Abstract
Background:
Pleural effusion (PE) is a primary manifestation or secondary complication of many disorders. This study reviews the pattern and management of PE in a Nigerian hospital.
Materials and Methods:
The medical records of 213 patients with clinical diagnosis of PE over a period of 3 years were reviewed.
Results:
PE accounted for 0.5% of the total hospital admissions. The most common cause of PE was tuberculosis (TB) (32.9%), followed by malignancy (29.1%) and pneumonia (15.0%). The male to female ratio was 1.3:1. TB was the leading cause of effusion in males, while it was malignancy in females. Pneumonia accounted for 61.9% of PE in preschool age and 66.7% in school age. Breathlessness (50.0%), cough (39.4%), and chest pain (24.9%) were the common presentations. Most (90.1%) of them were exudative effusion and with half in the right lung. Chest radiography (91.6%), pleural fluid for Ziehl–Neelsen stain (74.7%), cytology (59.2%), and tissue biopsy (57.8%) were the common diagnostic investigations. The majority (92.0%) had closed thoracostomy tube drainage, while 9.9% had chemical pleurodesis. The intra-hospital mortality was 10 (4.7%).
Conclusion:
TB, malignancy, and pneumonia are the leading causes of PE. A multidisciplinary approach is needed for optimal management.
Key words: Etiology, management, Nigeria, pattern, pleural effusion
INTRODUCTION
Pleural effusion (PE) is defined as the excessive accumulation of fluid in the pleural space, resulting from an imbalance between pleural fluid formation and removal.1 It is a common clinical problem which can be a primary manifestation or a secondary complication of many disorders.2 The PE can be due to either exudative or transudative process.3 Common causes of transudative effusion are heart failure, liver cirrhosis, and hypoalbuminemia; common causes of an exudative effusion are malignancy, emphysema, parapneumonic effusion, and tuberculosis (TB).1,2,3 However, the etiology of PE remains unclear in nearly 20% of cases.1,2 The estimated prevalence of PE is 320 cases per 100,000 people in industrialized countries, with a distribution of etiologies related to the prevalence of underlying diseases.4 The incidence in the United States is estimated to be at least 1.5 million cases annually5 and >0.3% of the population each year in the UK.1 In Southwest Nigeria, pleural diseases accounted for 7.7% of respiratory morbidity with the majority between the ages of 15 and 44 years.6 Ogunleye et al. reported 372 cases of the pleural fluid collection over a 55-month period with male to female ratio of 1:1 and most of them between the ages of 20 and 49 years.7 Patients with PE most commonly present with dyspnea, initially on exertion, predominantly dry cough, and pleuritic chest pain. To treat PE appropriately, it is important to determine its etiology and distinguish pleural fluid transudate from exudates.8,9 There is a paucity of information on the burden of PE and most of the earlier works were on TB-related effusion.10,11,12 There is a need to document our local experiences in order to contribute the body of knowledge in Nigeria. The aims of this study were to determine the pattern and management of PE in a Nigerian hospital.
MATERIALS AND METHODS
This was a retrospective study carried out at the University of Ilorin Teaching Hospital, Ilorin, Nigeria. The study center is a tertiary hospital that serves as a referral center to four neighboring states. The hospital also runs an internship and postgraduate training programs in all the branches of medicine. We retrieved and reviewed all the medical case records of all patients who had a clinical diagnosis of PE in the hospital between November 2010 and October 2013 to obtain necessary data. Cases that had complete information and met the clinical criteria for diagnosis and classification of PE subtypes were studied. Sociodemographic information, clinical features, etiology, risk factors, comorbid conditions, duration of hospital stay, clinical characteristics, diagnostic approach, and modalities of managements were extracted from their case records. In addition, physical examination findings at admission, hematological, biochemical, cytological, histopathological, and microbiological results were obtained.
Diagnosis of pleural effusion
The diagnosis of PEs in the study participants was based on (1) clinical manifestations and (2) radiologic investigation – chest radiography and computed tomography (CT).
Ethical approval was obtained from the Institution Ethical Research Committee for the study.
Data analysis
The data were extracted by a postgraduate resident undergoing a clerkship rotation to remove bias; the clinical information was coded and entered into the computer Excel spreadsheet. Medical records with important missing information were excluded from the analysis. The data were analyzed using the Statistical Package for the Social Sciences, version 16 (SPSS Inc., Chicago, IL, USA). Descriptive and frequency statistics were obtained for the variables of interest. Etiology of PEs in patients was stratified by gender. Chi-square test was used to test for statistical significance between categorical variables. A P < 0.05 was considered statistically significant.
RESULTS
A total of 40,301 patients were admitted during the period of review; this included 30,680 adults and 9621 children and adolescents. Out of the 40,301 admissions, 213 were clinically diagnosed as PE and this figure accounted for 0.5% of the total hospital admissions. The age of the patients ranged from 2 months to 90 years, with a median age of 38 (interquartile range [IQR] 22–55) years. One hundred and twenty three patients (57.7%) were males and the male to female ratio was 1.3:1. Twenty-six (12.2%) of the patients were below the age of 18 years and this accounted for approximately 0.3% of the hospital admissions within this age range; in addition, they also have equal sex distribution. The median hospital stay was 14 (IQR 9–22) days. The other characteristics of the patients are shown in Table 1.
Table 1.
General characteristics' of the patients

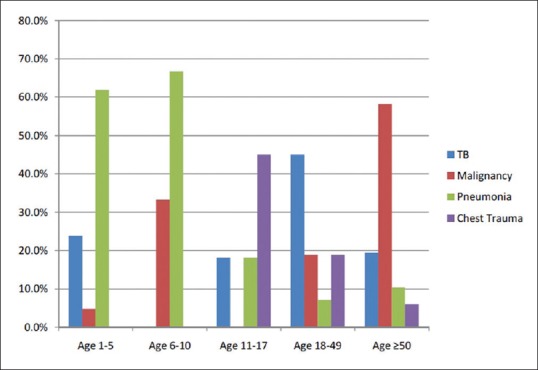
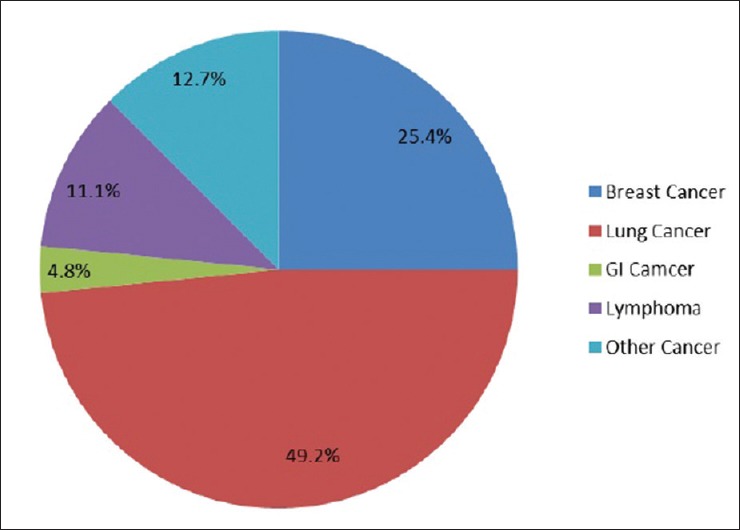
The most common cause of PE was TB (32.9%), followed by malignancy (29.1%) and pneumonia (15.0%). In the males, TB was the leading cause of PE, while it was malignancy among females [Table 2]. Pneumonia was the leading cause of PE in the preschool (61.9%) and school age (66.7%), while it was chest trauma in adolescent (45.0%). There were two cases of malignant PE in childhood (one due to nephroblastoma and one occult malignancy). TB was the most common cause of PE in adults <50 years (45.0%) and malignancy (58.2%) in 50 years and above [Figure 1]. Lung cancer (49.2%) and advanced breast cancer (25.4%) were the leading causes of malignant PE [Figure 2]. Furthermore, 89.1% of the cases had exudative PE. In this study, half of the cases have their effusion located in the right hemithorax and also presented with difficulty in breathing, while 39.4% reported a cough [Table 3]. Chest radiography (91.6%) and pleural fluid acid-alcohol-fast bacilli (74.7%) were leading methods of investigations. Nearly two-third of the patients were evaluated by pleural fluid cytology (59.2%) and tissue (either pleura or lung) biopsy (57.8%) and with less than half screened for HIV infection [Table 4]. In the treatment of PE, 196 (92.0%) cases had closed thoracostomy tube drainage (CTTD). Twenty-one cases (9.9%) had CTTD and chemical pleurodesis (2 g of tetracycline or 2 g of doxycycline in 60 ml slurry of 0.5% lidocaine). Seventeen out of 21 (81%) cases who had CTTD and chemical pleurodesis reported pleural drainage of ≤3 days postpleurodesis. Chemical pleurodesis was performed only in patients with malignant etiology. There was no significant difference (P = 0.573) in duration of drainage postpleurodesis between tetracycline (mean = 2.9 days) and doxycycline (mean = 2.5 days). The majority (67.1%) of the patients were treated with antimicrobials which consisted of antibiotics and anti-TB medication [Table 5]. A total ten patients with PE died within the period of admission in the hospital giving an intra-hospital mortality of 4.7% and 3 (1.4%) discharge themselves against medical advice.
Table 2.
Etiology of pleural effusions in patients by gender
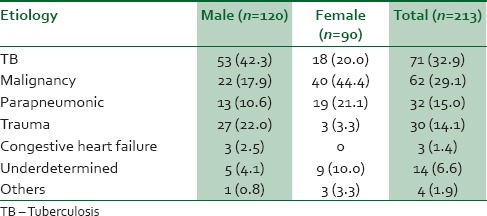
Figure 1.
Etiology of pleural effusions in patients by age group
Figure 2.
Etiology of malignant pleural effusion
Table 3.
Clinical presentations of patients with pleural effusion
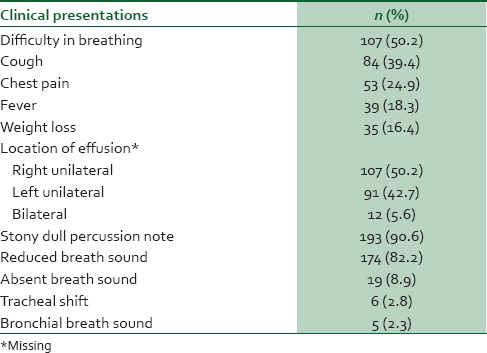
Table 4.
Diagnostic approach to pleural effusion
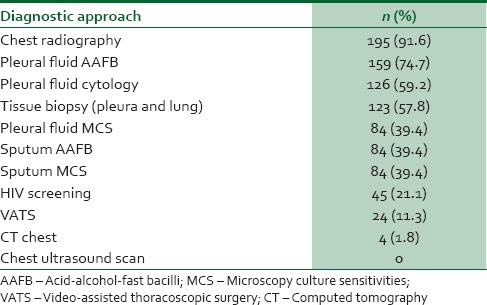
Table 5.
Treatment modalities in pleural effusion

DISCUSSION
Our study was conceived to determine the pattern and management of PE. Overall, PE accounted for 0.5% of the total hospital admissions meaning 5 out of every 1000 hospital admissions. The occurrence of PE varies across the Francophone West Africa countries from 1%–7% to 23%.13,14,15,16 In Ibadan, Nigeria, Onadeko et al noted that 56% of PE was caused by TB.17 However, there is a lack of uniformity in the methods or criteria used in reporting the burden of this condition making it difficult to compare results of study across different study populations. The demography in this study showed that the median age of the cases with PE was 38 years and this figure is similar to 37.8 years which was reported in Lagos, Nigeria,7 and 34.7 years reported from our center earlier,8 but it was less what was report from another part of the world.18,19,20,21,22 These variations may be attributed to the variation in the study population and the etiology and frequency of predisposing factors for PE in the different parts of the world. We also found a predilection for males in our study and this is in agreement with many other studies.7,8,18,19,21,22,23 The reason for this was due to more males high prevalence of smoking of tobacco and consumption of alcohol compared to female in our setting.24,25
TB accounted for one-third of effusion (32.9%) and is the leading cause of PE, followed by malignancy (18.7%). Lung cancer was responsible for half of the malignant PE. This is observation is in agreement with other previous studies;18,19,21,22,23,26,27,28 however, it is in contrast to the study by Ogunleye et al.,7 which reported breast cancer as the leading cause of cancer-related effusion. TB was the leading cause of PE in males while it was malignancy among females. The preponderance of TB as a leading cause of PE in this study was also reported previously from our center and other developing countries.8,18,19,20,21,22,26,27,28 On the other hand, this result is different from what is reported in Lagos, Nigeria, the Islamic Republic of Iran, and other developed countries.7,23,29,30 The second leading cause of PE was a malignancy and this result is similar to other observation18,20,21,22 and is in contrast to other studies that reported pneumonia.19,20 These etiological differences in PE causes could be explained by the fact that TB, HIV endemicity, and low socioeconomic status which are the risk factors for TB development are very common in this settings compared to the developed countries. In those studies that reported a contrasting result, this can be explained by the epidemiologic transition from communicable diseases to noncommunicable diseases such as cancer. Other factors might also be due to the type of patient's referral and clinic, the level of collaboration between the general and cardiothoracic surgeons, and the availability of video-assisted thoracoscopic surgery (VATS). Before this study, only 8.9% of cases of PE were reported to be of malignant etiology in our institution when VATS and percutaneous transthoracic biopsy were not available.8 In the center where VATS is not available, the diagnosis of malignant effusion is reportedly low6 and often patients with unexplained PE are made to undergo a therapeutic trial of anti-TB medication. In childhood, the leading cause of PE in the first decade of life is pneumonia, TB was the most common cause in adults <50 years, and malignancy in 50 years and above. This result is comparable to other studies in developed and developing countries.10,18,19,21,22 The risk of developing malignant effusion increases with age.2,3 Parapneumonic effusion is common in childhood because of the high incidence of acute respiratory infection in this age group. There is 8%–40% prevalence of parapneumonic effusions among the children with pneumonia in several other studies.31,32,33,34
The combination of clinical information, microbiological, and histological examination was the useful diagnostic tests for PE in this study. We did not determine the diagnostic yield of each diagnostic test because of the nature of the study, the role of predictive value in evidenced-based medicine may implicate the need for a future prospective study on PE. In the evaluation of the cases, it was an irony that 21% had HIV screening considering the fact that TB was the leading cause of PE. Early identification of comorbidity and concurrent management of immune depressive illness can improve the outcome of cancer cases. There was a right-sided dominance of PEs in this study which is similar to the findings of other previous studies.7,13,19,20,21,22,26,27,28,35 This result can be partly ascribed to the anatomy of the right bronchus, because the right bronchus is wider and shorter and runs more vertically than the left bronchus, aspirated microbes and biochemical particles are more likely to enter and lodge in it or one of its branches. There is also the hypothesis that greater blood volume is circulated through the right lung than the left.
The majority (67.1%) was treated with antibiotics and anti-TB medication, 92.0% had CTTD, and 9.9% had chemical pleurodesis. Malignant PE commonly complicates advanced cancer, especially in those with lung cancer, metastatic breast carcinoma, and lymphoma. This complication usually leads patients to suffer from troublesome dyspnea, which may impair their mobility and reduce their quality of life.36 A total ten patients with PE died during the period of admission in the hospital giving an intra-hospital mortality of 4.7%. This was lower than 16.6% reported in Eastern Nigeria, 6.4% in Ethiopia, and 13% in the Benin Republic.26,27,28 In view of the fact that the common causes of PE in this study are similar to the etiologies in these three latter studies, the lower mortality recorded may be due to the level care as a result of the collaboration of the physicians, surgeon, pathologies, and other healthcare workers in the PE study group. Other contributory factors are associated comorbidity and early presentation and diagnosis.
Limitations of the study
The study is retrospective in conduct and it is confronted with the problems of inability to carry out some studies such as CT scan, magnetic resonance imaging, tumor markers, which would have been useful in some cases due to out-of-pocket cost to the patients. Despite these limitations, we have been able to report the pattern of PE in our setting.
CONCLUSION
PE is a common clinical problem confronting physicians in Nigeria. TB, malignancy, and pneumonia are the leading causes of PE. A combination of clinicolaboratory and endoscopic approach is required for diagnosis. HIV screening is recommended as part of workup in patients with PE in our setting. Therefore, a multidisciplinary approach is needed for proper management.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Diaz-Guzman E, Dweik RA. Diagnosis and management of pleural effusions: A practical approach. Compr Ther. 2007;33:237–46. doi: 10.1007/s12019-007-8016-5. [DOI] [PubMed] [Google Scholar]
- 2.Davies RJO, Gleeson FV, Gary Lee YC, Porcel J, Brims F. Pleural Diseases. In: Warrell DA, Cox TM, Firth JD, editors. Oxford Textbook of Medicine. 5th ed. Vol. 2. Oxford: Oxford University Press; 2010. p. 18.17. [Google Scholar]
- 3.Loscalzo J. Pulmonary and critical care medicine. In: Wiener C, Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, et al., editors. Harrison's Principles of Internal Medicine. 17th ed. New York: McGraw-Hill; pp. 215–9. [Google Scholar]
- 4.Sahn SA. Pleural effusions of extravascular origin. Clin Chest Med. 2006;27:285–308. doi: 10.1016/j.ccm.2005.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Sahn SA. The value of pleural fluid analysis. Am J Med Sci. 2008;335:7–15. doi: 10.1097/MAJ.0b013e31815d25e6. [DOI] [PubMed] [Google Scholar]
- 6.Desalu OO, Oluwafemi JA, Ojo O. Respiratory diseases morbidity and mortality among adults attending a tertiary hospital in Nigeria. J Bras Pneumol. 2009;35:745–52. doi: 10.1590/s1806-37132009000800005. [DOI] [PubMed] [Google Scholar]
- 7.Ogunleye E, Thomas M, Olusoji O. Aetiology and demographic attributes of common pleural collections in an African population. Surg Sci. 2013;4:332–8. [Google Scholar]
- 8.Oguntoyinbo AE, Adeoye PO, Rahman GA, Abdulkadir AY. Radiological and clinical pattern of pleural effusion in Ilorin. West Afr J Radiol. 2008;15:1–5. [Google Scholar]
- 9.Karkhanis VS, Joshi JM. Pleural effusion: Diagnosis, treatment, and management. Open Access Emerg Med. 2012;4:31–52. doi: 10.2147/OAEM.S29942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adewole OO, Erhabor GE, Ogunrombi AB, Awopeju FA. Prevalence and patient characteristics associated with pleural tuberculosis in Nigeria. J Infect Dev Ctries. 2010;4:213–7. doi: 10.3855/jidc.699. [DOI] [PubMed] [Google Scholar]
- 11.Ezemba N, Eze JC, Anyanwu CH. Percutaneous needle pleural biopsies in pleural effusion of uncertain aetiology in a Nigerian teaching hospital. Trop Doct. 2006;36:112–4. doi: 10.1258/004947506776593422. [DOI] [PubMed] [Google Scholar]
- 12.Adegboye VO, Adebo OA, Osinowo O, Brimmo IA. Closed chest drainage without an underwater seal. Afr J Med Med Sci. 1996;25:353–5. [PubMed] [Google Scholar]
- 13.Ndongo S, Pouye A, Chavey SO, Ka MM, Diop TM. Current profile of pleurisies in Senegal: emergence of autoimmune diseases. Méd Afr Noire. 2009;5611:585–91. [Google Scholar]
- 14.Ouedraogo M, Ki C, Ouedraogo SM, Zoubga Az, Badoum G, Zigani A, et al. Epidemiological aspects of sero-fibrinous pleurisy at the Yalgada Ouédraogo National Hospital Center. Méd Afr Noire. 2000;4709:386–9. [Google Scholar]
- 15.Koffi N, Aka-Danguy E, Kouassi B, Ngom A, Blehou DJ. Etiologies of pleurisies in African milieu. Experience of the Cocody Pneumology department (Abidjan-Côte d'Ivoire) Rev Pneumol Clin. 1997;53:193–6. [PubMed] [Google Scholar]
- 16.Zannou DM, Ade G, Houngbé F, Agossou M, Azon-Kouanou A. Morbidity and mortality in hospitalization of internal medicine at the Hubert K. Maga National University Hospital Center, 2002-2003. Med Afr Noire. 2009;56:609–14. [Google Scholar]
- 17.Onadeko BO. Tuberculous pleural effusion: Clinical patterns and management in Nigerians. Tubercle. 1978;59:269–75. doi: 10.1016/0041-3879(78)90004-1. [DOI] [PubMed] [Google Scholar]
- 18.Valdés L, Alvarez D, Valle JM, Pose A, San José E. The etiology of pleural effusions in an area with high incidence of tuberculosis. Chest. 1996;109:158–62. doi: 10.1378/chest.109.1.158. [DOI] [PubMed] [Google Scholar]
- 19.Khan FY, Alsamawi M, Yasin M, Ibrahim AS, Hamza M, Lingawi M, et al. Etiology of pleural effusion among adults in the state of Qatar: A 1-year hospital-based study. East Mediterr Health J. 2011;17:611–8. [PubMed] [Google Scholar]
- 20.Dhital KR, Acharya R, Bhandari R, Kharel P, Giri KP, Tamrakar R. Clinical profile of patients with pleural effusion admitted to KMCTH. Kathmandu Univ Med J (KUMJ) 2009;7:438–44. doi: 10.3126/kumj.v7i4.2772. [DOI] [PubMed] [Google Scholar]
- 21.Liam CK, Lim KH, Wong CM. Causes of pleural exudates in a region with a high incidence of tuberculosis. Respirology. 2000;5:33–8. doi: 10.1046/j.1440-1843.2000.00223.x. [DOI] [PubMed] [Google Scholar]
- 22.Al-Qorain A, Larbi EB, Al-Muhanna F, Satti MB, Baloush A, Falha K. Pattern of pleural effusion in Eastern Province of Saudi Arabia: A prospective study. East Afr Med J. 1994;71:246–9. [PubMed] [Google Scholar]
- 23.Golshan M, Faghihi M, Ghanbarian K, Ghanei M. Common causes of pleural effusion in referral hospital in Isfahan, Iran 1997-1998. Asian Cardiovasc Thorac Ann. 2002;10:43–6. doi: 10.1177/021849230201000111. [DOI] [PubMed] [Google Scholar]
- 24.Desalu OO, Oluboyo PO, Olokoba AB, Adekoya AO, Danburam A, Salawu FK, et al. Prevalence and determinants of tobacco smoking among HIV patients in North Eastern Nigeria. Afr J Med Med Sci. 2009;38:103–8. [PubMed] [Google Scholar]
- 25.Nigeria Demographic and Health Survey 2013. Abuja, Nigeria, Rockville, Maryland, USA: NPC and ICF International; 2014. [Last accessed 2016 Nov 25]. National Population Commission (NPC) [Nigeria] and ICF International. Available from: https://www.dhsprogram.com/pubs/pdf/FR293/FR293.pdf . [Google Scholar]
- 26.Agossou M, Bashi BJ, Azon-Kouanou A, Zannou DM, Ade G, Houngbe F, et al. Pleural effusion at the internal medicine unit. Centre national hospitalier universitaire, Cotonou Benin. Afr J Respir Med. 2013;9:17–8. [Google Scholar]
- 27.Mbata GC, Ajuonuma BC, Ofondu EO, Okeke EC, Chukwuonye II, Aguwa EN, et al. Pleural effusion: Aetiology, clinical presentation and mortality outcome in a tertiary health institution in Eastern Nigeria – A five year retrospective study. J AIDS Clin Res. 2015;6:426. [Google Scholar]
- 28.Desalew M, Amanuel A, Addis A, Zewdu H, Jemal A. Pleural effusion: Presentation, causes and treatment outcome in a resource limited area, Ethiopia. Health. 2012;4:15–9. [Google Scholar]
- 29.Light RW. Clinical practice. Pleural effusion. N Engl J Med. 2002;346:1971–7. doi: 10.1056/NEJMcp010731. [DOI] [PubMed] [Google Scholar]
- 30.Marel M, Zrustová M, Stasný B, Light RW. The incidence of pleural effusion in a well-defined region. Epidemiologic study in central Bohemia. Chest. 1993;104:1486–9. doi: 10.1378/chest.104.5.1486. [DOI] [PubMed] [Google Scholar]
- 31.Kuti BP, Oyelami OA. Risk factors for parapneumonic effusions among children admitted with community acquired pneumonia at a tertiary hospital in Southwest Nigeria. Afr J Respir Med. 2014;10:26–34. [Google Scholar]
- 32.Cirino LM, Gomes FM, Batista BN. The etiology of extensive pleural effusions with troublesome clinical course among children. Sao Paulo Med J. 2004;122:269–72. doi: 10.1590/S1516-31802004000600008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson WB, Aderele WI, Osinusi KO, Gbadero DA. Community-acquired pneumonia in hospitalised Nigerian Children: Clinical and haematological correlates of diagnosis and outcome. Niger J Paediatr. 2001;28:101–14. [Google Scholar]
- 34.Gomez-Go GD, Gonzales L, Ong-Lim A. Clinical profile and outcome of children with parapneumonic effusion. PIDSP J. 2012;13:16–28. [Google Scholar]
- 35.Afful B, Murphy S, Antunes G, Dudzevicius V. The characteristics and causes of pleural effusions in Kumasi Ghana – A prospective study. Trop Doct. 2008;38:219–20. doi: 10.1258/td.2007.070275. [DOI] [PubMed] [Google Scholar]
- 36.Lumachi F, Mazza F, Ermani M, Chiara GB, Basso SM. Talc pleurodesis as surgical palliation of patients with malignant pleural effusion. Analysis of factors affecting survival. Anticancer Res. 2012;32:5071–4. [PubMed] [Google Scholar]


