Summary
A schwannoma is a rare, benign tumor originating from Schwann cells of peripheral nerve sheath. It commonly occurs in subjects between 20 and 50 years of age, and its malignant transformation is exceptional. While schwannomas usually affect the head and neck region, localization in the lower extremity is exceptionally rare, and even fewer cases have described schwannomas occurring in the foot.
We report a case of a giant schwannoma of the foot diagnosed in a 65-year-old woman.
A giant schwannoma of the foot is an extremely rare soft tissue tumor. MRI may allow an earlier diagnosis and provide valuable information about the size and possible bone invasion. This case report noted that a complete excision of the schwannoma may prevent the risk of local recurrence, regardless of its size.
Keywords: giant schwannona, forefoot, magnetic resonance imaging
Introduction
A schwannoma is a rare, benign tumor originating from Schwann cells of peripheral nerve sheath. It commonly occurs in subjects between 20 and 50 years of age, and its malignant transformation is exceptional (1). While schwannomas usually affect the head and neck region, localization in the lower extremity is exceptionally rare (2), and even fewer cases have described schwannomas occurring in the foot (3).
We report a case of a giant schwannoma of the foot diagnosed in a 65-year-old woman.
Case report
A 65-year-old woman was admitted to our institution complaining of a painful swelling of the right foot for 5 years, resulting in both a distress in weight-bearing and a disturbance of activities of daily living. The patient’s medical, development and family histories were unremarkable. Physical examination showed a huge rubbery mass located in the medial and plantar aspect of the foot, that was fixed to the skin and underlying tissues and was associated with an intermittent dysesthesia along the plantar aspect of the first metatarsal ray.
Magnetic resonance imaging (MRI) scans demonstrated a 12 × 8 × 5 cm soft tissue mass located in the medial and plantar aspect of the foot, extended from posterior to the calcaneocuboid joint to distally to the neck of the second metatarsal and into the first and second intermetatarsal space. The mass originated from the medial plantar nerve (i.e., one of 2 terminal branches of tibial nerve) and involved its common digital branches. It had a multilobular morphology and was characterized by a heterogeneous intermediate signal intensity on T1-weighted scans (Figure 1 a, b) and a homogeneous high signal intensity on T2-weighted scans (Figure 1 c, d).
Figure 1.
T1-wheigthed MRI scans: a) coronal view, b) axial view; T2-wheighted MRI scans: c) sagittal view, d) axial view.
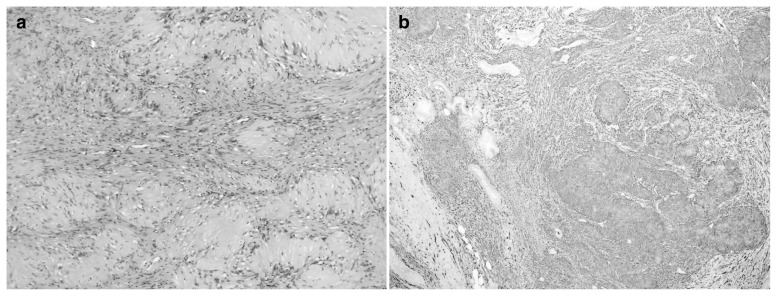
Histopathologic examination of a core biopsy specimen resulted in a benign neurinoma, as characterized by a proliferation of spindle cells with a biphasic pattern consisting of hypercellular areas with nuclear palisading and hypocellular areas with a loose stroma (i.e., the so called Antoni A and Antoni B areas, respectively). Cells showed a rare mitotic activity and there were no atypical nuclei (Figure 2 a). Immunohistochemical staining for S100 protein was diffusely and strongly positive (Figure 2 b). Biopsy results were discussed with the patient and the potential risks and benefits of a surgical excision of the mass were considered. As an alternative, a foot amputation was not taken into account due to the histological benignity of the mass.
Figure 2.
a) Hematoxylin and eosin stain photomicrograph of the schwannoma. b) S100 protein stain photomicrograph of the schwannoma.
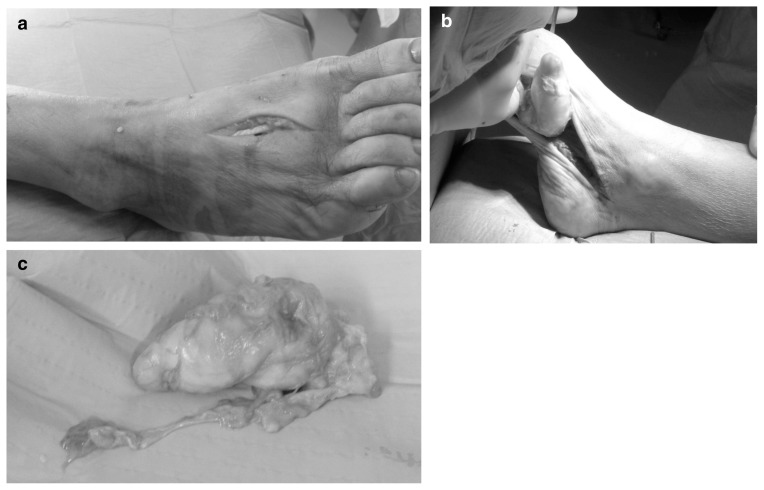
The surgery was performed under spinal anesthesia with the patient placed in a supine position and a pneumatic tourniquet inflated at 100 mmHg higher than the systolic pressure that was measured at the arm of the patient. A preliminary dissection was performed through an intermetatarsal approach, in order to release the mass from the metatarsals (Figure 3 a). Thereafter, a complete surgical excision was performed through a medial longitudinal incision along the medial plantar arch of the foot (Figure 3 b). The medial plantar nerve and its common digital branches were completely invaded by the mass, and we were not able to detect any effective cleavage plane to perform a microsurgical dissection. Hence, we decided to perform an en bloc resection with the sacrifice of the encased nerve. The mass appeared capsulated, white, and glistening (Figure 3 c). A final histopathologic examination of the whole excised mass was carried out, and the pathologist ultimately diagnosed a schwannoma.
Figure 3.
Surgical approach to the schwannoma: a) intermetatarsal approach, b) medial approach, c) macroscopic aspect of the excised schwannoma.
At the latest available examination 9 months postoperatively, the patient had a painless foot with a mild, persistent hypoesthesia along the medial aspect of the first and second metatarsal rays. No signs of local recurrence of disease were manifested.
Discussion
This report describes a case of a giant schwannoma of the foot, thus being clearly atypical for both localization and size. In a previous large cohort of schwannomas by Das Gupta et al. (4), most of the tumors occurred in the head and neck region, while only 14% of them located in the lower extremity, but no localizations in the foot were recorded. Spiegl et al. (5) previously published a series of schwannomas of the lower extremity, and only 11% of them occurred in the foot.
The average length of a schwannoma in the foot or ankle is 1.5 to 2 cm (6). Despite schwannomas can vary in size from a few millimeters to more than 20 cm, the majority of them are smaller than 5 cm (4), whereas those larger are termed giant schwannomas (7).
To the best of our knowledge, as shown in Table 1 only 6 giant schwannomas of the foot have been reported to date (1–3, 6, 8, 9). Mangrulkar et al. (3) described a 14 × 5 × 8 cm multinodular schwannoma of the medial and plantar aspect of the foot, involving both the ankle and the intermetatarsal spaces, that was characterized by a local recurrence 9 months postoperatively. Overall, the recurrence rate accounts for less than 5% of schwannomas in the available literature, and seems to be prevented through a complete excision (10).
Table 1.
Case reports describing giant schwannomas of the foot.
| Article | Year | Localization | Size | Bone invasion | Local recurrence |
|---|---|---|---|---|---|
| Torossian et al. (2) | 2001 | heel | 7.5 × 5.5 × 5 cm | no | no |
| Pasternack et al. (6) | 2005 | dorsal aspect of the foot | 8 × 4.5 × 2.5 cm | no | no |
| Mangrulkar et al. (3) | 2007 | medial aspect of the ankle and hindfoot | 14 × 5 × 8 cm | no | yes |
| Ansari et al. (8) | 2014 | dorsomedial aspect of the foot | 7 × 6 cm | yes | no |
| Flores Santos et al. (1) | 2014 | lateral and plantar aspect of the foot | 7 × 2.5 × 3 cm | yes | no |
| Wang et al. (9) | 2016 | dorsal aspect of the foot | not available | yes | no |
Three previous case reports (1, 8, 9) described giant schwannomas of the foot with a diffuse bone invasion. One should debate on whether these schwannomas were primarily intraosseous tumors with cortical disruption or aggressive soft tissue masses; this latter speculation often leads to the suspicion of malignancy (1). Actually, malignant transformation of a solitary schwannoma is extremely rare, and a differential diagnosis with malignant peripheral nerve sheath tumors (i.e., sarcomas originating from peripheral nerves or from cells associated with the nerve sheath) should be considered. Clinical presentation of such malignant tumors often deals with a rapidly enlarging mass. Histopathologic examination shows dense cellular fascicles alternating with myxoid regions. Cells may have a spindle-like, round or fusiform shape. Nuclear palisading is very rare compared to schwannoma and occurs in only 10% of cases. Malignancy is suggested by nuclear pleomorphism, necrosis, and mitotic activity.
As a main differential diagnosis, benign peripheral nerve sheath tumors includes both schwannomas and neurofibromas. In clinical practice, the distinction between these tumors is usually made with MRI. Indeed, neurofibromas may demonstrate an area of low signal intensity centrally and higher signal intensity peripherically on T2-weighted scans (i.e., the so-called target sign). The ultimate diagnosis relies on both histopathology and immunohistochemistry, being the diagnosis of a neurofibroma allowed with the recognition of spindle cells in a myxoid stroma with some collagen fibers, and a negativity or weak positivity of the immunohistochemical staining for S100 protein.
In the majority of cases, schwannomas can be easily enucleated through microsurgical dissection without damaging the nerve contiguity. However, due to the exceptionality of the current case in terms of both dimension and local aggressiveness with a complete disruption of the nerve, we decided to perform an en bloc excision of the schwannoma with the sacrifice nerve encased in the mass. As a further procedural alternative for such a borderline mass, a foot amputation should be proposed; however, considering the histological benignity of the schwannoma this possibility was not taken into account.
In summary, a giant schwannoma of the foot is an extremely rare soft tissue tumor. MRI may allow an earlier diagnosis and provide valuable information about the size and possible bone invasion. This case report noted that a complete excision of the schwannoma may prevent the risk of local recurrence, regardless of its size.
References
- 1.Flores Santos F, Pinheiro M, Felicissimo P. Large foot schwannoma with bone invasion - A case report. Foot Ankle Surg. 2014;20:e23–e26. doi: 10.1016/j.fas.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 2.Torossian JM, Augey F, Salle M, Beziat JL. Giant foot schwannoma. Br J Plast Surg. 2001;54:74–76. doi: 10.1054/bjps.1999.3478. [DOI] [PubMed] [Google Scholar]
- 3.Mangrulkar VH, Brunetti VA, Gould ES, Howell N. Unusually large pedal schwannoma. J Foot Ankle Surg. 2007;46:398–402. doi: 10.1053/j.jfas.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Das Gupta TK, Brasfield RD, Strong EW, Hadju SI. Benign solitary schwannomas (neurilemomas) Cancer. 1969;24:355–366. doi: 10.1002/1097-0142(196908)24:2<355::aid-cncr2820240218>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 5.Spiegl PV, Cullivan WT, Reiman HM, Johnson KA. Neurilemoma of the lower extremity. Foot Ankle. 1986;6:194–198. doi: 10.1177/107110078600600404. [DOI] [PubMed] [Google Scholar]
- 6.Pasternack WA, Winter-Reiken DJ. Unusually large cellular schwannoma of the foot. J Am Podiatr Med Assoc. 2005;95:157–160. doi: 10.7547/0950157. [DOI] [PubMed] [Google Scholar]
- 7.Ritt MJ, Bos KE. A very large neurilemmoma of the anterior interosseous nerve. J Hand Surg Br. 1991;16:98–100. doi: 10.1016/0266-7681(91)90141-a. [DOI] [PubMed] [Google Scholar]
- 8.Ansari MT, Rastogi S, Khan SA, Yadav C, Rijal L. Giant schwannoma of the first metatarsal: a rare entity. J Foot Ankle Surg. 2014;53:335–359. doi: 10.1053/j.jfas.2014.01.014. [DOI] [PubMed] [Google Scholar]
- 9.Wang G, Wen X, Qu L, Qi X, Yang C. Intraosseous schwannoma involving multiple bones of the foot: a case report. J Foot Ankle Surg. 2016;55:201–206. doi: 10.1053/j.jfas.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Odom RD, Overbeek TD, Murdoch DP, Hosch JC. Neurilemoma of the medial plantar nerve: a case report and literature review. J Foot Ankle Surg. 2001;40:105–109. doi: 10.1016/s1067-2516(01)80052-1. [DOI] [PubMed] [Google Scholar]