Summary
Purpose
Osteoarthritis (OA) is the most common joint disorder in the elderly, causing significant pain which negatively affects mobility and quality of life. The aim of the study was to assess the effectiveness of ultrasound image-guided intra-articular injections of Hyalubrix® combined with exercise therapy in the treatment of hip osteoarthritis.
Methods
This was a single site, prospective, open-label, Investigator-initiated study. Forty patients were enrolled and received three ultrasound image-guided injections of Hyalubrix®, 45 days apart, combined with three sessions a week of physical therapy (proprioceptive rehabilitation of the lower limbs; gait training; balance training) up to a total of 30 sessions (10 weeks), starting from one week after the first injection.
Results
The primary objective was to achieve a lasting reduction in OA symptoms related to pain during activity. During the course of the study the pain perceived by the patient during activity dropped from a mean value of 6.94 cm to a mean value of 1.46 cm and showed a statistically significant decrease from visit 1 compared to baseline (p < 0.05) which was confirmed at all the subsequent time points. Significant improvements were also observed in the evaluation of the secondary objectives: hip disability; OA-related pain at rest; daily functioning and NSAIDs intake.
Conclusions
Results from this study including 40 patients for a total of 65 treated hips demonstrate a significant improvement in OA-related pain, hip disability, and patient’s daily functioning as well as a reduction in NSAIDs intake. Patients suffering from hip OA seem to benefit from the treatment with Hyalubrix® injections plus exercise therapy.
Keywords: hip osteoarthrosis, viscosupplementation, hyaluronic acid, physical therapy
Introduction
Osteoarthritis (OA) is the most common type of arthritis and the main cause of disability in the elderly population worldwide. Hip OA is the second most frequent form of OA affecting a large joint, and its prevalence ranges from 3 to 11% in populations over 35 years old (1–3).
Risk factors include genetics, female gender, past trauma, advancing age and obesity. Given that the number of people aged 65 and over is expected to double by 2030 (4), along with escalations in obesity and physical inactivity (5, 6), the social and economic impact on society of OA-related disability can also be expected to increase.
The main symptoms of hip OA are joint pain and stiffness which can limit mobility, affect quality of life and may lead to disability.
Treatment is aimed at reducing pain and stiffness, limiting disease progression and improving mobility and quality of life.
Both nonpharmacological and pharmacologic treatment options are available, including complementary and alternative therapies and surgery, and many patients will be treated with a combination of both (7).
A nonpharmacological approach is particularly important in the elderly population due to the likelihood that medications are already being prescribed for co-morbidities with the associated risk of toxicity and polypharmacy (8).
Initial conservative recommendations include education, self-management, weight loss and physical exercise (9). Exercise is a core recommendation in all non-pharmacological guidelines for the management of patients with knee or hip OA as it focuses on strengthening muscles and improving the range of motion and can also contribute to ameliorating pain and function.
Nevertheless, physical therapy alone does not always provide sufficient pain relief and patients turn to pharmacological solutions such as acetaminophen, nonsteroidal anti-inflammatory drugs (NSAIDs) and/or cyclo-oxygenase 2 (COX-2) selective inhibitors. While effective in relieving pain and reducing stiffness and swelling, the associated possible cardiovascular, gastrointestinal and renal toxicities (10–12) mean caution should be exercised in prescribing these therapies, particularly in the elderly population and alternative solutions sought.
Another non-pharmacological option used for reducing pain and maintaining hip mobility is viscosupplementation, the administration of a hyaluronic acid (HA) preparation into the affected joint to supplement the viscoelasticity of the diseased synovial fluid. Published data suggest that intra-articular injections of HA in hip OA are effective in the relief of pain (13–15).
Studies comparing a combination of intra-articular HA injections and exercise to exercise alone in patients with knee OA showed promising results (16, 17). However, no similar studies have been performed in hip OA.
The present study aimed to evaluate the effectiveness of Hyalubrix®, combined with exercise therapy in the treatment of hip osteoarthritis.
The primary objective was to achieve an enduring reduction in OA symptoms related to pain during activity. Secondary objectives were the evaluation of hip disability, OA related pain, patients’ daily functioning and NSAIDs intake. The rationale of the study was that the combined approach could produce a synergic effect both on pain and in muscle strengthening allowing the patient to return to his/her daily and working activities.
Materials and methods
This single site, open-label, investigator-initiated, prospective study was designed to assess the effectiveness of intra-articular injections of Hyalubrix® in combination with exercise therapy in the treatment of hip osteoarthrosis.
The study was conducted between February 2011 and December 2012 and a total of 40 patients was enrolled.
The study was conducted in accordance with the 1964 Helsinki Declaration and subsequent amendments and the principles of Good Clinical Practice.
Patients referred to the site for treatment of hip OA were considered for the study. Before performing any study procedure and after the Clinical Investigator had explained the nature, aim, procedures and possible risks of the study, each patient was asked to give written consent to participate.
Inclusion criteria were: subject between 35 and 85 years of age suffering from hip osteoarthrosis with a Kellgren-Lawrence grade > 1 and providing signed informed consent. Subjects with any of the following conditions were not eligible to enter the study: neoplasia, cognitive impairment, pace-maker implant.
The hyaluronic acid test product was Hyalubrix®, a CE certified class III medical device, consisting in a sterile, nonpyrogenic, viscoelastic solution manufactured with Hyaluronic acid obtained by bacterial fermentation from a fraction of high molecular weight. Hyalubrix®, due to its viscosity and elasticity, exerts the same lubricating and shock absorbing functions as the synovial fluid does in normal joints to protect cartilage and soft tissues against mechanical injuries. As a synovial fluid temporary substitute, Hyalubrix® is indicated in patients affected by degenerative or mechanical arthropathy.
Each subject underwent three ultrasound image-guided injections of Hyalubrix®, using an anterior approach with a 20-gauge spinal needle after betadine preparation.
Injections were performed at 45-day intervals (T0, T1, T2) and were administered by the same experienced physician on patients in a supine position.
Excessive weight bearing and strenuous activity were discouraged for 48 hours after each injection.
In the event of bilateral hip osteoarthrosis, the most painful hip was treated first and treatment of the contralateral hip was started once the treatment of the first hip had been completed.
One week after receiving the first injection, all entered patients started physical therapy consisting in 3 sessions a week up to a total of 30 sessions (10 consecutive weeks).
Physical therapy focused on the following:
- proprioceptive rehabilitation of the lower limbs;
- gait training;
- balance training.
Patients were also instructed to perform home-based exercise regularly.
Assessment of clinical outcome and safety
Clinical evaluations were performed at baseline and after each intra-articular injection. Forty-five days and sixty days after the last injection, the patient returned to the clinic to perform a follow-up and final visit.
The following assessments were performed to evaluate the primary and secondary endpoints.
Pain during activity (primary endpoint) and at rest (secondary endpoint) were investigated by the Visual Analogue Scale (VAS) consisting in a line ranging from 0 cm, indicating the absence of pain, to 10 cm indicating unbearable pain. At each visit the patients were asked to respond in terms of their pain “at the present time” by indicating on the VAS their perceived pain, both during activity and at rest.
Hip disability was investigated in terms of range of motion (ROM), measured at each study time point by a goniometer and the results, expressed as degrees, recorded in the patient’s medical charts. Muscle and functional impairment were also assessed by means of the Thomas Test, the Trendelenburg Test and assessment of muscle hypotonia.
Normal values of hip ROM (18) were: Flexion: 125°, Extension: 10–15°, Abduction: 45°, Internal Rotation: 45°, External Rotation: 45°.
The Thomas test is a physical examination used to identify unilateral fixed flexion deformity of the hip. The test is performed by putting the patients in a supine position and asking him to bring one knee in the direction of the chest/flexes hip while the other leg remains extended. By passing the palm of the hand beneath the patient’s spine the clinician can identify lumbar lordosis evidencing, if positive, the fixed flexion deformity of the hip.
Painful hip disorders such as osteoarthritis may lead to a deficiency in the abductor mechanism of the hip. The Trendelenburg test is used to evaluate the strength of the abductor muscles of the hip, namely the gluteus medius and minimus, which play an important role during the stance phase of the gait cycle to maintain both hips at the same level. The Trendelenburg sign is said to be positive if, when standing on one leg, the pelvis drops on the side opposite to the stance leg to reduce the load by decreasing the lever arm. A positive Trendelenburg test therefore indicates a deficiency of the hip muscle.
At each study visit the presence/absence of hypotonia of the gluteal muscles and the quadriceps femoris muscle was assessed and recorded in the patient’s medical charts.
OA related pain was investigated in term of VAS at rest as well as the FABER test, a physical examination used to assess for the sacroiliac joint or hip joint being the source of the patient’s pain.
The patient’s tested leg is placed in a “figure - 4” supine position, where the knee is flexed and the ankle is placed on the opposite knee. The hip is placed in flexion, abduction, and external rotation (which is where the name FABER comes from). The examiner applies a posteriorly directed force against the medial knee of the bent leg towards the table top. A positive test occurs when groin pain or buttock pain is produced. Due to forces going through the hip joint as well, the patient may experience pain if the pathology is located in the hip as well.
Patient daily functioning, specifically the activities of daily living and mobility, was assessed during the study by the Barthel Index and Lequesne Index.
The Barthel Index is a questionnaire consisting in 10 items evaluating feeding, moving from wheelchair to bed and return, grooming, transferring to and from a toilet, bathing, walking on a level surface, going up and down stairs, dressing, continence of bowels and bladder and it is particularly helpful in monitoring improvement in activities of daily living over time.
The scores for each of the items are summed to create a total score. The higher the score the more “independent” the patient is. Independence means that the person needs no assistance with any part of the task.
The Lequesne Index is a 10-question survey given to patients with hip OA to investigate functional impairment. It consists in 5 questions pertaining to pain or discomfort, 1 question dealing with maximum distance walked, and 4 questions about activities of daily living. The total questionnaire is scored on a 0 to 24 scale. Lower scores indicate there is less functional impairment.
At each study visit the patient was asked about the NSAIDs intake since the previous visit. Intake was recorded in terms of yes/no.
Sample size and statistical analysis
Sample size was decided a priori and fixed at 40 treated patients as this was an exploratory Investigator-initiated study with no control group.
The Full Analysis Set, which included all subjects receiving treatment (Hyalubrix® and exercise), was considered for the statistical analysis performed on absolute values or on changes from baseline, as applicable, and at a level of significance adjusted for the number of comparisons. All comparisons were performed considering the Visit 0 as baseline. Demographic data were calculated on the 40 enrolled patients, descriptive and inferential statistics referred to coxarthrosis parameters were calculated on the 65 treated hips.
Descriptive statistics were produced at all time points. The last patient assessment (105 days after last injection) was labelled as Tfinal.
To describe the subjects’ conditions before treatment and demographic data, summary statistics (mean, median, standard deviation, minimum and maximum) were calculated for continuous variables and the number and percentage of events/patients in each category provided for categorical data.
Summary statistics (mean, median, standard deviation, minimum and maximum or number and percentage of patients) were calculated for performance variables at all time points. An analysis of variance for repeated measures was conducted on continuous variables to compare values at each time point against baseline; a McNeemar test was performed on dichotomous variables to assess changes from baseline. Analysis of variance for repeated measures was conducted considering time, gender, age group, BMI group and hypertension co-morbidity as factors.
Results
Forty patients were enrolled and performed the study in the period from February 2011 up to December 2012, for a total of 65 hips treated.
Baseline characteristics
All 40 subjects consenting to participate in the study and treated with the study product attended all the study visits and underwent 30 sessions of physical therapy. Among the 40 patients, 15 were treated in one hip only, while 25 were affected by bilateral coxarthrosis and received Hyalubrix®, injections in both hips.
There was a slightly higher number of female participants (58%). Included patients had a mean age of 61 years (s.d. 11.0; range 38–81) and a BMI of between 25 and 35 in 59% of cases. Almost all patients (95%) were non-smokers. The most frequent diseases affecting the patients at study entry were hypertension (65%) and heart disease (28%).
The disease characteristics and hip osteoarthritis symptoms at baseline are reported in Tables 1 and 2.
Table 1.
Disease characteristics of the 65 treated hips.
| n (%) | ||
|---|---|---|
| Hip | Monolateral | 15 (23.1) |
| Bilateral | 50 (76.9) | |
| Kellgren-Laurence | II | 24 (36.9) |
| Grade | III | 40 (61.5) |
| IVa | 1 (1.5) | |
| Presence of Hypotonia | Quadriceps | 11 (16.9) |
| Gluteal | 13 (20.0) | |
| Positive Test | Thomas | 59 (90.8) |
| FABER | 59 (90.8) | |
| Trendelenburg | 46 (70.8) | |
| NSAIDs intake | Yes | 39 (60.0) |
The one patient with a Kellgren-Laurence grade of IV in one of the two hips affected by OA received treatment with Hyalubrix® as the patient could not undergo surgery.
Table 2.
Hip osteoarthritis symptoms at baseline.
| mean | ± (s.d.) | |
|---|---|---|
| VAS during activity (cm) | 6.94 | (2.053) |
| VAS at rest (cm) | 6.18 | (2.537) |
| Barthel Index | 92.27 | (6.481) |
| Lequesne Index | 12.92 | (4.216) |
| Flexion (°) | 100.31 | (9.138) |
| Extension (°) | 13.77 | (5.156) |
| Adbuction (°) | 31.00 | (6.072) |
| Internal Rotation (°) | 15.92 | (7.649) |
| External Rotation (°) | 30.62 | (6.405) |
Clinical outcome
OA related pain
During the course of the study the pain perceived by the patient during activity dropped from a mean value of 6.94 cm (s.d. 2.053; range: 1–10) to a mean value of 1.46 cm (s.d. 1.393; range 0–6). The decrease was statistically significant from T1 compared to baseline (p < 0.05) and was confirmed at all of the subsequent time points (p<0.001).
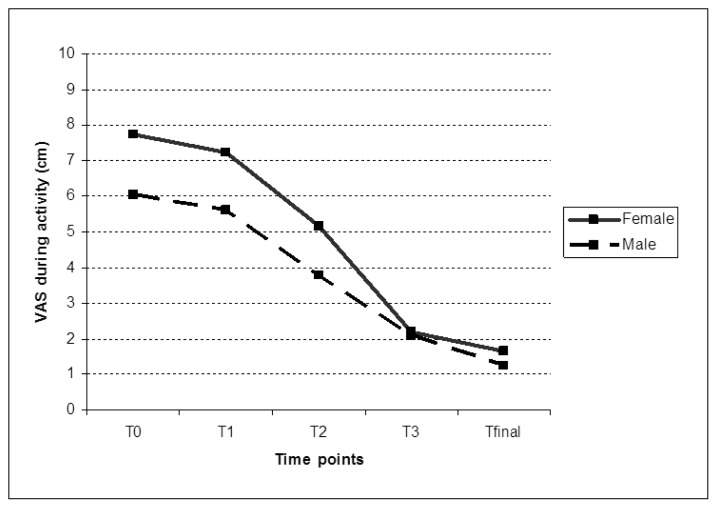
The analysis of the variance for repeated measures considering time, age group, BMI group and presence of hypertension as factors evidenced an interaction between time and gender.
Pain during activity decreased over time, but in female patients a higher decrease at T3 and Tfinal occurred compared to male patients: a mean change from baseline of 5.5 cm at T3 and 6.09 cm at Tfinal was observed in female patients, against a mean change of 3.97 cm at T3 and 4.81 cm at Tfinal in male patients (p< 0.05).
However, when considering the pain perceived during activity at baseline in male and female patients, it can be noted that female patients perceived greater pain during activity than male patients with a mean value of 7.74 cm (s.d. 1.88; range 1–10) against a mean value of 6.06 cm (s.d. 1.896; range: 2 – 10 cm) registered in male patients. It is therefore reasonable to believe that the time and gender interaction is due to the higher values in pain VAS during activity reported at baseline by female patients.
Figure 1 shows the VAS pain values during activity reported at each study time point by gender.
Figure 1.
VAS pain during activity at study time points by gender.
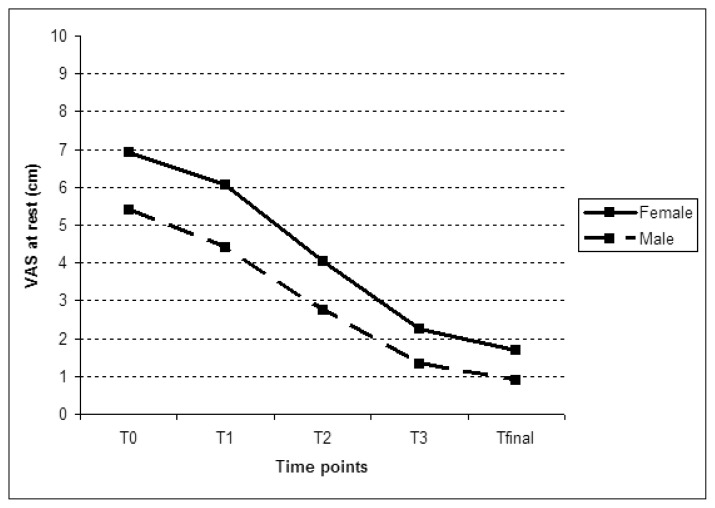
The effect of Hyalubrix® combined with physical exercises on pain at rest was similar to that observed on pain during activity.
VAS pain at rest decreased from a mean value of 6.18 (s.d. 2.537; range: 1–10 cm) reported at baseline to a mean value of 1.31 (s.d. 1.478; range: 0–9 cm) at Tfinal. The decrease at T1 compared to baseline was statistically significant (p < 0.05) and was confirmed at all of the subsequent time points (p<0.001). At baseline female patients reported a higher mean value in VAS at rest than male patients: 6.91 cm (s.d. 2.391; range: 1–10 cm) and 5.39 cm (s.d. 2.486; range 1–9 cm) respectively. The time and gender interaction evidenced by the analysis of variance for repeated measures is due to the lack of homogeneity of the variable at baseline.
Figure 2 shows the VAS pain values at rest reported at each study time point by gender.
Figure 2.
VAS pain at rest at study time points by sex.
Hip disability
The range of motion of treated hips improved during the study: flexion, extension, abduction, internal and external rotation reported at the end of the study showed a mean increase compared to baseline of 16.23° (s.d. 8.884; range: 0–35°), 8.00° (s.d. 7.385; range: −15–20 °), 11.15 (s.d. 6.298; range: 0–30), 11.77° (s.d. 8.359; range: −25–25°) and 8.69° (s.d. 6.267; range: −15–20°), respectively (Table 3).
Table 3.
Hip disability: range of motion - mean values at each time point.
| T0 | T1 | T2 | T3 | Tfinal | |
|---|---|---|---|---|---|
| Flexion (°) | 100,31 | 100,85 | 107,00 | 114,62 | 116,54 |
| Extension (°) | 13,77 | 12,62 | 15,77 | 18,69 | 21,77 |
| Abduction (°) | 31,00 | 32,00 | 35,85 | 41,25 | 42,15 |
| Internal Rotation (°) | 15,92 | 14,38 | 18,62 | 25,00 | 27,69 |
| External Rotation (°) | 30,62 | 30,46 | 34,15 | 39,31 | 39,31 |
Improvement in flexion, extension, internal and external rotation movements were statistically different from baseline from T2 (p< 0.001), while abduction improved from T1 (p<0.05).
No correlation with gender, age group, BMI group or hypertension emerged.
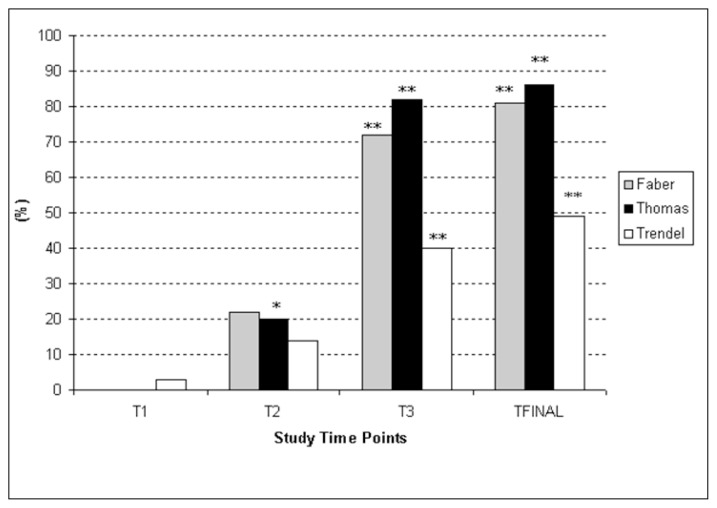
At baseline 91% of cases was positive to the Thomas Test, the percentage dramatically decreased over time reaching 5% at the final visit in three cases. The McNemar test showed a statistically significant difference compared to baseline from T2 (p< 0.0125) that was maintained at subsequent study time points (p<0.001).
Similarly, the percentage of positive Trendelenburg Test cases decreased from 71% at baseline to 23% at Tfinal. The McNemar test showed a statistically significant difference compared to baseline from T3 (p< 0.001) and was maintained at subsequent study time points.
The number of patients reporting pain on the hip joint at the FABER test decreased from T2, but became statistically significant after the third injection (T3 p< 0.001) and remained significant at Tfinal (p< 0.001) when compared to baseline: the percentage of patients previously positive to the test that became negative were 72% at T3 and 82% at Tfinal.
The percentages of cases changing from a positive test (Faber, Thomas and Trendelenburg) at baseline to a negative test at the subsequent time points are displayed in the Figure 3.
Figure 3.
Percentage improvement in the FABER, Thomas and Trendelenburg Test at each study time point.
* significant improvement compared to baseline (p<0.0125)
** significant improvement compared to baseline (p<0.001)
Patient’s daily functioning
The mean Lequesne index value of 12.9 (s.d. 4.2164; range: 4.00–19.50) at baseline progressively decreased to a mean value of 5.5 (s.d. 2.5731; range:1.5–14.5) at Tfinal. The decrease was statistically significant at T1 compared to baseline and was confirmed at all of the subsequent time points (p<0.001).
During the course of the study an increase in the Barthel Index at different study time points was observed: the mean value of 92.27 (s.d. 6.481; range: 75–100) registered at baseline increased up to a mean value of 97.23 (s.d. 3.191; range: 90–100) at Tfinal. The increase was statistically significant from T2 compared to baseline and was confirmed at all of the subsequent time points (p<0.001).
The changes from baseline observed after the first, second and third injection and at the final time point are reported in Table 4.
Table 4.
Patient’s Daily Functioning: Barthel and Lequesne Indices - mean values at each time point.
| T0 | T1 | T2 | T3 | Tfinal | |
|---|---|---|---|---|---|
| Barthel Index | 92,27 | 92,27 | 94,15 | 96,54 | 97,23 |
| Lequesne Index | 12,915 | 11,531 | 8,989 | 6,800 | 5,508 |
NSAIDs intake
At study entry more than half of the patients declared they were taking NSAIDs to alleviate pain symptoms (60% of cases).
At T3, 54% of the patients who had been taking NSAIDs before entering the study declared they had stopped intake and at the final observation (Tfinal) the percentage, among those patients taking NSAIDs before entering the study, further increased up to 55% (p<0.001 against baseline).
Safety
The treatment was well tolerated.
Mild transient adverse events were reported in 3 patients. These device-related local AEs consisted mostly of mild or moderate post injection pain and swelling which resolved spontaneously after a few days. Patients’ daily activities were unaffected by these events.
No serious adverse events were reported by the patients during the treatment.
Discussion and overall conclusions
Hip osteoarthritis is a degenerative disease which leads to loss of joint functioning. Treatment of symptomatic osteoarthritis includes educating the patient and continues with stretching, physical exercise, weight reduction, technical aids and analgesics. Subsequent options are treatment with viscosupplementation, paracetamol, NSAIDs and possibly opiates and finally insertion of an artificial joint.
Studies have demonstrated that viscosupplementation with hyaluronic acid may be effective in relieving hip osteoarthritis pain. However, exercise is also an important factor particularly amongst the elderly population who may have multiple co-morbidities affecting their mobility.
The present study therefore aimed to evaluate the effectiveness of Hyalubrix® combined with exercise therapy in the treatment of hip osteoarthritis. The rationale of the study was that the combined approach could produce a synergic effect both on pain and in strengthening muscles allowing the patient to return to his/her daily and working activities.
Results from this study including 40 patients for a total of 65 treated OA hips demonstrated a significant improvement in OA related pain, hip disability, patient’s daily functioning as well as a reduction in NSAIDs intake in patients receiving both Hyalubrix® and exercise therapy.
The reduction in VAS pain (both during activity and at rest), was already evident at the first assessment after the start of both treatments (45 days), while changes in the FABER test appeared at a later stage (135 days).
Abduction movements had improved at the first visit after the start of both treatments (45 days) thus resulting in a reduction in the Lequesne Index and improvement in patients’ functional activities. Improvement in flexion, extension, internal and external rotation occurred after two treatment sessions.
Deficiency in the hip related muscles only ameliorated as evidenced by the Trendelenburg test from day 135 onwards (T3), although gluteal and quadriceps muscles hypotonia showed no change from baseline conditions throughout the study.
Furthermore, the number of patients resorting to NSAIDs during the study decreased significantly from 135 days after starting injections and physical therapy.
The study data suggest that the pain reduction that occurs early in the treatment period allows the patient to undergo physical exercises leading to a significant improvement in hip range of motion and functional impairment right from the first assessment visit (45 days). Following the two Hyalubrix® injections and the compliance with the exercise program, the patient became more independent in the activities of daily living leading to a significant improvement in muscular deficiency and a reduction in NSAIDs intake shown after the third Hyalubrix® injection.
All these positive effects are still present at the final visit performed 105 days after the last Hyalubrix® injection.
Another strength of this study is the high patient compliance. The intra-articular administration using Hyalubrix® means just 3 injections can be performed every 45 days rather than more frequently as is the case with the 60 mg formulations used in many other published studies. Pain is reduced from the first injection and is maintained throughout the period, thus enabling optimal performance of the physical exercises with consequent greater recovery of joint range of motion and resolution of antalgic contractures and incorrect posture. The effect of the hyaluronic acid therefore enables the patient to comply better with the rehabilitation therapy, synergising the two therapeutic effects.
It could therefore be concluded that patients suffering from hip OA seem to benefit from the treatment with Hyalubrix® injections plus exercise therapy; however a further controlled study is indicated to evaluate the synergic effect of the two combined treatments.
Footnotes
Conflict of interest
The Authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
References
- 1.Felson DT. Epidemiology of hip and knee osteoarthritis. Epidemiol Rev. 1988;10:1–28. doi: 10.1093/oxfordjournals.epirev.a036019. [DOI] [PubMed] [Google Scholar]
- 2.Ingvarsson T, Hagglund G, Lohmander LS. Prevalence of hip osteoarthritis in Iceland. Ann Rheum Dis. 1999;58:201–207. doi: 10.1136/ard.58.4.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roux C, Saraux A, Mazieres B, Pouchot J, Morvan J, Fautrel B, et al. KHOALA Osteoarthritis Group. Screening for hip and knee osteoarthritis in the general population: predictive value of a questionnaire and prevalence estimates. Ann Rheum Dis. 2008;67:1406–1411. doi: 10.1136/ard.2007.075952. [DOI] [PubMed] [Google Scholar]
- 4.Nho SJ, Kymes SM, Callaghan JJ, Felson DT. The burden of hip osteoarthritis in the United States: epidemiologic and economic considerations. J Am Acad Orthop Surg. 2013;21(Suppl 1):S1–6. doi: 10.5435/JAAOS-21-07-S1. [DOI] [PubMed] [Google Scholar]
- 5.Felson DT. Osteoarthritis: new insights. Ann Intern Med. 2000;133:635–646. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- 6.Yelin E, Murphy L, Cisternas MG, Foreman AJ, Pasta DJ, Helmick CG. Medical care expenditures and earnings losses among persons with arthritis and other rheumatic conditions in 2003, and comparisons with 1997. Arthritis Rheum. 2007;56:1397–1407. doi: 10.1002/art.22565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dougados M, Hochberg MC. Management of osteoarthritis. In: Hochberg MC, Silman AJ, Smolen JS, Weinblatt ME, Weisman M, editors. Rheumatology. 5th ed. Philadelphia: Mosby/Elsevier; 2011. pp. 1793–1799. [Google Scholar]
- 8.Mushtaq S, Choudhary R, Scanzello C. Non-surgical treatment of osteoarthritis-related pain in the elderly. Curr Rev Musculoskelet Med. 2011;4:113–122. doi: 10.1007/s12178-011-9084-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang W, Nuki G, Moskowitz RW, et al. OARSI recommendations for the management of hip and knee osteoarthritis. Part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis and Cartilage. 2010;18:476–499. doi: 10.1016/j.joca.2010.01.013. [DOI] [PubMed] [Google Scholar]
- 10.Chan AT, Manson JE, Albert CM, et al. Nonsteroidal antiinflammatory drugs, acetaminophen, and the risk of cardiovascular events. Circulation. 2006;113:1578–1587. doi: 10.1161/CIRCULATIONAHA.105.595793. [DOI] [PubMed] [Google Scholar]
- 11.Rahme E, Barkun A, Nedjar H, et al. Hospitalizations for upper and lower GI events associated with traditional NSAIDs and acetaminophen among the elderly in Quebec, Canada. Am J Gastroenterol. 2008;103:872–882. doi: 10.1111/j.1572-0241.2008.01811.x. [DOI] [PubMed] [Google Scholar]
- 12.Curhan GC, Knight EL, Rosner B, et al. Lifetime nonnarcotic analgesic use and decline in renal function in women. Arch Intern Med. 2004;164:1519–1524. doi: 10.1001/archinte.164.14.1519. [DOI] [PubMed] [Google Scholar]
- 13.Abate M, Scuccimarra T, Vanni D, et al. Femoroacetabular impingement: is hyaluronic acid effective? Knee Surg Sports Traumatol Arthrosc. 2014;22(4):889–892. doi: 10.1007/s00167-013-2581-1. [DOI] [PubMed] [Google Scholar]
- 14.Migliore A, Bizzi E, Massafra U, et al. The impact of treatment with hylan G-F 20 on progression to total hip arthroplasty in patients with symptomatic hip OA: a retrospective study. Curr Med Res Opin. 2012;28(5):755–760. doi: 10.1185/03007995.2011.645563. [DOI] [PubMed] [Google Scholar]
- 15.Migliore A, Massafra U, Bizzi E, et al. Intra-articular injection of hyaluronic acid (MW 1,500 – 2,000 kDa; HyalOne) in symptomatic osteoarthritis of the hip: a prospective cohort study. Arch Orthop Trauma Surg. 2011;131(12):1677–1685. doi: 10.1007/s00402-011-1353-y. [DOI] [PubMed] [Google Scholar]
- 16.Huang MH, Yang RC, Lee CL, Chen TW, Wang MC. Preliminary results of integrated therapy for patients with knee osteoarthritis. Arthritis 8Rheum. 2005;53(6):812–820. doi: 10.1002/art.21590. [DOI] [PubMed] [Google Scholar]
- 17.Bayramoğlu M, Karataş M, Cetin N, Akman N, Sozay S, Dilek A. Comparison of two different viscosupplements in knee osteoarthritis — a pilot study. Clin Rheumatol. 2003;22(2):118–122. doi: 10.1007/s10067-002-0691-0. [DOI] [PubMed] [Google Scholar]
- 18.Daniels L, Wonhingham C. Muscle Testing: Techniques of Manual Examination. 3rd ed. Philadelphia, Pa: WB Saunders Co; 1972. [Google Scholar]