negative effects are significant for all Mexican and African cohorts as well as the two most recent Southeast Asian cohorts. They are not significant for Russians in the third cohort or Southeast Asians in the second cohort. The effects are significantly positive for Russians in the first and second cohorts. They are positive, but insignificant, for Russians in the final cohort as well as Southeast Asians in the first cohort.
4.5. Duration effects
With regard to self-rated health duration effects, the probability of poor self-rated health decreases for African immigrants in the 5–9 year period and for Southeast Asians in the 5–9 and 10–14 year periods. None of these changes are statistically significant. The probability of poor self-rated health is significantly increased for Mexicans after 10 years. Probabilities also increase, although are not significant, for Mexicans in earlier periods as well as for Russians in all periods, Africans in the final two periods and Southeast Asians in the final period.
In the case of heart condition, duration effects indicate that the probability of a heart condition decreases significantly for Russians in the final two periods and Southeast Asians in the middle period. Probabilities also decrease, with marginal significance, for Africans in the final period. Probabilities for Russians and Southeast Asians in other periods, as well as for Mexicans during the 5–9 and 10–14 year periods, are decreased, but not significantly. No groups experience significantly increased probabilities of heart disease, although Mexican and African immigrants do have non-significant positive marginal effects for the final and first two periods, respectively.
5. Discussion
Over a decade ago, Singh and Siahpush (2001, 2002) documented heterogeneity in morbidity and mortality among America’s largest racial/ethnic populations (non-Hispanic whites, blacks, Hispanics, and Asian/Asian Pacific Islanders). Since that time, research and data collection techniques on immigrant health have continued to evolve to acknowledge the ever-changing demographic profile of U.S. immigrants. Our paper contributes to this line of inquiry using unique region of birth information to make comparisons that further illuminate heterogeneity among immigrants upon arrival and over time in the U.S.
Our findings reveal both similarities and diversity in immigrant health—on arrival and over time—based on region of origin and reference category. On arrival, Mexican, European, African, Indian, Asian and Southeast Asian immigrants have significantly lower odds of poor self-rated health when compared to U.S.-born whites. In contrast, Middle-Eastern and Russian immigrants do not have a significant health advantage over the U.S.-born. Even in the case of heart conditions, where there is a uniform advantage among immigrants from all regions of origin relative to U.S.-born whites, the size of this advantage varies depending on region of origin. When the comparison group is Mexican immigrants, we again find similarities and differences to the Mexican case by region of origin and health outcome. For self-rated health, Europeans, Africans, and Asians have significantly lower odds of poor health relative to Mexican immigrants, while Russians have significantly higher odds. Middle-Eastern, Indian and Southeast Asian immigrants do not have statistically different odds of poor self-rated health than do Mexican immigrants. In the case of heart conditions, Asian immigrants have significantly lower odds of receiving a diagnosis relative to the Mexican-born, while European and Russian immigrants have significantly higher odds.
The conclusion is likewise complicated in terms of the health deterioration hypothesis. Here we find that the pattern for self-rated health is generally one of deterioration although, except in the case of Mexicans, few of the duration of stay categories are statistically significant, likely owing to the small sample sizes. Most groups arrive with better self-rated health relative to U.S.-born whites but the advantage diminishes over time. The story with heart disease is different. Here we find that the probabilities decrease for Russians and Southeast Asians in all periods after the initial one and that, despite the very modest sample size, these decreases are significant in at least one period for three of the four groups (Russians in final two periods, Southeast Asians in middle and Africans in final). While some groups experience increased odds of heart disease over time (Africans consistently and Mexicans in the final period), none of these increases are statistically significant.
Overall, our findings illuminate variation in health outcomes and trajectories among different immigrant groups by world region of origin. Although the exploration of specific mechanisms responsible for such variation is not the primary focus of this paper, they are important to consider. It is likely that some of the diversity can be explained by the existing contexts of migration from different regions of the world, as well as diversity of conditions that immigrants face upon arrival to the U.S. The health of immigrants from different regions of the world may be shaped by geopolitical contexts of international migration and the nature of existing migration streams (Lindstrom and Ramirez, 2010), access to health care and social services (Berk et al., 2000), local and transnational social networks (Viruell-Fuentes, 2007), and experiences based on race and ethnicity (Ryan et al., 2006). Further study of mechanisms responsible for divergent health trajectories among immigrant groups would be a logical next step on the path to understanding diversity within the immigrant population in the U.S.
This investigation is not without limitations. We do not have data on those who remained in each region of origin. Consequently, we cannot assess the extent to which health advantages may be biased by return migration (Riosmena et al., 2013). Research comparing origin and host countries has made great strides in evaluating whether immigrants who migrate are healthier because they represent the most robust inhabitants of their nation or because inhabitants of a given nation are healthier to begin with. This research generally suggests, in the case of Mexico at least, that some part of both of these stories is true. The lack of data on health in regions of origin prohibits us from adjudicating between these explanations in the current study. We are made more confident by the fact that while return migration may lead to overestimates of health advantages, it may also lead to underestimates of health disadvantages. Therefore, the observed differences between immigrants from different regions of origin are likely to remain even if return migration attenuates health advantages among the foreign-relative to native-born.
The data used in this study also do not allow us to differentiate between immigrants based on their documentation status. Unauthorized immigrants comprise an estimated 4% of the U.S. population and certain regional origin groups (for example, migrants from Mexico) are more likely to be undocumented compared to other immigrant subpopulations (Passel and Cohn, 2009). Undocumented immigrants can be expected to have health profiles that are different from those found in the general immigrant population. Undocumented migrants are more likely to face barriers in access to health care, often avoiding health facilities and providers for fear of being denied care (Berk et al., 2000). While the lack of access to health care leaves undocumented migrants with fewer tools available to manage their health, it may also result in them appearing healthier, as access to health care is linked to the likelihood of receiving a medical diagnosis.
Similarly, since the birthplace information in the public use NHIS data files is aggregated to regional level, we cannot differentiate between individual countries within each of the world regions. Existing research (and common sense) suggests that such variation exists among Hispanic (Acevedo-Garcia et al., 2005) and Asian subgroups (Gee et al., 2007). However, less is known about within-group diversity in smaller immigrant subpopulations, such as the immigrants from Africa, Russia and the Middle East. One of the strengths of the current study is inclusion of these often overlooked populations into the larger discussion of immigrant health in the U.S.
Additionally, research on health and illness has begun to question whether one’s own self-rated health is evaluated uniformly across groups (Grol-Prokopczyk et al., 2011; Jyhlä, 2009). Since the data did not allow us to test this possibility, we also included a more objective ( i.e. – diagnosed) health condition. The consistency in results across health outcomes provides additional confidence in our findings and highlights the need for future work to continue investigating similarities and differences in health among immigrants from different world regions of origin.
6. Conclusion
In contrast to assumptions of uniformity across immigrant groups we find that the immigrant health advantage is not present for immigrants from all regions of world origin. We also find that when an advantage is observed, the size of the advantage varies depending on the immigrants’ region of origin. Statistically and substantively meaningful differences between non-Mexican and Mexican immigrants, made evident in analyses using the Mexican-born as the reference category, underlie these variations.
Given that Mexican immigrants tend to display a health advantage on many specific outcomes, it is easy to overlook disadvantages that many immigrants face in the realm of health and healthcare. Focusing on a single, albeit large, region of origin limits our understanding of the diverse health trajectories and unique health needs of other minority populations. The size of these groups is not trivial: immigrants born in Vietnam, China, Korea, India and the Philippines remain among the largest immigrant groups in the U.S., each comprising up to 5% of the total immigrant population. Other immigrant groups, like those born in Africa, while remaining relatively small, have increased significantly in size in the last several years.
Additionally, immigrant populations from different countries of origin are not evenly geographically distributed within the U.S. Thus, looking at smaller immigrant populations might be of practical importance to major receiving areas, as well as emerging immigrant destinations. Studies such as this have special relevance at these local and regional levels, where health policy is often drafted and enacted. If health upon arrival, and, even more importantly, over time varies depending on the region of origin, then broad-based policy efforts are likely to have uneven effects across subgroups of the immigrant population in a given city, county or state. Knowledge of these initial and evolving health profiles can provide insight into how policies might be tailored to successfully achieve goals for all targeted groups.
References
- Acevedo-Garcia D, Soobader MJ, Berkman LF. The differential effect of foreign-born status on low birth weight by race/ethnicity and education. Pediatrics. 2005;115(1):e20–e30. doi: 10.1542/peds.2004-1306. [DOI] [PubMed] [Google Scholar]
- Akresh IR. Dietary assimilation and health among Hispanic immigrants to the United States. J. Health Soc. Behav. 2007;48(4):404–417. doi: 10.1177/002214650704800405. [DOI] [PubMed] [Google Scholar]
- Antecol H, Bedard K. Unhealthy assimilation: why do immigrants converge to American health status levels? Demography. 2006;43(2):337–360. doi: 10.1353/dem.2006.0011. [DOI] [PubMed] [Google Scholar]
- Alcántara C, Molina KM, Kawachi I. Transnational, social and neighborhood ties and smoking among Latino immigrants: does gender matter? Am. J. Public Health. 2015;105(4):741–749. doi: 10.2105/AJPH.2014.301964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, Torres M, Chen C, Meng X. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am. J. Psychiatry. 2008;165(3):356–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berk ML, Schur CL, Chavez LR, Frankel M. Health care use among undocumented Latino immigrants. Health Aff. 2000;19(4):51–64. doi: 10.1377/hlthaff.19.4.51. [DOI] [PubMed] [Google Scholar]
- Borjas G. Assimilation, changes in cohort quality, and the earnings of immigrants. J. Labor Econ. 1985;3:463–489. doi: 10.1086/298373. [DOI] [PubMed] [Google Scholar]
- Bostean G. Does selective migration explain the Hispanic paradox? A comparative analysis of Mexicans in the U.S. and Mexico. J. Immigr. Minor. Health/Cent. Minor. Public Health. 2013;15(3):624–635. doi: 10.1007/s10903-012-9646-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ceballos M. Simulating the effects of acculturation and return migration on the maternal and infant health of Mexican immigrants in the United States: a research note. Demography. 2011;48(2):425–436. doi: 10.1007/s13524-011-0017-4. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control. National Vital Statistics Report. Final Data for 2013. 2015;64(2) 2015. [Google Scholar]
- Cockerham WC. Health lifestyles in Russia. Soc. Sci. Med. 2000;51(9):1313–1324. doi: 10.1016/s0277-9536(00)00094-0. [DOI] [PubMed] [Google Scholar]
- Cunningham SA, Ruben JD, Narayan KMV. Health of foreign-born people in the United States: a review. Health & Place. 2008;14(4):623–635. doi: 10.1016/j.healthplace.2007.12.002. [DOI] [PubMed] [Google Scholar]
- Dallo FJ, Borrell LN. Self-reported diabetes and hypertension among Arab Americans in the United States. Ethn. Dis. 2006;16(3):699. [PubMed] [Google Scholar]
- Dallo FJ, James SA. Acculturation and blood pressure in a community-based sample of Chaldean-American women. J. Immigr. Minor. Health. 2000;2(3):145–153. doi: 10.1023/A:1009560903668. [DOI] [PubMed] [Google Scholar]
- David RJ, Collins JW., Jr Differing birth weight among infants of US-born blacks, African-born blacks, and US-born whites. N. Engl. J. Med. 1997;337(17):1209–1214. doi: 10.1056/NEJM199710233371706. [DOI] [PubMed] [Google Scholar]
- Ferraro KF, Farmer MM, Wybraniec JA. Health trajectories: long-term dynamics among black and white adults. J. Health Soc. Behav. 1997;38(1):38–54. [PubMed] [Google Scholar]
- Forna F, Jamieson DJ, Sanders D, Lindsay MK. Pregnancy outcomes in foreign-born and us-born women. Int. J. Gynaecol. Obstet. 2003;83(3):257–265. doi: 10.1016/s0020-7292(03)00307-2. [DOI] [PubMed] [Google Scholar]
- Frank R, Akresh IR. Social patterning in body mass index (BMI) among contemporary immigrant groups: the emergence of a gradient. Demography. 2013;50(3):993–1012. doi: 10.1007/s13524-012-0174-0. [DOI] [PubMed] [Google Scholar]
- Frisbie WP, Cho YT, Hummer RA. Immigration and the health of Asian and Pacific islander adults in the United States. Am. J. Epidemiol. 2001;153(4):372–380. doi: 10.1093/aje/153.4.372. [DOI] [PubMed] [Google Scholar]
- Fuentes-Afflick E, Hessol NA, Perez-Stable EJ. Maternal Birthplace, Ethnicity, and Low Birth Weight in California. Arch. Pediatr. Adolesc. Med. 1998;152(11):1105–1112. doi: 10.1001/archpedi.152.11.1105. [DOI] [PubMed] [Google Scholar]
- Gee GC, Spenser MS, Chen J, Takeuchi D. A nationwide study of discimination and chronic conditions among Asian Americans. Am. J. Public Heatlh. 2007;97(7):1275–1282. doi: 10.2105/AJPH.2006.091827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grieco EM, Acosta YD, de la Cruz GP, Gambino C, Gryn T, Larsen LJ, Trevelyan EN, Walters NP. The Foreignborn Population in the United States: 2010 in American Community Survey Reports. U.S. Census Bureau; Washington, D.C: 2012. [Google Scholar]
- Grol-Prokopczyk H, Freese J, Hauser RM. Using anchoring vignettes to assess group differences in general self-rated health. J. Health Soc. Behav. 2011;52(2):246–261. doi: 10.1177/0022146510396713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gubernskaya Z. Age at migration and self-rated health trajectories after age 50: understanding the older immigrant health paradox. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2015;70(2):279–290. doi: 10.1093/geronb/gbu049. [DOI] [PubMed] [Google Scholar]
- Hayward MD, Hummer RA, Chiu C, Gonzalez-Gonzalez C, Wong R. Does the Hispanic paradox in US adult mortality extend to disability? Popul. Res. Policy Rev. 2014;33(1):81–96. doi: 10.1007/s11113-013-9312-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton TG, Hummer RA. Immigration and the health of U.S. black adults: does country of origin matter? Soc. Sci. Med. 2011;73(10):1551–1560. doi: 10.1016/j.socscimed.2011.07.026. [DOI] [PubMed] [Google Scholar]
- Hamilton TG, Palermo T, Green T. Health assimilation among hispanic immigrants in the United States: the impact of ignoring arrival-cohort effects. J. Health Soc. Behav. 2015;56(4):460–477. doi: 10.1177/0022146515611179. [DOI] [PubMed] [Google Scholar]
- Hendi AS, Mehta NK, Elo IT. Health among black children by maternal and child nativity. Am. J. Public Health. 2015;105(4):703–710. doi: 10.2105/AJPH.2014.302343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hessol NA, Fuentes-Afflick E. The perinatal advantage of Mexicanorigin Latina women. Ann. Epidemiol. 2000;10(8):516–523. doi: 10.1016/s1047-2797(00)00073-9. [DOI] [PubMed] [Google Scholar]
- Holmes JS, Driscoll AK, Heron M. Mortality among US-born and immigrant Hispanics in the US: effects of nativity, duration of residence, and age at immigration. Int. J. Public Health. 2015;60(5):609–617. doi: 10.1007/s00038-015-0686-7. [DOI] [PubMed] [Google Scholar]
- Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): infant mortality among the Mexican-origin population in the United States. Demography. 2007;44(3):441–457. doi: 10.1353/dem.2007.0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Community studies reporting association between self-rated health and mortality. Res. Aging. 1999;21:392–401. [PubMed] [Google Scholar]
- Idler EL, Kasl SV. Self-ratings of health: do they also predict change in functional ability? J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 1995;50(6):S344–S353. doi: 10.1093/geronb/50b.6.s344. [DOI] [PubMed] [Google Scholar]
- Janevic T, Savitz DA, Janevic M. Maternal education and adverse birth outcomes among immigrant women to the United States from eastern Europe: a test of the healthy migrant hypothesis. Soc. Sci. Med. 1982. 2011;73(3):429–435. doi: 10.1016/j.socscimed.2011.05.041. [DOI] [PubMed] [Google Scholar]
- Jasso G, Massey DS, Rosenzweig MR, Smith JP. Immigrant Health: Selectivity and Acculturation. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. 2004:227–266. [Google Scholar]
- Jyhlä M. What is self-rated health and why does it predict mortality? Toward a unified conceptual model. Soc. Sci. Med. 2009;69(3):307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- Korenbrot CC, Dudley RA, Greene JD. Changes in births to foreign-born women after welfare and immigration policy reforms in California. Matern. Child Health J. 2000;4(4):241–250. doi: 10.1023/a:1026695605457. [DOI] [PubMed] [Google Scholar]
- Lee S, O’Neill AH, Ihara ES, Chae DH. Change in self-reported health status among immigrants in the United States: associations with measures of acculturation. Plos One. 2013;8(10) doi: 10.1371/journal.pone.0076494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindstrom DP, Ramirez AL. Pioneers and followers: migrant selectivity and the development of U.S. migration streams in Latin America. Ann. Am. Acad. Political Soc. Sci. 2010;630(1):53–77. doi: 10.1177/0002716210368103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez L, Peralta CA, Lee A, Al Hazzouri AZ, Haan MN. Impact of acculturation on cardiovascular risk factors among elderly Mexican Americans. Ann. Epidemiol. 2014;24(10):714–719. doi: 10.1016/j.annepidem.2014.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markides KS, Coreil J. The health of Hispanics in the southwestern United States: and epidemiologic paradox. Public Health Rep. 1986;101(3):253–265. [PMC free article] [PubMed] [Google Scholar]
- Martinez JN, Aguayo-Tellez E, Rangel-Gonzalez E. Explaining the Mexican-Americab health paradox using selectivity effects. Int. Migr. Rev. 2014;49(4):879–906. [Google Scholar]
- Orrenius PM, Zavodny M. Do immigrants work in riskier jobs? Demography. 2009;46(3):535–551. doi: 10.1353/dem.0.0064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oza-Frank R, Narayan KMV. Overweight and diabetes prevalence among US immigrants. Am. J. Public Health. 2010;100(4):661–668. doi: 10.2105/AJPH.2008.149492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41(3):385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Passel JS, Cohn D. A Portrait of Unauthorized Immigrants in the United States. Pew Hispanic Center; Washington, DC: 2009. [Google Scholar]
- Powers DA. Paradox revisited: a further investigation of racial/ethnic differences in infant mortality by maternal age. Demography. 2013;50(2):495–520. doi: 10.1007/s13524-012-0152-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pransky G, Moshenberg D, Benjamin K, Portillo S, Thackrey JL, Hill-Fotouhi C. Occupational risks and injuries in non-agricultural immigrant Latino workers. Am. J. Ind. Med. 2002;42(2):117–123. doi: 10.1002/ajim.10092. [DOI] [PubMed] [Google Scholar]
- Qin C, Gould JB. Maternal nativity status and birth outcomes in Asian immigrants. J. Immigr. Minor. Health. 2010;12(5):798–805. doi: 10.1007/s10903-008-9215-6. [DOI] [PubMed] [Google Scholar]
- Read JG, Amick B, Donato KM. Arab immigrants: a new case for ethnicity and health? Soc. Sci. Med. 2005;61(1):77–82. doi: 10.1016/j.socscimed.2004.11.054. [DOI] [PubMed] [Google Scholar]
- Read JG, Emerson MO. Racial context, black immigration and the US black/ white health disparity. Soc. Forces. 2005;84(1):181–199. [Google Scholar]
- Read JG, Reynolds MM. Gender differences in immigrant health: the case of Mexican and Middle Eastern immigrants. J. Health Soc. Behav. 2012;53(1):99–123. doi: 10.1177/0022146511431267. [DOI] [PubMed] [Google Scholar]
- Richardson K, Jatrana S, Tobias M, Blakely T. Migration and Pacific mortality: estimating migration effects on Pacific mortality rates using Bayesian models. Demography. 2013;50(6):2053–2073. doi: 10.1007/s13524-013-0234-0. [DOI] [PubMed] [Google Scholar]
- Riosmena F, Wong R, Palloni A. Migration selection, protection, and acculturation in health: a binational perspective on older adults. Demography. 2013;50(3):1039–1064. doi: 10.1007/s13524-012-0178-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal T. The effect of migration on hypertension and other cardiovascular risk factors: a review. J. Am. Soc. Hypertens. 2014;8(3):171–191. doi: 10.1016/j.jash.2013.12.007. [DOI] [PubMed] [Google Scholar]
- Ryan AM, Gee GC, Laflamme DF. The association between self-reported discrimination, physical health and blood pressure: findings from African-Americans, Black Immigrants, and Latino immigrants in New Hampshire. J. Health Care Poor Underserved. 2006;17(2):116–132. doi: 10.1353/hpu.2006.0092. [DOI] [PubMed] [Google Scholar]
- Scheder JC. A sickly-sweet harvest: farmworker diabetes and social equality. Med. Anthropol. Q. 1988:251–277. [Google Scholar]
- Singh GK, Lin SC. Dramatic increases in obesity and overweight prevalence among Asian subgroups in the United States, 1992–2011. Int. Sch. Res. Notices Prev. Med. 2013 doi: 10.5402/2013/898691. Article ID 898691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Lin SC. Marked ethnic, nativity, and socioeconomic disparities in disability and health insurance among US children and adults: the 2008–2010 American Community Survey. BioMed Res. Int. 2013 doi: 10.1155/2013/627412. Article ID 627412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am. J. Public Health. 2001;91(3):392–399. doi: 10.2105/ajph.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two national data bases. Hum. Biol. 2002;74(1):83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]
- Son J. Are immigrants from Asia healthier than immigrants from other regions?: self-reported health status and functional difficulties of immigrants in the USA. J. Int. Migr. Integr. 2013;14(1):19–38. [Google Scholar]
- U.S. Bureau of the Census. Current Population Survey. U.S. Government Printing Office; Washington, DC: 2013. [Google Scholar]
- Van Hook J, Bean FD, Bachmeier JD, Tucker C. Recent trends in coverage of the Mexican-born population of the United States: results from applying multiple methods across time. Demography. 2014;51(2):699–726. doi: 10.1007/s13524-014-0280-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viruell-Fuentes EA. Beyond acculturation: immigration, discrimination and health research among Mexicans in the United States. Soc. Sci. Med. 2007;65(7):1524–1535. doi: 10.1016/j.socscimed.2007.05.010. [DOI] [PubMed] [Google Scholar]
- Whatley M, Batalova J. Indian Immigrants in the United States. Migration Policy Institute; Washington, D.C: 2013. [Google Scholar]
- Wingate MS, Alexander GR. The healthy migrant theory: variations in pregnancy outcomes among US-born migrants. Soc. Sci. Med. 2006;62(2):491–498. doi: 10.1016/j.socscimed.2005.06.015. [DOI] [PubMed] [Google Scholar]