Summary
Purpose
Is it possible a correlation between some periprosthetic femoral fractures and atypical fractures?
Case
We present a case of a 77-year-old woman with atypical periprosthetic femoral fracture. The patient had a history of long-term bisphosphonate use. We performed an open reduction, a synthesis of the fracture and a histological exam. The patient stopped the bisphosphonate (BF) therapy. Three months later, before starting the teriparatide treatment, the patient had a re-fracture so we did a second osteosynthesis and began a teriparatide therapy. After six months, the radiography showed a bone healing at the fracture site.
Result
The histological examination confirmed the diagnosis of atypical femoral fracture.
Conclusion
At first, the fracture showed a delayed union which led to a new surgery, as often happens in BF-related atypical fractures. Appropriate treatment (BF suspension and teriparatide beginning) permitted fracture healing. The atypical characteristic of the fracture was confirmed by histological exam.
Some periprosthetic femoral fractures in patients treated with BF, especially in long time therapies, should be suspected as atypical fractures and a specific medical treatment should be performed, as well as a correct surgical treatment.
Keywords: atypical fracture, bisphosphonate, periprosthetic fracture, fracture healing, hip replacement
Introduction
Hip arthroplasty procedures in patients with osteoarthritis and femur neck fragility fractures are continuously increasing (1). Consequently, periprosthetic fractures are growing because of periprosthetic bone mineral decreasing after hip arthroplasty (2).
Nowadays the use of antiresorptive drugs is increasing both to treat osteoporosis and improve prosthesis-bone osseointegration, and to reduce the bone loosening (3). To date, most commonly used antiresorptive drugs are bisphosphonates (BF). They are potent osteoclast inhibitors that reduce the risk of fragility fractures.
Many studies show a possible correlation between prolonged use of bisphosphonates and the onset of atypical femoral (subtrocantheric and femoral shaft) fractures. It’s hypothesized that BF can alter the normal collagen cross-linking and matrix heterogeneity and can reduce the vascularity (4, 5).
Atypical femoral fractures can be considered “de novo stress fractures” occurring in an altered bone structure located in high bending forces sites, as femoral shaft. In these high stressed sites, the formation of micro-crackers couldn’t be repaired by the normal bone remodeling. This fracture, in a higher percentage than “typical fractures”, is associated with slow healing and prolonged post-operative immobility (6, 7).
Periprosthetic femoral fractures are not included in atypical fractures, (5, 8) but recently some Authors reported cases of BF-associated fractures involving prosthetic stem (9).
We report a case of a patient, a 77-year-old female, with atraumatic refracture at femoral periprosthetic fracture site.
Clinical case
A 77-year-old woman with THA (total hip arthroplasty) at the right femur following a fragility fracture (in 2002). In July 2014, a sub-prosthetic hip fracture occurred after a fall from standing position (low-energy trauma). She reported that never felt pain at the right thigh before.
The patient declared to be a non-smoker and to drink half a glass of wine during meals; BMI (body mass index) was 24.24. The patient had generalized osteoarthritis, polymyalgia rheumatica and osteoporosis (DEXA May 2014, T-score: total left femur −1.6, spineL1–L4 −1.1).
At the time of periprosthetic fracture she was treated with methylprednisolone (4 mg/day) and prednisone (2 mg/day) for less than 1 year, hydroxychloroquinesulfate (200 mg/day), alendronic acid + cholecalciferol (for more than 10 years). During hospitalization the patient performed blood tests and X-ray of the contralateral femur; she underwent surgery to reduce and fix the fracture with plate, screws, cerclage wiring, and bone graft.
Furthermore, intraoperative bone sampling was performed to make histological examination and bone scintigraphy was scheduled.
The patient was discharged from the hospital and it was suggested to stop the alendronic acid therapy and start a therapy with cholecalciferol, magneto therapy, calcium supplement, heparin prophylaxis, active and passive physiotherapy of the limb operated with no weight bearing.
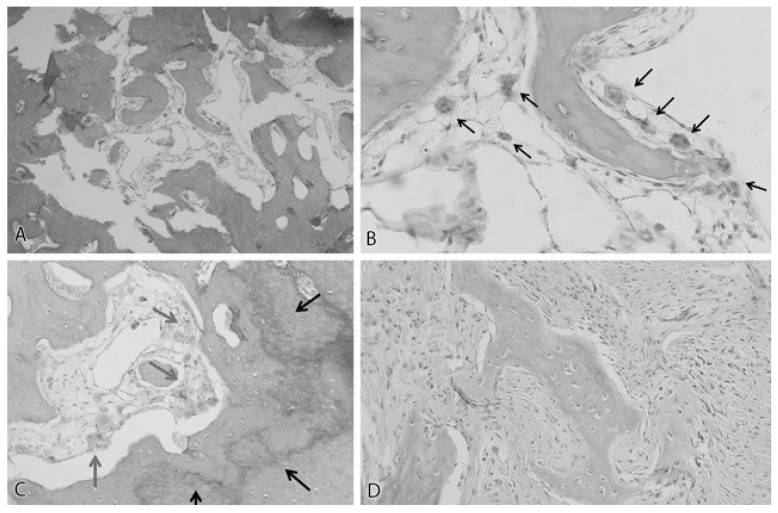
The result of the histological exam was compatible with the diagnosis of atypical femoral fracture (“cortical bone showed multiple fractures, with average diameter of 160 microns, in which context amorphous cell-free material was observed. Resorption cavities with numerous osteoclasts was found close to fracture lines and there were signs of new bone apposition and callus reaction bordering the fracture gaps”) (Figure 1).
Figure 1.
A) Close to the fracture gap, irregularly-shaped fragments of woven bone can be found breaking off from the fracture surface. Fragments show off variable degree of degradation. [Magn. 10x]; B) Giant osteoclasts (black arrows) - typical finding in bisphosphonate users - are frequently found close to fracture lines, particularly in patients under treatment with biphosphonates. [Magn. 40x]; C) Close to fracture gap, signs of recent bone remodeling, with osteons interrupted by new woven bone bordering fracture gap. Newly formed bone displays irregularly shaped lamellae (black arrows). Note giant osteoclasts above the irregular bone surface (red arrows). [Magn. 20x]; D) The thick callus layer next to fracture line consists of some woven bone but mainly of a highly cellular soft tissue therefore it is unlikely to provide a concrete mechanical stability. No distinct cartilage tissue is found. [Magn. 20x].
The following blood tests were: Ca 9.1 mg/dl, P 4.5 mg/dl, Vit D 8.8ng/ml, PTH 37.4 pg/ml, ALP 151IU/l, creatinine 0.53 mg/dl and serumtotal protein 6.5 g/dl.
The bone scintigraphy showed no bone lesions compatible with pre-fractures concerning the contralateral femur.
Considering the results of these further investigations, at the time of the next ambulatory follow-up visit, it was prescribed teriparatide treatment.
The patient, for personal reasons, didn’t start the therapy immediately. In October 2014, the patient returned to our attention for the onset of pain in the right thigh with no apparent trauma (at the time she had walked with partial weight bearing on the treated limb); radiographic examination showed a periprosthetic fracture of the femur, at the same level of the prior fracture, with internal fixation rupture.
The patient underwent a new surgery of reduction and synthesis of the fracture. During the procedure we found that the cortical bone in the affected area was sclerotic and thickened. So it was decided to start a treatment with teriparatide and, at the time of discharge from the hospital, we told the patient to continue the previous treatment with the integration of Ca and vit. D, active and passive physiotherapy for operated limb with no weight bearing.
In the subsequent control visits in the clinic, it was a progressive weight bearing on the right lower limb, up to the achievement of the full weight bearing. In addition, due to the onset of low back pain, the patient performed X-ray and MRI of the spine that showed multiple vertebral fractures.
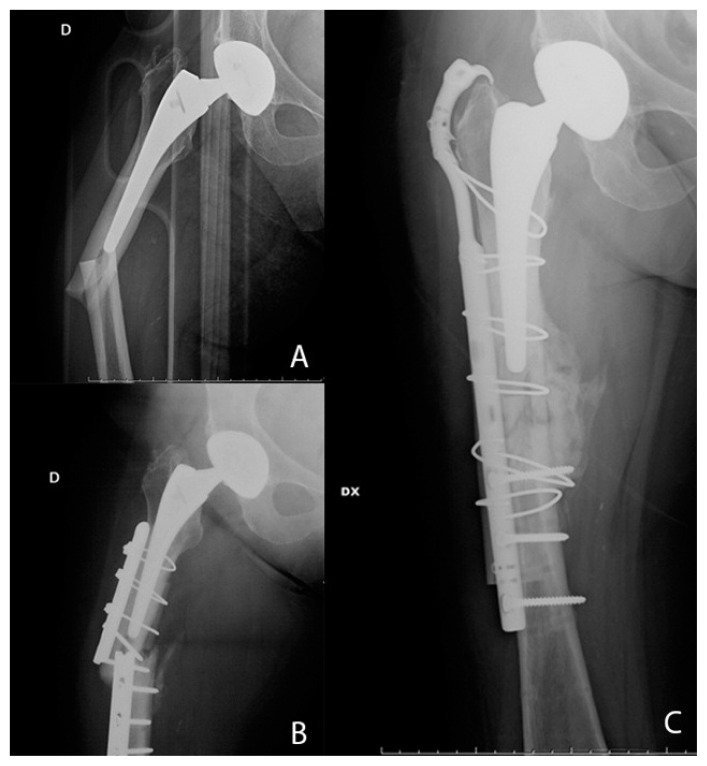
During the last check in April 2015, the patient was walking independently, she had no pain and a goodhip’s range of motion; the radiography showed abone healing at the femoral fracture site (Figure 2).
Figure 2.
A) Sub-prosthetic hip fracture; B) re-fracture; C) new osteosynthesis and fracture healing.
According to Italian law, the ethical approval for this study was not required because it involved only a clinical routine follow-up and a radiographic examination. The patient was informed that data concerning the case would be submitted for publication and she agreed.
Discussion
The corrected stem position and well fixed implant excluded a “tip effect” in determining the periprosthetic fracture. There was a radiographic lateral femoral cortical thickening at the site of the fracture. These findings, associated with the low energy trauma which determined the fracture, can suggest that there were intrinsic bone structural abnormalities.
The patient clinical history focused a long period of BF assumption associated with proton pump inhibitors. The histological intraoperative exam confirmed the presence of an atypical fracture (10, 11).
Although the fracture was correctly treated with a surgical synthesis and weight bearing abstention and even if there was associated a correct medical treatment featured in immediately stop of BF assumption, implementation of calcium and Vit D support, there was a new spontaneous fracture (with plate rupture) after three months, which required a new surgical treatment. It’s important to stress that the anabolic treatment with teriparatide wasn’t started at the prescription time, for personal choice of the patient.
BFs can be recognizable as cause of a tight pain in hip replacement. Their action in preventing fragility fractures can cause a hip’s range of motion alteration in a few patients. This can cause micro fractures especially in more mechanical stress sites as the lateral femoral cortex (12, 13).
In hip prosthesis the femoral stem presence, changing the bone modulus of elasticity, can increase the amount of mechanical stress and promote the occurrence of femoral atypical fractures.
The well-known hip stem effect on lateral femoral cortical bone, together with a decreased bone elastic resistance BF induced, can produce a tight pain unto an atraumatic periprosthetic femoral fracture even in well positioned stem. Despite the large and continuously growing use of BF in association with orthopedic and traumatologic surgery, nowadays there isn’t enough literature data about the effect in atypical femoral periprosthetic fractures induced by BF; there have been only a few cases reported in the literature of femoral periprosthetic fracture in patients with long BF therapy (4, 12). This problem can become realistically more common so that it should be suspected in every tight pain in patients treated with BF.
It is important to make a precise diagnosis in order to realize a correct treatment strategy both in terms of surgical and medical choices. First of all, it is necessary to evaluate at the same time the implant stability and the metabolic status of the bone. It is also important to look for the presence of a cortical spike at the fracture level. Then it is necessary to combine a correct surgical treatment with an immediate stop of the BF therapy. As soon as possible it should be performed a metabolic therapy [for instance teriparatide (14, 15)] and an appropriate integration with calcium and Vit D.
It can be useful magnetotherapy application to optimize the bone metabolic properties.
In cases of non-surgical treatment, a limited hip’s range of motion is indicated. It’s also necessary a follow-up to monitor the prodromal symptoms of a possible fracture (as persistent or increased tight pain).
Nowadays it is important to suspect a potential atypical BF-induced fracture in every tight pain in hip replacement in patients treated for a long period with BF, especially those with comorbidities as: Rheumatoid arthritis RA, steroid therapy.
Atypical periprosthetic fractures are different from “typical” femoral fractures also because of the bone structural alterations that can cause a delayed healing.
Thus it is important to consider the atypical periprosthetic fractures as an independent pathology, different from “typical traumatic” periprosthetic fractures, that requires a specific diagnostic plan and treatment.
Conclusion
The etiology of thigh pain and some periprosthetic stem femoral fractures in patients treated with BF, especially in long time therapies, should be suspected as atypical fractures and a specific medical treatment should be performed, as well as a correct surgical treatment.
Footnotes
Disclosure
The Authors declare no conflict of interest. No financial support was received for this study.
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
References
- 1.Bottai V, Dell’Osso G, Celli F, Bugelli G, Cazzella N, Cei E, Guido G, Giannotti S. Total hip replacement in osteoarthritis: the role of bone metabolism and its complications. Clin Cases Miner Bone Metab. 2015;12(3):247–250. doi: 10.11138/ccmbm/2015.12.3.247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mann T, Eisler T, Boden H, Muren O, Stark A, Salemyr M, Skoldenberg O. Larger femoral periprosthetic bone mineral density decrease following total hip arthroplasty for femoral neck fracture than for osteoarthritis: A prospective, observational cohort study. J Orthop Res. 2015;33(4):504–512. doi: 10.1002/jor.22783. [DOI] [PubMed] [Google Scholar]
- 3.Cavalli L, Brandi ML. Periprosthetic bone loss: diagnostic and therapeutic approaches. F1000 Res. 2014;17(2):266. doi: 10.12688/f1000research.2-266.v2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cross MB, Nam D, van der Meulen MC, Bostrom MP. A rare case of a bisphosphonate-induced peri-prosthetic femoral fracture. J Bone Joint Surg Br. 2012;94(7):994–997. doi: 10.1302/0301-620X.94B7.28778. [DOI] [PubMed] [Google Scholar]
- 5.Bottai V, Giannotti S, Dell’Osso G, De Paola G, Menconi A, Falossi F, Raffaeta G, Guido G. Atypical femoral fractures: retrospective radiological study of 319 femoral fractures and presentation of clinical cases. Osteoporos Int. 2014;25(3):993–997. doi: 10.1007/s00198-013-2546-8. [DOI] [PubMed] [Google Scholar]
- 6.Teo BJ, Koh JS, Goh SK, Png MA, Chua DT, Howe TS. Post-operative outcomes of atypical femoral subtrochanteric fracture in patients on bisphosphonate therapy. Bone Joint J. 2014;96-B(5):658–64. doi: 10.1302/0301-620X.96B5.32887. [DOI] [PubMed] [Google Scholar]
- 7.Giannotti S, Bottai V, Dell’Osso G, De Paola G, Ghilardi M, Guido G. Pseudoarthrosis in atypical femoral fracture: case report. Osteoporos Int. 2013;24(11):2893–2895. doi: 10.1007/s00198-013-2397-3. [DOI] [PubMed] [Google Scholar]
- 8.Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, Einhorn TA, Genant HK, Geusens P, Klaushofer K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O’Keefe R, Papapoulos S, Howe TS, van der Meulen MC, Weinstein RS, Whyte MP. Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res. 2014;29(1):1–23. doi: 10.1002/jbmr.1998. [DOI] [PubMed] [Google Scholar]
- 9.Lee JY, Soh T, Howe TS, Koh JS, Kwek EB, Chua DT. Bisphosphonate-associated peri-implant fractures: a new clinical entity? Acta Orthop. 2015;30:1–5. doi: 10.3109/17453674.2015.1036339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schilcher J, Sandberg O, Isaksson H, Aspenberg P. (2014) Histology of 8 atypical femoral fractures: remodeling but no healing. Acta Orthop. 2014 Jun;85(3):280–286. doi: 10.3109/17453674.2014.916488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schilcher J. Epidemiology, radiology and histology of atypical femoral fractures. Acta Orthop. 2013 Dec;84(352):1–26. doi: 10.3109/17453674.2013.850008. [DOI] [PubMed] [Google Scholar]
- 12.Curtin BM, Fehring TK. Bisphosphonate fractures as a cause of painful total hip arthroplasty. Orthopedics. 2011;34(12) doi: 10.3928/01477447-20111021-36. [DOI] [PubMed] [Google Scholar]
- 13.Bhattacharyya R, Spence S, O’Neill G, Periasamy K. Bisphosphonate-induced periprosthetic fracture: a cause of painful total hip arthroplasty. Case Rep Surg. 2014 doi: 10.1155/2014/631709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giannotti S, Bottai V, Dell’Osso G, de Paola G, Pini E, Guido G. Atrophic femoral nonunion successfully treated with teriparatide. Eur J Orthop Surg Traumatol. 2013;23(Suppl2):S291–294. doi: 10.1007/s00590-012-1143-1144. [DOI] [PubMed] [Google Scholar]
- 15.Giannotti S, Bottai V, Dell’Osso G, Pini E, De Paola G, Bugelli G, Guido G. Current medical treatment strategies concerning fracture healing. Clin Cases Miner Bone Metab. 2013;10(2):116–120. [PMC free article] [PubMed] [Google Scholar]