Abstract
Introduction
Physical exercise after stroke is essential for improving recovery and general health, and reducing future stroke risk. However, people with stroke are not sufficiently active on return to the community after rehabilitation. We developed the Promoting Optimal Physical Exercise for Life (PROPEL) programme, which combines exercise with self-management strategies within rehabilitation to promote ongoing physical activity in the community after rehabilitation. This study aims to evaluate the effect of PROPEL on long-term participation in exercise after discharge from stroke rehabilitation. We hypothesise that individuals who complete PROPEL will be more likely to meet recommended frequency, duration and intensity of exercise compared with individuals who do not complete the programme up to 6 months post discharge from stroke rehabilitation.
Methods and analysis
Individuals undergoing outpatient stroke rehabilitation at one of six hospitals will be recruited (target n=192 total). A stepped-wedge design will be employed; that is, the PROPEL intervention (group exercise plus self-management) will be ‘rolled out’ to each site at a random time within the study period. Prior to roll-out of the PROPEL intervention, sites will complete the control intervention (group aerobic exercise only). Participation in physical activity for 6 months post discharge will be measured via activity and heart rate monitors, and standardised physical activity questionnaire. Adherence to exercise guidelines will be evaluated by (1) number of ‘active minutes’ per week (from the activity monitor), (2) amount of time per week when heart rate is within a target range (ie, 55%–80% of age-predicted maximum) and (3) amount of time per week completing ‘moderate’ or ‘strenuous’ physical activities (from the questionnaire). We will compare the proportion of active and inactive individuals at 6 months post intervention using mixed-model logistic regression, with fixed effects of time and phase and random effect of cluster (site).
Ethics and dissemination
To date, research ethics approval has been received from five of the six sites, with conditional approval granted by the sixth site. Results will be disseminated directly to study participants at the end of the trial, and to other stake holders via publication in a peer-reviewed journal.
Trial registration number
NCT02951338; Pre-results.
Keywords: Stroke, Exercise, Physical Activity, Behaviour Change, Physiotherapy
Strengths and limitations of this study.
This multicentre trial will determine if an exercise and self-management intervention can increase participation in physical activity after stroke rehabilitation.
The novel ‘stepped-wedge’ trial design is suitable given the group-based delivery of the intervention and relatively small number of sites involved.
Participation in physical activity will be determined with three methods: self-report (activity questionnaire), daily heart rate monitoring and daily activity monitoring.
The trial is single-blinded (participants cannot be blinded to intervention allocation), which potentially introduces a source of bias.
Introduction
Background and rationale
People often have low aerobic capacity after stroke,1 2 which can limit the stroke survivors’ ability to complete activities of daily living.1 3 4 Aerobic exercise is beneficial post stroke for improving aerobic capacity,5–7 maintaining or promoting recovery8 and for general health, including reducing risk of another stroke or other cardiovascular events.9 Indeed, aerobic exercise is beneficial and feasible even early after stroke and during routine rehabilitation.6 10 However, due to the brief length of stay in stroke rehabilitation (4–6 weeks), ongoing self-directed physical activity post discharge is necessary to maintain these benefits.
People with stroke do not maintain adequate levels of long-term exercise. Community-living people with stroke walk, on average, 70–5800 steps/day,11 which is less than the 6000 steps/day recommended for people with physical disabilities.12 Data from heart rate monitors revealed that, even when individuals with stroke were active, the activity was not of sufficient intensity for aerobic benefit.13 This chronic inactivity means that gains in aerobic fitness made during rehabilitation will be lost post discharge.14
There is a need to establish strategies to promote long-term uptake of exercise after stroke.15 Most studies aiming to increase self-directed exercise post stroke have been implemented in the community after formal rehabilitation is complete.16 17 While some community-based programmes have reported increased physical activity after the programme,18–20 many people have difficulty accessing community programmes16 and consequently attendance can be low.21 The early recovery period during rehabilitation may be an optimal time to not only deliver fitness programming to increase exercise capacity, but also to shape long-term self-directed exercise behaviour.14 To our knowledge, only one group has studied such a programme during stroke rehabilitation.22 This study found that 67% of those who completed the intervention met exercise recommendations compared with 55% in the control group. However, this study was limited by a non-randomised design, high rates of withdrawal in the intervention group compared with the control group (28% vs 12%) and low rates of compliance with the intervention (<67%). Furthermore, this study included individuals receiving rehabilitation for various conditions and was not focused solely on people with stroke, who have unique challenges to participating in exercise.23
We developed Promoting Optimal Physical Exercise for Life (PROPEL)—a combined group exercise and self-management programme that aims to promote long-term engagement in exercise and physical activity after stroke. Our pilot non-randomised study suggests that those who complete PROPEL are more physically active after discharge from rehabilitation than those who do not (box).24
Box. WHO data set.
Trial registration: clinicaltrials.gov, NCT02951338.
Date of registration: 31 October 2016.
Secondary identification numbers: Not applicable.
Sources of monetary or material support: This study is supported by the Canadian Institutes of Health Research (PJT-148906). AM holds a New Investigator Award from the Canadian Institutes of Health Research (MSH-141983). DB holds a Canada Research Chair. AT is supported by a personnel award from the Heart and Stroke Foundation, Ontario Provincial Office (CS I 7468). The views expressed are not necessarily those of the funders.
Primary sponsor: Avril Mansfield.
Secondary sponsors: Dina Brooks, Ada Tang, Denise Taylor.
Contact for public queries: Avril Mansfield; address: 550 University Ave, Toronto, ON, M5G 2A2; tel: 416-597-3422 ext 7831; e-mail: avril.mansfield@uhn.ca
Contact for scientific queries: Avril Mansfield; address: 550 University Ave, Toronto, ON, M5G 2A2; tel: 416-597-3422 ext 7831; e-mail: avril.mansfield@uhn.ca
Public title: Promoting Optimal Physical Exercise for Life (PROPEL) in people with stroke.
Scientific title: Promoting Optimal Physical Exercise for Life (PROPEL)—aerobic exercise and self-management early after stroke to increase daily physical activity: study protocol for a stepped-wedge randomised trial.
Countries of recruitment: Canada.
Interventions: Group aerobic exercise only (Active Comparator): Supervised group exercise up to three times/week for 6 weeks. A typical exercise session will involve a 3–5 min 'warm-up', 20–30 min of aerobic exercise at a target heart rate determined from a submaximal or maximal aerobic capacity test and a 3–5 min 'cool-down' of low-intensity exercise. The choice of exercise modality for the submaximal test and for training (eg, recumbent stepper, cycle ergometer or treadmill) will be individually prescribed based on patients' sensorimotor recovery, postural control, functional abilities and safety. Heart rate, blood pressure, rate of perceived exertion, workload and duration of training will be documented for each session. These data will be reviewed by the physiotherapist with appropriate progression of the intensity and/or duration of exercise as necessary. Participants may receive general advice to keep physically active after discharge and may receive an individualised home exercise programme, as is currently routine care at all sites. PROPEL programme (experimental): The PROPEL programme involves both group aerobic exercise (as described above) and group discussion aimed at enabling participation in exercise after discharge. Components of the PROPEL programme were developed according to the Transtheoretical Model of health behaviour change and Social Cognitive Theory. In addition to group exercise, participants will attend 1 hour small group discussion sessions once weekly to learn self-management skills for exercise in preparation for discharge from rehabilitation. These discussions include identifying and solving problems around barriers to exercise; understanding personal and general benefits of exercise; exploring appropriate community resources for exercise and finding individualised and realistic strategies for incorporating exercise in a regular routine. Participants will become comfortable with progressing their exercise and will set short-term and long-term goals for engaging in physical activity and exercise after discharge.
Key inclusion and exclusion criteria: Inclusion criteria: Adults with stroke who are referred to the group aerobic exercise or PROPEL programmes as part of their stroke rehabilitation. Exclusion criteria: Language or communication barrier that prevents completion of questionnaires (eg, severe receptive or global aphasia or non-English speaking); cognitive impairment that would prevent participation in unsupervised exercise; attend <50% of group aerobic exercise/PROPEL sessions; and/or attend less than four of the six group discussion sessions (for individuals referred to the PROPEL programme).
Study type: Interventional stepped-wedge cluster randomised trial.
Date of first enrolment: February 2017 (anticipated).
Target sample size: 192.
Recruitment status: Pending: participants are not yet being recruited or enrolled at any site.
Primary outcomes: Number of patients who meet recommended intensity, frequency and duration of physical activity; that is, at least 150 min per week of moderate-to-vigorous intensity exercise. Physical activity will be assessed using a step counter, heart rate monitor and questionnaire for seven continuous days at 1, 4 and 6 months post discharge.
Secondary outcomes: Short Self-efficacy for Exercise Scale; Short Outcome Expectation for Exercise Scale and Barriers to Being Active Quiz.
Objectives
The primary aim of this study is to evaluate the effect of PROPEL delivered during stroke rehabilitation on participation in self-directed exercise after rehabilitation. Our secondary aims are to evaluate the effect of PROPEL on self-efficacy and outcome expectations for exercise, and barriers to exercise. We hypothesise that, compared with those who complete group aerobic exercise (GAE) only, those who complete PROPEL will (1) be more likely to meet the recommended intensity and duration of self-directed physical activity in the community (ie, ≥150 min/week of moderate-intensity exercise25) and (2) report higher self-efficacy and outcome expectations for exercise, and fewer barriers to community activity.
Trial design
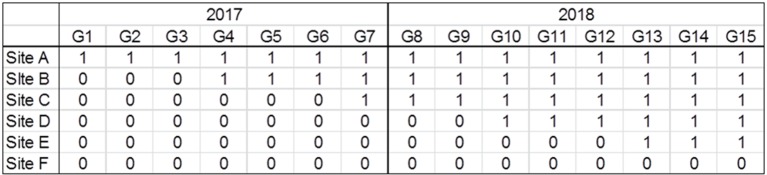
This study involves a single-blind (assessor blinded), continuous recruitment short exposure, stepped-wedge cluster randomised controlled superiority trial (SWT).26 Six sites will be involved in the study; at a randomly determined time within the study period (figure 1), each site will transition from the control intervention (GAE only) to the experimental intervention (PROPEL). New participants will be recruited continuously throughout the study period and will either complete the GAE or PROPEL intervention, depending on which programme that site is administering at the time at which they are admitted to rehabilitation.
Figure 1.
Intervention allocation schedule. G1, G2, and so on are the 6-week long group aerobic exercise (GAE) or Promoting Optimal Physical Exercise for Life (PROPEL) groups. Each site should be able to complete eight groups per year; however, only seven groups will be completed in 2017 to allow for additional time at the start of the year to obtain research ethics approval, inter-institutional agreements and pilot implementation at all sites (see also figure 2). ‘0’ indicates that the site will complete GAE in that time period, whereas ‘1’ indicates that they will complete PROPEL. A simple randomisation procedure will be used to determine the time at which each site transitions from GAE to PROPEL. Sites will be allocated in order by drawing names from a hat; for example, the first site to be drawn will be site A, the second will be site B, and so on.
The group format is essential to PROPEL (see below). In our pilot study,24 there was often a delay to start the group in order to have ≥3 people enrolled. Therefore, a study design whereby individual participants are randomly allocated to either GAE or PROPEL would be problematic as there would be even greater delays in starting the groups since twice as many people would be required to be enrolled in order to run concurrent groups. Likewise, a traditional cluster randomised controlled trial, where sites are randomly assigned to either complete GAE or PROPEL, would not be ideal due to the relatively low number of sites (6), and thus, reduced statistical power.27 Therefore, the SWT is a pragmatic trial design that is suitable for evaluating interventions that are implemented routinely at the level of cluster.26 27 It balances the need for robust evaluation with logistic constraints in programme evaluation, particularly in cases of intersite variability.28 Indeed, previous authors have argued that well-designed and executed SWTs can be as rigorous as traditional cluster randomised trials.26
Methods: participants, interventions and outcomes
Study setting
Participants will be recruited from one of six rehabilitation hospitals in Ontario: (1) Hamilton Health Sciences, Hamilton, Ontario; (2) St. Joseph’s Care Group, Thunder Bay, Ontario; (3) Sunnybrook Health Sciences Centre—St. John’s Rehab, Toronto, Ontario; (4) Toronto Rehabilitation Institute—Rumsey Centre, Toronto, Ontario; (5) Toronto Rehabilitation Institute—University Centre, Toronto, Ontario; and (6) West Park Healthcare Centre, Toronto, Ontario. Each site will be staffed by a research assistant (RA) and a physiotherapist (PT). The RA will be responsible for recruiting participants and collecting data. The PT will administer the interventions.
Eligibility criteria
Individuals who complete either GAE or PROPEL as part of routine care at one of the six sites will be invited to participate in the study. To be eligible for referral to GAE or PROPEL, patients must be admitted to the facility for rehabilitation after a diagnosed stroke and must have sufficient cognitive capacity to understand and follow instructions and to convey adverse symptoms with exercise (eg, pain, excessive exertion). Patients will be excluded from GAE or PROPEL if they have conditions that limit their ability to exercise, including uncontrolled hypertension, uncontrolled diabetes, other cardiovascular morbidity that limits exercise tolerance (eg, heart failure, abnormal blood pressure responses or ST-segment depression >2 mm, symptomatic aortic stenosis or complex arrhythmias), unstable angina, orthostatic blood pressure decrease of >20 mm Hg or musculoskeletal impairments or pain. Additionally, participants will be withdrawn from GAE or PROPEL if significant cardiovascular abnormalities are observed during the submaximal exercise test. We have used these criteria to successfully enrol patients with stroke in aerobic exercise during inpatient rehabilitation with no serious adverse events.10 Referral to the group will be made by the patients’ primary treating PTs, who will document the patients’ verbal consent for treatment, as is usual practice.
Patients will be screened for eligibility for the study within the final 2 weeks of the GAE/PROPEL programmes. Participants will be considered for inclusion in the study if they are referred to the GAE or PROPEL programme as part of their stroke rehabilitation. Participants will be excluded from the study if
they have a language or communication barrier that prevents completion of questionnaires (eg, severe receptive or global aphasia or non-English speaking);
they have cognitive impairment that would prevent participation in unsupervised exercise;
they attend less than nine group exercise sessions;
they attend less than four of the six group discussion sessions (for individuals enrolled in the PROPEL programme).
Communication and cognitive capacity to participate in the study will be determined via consultation with participants’ healthcare team.
Interventions
The interventions will be implemented as part of routine care at all sites according to the schedule outlined in figure 1 (eg, site B is expected to implement GAE in mid-February 2017, and PROPEL in around mid-May 2017). The interventions will supplement, rather than replace, current practice; that is, patients will still complete their regularly scheduled physiotherapy, occupational therapy and speech and language pathology sessions, as required. However, for patients who are enrolled in the GAE or PROPEL interventions, PTs might choose not to complete individualised aerobic exercise during patients’ regularly scheduled physiotherapy sessions as this will be completed as part of GAE/PROPEL, and to spend this time instead focusing on other rehabilitation goals (eg, balance or gait retraining).
Both interventions involve supervised, individualised, GAE 3 days/week for 6 weeks informed by a submaximal or maximal aerobic capacity test. Patients will be referred by their treating PT. The interventions will be delivered in a ‘closed group’ format. That is, participants referred to the programme will be placed on a waiting list until there are a sufficient number of participants to form a group (≥3), and all participants in the group will start and end the programme at the same time. The closed-group format is essential for the PROPEL phase as the education and group discussion topics will be presented in a specific order. An open-group format could be used for GAE; however, this would result in participants in the GAE phase being recruited to the study, on average, sooner post stroke than those in the PROPEL phase.24 Therefore, using a closed-group format for both phases will help to ensure that the mean time post stroke at study enrolment does not differ between the two phases of intervention. Prior to starting the group, participants may complete individualised or open-group aerobic exercise as part of their regular inpatient or outpatient rehabilitation.
PTs at each site will receive training in submaximal aerobic capacity testing for individuals with stroke, exercise prescription and leading the PROPEL programme from the study investigators (ELI, LB, CJD and AT).
Control intervention: GAE
The control intervention will involve GAE only. The intensity and duration of exercise will be determined for each individual patient from the results of a submaximal or maximal aerobic capacity test conducted prior to entry into the programme, and considering patients’ medical history and stroke-related impairments.10 In general, the duration of exercise will be 20–30 min, and the intensity will be 50%–70% of age-predicted maximum heart rate or a rating of 3/10 (‘moderate’) on the Borg category ratio (CR-10) scale.29 The choice of exercise modality for the submaximal test and for training (eg, recumbent stepper, cycle ergometer or treadmill) will be individually prescribed based on patients’ sensorimotor recovery, postural control, functional abilities and safety. Group exercise will be supervised by the PT. Each exercise session will begin with a 3–5 min ‘warm-up’ and end with a 3–5 min ‘cool-down’ of low-intensity exercise. Heart rate, blood pressure, rate of perceived exertion, workload and duration of training will be documented for each session. These data will be reviewed by the PT with appropriate progression of the intensity and/or duration of exercise as necessary.
Patients in the GAE programme may receive general advice to keep physically active after discharge and may receive an individualised home exercise programme, as is currently routine care at all sites.
Experimental intervention: PROPEL
The PROPEL programme,24 involves both GAE and group discussion aimed at enabling participation in exercise after discharge. Components of the PROPEL programme were developed according to the Transtheoretical Model of health behaviour change30 and Social Cognitive Theory.31 Participants will complete group exercise 3 days/week (described above for GAE). Additionally, participants will also attend 1 hour small group discussion sessions once weekly to learn self-management skills for exercise in preparation for discharge from rehabilitation. Specific objectives of the discussion sessions are to (1) increase participant knowledge regarding the benefits of exercise and physical activity after stroke, (2) build participant skill and self-efficacy for exercise and (3) establish a feasible postdischarge exercise plan. Through interactive discussions, individualised problem solving and goal setting, the following topics will be addressed, such that a feasible personal exercise plan is iteratively developed:
risks and benefits of exercise
current guidelines and recommendations for exercise
personal barriers to and preferences for exercise
components of an exercise prescription (ie, frequency, intensity, type and time)
how to monitor exercise intensity (eg, using heart rate and rating of perceived exertion)
how to progress an exercise programme
how to set short-term and long-term goals
strategies to sustain and/or re-engage in exercise.
Additionally, individuals are encouraged to identify and trial appropriate community resources for exercise, and find individualised and realistic strategies for incorporating exercise in a regular routine.
The group format helps to promote vicarious experiences. The PROPEL discussions will be led by the PT; access to a healthcare professional leading the group can increase an individual’s belief about personal skill,32 and support in teaching stroke survivors how to exercise independently, promoting feelings of safety and confidence.33 34
Outcomes
Primary outcomes: physical activity
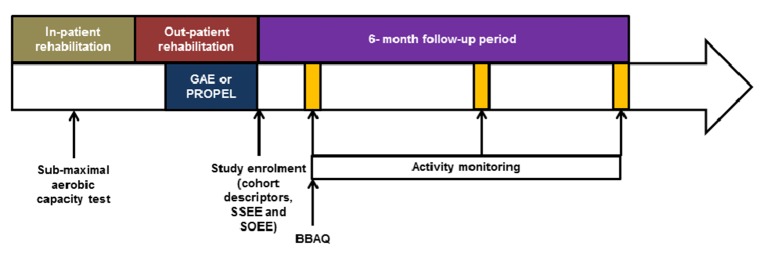
Physical activity will be assessed using a step counter and heart rate monitor for seven continuous days, as well as a physical activity questionnaire at three time points: (1) 1 month, (2) 4 months and (3) 6 months post intervention (figure 2). Because of the limitations of relying on a single method of data collection for physical activity data, combining data from these three sources is recommended.13 23 24 35 Participants will be supplied with a commercial wrist-worn step counter and heart rate monitor (FitBit Charge HR). Our pilot data suggest that this device provides reasonably accurate measures of walking activity and heart rate among individuals with stroke (unpublished data). Individuals who typically use a rollator for ambulation may also be provided with an activity monitor to be worn at the ankle (FitBit One), which would be more accurate for measuring walking activity than a wrist-worn device for these individuals.36 The devices will be configured to not provide participants with information regarding step counts and heart rate. The devices will be mailed to participants with a postage-paid return envelope. Participants will be instructed to wear the device at all times (except when bathing) for 7 days continuously.
Figure 2.
Hypothetical timeline for one participant. The exact timing of inpatient and outpatient rehabilitation will vary for each participant. The submaximal aerobic capacity test is completed during inpatient rehabilitation. After this point, the participant could participate in individual or open-group aerobic exercise during inpatient and outpatient rehabilitation (while waiting to be enrolled in the study intervention). The closed-group study intervention (group aerobic exercise (GAE) only or Promoting Optimal Physical Exercise for Life (PROPEL)) will likely start during outpatient rehabilitation, though some patients may start during inpatient rehabilitation. The participant will be enrolled in the study at the end of the study intervention, at which point cohort descriptors, the Short Self-Efficacy for Exercise (SSEE) scale and the Short Outcome Expectations for Exercise (SOEE) scale, will be collected. Activity monitoring will be conducted for 7 days continuously at three time points: (1) 1 month, (2) 4 months and (3) and 6 months after the end of the study intervention. The Barriers to Being Active Quiz (BBAQ) will be conducted at the 1-month postintervention time point.
The Physical Activity Scale for Individuals with Physical Disabilities (PASIPD)37 will be conducted by telephone with a blinded RA at the end of the 7-day monitoring period. The PASIPD is a 13-item questionnaire in which participants are asked to indicate the frequency and duration of recreational, household and occupational physical activities completed in the previous seven days. The PASID has been validated within a group of individuals with various physical disabilities, including individuals with stroke, showing good test–retest reliability (ρ=0.77) and criterion validity compared with accelerometer-based activity monitoring (ρ=0.30).38
We will use the step activity, heart rate and questionnaire data to determine if participants meet the recommended intensity and duration of physical activity in the community; that is, at least 150 min per week of moderate–vigorous intensity exercise.25 Participants will be deemed to meet the recommendations within a given week if they meet at least two of three criteria: (1) record at least 150 ‘active minutes’ (from the step activity monitor), (2) record at least 150 min of heart rate between 55% and 80% of age-predicted maximum9 and/or (3) report at least 150 min of moderate and/or vigorous intensity activity on the PASIPD.
Secondary outcomes: self-efficacy and outcome expectations for exercise, and barriers to activity
Exercise self-efficacy will be assessed using the Short Self-Efficacy for Exercise (SSEE) scale.39 The SSEE is a four-item questionnaire where participants are required to rate their confidence exercising through pain and fatigue, and when alone and depressed on a five-point scale. The Short Outcome Expectation for Exercise (SOEE) scale39 will be used to assess beliefs and attitudes related to exercise. The SOEE is a five-item questionnaire where participants are asked to rate their beliefs regarding the benefits of exercise on a five-point scale. The SSEE and SOEE will be assessed at enrolment into the study. The SSEE and SOEE have been shown to be valid and reliable among individuals with chronic stroke.39
Perceived barriers to physical activity will be assessed 1 month post intervention with the Barriers to Being Active Quiz (BBAQ).23 40 41 The BBAQ has previously been used to evaluate barriers to exercise among individuals with stroke.23 The BBAQ is a 21-item scale where individuals are required to indicate how likely they are to make specific statements regarding barriers to exercise, for example, ‘I’m getting older so exercise can be risky’.40 Items on seven categories of barriers are included in the questionnaire: lack of time, social influence, lack of energy, lack of willpower, fear of injury, lack of skill and lack of resources. Each individual item is scored from 0 to 3 and scores for each barrier category are the sum of the scores for the three items in that category. Participants are considered to have a ‘significant’ barrier to being active if the score for a category is ≥5.23 The average number of significant barriers per participant will be calculated. The BBAQ has good internal consistency among older adults (Cronbach’s α=0.87).42
Cohort descriptors
The following information will be obtained from chart review in order to characterise individuals who participate in the study: age, sex, time post stroke (at enrolment into the study), lesion location, mobility status and medical conditions/history. The National Institutes of Health Stroke Scale (NIH-SS),43 the Chedoke-McMaster Stroke Assessment (CMSA)44 foot and leg scores and the Montreal Cognitive Assessment (MOCA)45 will be administered at enrolment into the study by the RA or study PT; however, if these measures were conducted as part of clinical care within 1 week of study enrolment, the scores will be extracted from the hospital charts to minimise participant burden. The NIH-SS is an 11-item scale that provides a gross measure of the effects and severity of stroke. The NIH-SS has good intra-rater (ICCs=0.93) and inter-rater (ICCs=0.95) reliability.46 The CMSA assigns a score according to the level of motor recovery in the foot and leg and is frequently used to evaluate level of motor recovery post stroke in clinical settings. The CMSA foot and leg scores have good intra-rater (ICCs=0.94–0.98) and inter-rater (ICCs=0.85–0.96) reliability.44 The MOCA45 is a paper-based test that can be used to screen for mild cognitive impairment; patients are scored on visuospatial and executive function, naming, memory, attention, language, abstraction, delayed recall and orientation.
We will document the frequency, intensity and duration of exercise during inpatient and outpatient rehabilitation by chart review. We will also document details of any home exercise programme or general advice to be physically active that participants receive (outside of the PROPEL intervention). Participants will complete a questionnaire at baseline that asks about their social supports, employment, familial responsibilities, living situation and so on, which are factors that could influence participation in physical activity. Many of these questions have been adapted from the Canadian Longitudinal Study on Aging.47 Some questions will be repeated at the 6-month postdischarge time point to account for lifestyle changes since discharge from rehabilitation. Premorbid exercise behaviour will be evaluated with the Schmidt retrospective physical activity scale.48 This scale shows good agreement with previously completed questionnaires regarding physical activity.48 We will use this scale to estimate participants’ average amount of time (hours/day) prior to their strokes spent in sedentary activities (eg, watching television, sedentary occupational activity) and in physical recreational activity or exercise.
Sample size
We expect that approximately 25% of people who complete GAE49 and 50% of individuals who complete PROPEL24 will be classified as ‘active’. A sample of 96 per phase will provide 80% power to detect a 25%–50% difference at alpha of 0.05 for the six sites taking into account an intracluster correlation of 0.05.50 The sample size calculation was run using PASS V.12 (Hintze, J, 2014, NCSS, Kaysville, Utah, USA). We will aim to recruit 120 participants total per phase to account for a conservative 20% drop-out rate.
Recruitment
There are approximately 710 admissions annually to outpatient stroke rehabilitation at all sites combined. We conservatively estimate that 40% of these individuals will be eligible for the study and, of these, 50% will consent to participate. Thus, we expect to recruit ~140 participants annually to meet the target sample size with ~2 years of recruiting. Target sample sizes for each site are Hamilton Health Sciences, 24; St Joseph’s Care Group, 24; Sunnybrook Research Institute—St John’s Rehab, 60; Toronto Rehabilitation Institute—Rumsey Centre, 58; Toronto Rehabilitation Institute—University Centre, 58; and West Park Healthcare Centre, 60. To encourage recruitment to the study, participants will receive a gift card ($C30 value) as a modest incentive to participate.
In order to generate a Consolidated Standards of Reporting Trials flow diagram for participant recruiting,51 RA will count the number of individuals who are admitted to the outpatient stroke programme and, of these, the number who are referred to the GAE or PROPEL programme. The RA will also maintain documentation related to screening and enrolment of potential participants. Identifying or health-related information will not be documented for individuals who do not consent to participate in the study.
Methods: assignment of interventions
Intervention allocation
The time at which each site transitions from GAE to PROPEL will be determined by drawing site names at random (figure 1). One site will implement PROPEL at the start of the study period, whereas one site will never transition to PROPEL; this will help to ensure blinding of assessors (see 'Blinding'). The site that does not transition to PROPEL during the study period will be offered training in PROPEL at the end of the study period. Intervention allocation will be performed at the start of the study period by the principal investigator, who will not be directly involved in recruiting or data collection. The site leads and PTs at each site will be informed of the transition to PROPEL approximately 3 months prior to the transition to allow for sufficient time for training and planning.
Blinding
Participants cannot be blinded to intervention allocation, although they will not be aware of the existence of another intervention arm. Assessors (RA at each site) who collect data, including administering questionnaires, will be unaware of the time at which the site transitions from GAE to PROPEL. While it is more likely that a given site will be allocated to GAE at the start of the study period, and to PROPEL at the end of the study, inclusion of two sites that always complete either GAE or PROPEL will create uncertainty in intervention allocation at all time points. Furthermore, using objective methods to collect data pertaining to the primary outcome (ie, heart rate and activity monitor) helps to protect against bias if assessors inadvertently become unblinded.
Methods: data collection, management and analysis
Data collection methods
Data will be collected primarily by the RA either directly from the participant or by chart review (see table 1 for further details). RAs at each site will receive training regarding data collection from the principal investigator (AM) and central study coordinator (AA). Questionnaires will be completed via in-person interview at enrolment and over the telephone at the follow-up time points. Activity monitors will be sent to participants and returned to the site via mail. Participants will be contacted via telephone just prior to mailing the activity monitors to remind them that they will be receiving the activity monitors and to ensure that they will be home to receive them (eg, that they are not planning to be on vacation at that time).
Table 1.
Overview of data collection time points
| Study enrolment | Post discharge | |||
| 1 month | 4 months | 6 months | ||
| Cohort descriptors | ||||
| Chart review form | RA-CR | |||
| NIH-SS | RA-P | |||
| CMSA | RA/PT-CR/P | |||
| MOCA | RA-P | |||
| Baseline questionnaire | RA-P | |||
| Six-month follow-up questionnaire | RA-P | |||
| Schmidt questionnaire | RA-P | |||
| Primary outcomes | ||||
| FitBit activity monitoring* | RA-P | RA-P | RA-P | |
| FitBit heart rate data* | RA-P | RA-P | RA-P | |
| PASIPD† | RA-P | RA-P | RA-P | |
| Secondary outcomes | ||||
| SSEE | RA-P | |||
| SOEE | RA-P | |||
| BBAQ | RA-P | |||
*Activity and heart rate monitoring for 7 days continuously.
†PASIPD questionnaire should be done at the end of the 7-day activity/heart rate monitoring period.
BBAQ, Barriers to Being Active Quiz; CMSA, Chedoke-McMaster Stroke Assessment; MOCA, Montreal Cognitive Assessment; NIH-SS, National Institutes of Health Stroke Scale; PASIPD, Physical Activity Scale for Individuals with Physical Disabilities; PT-CR, data collected by the physiotherapist by chart review; PT-P, data collected by the physiotherapist directly from the participant; RA-CR, data collected by the research assistant from chart review; RA-P, data collected by research assistant directly from the participant; SOEE, Short Outcome Expectations for Exercise; SSEE, Short Self-Efficacy for Exercise.
In order to avoid losing participants to follow-up, we will request contact information of a friend or family member. Participants who provide consent for us to contact their friends or family members will be provided with a contact form at the time when written consent is obtained and will be asked to return the form at the next visit or by mail (a stamped self-addressed envelope will be provided). This information will only be used to obtain information about the whereabouts of a research participant if we are unable to contact them after multiple attempts. Participants will primarily be contacted by telephone throughout the study, unless otherwise requested. Each time they are contacted, participants will be told when they should next expect to hear from the RA and will be asked to inform the RA of upcoming limited availability (eg, due to vacation or scheduled surgery). A letter will be mailed to participants who are unable to be reached: (1) because his/her telephone number is out of service or (2) five attempts have been made to telephone the participant over the course of 2 weeks (with at least two voicemail messages for participants who have voicemail and have provided consent for us to leave voicemail). In the latter case, telephone calls will be placed at varying times of the day in an attempt to reach participants who are unavailable at the same time each day due to regular appointments. The letter will request that participants contact the RA. If the RA does not hear from the participant 2 weeks after the letter was mailed, the RA will contact the alternative contact.
Data management
Each activity monitor will be linked to an anonymous account and activity monitor data will be stored on the manufacturer’s servers linked to these anonymous accounts. We will document internally which participants’ data are associated with which accounts; therefore, there will be no information about study participants (eg, name, age, study ID number) stored on the manufacturer’s servers. Activity data will be downloaded from the manufacturer’s servers as soon as possible after collection. All other electronic data will be stored at each site on secure institutional servers. Files containing patient names and contact information will be password protected and stored separately from other data. Hard copies of files containing deidentified data will be stored in locked cabinets and/or in offices that are locked when not occupied. Consent forms will be stored in locked cabinets/offices separately from other data. Only those individuals who require access to the data for the purpose of this study will be provided with the password to the file containing identifiers and/or the keys to the locked cabinet/office. Deidentified electronic data will be transferred to the main site (Sunnybrook Research Institute) using secure file transfer protocols.
Statistical analysis
We will compare cohort descriptors between the two phases (GAE and PROPEL) using t-tests, Mann-Whitney U tests or χ2 tests, as appropriate. If phases significantly differ at baseline on cohort descriptors, these measures may be used as covariates in the analysis. To test our primary hypothesis, we will compare the proportion of active and inactive individuals at the final assessment point (6 months post intervention) using mixed-model logistic regression, with fixed effects of time and phase and random effect of cluster (site).52 We will also examine between-phase differences in physical activity at the 1-month and 4-month time points, which could reveal short-term benefits of PROPEL, even if there are no differences at 6 months. A similar mixed-model analysis of variance will be used to compare SSEE, SOEE and BBAQ scores between programmes to test the secondary hypotheses. Only individuals who complete at least a minimum amount of the intervention will be included in the study; therefore, analysis will necessarily be ‘per protocol’. All recruited participants who comply with data collection will be included in the analysis; participants with missing data for one time point will be excluded from analysis of that variable for that time point.
Methods: monitoring
Data monitoring
There is no data monitoring committee for this study as the safety of aerobic exercise has already been established for this population,6 10 and the additional risk of the discussion components of the PROPEL programme and other study components (eg, questionnaires or activity monitoring) is minimal (see 'Potential harms and auditing'). Adverse events that meet all three of the following criteria will be reported immediately to the local research ethics board(s), as is routine practice: (1) unexpected in terms of nature, severity or frequency; (2) related or possibly related to participation in the research and (3) suggests a potential increase in risk of harm to research participants or to others. All adverse events will be collated and evaluated biannually by the principal investigator (AM).
There is no plan for any interim analysis; interim analysis is not feasible with an SWT design due to the fact that the experimental intervention is ‘rolled out’ gradually to each site, which means that the number of participants per phase will be uneven until the end of the trial. The trial will be stopped when one of the following criteria is met: (1) we have recruited at least 120 participants per phase, (2) 6-month follow-up data are available for at least 96 participants per phase or (3) all site investigators (AM, DB, AT and DT) agree that continuing the trial will not be feasible (eg, due to lower-than-expected recruiting and lack of funding to continue the trial).
Potential harms and auditing
Sites will implement two interventions as part of routine care (GAE or PROPEL). Some aerobic exercise is currently conducted at all sites, but might not be implemented in the systematic manner required for this study. However, aerobic exercise is recommended as part of stroke rehabilitation within the Canadian Stroke Best Practice Recommendations.53 Furthermore, with appropriate screening and prescription, aerobic exercise is safe and feasible early after stroke.10 Treating PTs will screen patients, with appropriate consultation with the interprofessional team, and provide the exercise prescription following established guidelines for aerobic exercise after stroke,54 prior to referring them to GAE or PROPEL. Heart rate and blood pressure will be measured at rest at the start of each intervention session to obtain a baseline measure of cardiovascular function. The interventions will be supervised by a trained registered PT, who will continue to monitor patients’ response to exercise and may choose to adjust the intensity or duration of exercise to minimise risk to participants.
The Canadian Stroke Best Practice Recommendations also recommend including a plan to enable patients to continue to exercise post discharge, including addressing barriers to physical activity.53 However, the specific education, self-management and problem-solving components of the PROPEL programme are not part of routine care at all sites. The additional risk to participants in completing this component of the PROPEL programme is minimal. Participants can opt out of any part of the discussion if they feel uncomfortable.
The additional measures conducted as part of the study pose minimal risk to participants. The CMSA, NIH-SS and MOCA are frequently conducted as part of clinical care in stroke rehabilitation. Other measures are questionnaires which ask routine questions about physical activity behaviour and lifestyle. Despite the minimal risk involved in these measures, participants will be reminded that they can opt out of any testing and/or decline to answer any of the questions in the questionnaires. The activity monitoring also poses minimal risk to participants; the devices are available commercially and are worn daily by millions of individuals around the world. Participants may develop skin irritation from wearing the device daily; they will be instructed to remove the device if this occurs. Participants may feel burdened by donning and doffing the activity monitors each day.
The study PT will document any adverse events that occur during the interventions; the RA will document adverse events for participants who enrol in the study during the follow-up period.
Ethics and dissemination
Research ethics approval
Research ethics approval has been received by the Research Ethics Boards of Sunnybrook Research Institute (study ID: 472–2016, approved 31 January 2017), the University Health Network (study ID: 16–5916, approved 14 November 2016), which covers two sites (Toronto Rehabilitation Institute—University Centre, and Toronto Rehabilitation Institute—Rumsey Centre), St. Joseph’s Care Group (study ID: 2016011, approved 13 February 2017) and Hamilton Health Sciences (study ID: 2274, approved 6 April 2017). Additionally, conditional approval has been granted by the Joint West Park Healthcare Centre—Toronto Central CCAC—Toronto Grace Health Centre Research Ethics Board, pending some clarifications in the protocol and minor site-specific edits to the consent documents (conditional approval: 20 April 2017). Due to one investigator’s affiliation, research ethics approval was also received from Thunder Bay Regional Health Sciences Centre (study ID: 2016139, approved 4 January 2017), although no recruiting or data collection will occur at this site.
Protocol amendments
Substantive changes to the design or conduct of the study will require a formal amendment to the study protocol. Such substantive amendments will be agreed on by the site investigators (AM, DB, AT and DT) and will be approved by the local Research Ethics Boards prior to implementation locally. Minor administrative changes to study documents (eg, correcting a typographical error or clarifying a questionnaire item) may also be implemented, with the Research Ethics Boards notified of the changes.
Consent
Potential participants will be assessed for eligibility by the study PT within the final 2 weeks of the patients’ participation in the GAE/PROPEL programmes. The study PT, who is in the patients’ circle of care, will ask eligible patients if they are interested in speaking with the RA about participating in the study. The RA will discuss the study at a time that is convenient for interested individuals. She/He will describe the study, as outlined in the consent form (see online supplementary appendix) and will answer any questions the patient may have about the study. The patient will be provided with a copy of the consent form and will be invited to discuss the study with friends or family members, and/or to take some time to think about being involved in the study. If a patient indicates that she/he would like to participate in the study, she/he will be asked to sign the consent form. At that time, the RA will arrange a time that is convenient for the participant to collect baseline data (see 'Cohort descriptors'). We will assume that patients who do not provide consent to the study within 2 weeks after they finish the GAE/PROPEL programme are not interested in participating in the study.
bmjopen-2017-015843supp001.pdf (228.5KB, pdf)
Confidentiality
The study PT will run the GAE and PROPEL interventions as part of routine care at each site. Patients who are referred to GAE or PROPEL may decline participation in the study. Therefore, individuals who do not consent to the study may participate in GAE or PROPEL. The study PT will be an individual who also has a role in clinical care on the stroke programme at the site and, therefore, will already be part of the circle of care. The study PT will not have a role in recruiting participants into the study, other than to introduce the study and, if interested, introduce the RA to potential participants.
Identifiable information (participant names and contact information) will be stored separately from health information and study data (see also 'Data management') in a password-protected file, with the password only known to those individuals who are responsible for data collection. A participant ID number will be used to link identifiable information with health information and study data. The link between the participant ID number and name will be destroyed after data have been collected and verified. Deidentified data will be kept in a secure and confidential location for 10 years.
Access to data
The principal investigator (AM) and biostatistician (AK) will have access to the full data set. The site investigators will have access to data collected locally. A study co-investigator or collaborator may be granted access to the full data set for secondary analysis with approval of all site investigators (AM, DB, AT and DT) and the coordinating institution (Sunnybrook Research Institute).
Ancillary and post-trial care
Each site will be responsible for providing out-of-pocket expenses to ensure that a participant receives immediate medical care in the event that the participant experiences an adverse health event (eg, injury) as a result of participation in the study.
Dissemination policy
Study participants will receive a letter of appreciation at the end of the study, which may include a very brief summary of the study results. Study results will be disseminated to others via publication in a peer-reviewed journal. We will aim to submit a paper describing analysis of the primary and secondary outcomes within 6 months of completing data collection. All individuals who meet the International Committee of Medical Journal Editors criteria for authorship will be included as authors on any publications arising from this work. There is no current plan to make the participant-level data set available publicly; however, the data set may be made available in future via a Data Access Committee, if such a committee is established by the coordinating institution.
Study strengths and limitations
We have adopted an ‘integrated knowledge translation’ approach, whereby knowledge users (rehabilitation managers and PTs) have been involved in the study from conception. The interventions are being implemented as part of routine care at each site. This also helps to increase the likelihood that the interventions will continue as part of routine care beyond the end of the study compared with implementing the interventions for study participants only.
The novel ‘stepped-wedge’ trial design is appropriate for evaluating the group-based PROPEL intervention as it is ‘rolled out’ as part of routine practice to each site.27 However, it is possible that factors that change over time will influence the study results. For example, stroke rehabilitation delivery in Ontario is supported by the Ministry of Health and Long-Term Care through the Ontario Health Insurance Program. During the course of the study, it is possible that the Ministry will dictate changes to care delivery, such as changes to lengths of stay. However, ‘vertical’ comparisons between sites can be made at any point in time to account for such secular trends.52 55 An alternative approach would be to have some sites start with the PROPEL intervention and transition to GAE; however, there would be a risk of contamination as staff administering the GAE would have been trained in PROPEL, which might influence how they treat their patients.26 56
Participants in the PROPEL phase will have one extra hour per week of interaction with the PT and with other participants in the group. It is possible that this extra attention/interaction alone, rather than the content of the PROPEL discussions, will influence the study results. We opted to not add an attention control activity to the GAE phase (eg, group discussion on a topic unrelated to physical activity) based on feedback from stakeholders. We designed the GAE phase to resemble clinical practice as closely as possible, while still maintaining controls and standardisation necessary for a research study. An unrelated discussion group would be contrived for the purpose of the study and would not reflect clinical practice.
This large multisite trial will determine if a simple clinical intervention, delivered during stroke rehabilitation, can increase participation in physical activity after discharge. This work addresses methodological limitations of studies aiming to increase exercise participation post-stroke16 17 by (1) basing the intervention on principles of behaviour modification, (2) using objective measures of exercise participation and (3) evaluating long-term self-directed exercise (ie, 6 months post intervention). If the study results are positive, translation of this programme into practice has the potential to reduce healthcare costs (by reducing risk of cardiovascular events) and increase independence for stroke survivors.
Supplementary Material
Footnotes
Contributors: AM conceived of the study and is the grant holder. AM, DB, AT and DT will lead implementation of the study at each site, with assistance from ELI, LB, RF, EF, KL and CD. ELI, LB and CD developed the intervention. AK provided statistical expertise and will conduct the primary statistical analysis. All authors contributed to refining the study protocol and approved the final manuscript.
Funding: This study was supported by the Canadian Institutes of Health Research (PJT148906).
Disclaimer: The funding sources had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data or decision to submit results.
Competing interests: AM holds a New Investigator Award from the Canadian Institutes of Health Research (MSH141983). DB holds a Canada Research Chair. AT is supported by a personnel award from the Heart and Stroke Foundation, Ontario Provincial Office (CS I 7468).
Ethics approval: Research Ethics Board of the University Health Network.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Tang A, Sibley KM, Thomas SG, et al. . Maximal exercise test results in subacute stroke. Arch Phys Med Rehabil 2006;87:1100–5. 10.1016/j.apmr.2006.04.016 [DOI] [PubMed] [Google Scholar]
- 2. Brooks D, Tang A, Sibley KM, et al. . Profile of patients at admission into an inpatient stroke rehabilitation programme: cardiorespiratory fitness and functional characteristics. Physiother Can 2008;60:171–9. 10.3138/physio.60.2.171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mackay-Lyons MJ, Makrides L. Exercise capacity early after stroke. Arch Phys Med Rehabil 2002;83:1697–702. 10.1053/apmr.2002.36395 [DOI] [PubMed] [Google Scholar]
- 4. Rimmer JH, Wang E. Aerobic exercise training in stroke survivors. Top Stroke Rehabil 2005;12:17–30. 10.1310/L6HG-8X8N-QC9Q-HHM8 [DOI] [PubMed] [Google Scholar]
- 5. Tang A, Marzolini S, Oh P, et al. . Feasibility and effects of adapted cardiac rehabilitation after stroke: a prospective trial. BMC Neurol 2010;10:40 10.1186/1471-2377-10-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tang A, Sibley KM, Thomas SG, et al. . Effects of an aerobic exercise program on aerobic capacity, spatiotemporal gait parameters, and functional capacity in subacute stroke. Neurorehabil Neural Repair 2009;23:389–97. 10.1177/1545968308326426 [DOI] [PubMed] [Google Scholar]
- 7. Stoller O, de Bruin ED, Knols RH, et al. . Effects of cardiovascular exercise early after stroke: systematic review and meta-analysis. BMC Neurol 2012;12:45 10.1186/1471-2377-12-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Saunders DH, Sanderson M, Brazzelli M, et al. . Physical fitness training for stroke patients. Cochrane Database Syst Rev 2013;10:CD003316 10.1002/14651858.CD003316.pub5 [DOI] [PubMed] [Google Scholar]
- 9. Billinger SA, Arena R, Bernhardt J, et al. . Physical activity and exercise recommendations for stroke survivors: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014;45:2532–53. 10.1161/STR.0000000000000022 [DOI] [PubMed] [Google Scholar]
- 10. Biasin L, Sage MD, Brunton K, et al. . Integrating aerobic training within subacute stroke rehabilitation: a feasibility study. Phys Ther 2014;94:1796–806. 10.2522/ptj.20130404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Michael KM, Allen JK, Macko RF. Reduced ambulatory activity after stroke: the role of balance, gait, and cardiovascular fitness. Arch Phys Med Rehabil 2005;86:1552–6. 10.1016/j.apmr.2004.12.026 [DOI] [PubMed] [Google Scholar]
- 12. Tudor-Locke C, Craig CL, Aoyagi Y, et al. . How many steps/day are enough? for older adults and special populations. Int J Behav Nutr Phys Act 2011;8:80 10.1186/1479-5868-8-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Baert I, Feys H, Daly D, et al. . Are patients 1 year post-stroke active enough to improve their physical health? Disabil Rehabil 2012;34:574–80. 10.3109/09638288.2011.613513 [DOI] [PubMed] [Google Scholar]
- 14. Morris JH, Williams B. Optimising long-term participation in physical activities after stroke: exploring new ways of working for physiotherapists. Physiotherapy 2009;95:227–33. 10.1016/j.physio.2008.11.006 [DOI] [PubMed] [Google Scholar]
- 15. Rosenberg DE, Bombardier CH, Hoffman JM, et al. . Physical activity among persons aging with mobility disabilities: shaping a research agenda. J Aging Res 2011;2011:1–16. 10.4061/2011/708510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Jones TM, Dean CM, Hush JM, et al. . A systematic review of the efficacy of self-management programs for increasing physical activity in community-dwelling adults with acquired brain injury (ABI). Syst Rev 2015;4:51 10.1186/s13643-015-0039-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Morris JH, Macgillivray S, McFarlane S. Interventions to promote long-term participation in physical activity after stroke: a systematic review of the literature. Arch Phys Med Rehabil 2014;95:956–67. 10.1016/j.apmr.2013.12.016 [DOI] [PubMed] [Google Scholar]
- 18. Kim H, Kim O. [The lifestyle modification coaching program for secondary stroke prevention]. J Korean Acad Nurs 2013;43:331–40. 10.4040/jkan.2013.43.3.331 [DOI] [PubMed] [Google Scholar]
- 19. Damush TM, Ofner S, Yu Z, et al. . Implementation of a stroke self-management program: a randomized controlled pilot study of veterans with stroke. Transl Behav Med 2011;1:561–72. 10.1007/s13142-011-0070-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gillham S, Endacott R. Impact of enhanced secondary prevention on health behaviour in patients following minor stroke and transient ischaemic attack: a randomized controlled trial. Clin Rehabil 2010;24:822–30. 10.1177/0269215510367970 [DOI] [PubMed] [Google Scholar]
- 21. Huijbregts MP, Myers AM, Streiner D, et al. . Implementation, process, and preliminary outcome evaluation of two community programs for persons with stroke and their care partners. Top Stroke Rehabil 2008;15:503–20. 10.1310/tsr1505-503 [DOI] [PubMed] [Google Scholar]
- 22. van der Ploeg HP, Streppel KR, van der Beek AJ, et al. . Successfully improving physical activity behavior after rehabilitation. Am J Health Promot 2007;21:153–9. 10.4278/0890-1171-21.3.153 [DOI] [PubMed] [Google Scholar]
- 23. Zalewski KR, Dvorak L. Barriers to physical activity between adults with stroke and their care partners. Top Stroke Rehabil 2011;18(Suppl 1):666–75. 10.1310/tsr18s01-666 [DOI] [PubMed] [Google Scholar]
- 24. Mansfield A, Knorr S, Poon V, et al. . Promoting optimal physical exercise for life: an exercise and Self-Management Program to encourage participation in physical activity after Discharge from Stroke Rehabilitation-A Feasibility Study. Stroke Res Treat 2016;2016:9476541 10.1155/2016/9476541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Garber CE, Blissmer B, Deschenes MR, et al. . American College of Sports Medicine position stand. quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 2011;43:1334–59. 10.1249/MSS.0b013e318213fefb [DOI] [PubMed] [Google Scholar]
- 26. Copas AJ, Lewis JJ, Thompson JA, et al. . Designing a stepped wedge trial: three main designs, carry-over effects and randomisation approaches. Trials 2015;16:352 10.1186/s13063-015-0842-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mdege ND, Man MS, Taylor Nee Brown CA, et al. . Systematic review of stepped wedge cluster randomized trials shows that design is particularly used to evaluate interventions during routine implementation. J Clin Epidemiol 2011;64:936–48. 10.1016/j.jclinepi.2010.12.003 [DOI] [PubMed] [Google Scholar]
- 28. Hemming K, Haines TP, Chilton PJ, et al. . The stepped wedge cluster randomised trial: rationale, design, analysis, and reporting. BMJ 2015;350:h391 10.1136/bmj.h391 [DOI] [PubMed] [Google Scholar]
- 29. Borg GA. Psychophysical bases of perceived exertion. Med Sci Sports Exerc 1982;14:377???381–81. 10.1249/00005768-198205000-00012 [DOI] [PubMed] [Google Scholar]
- 30. Prochaska JO, DiClemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy: Theory, Research & Practice 1982;19:276–88. 10.1037/h0088437 [DOI] [Google Scholar]
- 31. Bandura A. Health promotion by social cognitive means. Health Educ Behav 2004;31:143–64. 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- 32. Bandura A. Self efficacy: The exercise of control. New York: W.H. Freeman, 1997. [Google Scholar]
- 33. Kinne S, Patrick DL, Maher EJ. Correlates of exercise maintenance among people with mobility impairments. Disabil Rehabil 1999;21:15–22. 10.1080/096382899298052 [DOI] [PubMed] [Google Scholar]
- 34. Reed M, Harrington R, Duggan A, et al. . Meeting stroke survivors' perceived needs: a qualitative study of a community-based exercise and education scheme. Clin Rehabil 2010;24:16–25. 10.1177/0269215509347433 [DOI] [PubMed] [Google Scholar]
- 35. Resnick B, Michael K, Shaughnessy M, et al. . Inflated perceptions of physical activity after stroke: pairing self-report with physiologic measures. J Phys Act Health 2008;5:308–18. 10.1123/jpah.5.2.308 [DOI] [PubMed] [Google Scholar]
- 36. Klassen TD, Simpson LA, Lim SB, et al. . "Stepping up" activity poststroke: ankle-positioned accelerometer can accurately record Steps During Slow Walking. Phys Ther 2016;96:355–60. 10.2522/ptj.20140611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Washburn RA, Zhu W, McAuley E, et al. . The physical activity scale for individuals with physical disabilities: development and evaluation. Arch Phys Med Rehabil 2002;83:193–200. 10.1053/apmr.2002.27467 [DOI] [PubMed] [Google Scholar]
- 38. van der Ploeg HP, Streppel KR, van der Beek AJ, et al. . The physical activity Scale for individuals with physical Disabilities: test-retest reliability and comparison with an accelerometer. J Phys Act Health 2007;4:96–100. 10.1123/jpah.4.1.96 [DOI] [PubMed] [Google Scholar]
- 39. Shaughnessy M, Resnick BM, Macko RF. Reliability and validity testing of the short self-efficacy and outcome expectation for exercise scales in stroke survivors. J Stroke Cerebrovasc Dis 2004;13:214–9. 10.1016/j.jstrokecerebrovasdis.2004.07.002 [DOI] [PubMed] [Google Scholar]
- 40. Barriers to being active quiz: centers for Disease Control and Prevention. https://www.cdc.gov/diabetes/ndep/pdfs/8-road-to-health-barriers-quiz-508.pdf
- 41. U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for chronic disease Prevention and Health Promotion, Division of Nutrition and physical activity. Promoting physical activity: a guide for community action. Champaign, Illinois: Human Kinetics, 1999. [Google Scholar]
- 42. Sawchuk CN, Russo JE, Bogart A, et al. . Barriers and facilitators to walking and physical activity among american indian elders. Prev Chronic Dis 2011;8:A63. [PMC free article] [PubMed] [Google Scholar]
- 43. Goldstein LB, Bertels C, Davis JN. Interrater reliability of the NIH stroke scale. Arch Neurol 1989;46:660–2. 10.1001/archneur.1989.00520420080026 [DOI] [PubMed] [Google Scholar]
- 44. Gowland C, Stratford P, Ward M, et al. . Measuring physical impairment and disability with the Chedoke-McMaster Stroke Assessment. Stroke 1993;24:58–63. 10.1161/01.STR.24.1.58 [DOI] [PubMed] [Google Scholar]
- 45. Nasreddine ZS, Phillips NA, Bédirian V, et al. . The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005;53:695–9. 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- 46. Kasner SE. Clinical interpretation and use of stroke scales. Lancet Neurol 2006;5:603–12. 10.1016/S1474-4422(06)70495-1 [DOI] [PubMed] [Google Scholar]
- 47. Raina P, Wolfson C, Kirkland S. Canadian Longitudinal Study on Aging (CLSA) Protocol, 2013. [Google Scholar]
- 48. Schmidt ME, Slanger T, Chang-Claude J, et al. . Evaluation of a short retrospective questionnaire for physical activity in women. Eur J Epidemiol 2006;21:575–85. 10.1007/s10654-006-9042-9 [DOI] [PubMed] [Google Scholar]
- 49. Brown C, Fraser JE, Inness EL, et al. . Does participation in standardized aerobic fitness training during inpatient stroke rehabilitation promote engagement in aerobic exercise after discharge? A cohort study. Top Stroke Rehabil 2014;21(Suppl 1):S42–51. 10.1310/tsr21S1-S42 [DOI] [PubMed] [Google Scholar]
- 50. Donner A, Klar N. Design and analysis of cluster randomized trials in health research. London: Arnold, 2000. [Google Scholar]
- 51. Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 2001;357:1191–4. 10.1016/S0140-6736(00)04337-3 [DOI] [PubMed] [Google Scholar]
- 52. Davey C, Hargreaves J, Thompson JA, et al. . Analysis and reporting of stepped wedge randomised controlled trials: synthesis and critical appraisal of published studies, 2010 to 2014. Trials 2015;16:358 10.1186/s13063-015-0838-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Hebert D, Lindsay MP, McIntyre A, et al. . Canadian stroke best practice recommendations: stroke rehabilitation practice guidelines, update 2015. Int J Stroke 2016;11:459–84. 10.1177/1747493016643553 [DOI] [PubMed] [Google Scholar]
- 54. MacKay-Lyons M, Macko R, Eng J, et al. . Aerobic exercise recommendations to optimize best bractices in care after stroke, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hargreaves JR, Prost A, Fielding KL, et al. . How important is randomisation in a stepped wedge trial? Trials 2015;16:359 10.1186/s13063-015-0872-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Beard E, Lewis JJ, Copas A, et al. . Stepped wedge randomised controlled trials: systematic review of studies published between 2010 and 2014. Trials 2015;16:353 10.1186/s13063-015-0839-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-015843supp001.pdf (228.5KB, pdf)