Abstract
Nasal vestibular furunculosis is a common bacterial skin infection among the general population mostly affecting adults and children. It is characterized by acute localized infection of hair follicle in the skin lining of the nasal vestibule caused by Staphylococcus aureus. Immunodeficiency also plays an important role in recurrent skin and soft tissue infections (SSTI) including Nasal furunculosis. Though, the lesion is small, it is extremely painful and tender. Treatment is mostly conservative which consists of warm compresses, analgesics to relieve pain, topical and systemic antibiotics directed against staphylococcus. With rapidly increasing resistance to antibacterial agents, management of these bacterial infections is becoming increasingly difficult. In Ayurveda, it can be correlated with Nāsāruṇaśikhā (Nasal furunculosis). Morphologically, it appears like pīḍikā (Furuncle) which is characterized by Rāgayuktaśotha (inflammation with reddening. Jalaukāvacaraṇa (Leech therapy) is one of the ancient and important parasurgical procedures described in Ayurveda for treatment of various diseases. In this case, a leech has been applied at the affected area. After leech treatment, throbbing pain was reduced in its intensity followed by gradual reduction in swelling and reddening in two days. This case suggests the utility of leech application in Nasal vestibular furunculosis.
Keywords: Immunodeficiency, jalaukāvacaraṇa, nasaarunshika, nasal furunculosis
Introduction
Skin and soft tissue infections (SSTI) are one of the most common infections encountered in every age group which are caused by Staphylococcus aureus and Streptococcus, with occasional involvement of Gram-negative organisms.[1] Given the variable presentation of SSTIs, an assessment of their incidence and prevalence has been difficult. The estimated incidence rate of SSTIs is 24.6 per 1000 person/years. There is an increased prevalence among men (60% to 70% of all cases) and patients between 45 and 64 years of age.[2,3]
Nasal vestibular furunculosis is a common bacterial skin infection among the general population mostly affecting adults and children. It is characterized by acute localized infection of hair follicle in the skin lining of the nasal vestibule caused by Staphylococcus aureus.[4] Immunodeficiency also plays an important role for recurrent SSTI including Nasal furunculosis.[5] Though, the lesion is small, it is extremely painful and tender. This being a bacterial infection it has long-term morbid effects.[1]
Treatment is mostly conservative which consists of warm compresses, analgesics to relieve pain, topical and systemic antibiotics directed against staphylococcus.[6] With rapidly increasing resistance to antibacterial agents, management of these bacterial infections is becoming increasingly difficult.[7] Raktamokṣaṇa, i.e. blood letting is one of the ancient and important parasurgical procedures described in Ayurveda for treatment of various diseases. Jalaukāvacaraṇa or leech therapy has gained greater attention globally, because of its medicinal values. The saliva of leech contains biologically active substances, which have anti-inflammatory as well as anesthetic properties.
Present case report is of a patient with recurrent Nasal furunculosis who was not responding to antibiotics and was treated with Jalaukāvacaraṇa and (Śamana cikitsā) palliative treatment and the treatment was found to be effective in reducing the symptoms.
Case Report
On June 18, 2015 a 60-year-old male patient reported to O.P.D. with complaints of severe pain in left nostril since four days which was recurring from past six months. Severity of pain prevented him from his routine activity. Patient had taken medical treatment which included varieties of antibiotics, analgesics, anti-inflammatory medicines and topical antibiotics for six months; but felt only temporary relief. Recurrence of the Nasal furunculosis was observed after discontinuation of medication.
On examination of nose [Table 1] external appearance of nose didn’t reveal any pathology. The internal examination of nostrils revealed localized, inflamedred suppurated pus forming furuncle associated with throbbing pain in left nostril [Figure 1] while the right nostril was within normal limit. Routine hematological tests (Hemoglobin, Total Leucocytes Count, Differential Leucocytes Count, Erythrocyte sedimentationrate, and Absolute eosinophil count, Blood sugar fasting and Postprandial) werewithin normal limits. Vitals – pulse 72/min., regular, full volume, BP 130/80 mmHg (right arm sitting), Temperature 98.8 F, and Respiratory rate – 20/min. No significant abnormality of the nervous system, cardio-vascular system, and respiratory system were found. Per abdomen examination was also normal.
Table 1.
Local examination of nose
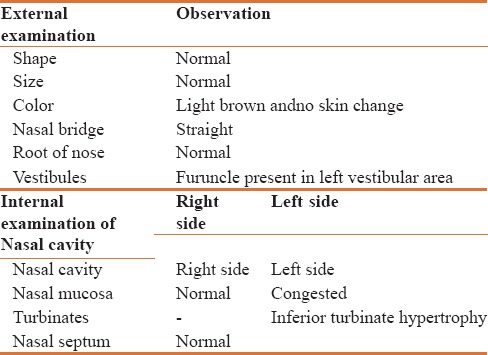
Figure 1.

Nasal furunculosis before treatment
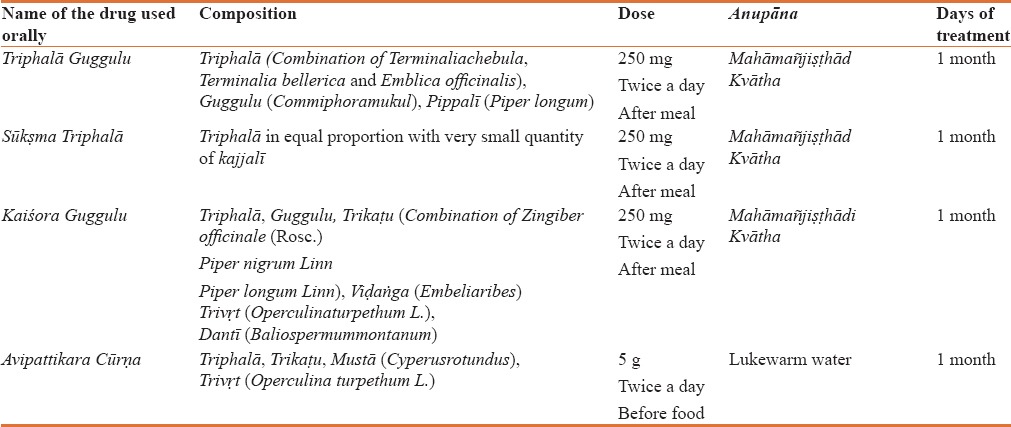
As per the classical texts of Ayurveda, observed symptoms which are presented in this case can be correlated with Nasārunaśikhā.[8] It was treated on the basis of treatment principles explained by Vāgbhaṭa in context of Jalaukāvacaraṇa. According to Vāgbhaṭa, pain and redness at the site of inflammation decreases radically followed by Jalaukāvacaraṇa due to letting out of vitiated rakta (blood).[9] In this case, after single setting of Jalaukāvacaraṇa, severe throbbing pain and redness in left nostrils due to nasal furunculosis was reduced. Later, patient was advised oral administration of Triphalā Guggulu[10] 250 mg, Kaiśora Guggulu[11] 250 mg and SūkṣmaTriphalā[12] 250 mg with Mahmañjiṣṭhādi Kvātha[13] 40 ml twice a day after lunch and dinner with Avipattikara Cūrṇa[14] 5 g twice a day before food for one month [Table 2].
Table 2.
Ayurvedic palliative treatment given for a case of recurrent nasal furunculosis
Method of Leech Application
As per standard protocol, a single leech was applied over nasal alae of left nostrils internally with due precautions, precision and all required care was taken to ensure patients safety.
Observations and Results
The patient was photographed before, [Figure 1] during and after leech application [Figures 2 and 3]. Photographs were taken with the same camera, magnification, lighting, angle, and film exposure. In this case, one leech was applied at the affected area. After leech application, throbbing pain reduced immediately despite swelling and reddening. These then gradually resolved in the next two days. The patient was advised to avoid diet which is predominant of kaṭu (pungent), amla (sour), lavaṇa (salty) tastes as they would, vitiate rakta and pitta.
Figure 2.

Leech application in Nasal furunculosis
Figure 3.

Nasal furunculosis after treatment
Discussion
Nasal Furunculosis is a quite common clinical entity affecting people of every age group especially in old age and children. Nose picking, plucking of the nasal hair with tweezers or trimming of the nasal hairs with nasal trimmers may also lead to Nasal Furunculosis. Many of these patients are chronic carriers of Staph. aureus in the nasal vestibule.[5] The initial symptom is focal pain in the tissues overlying the nasal vestibule which later on increases and causes significant difficulty affecting the daily activities of the patients.
The continuously increasing rates of infectious diseases have led to a higher usage of the commercially available antibiotics, which has resulted in resistance to antimicrobial agents.[15] In this case, the patient had taken higher antibiotics from different ENT specialists which may have resulted in developing antibiotic resistance.
Nasal Furunculosis is very well correlated with nasal disease Nāsāruṇaśikhā in Ayurveda. Though it is only described by Caraka in brief. According to Caraka it is Pākavantī Pīḍikā (Suppurated furuncle) caused due to vitiation of vāta and pitta.[8] In present case, patient had throbbing pain and reddening at furuncle site due to vitiation of vāta and pitta. As per treatment principle mentioned by Vāgbhaṭa in the context of Jalaukāvacaraṇa, we decided to apply a leech at the affected site.[16] After a single setting of leech therapy, patient experienced complete relief from throbbing pain followed by complete shrinkage of furuncle within two days.
The saliva of leech contains numerous biologically active substances, which have anti inflammatory as well as anesthetic properties. It also contains anesthetic substances which help to decrease the symptoms such as pain and tenderness. It contains various anti-inflammatory substances such as Bdellins and Eglins which are helpful in reduction of inflammation by reducing inflammatory components.[17] Salivary gland secretion obtained from the tropical leech H. manillensis was found to have wide spectrum antibacterial activity against both Gram-positive (S.aureus) and Gram-negative (Sal. Typhi and E. coli) bacterial strains confirming its antibacterial activity.[18] Leech saliva also contains hirudin-, calin-, and destabilase-like substances which increase microcirculation by decreasing the blood viscosity. Corboxypeptidase A inhibitor increases the inflow of blood at the site of bite. Histamine-like substances are also present in leech saliva which act as vasodilators.[19] It sucks the blood at superficial level from capillaries or extra-cellular spaces and hence the blood may be more impure than other body channels.[20] Various substances of leech saliva increase the microcirculation, decrease the inflammation as well as tenderness at furuncle site. Leech saliva promotes the increasing of local immunity as well.[21]
Following Jalaukāvacaraṇa, Śamana Cikitsā (Palliative treatment) was prescribed. Sūkṣma Triphalā, Triphalā Guggulu and Kaiśora Guggulu had been advised with Mahāmañjiṣṭhādi kvātha along with Avipattikara cūrṇa twice a day before food for one month. Triphalā is one of the important ingredients of above mentioned medicine. Itstrengthens the different tissues of the body, prevents ageing, and promotes health and immunity. It correctsconstipation, cleanses and tonifies the gastrointestinal tractand also detoxifies the whole body, and improves digestion and assimilation[22] Triphalā exhibits anti-viral, anti-bacterial, antifungal and anti-allergic properties.[23] Triphalā shows immunomodulatory properties and helps in improving the body’s defense system.[24]
Kaiśora Guggulu has Antiallergic, antibacterial and blood purifying properties which are used in skin diseases and gout.[25] Sūkṣma Triphalā is found to be effective in various infections like stye, decryocystitis, acnevulgaris and even against some viral infections such as viral pharyngitis.[26] Triphalā Guggulu has antimicrobial activity which has been implemented in treatment of sinusitis, allergies, boils, constipation, piles, high cholesterol, mal-absorption and as a purgative.[27] Both Guggulu formulations, mainly consists of Guggulu (Commiphoramukul) which is known to have analgesic, anti-inflammatory activity, antibacterial, and antioxidant property etc.[28] Mahāmañjiṣṭhādi Kvātha is one of the popular Ayurvedic preparations that is used as a blood purifier and in treating various skin diseases such as Acne vulgaris, Psoriasis etc., It promotes skin health and complexion, Pacifies pitta, acts as immune modulator.[29] Mañjiṣṭhā (Rubiacordifolia Linn) which is one of the important ingredient of Mahāmañjiṣṭhādi kvātha acts as a potent blood purifier, antioxidant, anti-inflammatory, anti stress, antimicrobial which can play important role to cure furuncle like skin infections and improve skin health.[30,31] Avipattikara Cūrṇa is indicated in all pitta vikāras. Pitta and rakta has āśrayāśrayībhāva (inter relationship of doṣa with dhātu) if pitta gets vitiated rakta also gets vitiated and this is the root cause of Nasāruṇaśikhā. Avipattikara cūrṇa pacifies pitta and ultimately pacify Rakta too.[32]
Application of leech, in the case of recurrent Nasal furunculosis is not published previously. Rakta and pitta are prime doṣas for causing Nāsāruṇashikhā (Nasal furuncle). There is no other doṣa involved in pathogenesis of Nāsāruṇashikhā except vāta and pitta. Pitta vitiates rakta which causes suppuration resulting in blockage of vāta. Due to obstructed path of vāta doṣa by suppuration results in throbbing pain at the affected site. Here removing the blockage by Jalaukāvacaraṇa plays vital role in treatment of Nāsāruṇashikhā. In this case, Leech therapy was found to be effective not only in reducing the pain but also subsiding progression of furuncle. During the follow-up period of two months, recurrence of Nasal furunculosis was not seen. These observations and results indicate effectiveness of Ayurvedic approach in management of Nasal furunculosis.
Conclusion
The present case suggests effectiveness of leech application which significantly reduced throbbing pain, erythema, and inflammation in Nasal furunculosis. Jalaukāvacaraṇa in this condition provided a safe and amenable treatment option which is least expensive and is easy to be done. Instant relief in painful condition of Nasal furunculosis after Jalaukāvacaraṇa indicates its utility in other inflammatory disorders. As vāta and pitta are only doṣa causes of Nāsāruṇashikhā and there is no other type of this disease is mentioned in classical texts, hence the present treatment modality need to be studied at larger sample sizes to establish its efficacy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Department of Agadtantra and Vyavahar Ayurveda and Department of Kayachikitsa, MGACH and RC, Salod (H) Wardha.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Palit A, Inamadar AC. Current concepts in the management of bacterial skin infections in children. Indian J Dermatol Venereol Leprol. 2010;76:476–88. doi: 10.4103/0378-6323.69053. [DOI] [PubMed] [Google Scholar]
- 2.Ellis Simonsen SM, van Orman ER, Hatch BE, Jones SS, Gren LH, Hegmann KT, et al. Cellulitis incidence in a defined population. Epidemiol Infect. 2006;134:293–9. doi: 10.1017/S095026880500484X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eron LJ, Lipsky BA, Low DE, Nathwani D, Tice AD, Volturo GA, et al. Managing skin and soft tissue infections: Expert panel recommendations on key decision points. J Antimicrob Chemother. 2003;52(Suppl 1):i3–17. doi: 10.1093/jac/dkg466. [DOI] [PubMed] [Google Scholar]
- 4.Weston V. Scott Brown's Text Book of Otorhinolaryngology and Head and Neck Surgery. 7th ed. Vol. 17. London: Edward Arnold Ltd; 2008. p. 196. [Google Scholar]
- 5.Das A, Borah H, Jamil MD, Hanifa A, Das KB. Unusually high incidence and complications of nasal furunculosis at North East region of Assam. Nation J Otorhinolaryngol Head Neck Surg. 2014;2:20–1. [Google Scholar]
- 6.Dhingra PL, Dhingra S, Dhingra D. Diseases of Ear, Nose and Throat & Head and Neck Surgery. 6th ed. New Delhi: Elsevier Publication; 2014. p. 145. [Google Scholar]
- 7.Sharma C, Singh C, Sharma LN, Purvia R, Adlakha M. Antibiotic resistant organism: An emerging public health problem and role of Ayurveda (an overview) Int J Ayurveda Pharm Res. 2014;2:17–29. [Google Scholar]
- 8.Sastri K, Chaturvedi GK. Chikitsasthan 26/117. Vol. 2. Varanasi: Chaukumba Bharti Academy; 2004. Caraka Samhita;Vidyotini Hindi Commentary; p. 740. [Google Scholar]
- 9.Gupta A. Ashtanga Hridaya, Vidyotini Hindi Commentary, Sutrasthan 26/47. Reprint ed. Delhi: Chaukhambha Sanskrit Sansthan; 2005. p. 147. [Google Scholar]
- 10.Srivastav S. Sharangdhar Samhita Jiwanprada Hindi Commentary, Madhyam Khandvatakkalpana-Triphala Guggulu. Ch. 7/82-83. Varanasi: Choukhamba Orientalia; 1999. p. 205. [Google Scholar]
- 11.Dasaji G, Shastri A. Bhaishajya Ratnavali. 19th ed. Ch. 27/98-108. Varanasi: Chaukhamba Sanskrit Sansthan; 2008. Kaishorguggulu; p. 598. [Google Scholar]
- 12.Date BB. Therapeutic Index, Formulation Sukshm Triphala. Pune: Ayurvedrasashala; 2006. p. 34. [Google Scholar]
- 13.Srivastav S. Varanasi: Choukhamba Orientalia; 1999. Sharangdhar Samhita Jiwanprada Hindi Commentary, Madhyam Khand Kwathkalpana, Mahamnjishtadi Kwath; Ch 2/139-144; p. 156. [Google Scholar]
- 14.Dasaji G, Shastri A. Bhaishajyaratnavali. 19th ed. Ch. 56/25-29. Varanasi: Chaukhamba Sanskrit Sansthan; 2008. Avipattikar Churna; p. 922. [Google Scholar]
- 15.Tasiemski A, Salzet M. U.S. Patent No. 20,120,251,625. Use of Extract of Leeches as Antibacterial Agent. WO. 2011/045427 A1. 2011. Washington, DC: U.S. Patent and Trademark Office; 4 October; 2012. [Google Scholar]
- 16.Subhose V, Srinivas P, Narayana A. Biography of mădhavakara: His scholarly contribution. Bull Indian Inst Hist Med Hyderabad. 2005;35:113–30. [PubMed] [Google Scholar]
- 17.Rai PK, Singh AK, Singh OP, Rai NP, Dwivedi AK. Efficacy of leech therapy in the management of osteoarthritis (Sandhivata) Ayu. 2011;32:213–7. doi: 10.4103/0974-8520.92589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abdualkader AM, Merzouk A, Ghawi AM, Alaama M. Some biological activities of Malaysian leech saliva extract. Int Islamic Univ Malaysia Eng J. 2011;12:1–9. [Google Scholar]
- 19.Michalsen A, Klotz S, Lüdtke R, Moebus S, Spahn G, Dobos GJ, et al. Effectiveness of leech therapy in osteoarthritis of the knee: A randomized, controlled trial. Ann Intern Med. 2003;139:724–30. doi: 10.7326/0003-4819-139-9-200311040-00006. [DOI] [PubMed] [Google Scholar]
- 20.Raval H, Thakar A. Raktamokshana by Jalaukavacharana & Shiravedhana-Vicharchika (Eczema)-MD Dissertation. IPGT&RA, GAU, Jamnagar. 2010 [Google Scholar]
- 21.Bhagat PJ, Raut SY, Lakhapati AM. Clinical efficacy of jalaukawacharana (leech application) in Thrombosed piles. Ayu. 2012;33:261–3. doi: 10.4103/0974-8520.105248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehta BK, Shitut S, Wankhade H. In vitro antimicrobial efficacy of Triphala. Fitoterapia. 1993;64:371–2. [Google Scholar]
- 23.Sumathi P, Parvathi A. Antibacterial potential of the three medicinal fruits used in Triphala: An ayurvedic formulation. J Med Plants Res. 2010;4:1682–5. [Google Scholar]
- 24.Naik GH, Priyadarsini KI, Bhagirathi RG, Mishra B, Mishra KP, Banavalikar MM, et al. In vitro antioxidant studies and free radical reactions of triphala, an ayurvedic formulation and its constituents. Phytother Res. 2005;19:582–6. doi: 10.1002/ptr.1515. [DOI] [PubMed] [Google Scholar]
- 25.Lather A, Gupta V, Bansal P, Sahu M, Sachdeva K, Ghaiye P. An ayurvedic polyherbal formulation kaishore guggulu: A review I. Int J Pharm Biol Arch. 2011;2:497–503. [Google Scholar]
- 26.Dawane JS, Pandit VA, Borole KD, Kulkarni SD, Asalkar MR. Anti-infective activities of Sookshma Triphala in abdominal sepsis induced by cecal ligation in rats. Int J Pharm Biomed Res. 2011;2:250–3. [Google Scholar]
- 27.Itankar P, Nagulwar DB, Bhatlawande B. Physical, phytochemical and chromatographic evaluation of triphala guggul tablets. E Int J Pharm Phytopharmacol Res. 2015;4:306–9. [Google Scholar]
- 28.Chander R, Khanna AK, Pratap R. Antioxidant activity of guggulsterone, the active principle of guggulipid from Commipheramukul. J Med Aromat Plant Sci. 2002;24:370. [Google Scholar]
- 29. [Last accessed on 2015 Sep 29; 2: 15 PM]. Available from: http://www.bimbima.com/./mahamanjishthadi-kwath-for-skin-diseases.aspx .
- 30. [Last accessed on 2015 Sep 29; 5: 10 PM]. Available from: https://www.satveda.com/p/mahamanjishth adikwathlast .
- 31.Meena V, Chaudhary AK. Manjistha (Rubiacordifolia) – A helping herb in cure of acne. J Ayurveda Holist Med. 2015;3:11–7. [Google Scholar]
- 32.Gyawali S, Khan GM, Lamichane S, Gautam J, Ghimire S, Adhikari R, et al. Evaluation of anti-secretory and anti-ulcerogenic activities of avipattikar churna on the peptic ulcers in experimental rats. J Clin Diagn Res. 2013;7:1135–9. doi: 10.7860/JCDR/2013/5309.3058. [DOI] [PMC free article] [PubMed] [Google Scholar]