Abstract
Purpose
Disordered eating is more prevalent among adolescents with attention deficit/hyperactivity disorder. Both inattention and hyperactivity/impulsivity symptoms show strong associations with disordered eating, but few investigations of these associations have been longitudinal. Thus, we examined the effect of childhood-to-adolescent inattention and hyperactivity/impulsivity symptom trajectories on late adolescent disordered eating.
Methods
We used growth mixture modeling to identify distinct inattention and hyperactivity/impulsivity symptom trajectories (called “classes”) across three time points (ages 8–9, 13–14, and 16–17) in the Swedish Twin study of CHild and Adolescent Development. The resulting classes were used to predict Eating Disorder Inventory-2 (EDI) Bulimia, Drive for Thinness, and Body Dissatisfaction subscales at age 16–17, with adjustment for sex and body mass index (BMI) at age 16–17.
Results
The combined inattention and hyperactivity/impulsivity symptom trajectory classes included: a ‘Low Symptom’ class characterized by low inattention and hyperactivity/impulsivity throughout childhood/adolescence; a ‘Predominantly Inattention’ class characterized by elevated inattention, but not hyperactivity/impulsivity, throughout childhood/adolescence; a ‘Predominantly Hyp/Imp’ class characterized by elevated hyperactivity/impulsivity, but not inattention, throughout childhood/adolescence; and a ‘Both Inattention and Hyp/Imp’ class characterized by elevated inattention and hyperactivity/impulsivity throughout childhood/adolescence. After adjusting for sex and BMI or sex and anxiety/depression symptoms, the ‘Both Inattention and Hyp/Imp’ (versus ‘Low Symptom’) class predicted significantly higher EDI subscale scores during late adolescence.
Conclusions
Increased vigilance for disordered eating among children who have both inattention and hyperactivity/impulsivity symptoms throughout childhood and adolescence could aid in early identification of eating disorders.
Keywords: Attention deficit/hyperactivity disorder, disordered eating, symptom trajectories, longitudinal design, population study
Introduction
Disordered eating is more prevalent among children and adolescents with attention deficit/hyperactivity disorder (ADHD) than the general population (1). Further, several large population-based studies have indicated a prospective relationship between ADHD and varying degrees of subsequent disordered eating (2–7); for instance, girls with ADHD may be up to six times more likely to develop an eating disorder than girls without ADHD (8). In clinical settings, 20–24% of adults with bulimia nervosa retrospectively report having experienced ADHD symptoms during childhood (9, 10), and ADHD symptoms are associated with greater eating disorder severity (10, 11). Whereas ADHD symptoms onset in early childhood, disordered eating tends to onset during adolescence/young adulthood (12). Thus, gaining a better understanding of the nature of the association between ADHD and disordered eating using longitudinal ADHD data could provide important insight into one risk pathway leading to disordered eating and, potentially, the development of full-threshold eating disorders (13).
To date, few studies have evaluated whether it is the inattention versus hyperactivity/impulsivity symptoms of ADHD that serve as a risk factor for disordered eating (2, 3, 6). ADHD is defined by difficulty with self-regulation, specifically in the areas of attention (i.e., inattention) and behavior regulation (i.e., impulsivity), with ADHD-related impairments also observed across a variety of other areas including motivation, emotion regulation, and organizational skills (14). One hypothesis is that impulsivity and the related construct, lack of inhibition, may contribute to disordered eating behaviors such as binge eating (3, 15). Impulsivity is a predictor of eating disorder severity and poor treatment outcome (16), suggesting that impulsivity may influence eating disorders, especially those marked by binge-eating and/or purging behaviors. Another non-mutually exclusive hypothesis is that disordered eating may be influenced by inattentiveness to the internal sense of hunger, satiety, and amount of food consumed on a daily basis, which is also a phenomenon observed in individuals with ADHD (17). Preliminary evidence suggests that disordered eating in individuals with bulimia nervosa is associated with both inattention and hyperactivity/impulsivity; however, the association may be stronger for inattention than for impulsivity/hyperactivity (10).
Although preliminary results support both of the above hypotheses, most studies investigating the relative contributions of inattention and hyperactivity/impulsivity symptoms have examined these symptoms cross-sectionally or retrospectively. The few longitudinal studies conducted to date (2–4, 6, 8) have relied on broad dichotomous classifications of ADHD, thus failing to capture how the specific types of ADHD symptoms relate to disordered eating. Additionally, previous studies (2, 3, 10, 11) often recruited individuals with clinical ADHD and/or eating disorders and did not investigate these symptoms in the community, so it is unknown if these associations generalize to non-clinical populations.
Thus, the goal of the present study was to evaluate whether inattention, hyperactivity/impulsivity, or combined symptoms across childhood and early adolescence played a role in the development of disordered eating in late adolescence in a Swedish community-based cohort. We hypothesized that children with persistently high inattention and hyperactivity/impulsivity trajectories across childhood and early adolescence would be more likely to report disordered eating in late adolescence. In addition, given that ADHD symptoms are associated with higher body mass index (BMI) (18) and that higher BMI is a risk factor for disordered eating (19), we also examined if the relationship between ADHD symptoms and disordered eating remained after adjusting for BMI. Likewise, given that ADHD symptoms are also associated with higher levels of anxiety and depression (20), which are risk factors for disordered eating (21, 22), we also examined if the relationship between ADHD symptoms and disordered eating remained after adjusting for anxiety and depression symptoms.
Methods
Participants
Our study sample consisted of participants from the Swedish Twin Study of CHild and Adolescent Development (TCHAD). TCHAD comprises all twins born between May 1985 and December 1986 in Sweden (23). The Swedish Medical Birth Register (24) was used to identify the twins and their parents, who were invited to participate by completing parent- and self-report questionnaires at four different time points: Wave 1 (ages 8–9), Wave 2 (ages 13–14), Wave 3 (ages 16–17), and Wave 4 (ages 18–19).
For the purpose of this study, we used data collected at Waves 1–3 (see Supplemental Figure 1). Our analysis sample included 2,315 participants (78.4% of the total sample) who had all covariates observed and data on inattention or hyperactivity/impulsivity at at least one time point. Of the included participants, 50.6% were female and 39.9% were monozygotic twins, with the remaining twins belonging to either same- or opposite-sex dizygotic twin pairs. The mean ages at Waves 1, 2, and 3 were 8.7 ± 0.5, 13.7 ± 0.5, and 16.7 ± 0.5 years, respectively.
Consent was obtained from all twins and their parents who participated. Ethical approval for each wave was provided by the Ethics Committee at Karolinska Institutet in Stockholm, Sweden, and the study was approved by the University of North Carolina Institutional Review Board.
Measures
Eating Disorder Inventory-2
The Swedish version of the Eating Disorder Inventory-2 (EDI) (25), which has been validated and shown to have good psychometric properties (26), was used to assess disordered eating attitudes and behaviors by adolescent self-report at Wave 3. Specifically, the 7-item Bulimia (tendency toward episodes of binge eating that may be followed by the impulse to induce vomiting), 7-item Drive for Thinness (excessive concern with dieting, preoccupation with weight, an extreme pursuit of thinness), and 8-item Body Dissatisfaction (belief that specific parts of the body are too large) subscales were administered.
ADHD
The Diagnostic and Statistical Manual of Psychiatric Disorders, 4th edition (27) ADHD criteria were used to develop a 14-item checklist assessing the presence or absence of ADHD symptoms in the previous six-month period. The checklist was administered to parents, who reported on their children at Waves 1, 2, and 3 of TCHAD. Details regarding the development and validation of this checklist, including the inattention (6-items) and hyperactivity/impulsivity (8-items) subscales, have been described in depth elsewhere (28).
BMI
Height and weight were provided via adolescent self-report at Wave 3. We used age- and sex-specific means and standard deviations (SDs) from a sample of Swedish children born in 1981 to remove values 6 SD above and below the mean for height and log(weight) (29). We then used the World Health Organization 2007 package for R to calculate age- and sex-adjusted BMI z-scores (30).
Anxiety and Depression
The 14-item Anxious/Depressed subscale of the Child Behavior Checklist Youth Self-Report version (31), which has been extensively administered and shown to have good psychometric properties (32), was used to assess symptoms of anxiety and depression at Wave 3.
Statistical Analysis
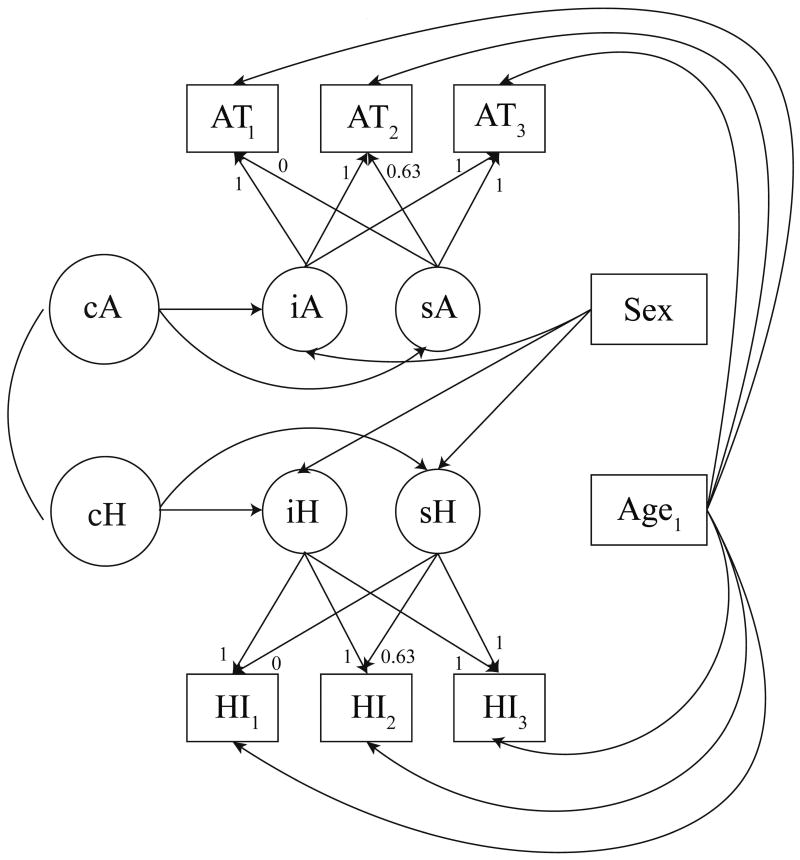
The analyses consisted of 3 steps. In Step 1, we used growth mixture modeling (GMM) to identify distinct groups (“classes”) of individual trajectories for ADHD symptoms across Waves 1–3. In keeping with prior work characterizing ADHD symptom trajectories in TCHAD (33), we fitted a GMM with two classes to the inattention symptoms from Waves 1–3 and a separate GMM with two classes to the hyperactivity/impulsivity symptoms from Waves 1–3. In Step 2, we combined the two inattention trajectory classes with the two hyperactivity/impulsivity trajectory classes to create four combined inattention and hyperactivity/ impulsivity classes. In Step 3, we used linear regression to predict each Wave 3 EDI subscale as a function of the combined trajectory classes and covariates (sex; sex and BMI z-score; or sex and anxiety/depression symptoms) in order to examine whether ADHD symptom trajectories across childhood and adolescence predict disordered eating in late adolescence. To fit the above models (depicted in Figure 1), we used a robust maximum likelihood estimator (which corrects standard errors to account for non-independence due to the twin design), and we handled missing data through Full Information Maximum Likelihood. Appendix A in the online supplemental materials contains additional technical details of the GMM approach.
Figure 1.
Distal Outcome Models
Results
Table 1 provides descriptive summary statistics for the inattention and hyperactivity/impulsivity scores at Waves 1–3 and the EDI subscale scores at Wave 3. On average, inattention and hyperactivity/impulsivity scores decreased from childhood to late adolescence. Inattention scores were (on average) higher for males at all three time points (p < .001 for each wave). Similarly, hyperactivity/impulsivity scores were higher for males at Waves 1 and 2 (p < .01 for Waves 1 and 2), but not at Wave 3 (p < .46). All Wave 3 EDI subscale scores were higher for females.
Table 1.
Summary Statistics for the Classification Model Sample by Sex (total n = 2,315)
| Mean | SD | Range | % Missing | ||
|---|---|---|---|---|---|
| Inattention (Wave 1)a | Males | 0.83 | 1.19 | (0, 6) | 14.60 |
| Females | 0.53 | 0.92 | (0, 6) | 18.10 | |
|
| |||||
| Inattention (Wave 2)a | Males | 0.72 | 1.13 | (0, 6) | 14.16 |
| Females | 0.50 | 0.95 | (0, 6) | 13.83 | |
|
| |||||
| Inattention (Wave 3)a | Males | 0.85 | 1.31 | (0, 6) | 13.02 |
| Females | 0.58 | 1.07 | (0, 6) | 14.09 | |
|
| |||||
| Hyperactivity/Impulsivity (Wave 1)b | Males | 1.13 | 1.67 | (0, 8) | 14.86 |
| Females | 0.92 | 1.46 | (0, 8) | 18.36 | |
|
| |||||
| Hyperactivity/Impulsivity (Wave 2)b | Males | 0.57 | 1.27 | (0, 8) | 14.34 |
| Females | 0.43 | 1.05 | (0, 8) | 13.49 | |
|
| |||||
| Hyperactivity/Impulsivity (Wave 3)b | Males | 0.35 | 0.98 | (0, 8) | 12.76 |
| Females | 0.38 | 0.96 | (0, 8) | 13.83 | |
|
| |||||
| BMI z-score (Wave 3) | Males | −0.14 | 0.98 | (−4.75, 2.86) | 15.03 |
| Females | −0.24 | 0.89 | (−3.68, 2.73) | 11.44 | |
|
| |||||
| EDI Bulimia (Wave 3) | Males | 0.46 | 1.18 | (0, 11) | 12.76 |
| Females | 0.51 | 1.46 | (0, 21) | 9.14 | |
|
| |||||
| EDI Drive for Thinness (Wave 3) | Males | 0.88 | 1.75 | (0, 20) | 16.35 |
| Females | 2.84 | 4.20 | (0, 21) | 13.49 | |
|
| |||||
| EDI Body Dissatisfaction (Wave 3) | Males | 2.24 | 3.66 | (0, 24) | 11.63 |
| Females | 5.66 | 6.21 | (0, 24) | 7.17 | |
|
| |||||
| YSR Anxiety/Depression (Wave 3) | Males | 2.89 | 3.37 | (0, 25) | 11.71 |
| Females | 5.67 | 5.01 | (0, 24) | 6.66 | |
Abbreviations: EDI = Eating Disorder Inventory-2; SD = standard deviation; YSR = Youth Self-Report
Levels of ordinal variable assigned values 0–6 in order to calculate summary statistics.
Levels of ordinal variable assigned values 0–8 in order to calculate summary statistics.
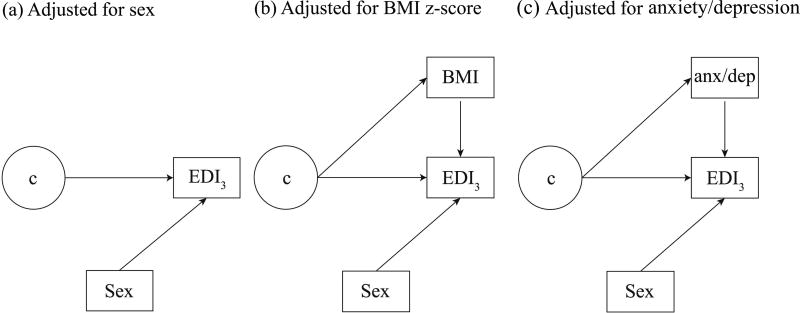
Step 1 of our analyses involved fitting GMMs to identify inattention and hyperactivity/impulsivity trajectory classes respectively; the final model is depicted in Figure 2. In the final model, the two inattention trajectory classes are characterized by different intercepts and slopes, as are the two hyperactivity/impulsivity trajectory classes, and inattention class membership is correlated with hyperactivity/impulsivity class membership. Although sex affected the intercepts for the two inattention classes and the intercepts and slopes for the two hyperactivity/impulsivity classes as described below, it did not affect the slopes for the inattention classes—or class membership—in the final model: these paths were found to be non-significant during model fitting. The entropy value for the final model was 0.8, which is within the acceptable range.
Figure 2.
Step 1 Classification Model (Growth Mixture Model Approach)
Abbreviations: BMI = body mass index z-score; c = latent trajectory classes; EDI3 = Eating Disorder Inventory-2 at Wave 3; anx/dep = Anxiety/Depression
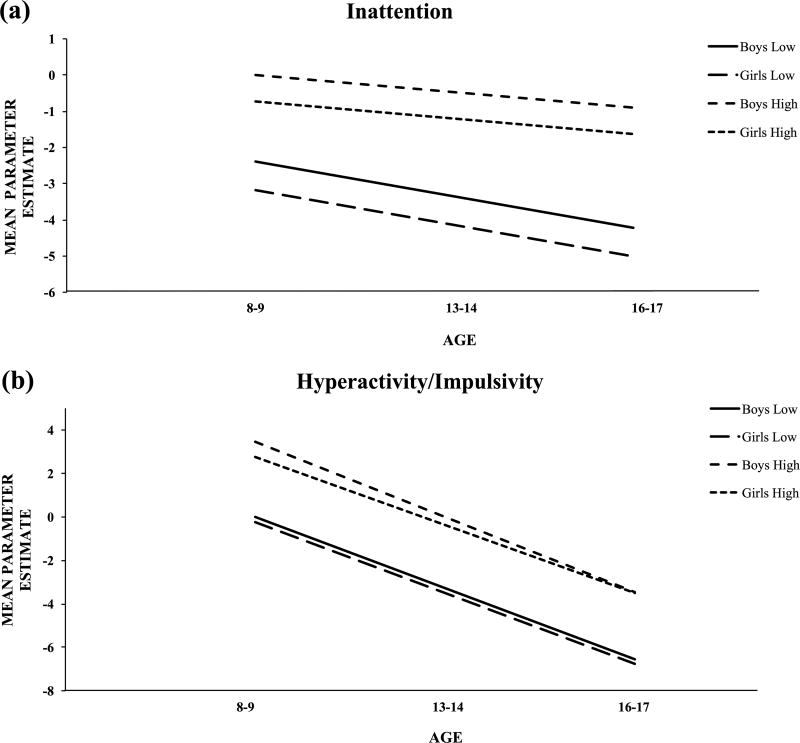
Estimates, standard errors, and p-values for the parameters in the final model are presented in Supplemental Table 1. Figure 3a depicts the symptom trajectories for the inattention classes (which we refer to as the ‘Low Inattention’ class and the ‘High Inattention’ class). As illustrated, both inattention classes had effectively flat trajectories over time, although the trajectory for the ‘Low Inattention’ class started lower at Wave 1. Further, in both inattention classes, the trajectory started significantly lower at Wave 1 for females compared with males. Figure 3b depicts the symptom trajectories for the hyperactivity/impulsivity classes (which we refer to as the ‘Low Hyperactivity/Impulsivity’ class and the ‘High Hyperactivity/Impulsivity’ class). Trajectories for both hyperactivity/impulsivity classes decreased at a similar rate over time, although the trajectory for the ‘Low Hyperactivity/Impulsivity’ class started lower at Wave 1. Further, for females (versus males) in the ‘High Hyperactivity/Impulsivity’ class, the trajectory started significantly lower at Wave 1 and decreased significantly less steeply over time.
Figure 3.
Trajectories of Inattention and Hyperactivity/Impulsivity for Boys and Girls between 8–9 and 16–17 Years of Age
In Step 2, the inattention and hyperactivity/impulsivity classes were combined into four combined trajectory classes for ADHD symptoms: ‘Low Inattention & Low Hyperactivity/Impulsivity’ (referred to as ‘Low Symptom’), which had a class membership probability of 72.5%; ‘High Inattention & Low Hyperactivity/Impulsivity’ (referred to as ‘Predominantly Inattention’), which had a class membership probability of 4.7%; ‘Low Inattention & High Hyperactivity/Impulsivity’ (referred to as ‘Predominantly Hyp/Imp), which had a class membership probability of 1.2%; and ‘High Inattention & High Hyperactivity/Impulsivity’ (referred to as ‘Both Inattention and Hyp/Imp’), which had a class membership probability of 21.6%.
Table 2 summarizes the results from Step 3, which examines the relationship between the four combined trajectory classes and the EDI scores in late adolescence. Notably, scores for the Bulimia, Drive for Thinness, and Body Dissatisfaction subscales were significantly higher in the ‘Both Inattention and Hyp/Imp’ class compared with the referent ‘Low Symptom’ class, even after adjustment for sex and BMI z-score. Likewise, adjusting for anxiety/depression scores did not significantly affect the association, even though anxiety/depression scores were elevated in the ‘Both Inattention and Hyp/Imp’ class relative to the ‘Low Symptom’ class (see Supplemental Table 2).
Table 2.
Coefficienta Estimates, (Standard Errors), and p-Values from Model for Wave 3 EDI-2 Subscales as a Function of Joint Inattention and Hyperactivity/Impulsivity Classb
| Outcomes: Wave 3 EDI-2 Subscales |
|||
|---|---|---|---|
|
| |||
| Bulimia | Drive For Thinness |
Body Dissatisfaction |
|
|
| |||
| Model adjusted for sex | |||
|
| |||
| ‘Low Symptom’ (≈72% of samplec) | 0.34 (0.10) | −1.30 (0.21) | −1.55 (0.35) |
| -- | -- | -- | |
|
| |||
| ‘Predominantly Inattention’ (≈5% of samplec) | 0.21 (0.17) | −1.42 (0.46) | −1.02 (0.78) |
| p < 0.46 | p < 0.79 | p < 0.49 | |
|
| |||
| ‘Predominantly Hyp/Imp’ (≈1% of samplec) | 0.60 (0.48) | −0.64 (1.90) | −2.78 (1.43) |
| p < 0.59 | p < 0.74 | p < 0.39 | |
|
| |||
| ‘Both Inattention and Hyp/Imp’ (≈22% of samplec) | 0.73 (0.12) | −0.14 (0.31) | 0.43 (0.50) |
| p < 0.01 | p < 0.01 | p < 0.01 | |
|
| |||
| Model adjusted for sex and BMI z-score | |||
|
| |||
| ‘Low Symptom’ (≈72% of samplec) | 0.35 (0.10) | −1.24 (0.21) | −1.48 (0.34) |
| -- | -- | -- | |
|
| |||
| ‘Predominantly Inattention’ (≈5% of samplec) | 0.23 (0.18) | −1.26 (0.46) | −0.83 (0.77) |
| p < 0.48 | p < 0.98 | p < 0.38 | |
|
| |||
| ‘Predominantly Hyp/Imp’ (≈1% of samplec) | 0.63 (0.49) | −0.57 (1.88) | −2.71 (1.37) |
| p < 0.56 | p < 0.72 | p < 0.37 | |
|
| |||
| ‘Both Inattention and Hyp/Imp’ (≈22% of samplec) | 0.73 (0.12) | −0.21 (0.30) | 0.19 (0.47) |
| p < 0.01 | p < 0.01 | p < 0.01 | |
|
| |||
| Model adjusted for sex and YSR anxiety/depression | |||
|
| |||
| ‘Low Symptom’ (≈72% of samplec) | 0.36 (0.09) | −1.22 (0.20) | −1.45 (0.34) |
| -- | -- | -- | |
|
| |||
| ‘Predominantly Inattention’ (≈5% of samplec) | 0.09 (0.17) | −1.81 (0.48) | −1.67 (0.81) |
| p < 0.11 | p < 0.21 | p < 0.79 | |
|
| |||
| ‘Predominantly Hyp/Imp’ (≈1% of samplec) | 0.68 (0.44) | −0.39 (1.65) | −2.40 (1.24) |
| p < 0.47 | p < 0.62 | p < 0.44 | |
|
| |||
| ‘Both Inattention and Hyp/Imp’ (≈22% of samplec) | 0.65 (0.12) | −0.39 (0.30) | 0.01 (0.46) |
| p < 0.01 | p < 0.01 | p < 0.001 | |
Abbreviations: BMI = body mass index; EDI = Eating Disorder Inventory-2; Hyp/Imp = Hyperactivity/Impulsivity; YSR = Youth Self-Report
Coefficients represent the means of the EDI subscales for a particular class, after adjustment for covariates. The table also presents the coefficients’ standard errors (in parentheses), and the p-values from a two-sided test of the hypothesis that the difference between the coefficient for the given class and the referent class (‘Low Symptom’) equals 0. The coefficients come from a model for each EDI-2 subscale as function of covariates (sex, or sex and BMI z-score) and the joint inattention - hyperactivity classes (treated as a 4-level categorical variable, with ‘Low Symptom’ as the reference category).
To determine the classes for inattention (and hyperactivity/impulsivity), we fitted a growth mixture model to the inattention (and hyperactivity/impulsivity) symptoms from Waves 1–3. The model empirically determined two classes characterizing the trajectories of the inattention (and hyperactivity/impulsivity) symptoms across the three time points: a declining trajectory with low levels of symptoms at all time points, referred to as the ‘Low’ class, and a declining trajectory with higher levels of symptoms at all time points, referred to as the ‘High’ class. We created the joint inattention & hyperactivity/impulsivity classes by combining the inattention classes with the hyperactivity/impulsivity classes, such that there were four joint classes (‘Low Symptom’; ‘Predominantly Inattention; ‘Predominantly Hyp/Imp’; and ‘Both Inattention and Hyp/Imp’).
Percentage represents the proportion of the sample most likely to be assigned to the relevant class.
Discussion
To our knowledge, this is the first longitudinal, community-based study focusing on the prospective prediction of disordered eating in late adolescence based on ADHD symptom trajectories in childhood and early adolescence. We found that a combination of higher inattention symptoms and higher hyperactivity/impulsivity symptoms throughout childhood and adolescence was associated with increased levels of disordered eating in late adolescence. Notably, this association remained significant after controlling for BMI z-scores or for anxiety and depression symptoms, suggesting that the pathway to disordered eating attitudes and behaviors from ADHD symptoms is not simply attributable to higher BMIs or to elevated anxiety and mood symptoms among those with ADHD symptoms. Our results provide evidence that combined inattention and hyperactivity/impulsivity symptoms in childhood and early adolescence increase susceptibility to disordered eating (as measured by the three EDI subscales) in late adolescence, consistent with our hypothesis and in line with previous findings on children with ADHD diagnoses (2, 3).
Our findings did not suggest that either inattention or hyperactivity/impulsivity on its own is associated with significant elevations in disordered eating in late adolescence. As previously hypothesized, impulsivity may contribute to severity through lack of inhibition, whereas inattention could contribute to disordered eating pathology through a lack of awareness of hunger or the amount of food consumed. Further, both inattention and hyperactivity/impulsivity are associated with poor organizational skills (34) and emotional dysregulation (35), which can contribute to disordered eating (36). Although deficits in either domain alone may not serve as risk factors, their combination appears to be sufficient for increased susceptibility to disordered eating. Another possibility is that although each ADHD subtype contributes to disordered eating through a distinct set of cognitive vulnerabilities, the EDI subscales we studied fail to capture these distinct contributions. Alternatively, it is plausible that the differential effects of inattention and hyperactivity/impulsivity on disordered eating attitudes and behaviors could be present only when the clinical threshold for ADHD or an eating disorder is reached. Finally, it is possible that we did not have sufficient power to examine the individual contributions of inattention and hyperactivity/impulsivity trajectories to disordered eating, as only a small percentage of our participants were in the ‘Predominantly Hyp/Imp’ (1.2%) and the ‘Predominantly Inattention’ (4.7%) trajectory classes.
The present study has notable strengths. Most importantly, the longitudinal design of the ADHD data collection allowed us to make prospective predictions about the emergence of disordered eating in late adolescence from core ADHD symptom developmental trajectories throughout childhood and adolescence. TCHAD also has high response rates for both self- and parent-report measures (23). Having both self- and parent-reports available allowed us to use different informants for the predictor (i.e., ADHD) and the outcomes (i.e., EDI subscale scores), thus reducing bias due to shared method variance. Instead of viewing ADHD as a single construct, we examined inattention and hyperactivity/impulsivity separately in order to carefully assess the individual contribution of each joint trajectory class to disordered eating risk. Also, our large sample included both boys and girls. Unlike clinical studies which often focus on threshold ADHD and/or eating disorders in treatment-seeking individuals with increased disorder severity and chronicity, TCHAD is a community-based cohort that allowed for the examination of the subthreshold ADHD symptom trajectories, dysfunctional eating attitudes, and disordered eating behaviors.
An additional strength of our study is that the potential confounding effects of psychostimulants on eating behavior and body weight are unlikely to affect our findings: during the TCHAD data collection period (i.e., mid- and late-1990s), the rate of psychostimulant prescription for the treatment of ADHD was around 0.08% in Sweden, which was 35 times lower than the rate in the United States for this same period (37). Thus, the percentage of children and adolescents on psychostimulants is likely to be very low in our cohort (although this was not directly assessed).
Despite its strengths, our study also has limitations that merit consideration. We were unable to test for sex differences in the effect of ADHD trajectory class on disordered eating due to a lack of statistical power. Simulations revealed that, even with such a large sample size, we had limited power to detect a sex by trajectory class interaction due to a variety of factors including low class membership for some of the trajectory classes, missing EDI outcomes, and the non-independence of twin data. Because there were no behavioral data on ADHD symptoms, parental report of ADHD symptoms formed the basis of our inattention and hyperactivity/impulsivity trajectories. Also, since inattention is more difficult to observe than hyperactivity/impulsivity, parental report of inattention may not capture the full picture of the twins’ inattention symptoms, thus potentially leading to underreporting (38). In the absence of behavioral data, inclusion of a second measure, such as teacher ratings, could have potentially provided a more complete ADHD assessment (39). We were also unable to distinguish the effects of hyperactivity versus impulsivity on disordered eating. This is a notable limitation in light of a previous report on childhood impulsivity being a better predictor of bulimic symptoms than inattention or hyperactivity in girls with ADHD (3). Also, because the EDI was administered only at Wave 3, we were unable to account for disordered eating in childhood and early adolescence in the model or examine the bidirectional relationship between disordered eating and ADHD symptoms.
In conclusion, higher inattention combined with higher hyperactivity/impulsivity throughout childhood and adolescence was associated with increased disordered eating in late adolescence in a large Swedish population cohort. One important research implication of our results is that ADHD-related constructs should be considered in etiologic models of disordered eating, as ADHD symptoms may be one of many pathways to disordered eating. Our results, coupled with previous reports, may also have implications for prevention, detection, and treatment. In addition, our results argue for increased vigilance by parents, teachers, and health care providers for the emergence of disordered eating attitudes and behaviors among children and adolescents who present with elevated inattention and hyperactivity/impulsivity symptoms. Whereas depression and anxiety have historically been associated with the emergence of disordered eating in youth, ADHD symptoms have received far less attention. Given the high interrelatedness of all psychiatric syndromes on both a genetic and a symptom level (40), it is critical to continue to monitor youth for the emergence of symptoms that fall outside of the narrow profile of their primary diagnosis. Such broad monitoring and rapid response may help halt the progression of emergent symptoms into full-blown disorders.
Supplementary Material
Supplemental Figure 1. Study Design and Assessment Schedule (n = 2,315)
Implications and Contribution.
In this longitudinal, community-based study, a combination of higher inattention and higher hyperactivity/impulsivity symptoms throughout childhood and adolescence was associated with increased disordered eating risk in late adolescence. These findings encourage increased vigilance by parents, teachers, and healthcare providers for the emergence of disordered eating among youth with ADHD symptoms.
Acknowledgments
Drs. Yilmaz and Javaras were supported by the National Institutes of Health (NIH) Grant T32MH076694 (PI: Bulik). Dr. Yilmaz is funded by NIH K01MH109782. Dr. Baker is supported by grant NIH K01MH106675. Dr. Javaras acknowledges financial support from The Phyllis and Jerome Lyle Rappaport Foundation, Nancy Dearman, and the Martini Family Foundation. Dr. Bulik acknowledges financial support from the Swedish Research Council (VR Dnr: 538-2013-8864). Dr. Larsson acknowledges financial support from the Swedish Research Council (2014–3831). Dr. Lichtenstein acknowledges financial support from the Swedish Research Council for Health, Working Life and Welfare (2012-1678) and the Swedish Research Council (2011–2492).
List of Abbreviations
- ADHD
attention deficit/hyperactivity disorder
- BMI
body mass index
- TCHAD
Swedish Twin study of CHild and Adolescent Development
- EDI
Eating Disorder Inventory-2
- SD
standard deviation
- GMM
growth mixture modeling
- Hyp/Imp
hyperactivity/impulsivity
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Findings of this study were presented as a poster at the 2015 annual meeting of the International Conference for Eating Disorders in Boston, MA.
Conflict of Interest: Drs. Bulik and Larsson are grant recipients from Shire. Dr. Larsson has also served as a speaker for Eli Lilly and Shire on topics unrelated to this submission.
References
- 1.Swanson SA, Crow SJ, Le Grange D, et al. Prevalence and correlates of eating disorders in adolescents. Results from the national comorbidity survey replication adolescent supplement. Arch Gen Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mikami AY, Hinshaw SP, Patterson KA, et al. Eating pathology among adolescent girls with attention-deficit/hyperactivity disorder. J Abnorm Psychol. 2008;117:225–235. doi: 10.1037/0021-843X.117.1.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mikami AY, Hinshaw SP, Arnold LE, et al. Bulimia nervosa symptoms in the multimodal treatment study of children with ADHD. Int J Eat Disord. 2010;43:248–259. doi: 10.1002/eat.20692. [DOI] [PubMed] [Google Scholar]
- 4.Yoshimasu K, Barbaresi WJ, Colligan RC, et al. Childhood ADHD is strongly associated with a broad range of psychiatric disorders during adolescence: a population-based birth cohort study. J Child Psychol Psychiatry. 2012;53:1036–1043. doi: 10.1111/j.1469-7610.2012.02567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bleck J, DeBate RD. Exploring the co-morbidity of attention-deficit/hyperactivity disorder with eating disorders and disordered eating behaviors in a nationally representative community-based sample. Eat Behav. 2013;14:390–393. doi: 10.1016/j.eatbeh.2013.05.009. [DOI] [PubMed] [Google Scholar]
- 6.Sonneville KR, Calzo JP, Horton NJ, et al. Childhood hyperactivity/inattention and eating disturbances predict binge eating in adolescence. Psychol Med. 2015:1–10. doi: 10.1017/S0033291715000148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bleck JR, DeBate RD, Olivardia R. The Comorbidity of ADHD and Eating Disorders in a Nationally Representative Sample. J Behav Health Serv Res. 2015;42:437–451. doi: 10.1007/s11414-014-9422-y. [DOI] [PubMed] [Google Scholar]
- 8.Biederman J, Ball SW, Monuteaux MC, et al. Are girls with ADHD at risk for eating disorders? Results from a controlled, five-year prospective study. J Dev Behav Pediatr. 2007;28:302–307. doi: 10.1097/DBP.0b013e3180327917. [DOI] [PubMed] [Google Scholar]
- 9.Yilmaz Z, Kaplan AS, Zai CC, et al. COMT Val158Met variant and functional haplotypes associated with childhood ADHD history in women with bulimia nervosa. Prog Neuropsychopharmacol Biol Psychiatry. 2011;35:948–952. doi: 10.1016/j.pnpbp.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 10.Seitz J, Kahraman-Lanzerath B, Legenbauer T, et al. The role of impulsivity, inattention and comorbid ADHD in patients with bulimia nervosa. PLoS One. 2013;8:e63891. doi: 10.1371/journal.pone.0063891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fernandez-Aranda F, Aguera Z, Castro R, et al. ADHD symptomatology in eating disorders: a secondary psychopathological measure of severity? BMC Psychiatry. 2013;13:166. doi: 10.1186/1471-244X-13-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kaplan AS, Howlett AL, Yilmaz Z, et al. Attention Deficit Hyperactivity Disorder and Binge Eating: Shared Phenomenology, Genetics and Response to Treatment. Int J Child Adolesc Health. 2009;2:165. [Google Scholar]
- 13.Stice E, Davis K, Miller NP, et al. Fasting increases risk for onset of binge eating and bulimic pathology: a 5-year prospective study. J Abnorm Psychol. 2008;117:941–946. doi: 10.1037/a0013644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. fifth edition. Washington DC: Author; 2013. [Google Scholar]
- 15.Reinblatt SP, Mahone EM, Tanofsky-Kraff M, et al. Pediatric loss of control eating syndrome: Association with attention-deficit/hyperactivity disorder and impulsivity. Int J Eat Disord. 2015;48:580–588. doi: 10.1002/eat.22404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boisseau CL, Thompson-Brenner H, Caldwell-Harris C, et al. Behavioral and cognitive impulsivity in obsessive-compulsive disorder and eating disorders. Psychiatry Res. 2012;200:1062–1066. doi: 10.1016/j.psychres.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 17.Fleming J, Levy L. Eating disorders in women with AD/HD. In: Quinn PO, Nadeau KG, editors. Gender issues and AD/HD: research, diagnosis, and treatment. Silver Spring, MD: Advantage Books; 2002. p. 411. [Google Scholar]
- 18.Schwartz BS, Bailey-Davis L, Bandeen-Roche K, et al. Attention deficit disorder, stimulant use, and childhood body mass index trajectory. Pediatrics. 2014;133:668–676. doi: 10.1542/peds.2013-3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Westerberg-Jacobson J, Edlund B, Ghaderi A. Risk and protective factors for disturbed eating: a 7-year longitudinal study of eating attitudes and psychological factors in adolescent girls and their parents. Eat Weight Disord. 2010;15:e208–218. doi: 10.1007/BF03325302. [DOI] [PubMed] [Google Scholar]
- 20.Costello EJ, Mustillo S, Erkanli A, et al. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch Gen Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- 21.Puccio F, Fuller-Tyszkiewicz M, Ong D, et al. A systematic review and meta-analysis on the longitudinal relationship between eating pathology and depression. Int J Eat Disord. 2016;49:439–454. doi: 10.1002/eat.22506. [DOI] [PubMed] [Google Scholar]
- 22.Kaye WH, Bulik CM, Thornton L, et al. Comorbidity of anxiety disorders with anorexia and bulimia nervosa. Am J Psychiatry. 2004;161:2215–2221. doi: 10.1176/appi.ajp.161.12.2215. [DOI] [PubMed] [Google Scholar]
- 23.Lichtenstein P, Tuvblad C, Larsson H, et al. The Swedish Twin study of CHild and Adolescent Development: the TCHAD-study. Twin Res Hum Genet. 2007;10:67–73. doi: 10.1375/twin.10.1.67. [DOI] [PubMed] [Google Scholar]
- 24.Cnattingius S, Ericson A, Gunnarskog J, et al. A quality study of a medical birth registry. Scand J Soc Med. 1990;18:143–148. doi: 10.1177/140349489001800209. [DOI] [PubMed] [Google Scholar]
- 25.Garner D. Eating Disorders Inventory-2: Professional Manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- 26.Nevonen L, Clinton D, Norring C. Validating the EDI-2 in three Swedish female samples: eating disorders patients, psychiatric outpatients and normal controls. Nord J Psychiatry. 2006;60:44–50. doi: 10.1080/08039480500504537. [DOI] [PubMed] [Google Scholar]
- 27.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4h edition, text revision. Washington DC: Author; 2000. [Google Scholar]
- 28.Larsson H, Dilshad R, Lichtenstein P, et al. Developmental trajectories of DSM-IV symptoms of attention-deficit/hyperactivity disorder: genetic effects, family risk and associated psychopathology. J Child Psychol Psychiatry. 2011;52:954–963. doi: 10.1111/j.1469-7610.2011.02379.x. [DOI] [PubMed] [Google Scholar]
- 29.Werner B, Bodin L. Growth from birth to age 19 for children in Sweden born in 1981: descriptive values. Acta Paediatr. 2006;95:600–613. doi: 10.1080/08035250600582822. [DOI] [PubMed] [Google Scholar]
- 30.de Onis M, Onyango AW, Borghi E, et al. Development of a WHO growth reference for school-aged children and adolescents. Bulletin of the World Health Organization. 2007;85:660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Achenbach TM. Manual for Child Behavior Checklist/ 4–18 and 1991 Profile. Burlington, VT: University of Vermont, Dept. of Psychiatry; 1991. [Google Scholar]
- 32.McConaughy SH. Advances in empirically based assessment of children’s behavioral and emotional problems. School Psych Rev. 1993;22:285–307. [Google Scholar]
- 33.Larsson H, Lichtenstein P, Larsson JO. Genetic contributions to the development of ADHD subtypes from childhood to adolescence. J Am Acad Child Adolesc Psychiatry. 2006;45:973–981. doi: 10.1097/01.chi.0000222787.57100.d8. [DOI] [PubMed] [Google Scholar]
- 34.Abikoff H, Nissley-Tsiopinis J, Gallagher R, et al. Effects of MPH-OROS on the organizational, time management, and planning behaviors of children with ADHD. J Am Acad Child Adolesc Psychiatry. 2009;48:166–175. doi: 10.1097/CHI.0b013e3181930626. [DOI] [PubMed] [Google Scholar]
- 35.Martel MM. Research review: a new perspective on attention-deficit/hyperactivity disorder: emotion dysregulation and trait models. J Child Psychol Psychiatry. 2009;50:1042–1051. doi: 10.1111/j.1469-7610.2009.02105.x. [DOI] [PubMed] [Google Scholar]
- 36.Davis C, Levitan RD, Smith M, et al. Associations among overeating, overweight, and attention deficit/hyperactivity disorder: a structural equation modelling approach. Eat Behav. 2006;7:266–274. doi: 10.1016/j.eatbeh.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 37.Ekman JT, Gustafsson PA. Stimulants in AD/HD, a controversial treatment only in Sweden? Eur Child Adolesc Psychiatry. 2000;9:312–313. doi: 10.1007/s007870070036. [DOI] [PubMed] [Google Scholar]
- 38.Rowland AS, Skipper B, Rabiner DL, et al. The shifting subtypes of ADHD: classification depends on how symptom reports are combined. J Abnorm Child Psychol. 2008;36:731–743. doi: 10.1007/s10802-007-9203-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Efstratopoulou M, Simons J, Janssen R. Concordance among physical educators', teachers', and parents' perceptions of attention problems in children. J Atten Disord. 2013;17:437–443. doi: 10.1177/1087054711431698. [DOI] [PubMed] [Google Scholar]
- 40.Anttila V, Bulik-Sullivan B, Finucane HK, et al. Analysis of shared heritability in common disorders of the brain. bioRxiv. 2016 doi: 10.1126/science.aap8757. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Study Design and Assessment Schedule (n = 2,315)