Abstract
IMPORTANCE
Black patients with advanced osteoarthritis (OA) of the knee are significantly less likely than white patients to undergo surgery. No strategies have been proved to improve access to surgery for black patients with end-stage OA of the knee.
OBJECTIVE
To assess whether a decision aid improves access to total knee replacement (TKR) surgery for black patients with OA of the knee.
DESIGN, SETTING, AND PARTICIPANTS
In a randomized clinical trial, 336 eligible participants who self-identified as black and 50 years or older with chronic and frequent knee pain, a Western Ontario McMaster Universities Osteoarthritis Index score of at least 39, and radiographic evidence of OA of the knee were recruited from December 1, 2010, to May 31, 2014, at 3 medical centers. Exclusion criteria were history of major joint replacement, terminal illness, inflammatory arthritis, prosthetic leg, cognitive impairment, lack of a telephone, or contraindications to elective replacement surgery. Data were analyzed on a per-protocol and intention-to-treat (ITT) basis.
EXPOSURE
Access to a decision aid for OA of the knee, a 40-minute video that describes the risks and benefits of TKR surgery.
MAIN OUTCOMES AND MEASURES
Receipt of TKR surgery within 12 months and/or a recommendation for TKR surgery from an orthopedic surgeon within 6 months after the intervention.
RESULTS
Among 336 patients (101 men [30.1%]; 235 women [69.9%]; mean [SD] age, 59.1 [7.2] years) randomized to the intervention or control group, 13 of 168 controls (7.7%) and 25 of 168 intervention patients (14.9%) underwent TKR within 12 months (P = .04). These changes represent a 70% increase in the TKR rate, which increased by 86%(11 of 154 [7.1%] vs 23 of 150 [15.3%]; P = .02) in the per-protocol sample. Twenty-six controls (15.5%) and 34 intervention patients (20.2%) in the ITT analysis received a recommendation for surgery within 6 months (P = .25). The difference in the surgery recommendation rate between the controls (24 of 154 [15.6%]) and the intervention group (31 of 150 [20.7%]) in the per-protocol analysis also was not statistically significant (P = .25). Adjustment for study site yielded similar results: for receipt of TKR at 12 months, adjusted ORs were 2.10 (95%CI, 1.04–4.27) for the ITT analysis and 2.39 (95%CI, 1.12–5.10) for the per-protocol analysis; for recommendation of TKR at 6 months, 1.39 (95%CI, 0.79–2.44) and 1.41 (95%CI, 0.78–2.55).
CONCLUSIONS AND RELEVANCE
A decision aid increased rates of TKR among black patients. However, rates of recommendation for surgery did not differ significantly. A patient-centered counseling and educational intervention may help to address racial variations in the use of TKR for the management of end-stage OA of the knee.
TRIAL REGISTRATION
clinicaltrials.gov Identifer: NCT01851785
Osteoarthritis (OA), which increases in prevalence with aging, is a leading cause of limitations in activity and work in the United States1; these limitations as well as the burden of severe pain disproportionately affect black patients.2 The prevalence of OA among older black individuals is at least as high as that reported for white individuals,3,4 and OA is among the leading causes of disability, particularly for the elderly, in the United States.5–13 Total knee replacement (TKR) is the most effective and cost-effective surgical option for moderate to severe OA of the knee.14 However, a significant racial variation in the use of TKR exists. Black patients are less likely to undergo TKR compared with white patients11,15–17 despite the fact that black patients have similar prevalence or severity of OA of the knee,18,19 report a lower quality of life,20 and have higher odds of disability21 due to OA.
Black candidates for joint replacement differ in their preferences for treatment, which are primarily shaped by differences in understanding of treatment risks and benefits.22Lower patient preference for the treatment reduces patient likelihood of receiving a recommendation for joint replacement from an orthopedic surgeon, even when clinically indicated.23 Furthermore, a patient-centered educational intervention using a decision aid for OA of the knee significantly increases black patients’ knowledge about TKR and consequently improves their willingness to undergo the treatment if clinically indicated and recommended by a physician.24 Whether a decision aid actually improves receipt of joint replacement and/or a recommendation for surgery from an orthopedic surgeon remains unclear. Therefore, in this randomized clinical trial, we tested whether a decision aid for OA of the knee, a source of evidence-based information about the management of knee OA, actually improves access to the surgery for black patients who are referred to orthopedic surgery and are clinically appropriate candidates for TKR.
Methods
Design Overview
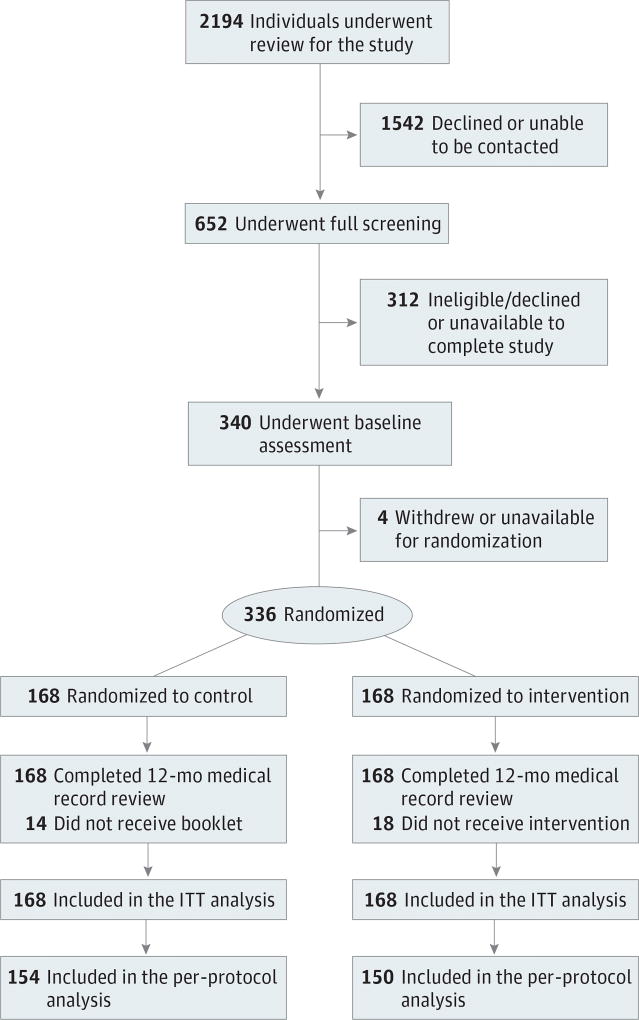
The study methods and recruitment process were described previously.25 In brief, this randomized clinical trial compared the effects of a decision aid for OA of the knee (intervention) with receipt of an OA education booklet (control condition) in persons with moderate-to-severe OA of the knee. Participants were randomized at baseline to the intervention or the control group (Figure 1). The study protocols (available in the Supplement)were approved by the institutional review boards of the University of Pennsylvania, Philadelphia, Temple University Health System, Philadelphia, and the Philadelphia Veterans Affairs Medical Center. All participants provided written informed consent before the study and were compensated for their time and participation.
Figure 1. CONSORT Diagram.
The control condition consisted of a booklet about osteoarthritis (OA) of the knee; the intervention, a video examining all treatment options for OA of the knee. ITT indicates intention to treat.
Setting and Participants
Participants were recruited from December 1, 2010, to May 31, 2014. Potentially eligible participants were identified by screening the electronic medical records of patients referred to the orthopedic surgery clinic at any of the 3 study sites. All identified persons underwent assessment for study eligibility by telephone interview. Eligible participants were those who self-identified as black, were 50 years or older, had chronic and frequent knee pain based on the National Health and Nutrition Examination Survey questionnaire,26 had a Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) score27 of at least 39 (range, 0–100, with higher scores indicating increased pain, stiffness, and functional limitations), and had radiographic evidence of OA of the knee. Exclusion criteria consisted of a history of major joint replacement, diagnosis of a terminal illness (eg, end-stage cancer), physician diagnosis of inflammatory arthritis (ie, rheumatoid arthritis, connective tissue disease, ankylosing spondylitis, or other seronegative spondyloarthropathy), contraindications to replacement surgery (eg, lower extremity paralysis as a result of stroke), having a prosthetic leg, cognitive impairment (eg, dementia), and not having home telephone service.
Randomization and Intervention
Participants were randomized to one of the 2 study arms using a computer-generated assignment. The computer-generated randomization result was sent to the study coordinator via email before the scheduled intervention session. Owing to the nature of the intervention, participants could not have been blinded to the study arm to which they were randomized. The orthopedic surgeons were blinded to patient randomization.
Control Group
Participants randomly assigned to the control group received an educational booklet developed by the National Institute of Arthritis and Musculoskeletal and Skin Diseases28 that summarizes how to live with knee OA but does not mention joint replacement. The purpose of the booklet was to offer patients some benefit in participating in the study.
Intervention Group
This study used the patient decision aid for OA of the knee developed by the Foundation for Informed Medical Decision Making as a vehicle to deliver high-quality, relevant, and timely information on knee OA and joint replacement. The decision aid consists of a 40-minute video that discusses treatment options, including lifestyle changes, medications, injections, complementary therapy, and surgery. The risks, benefits, and known efficacy of each treatment option are outlined. Clinical indications, operative duration, hospital duration, the need for rehabilitative care and physical therapy, recovery time and effort, and cost are also covered. The risks of knee replacement surgery, including death, how long a single prosthesis lasts, and consideration of whether to have both knees replaced at the same time or one at a time are discussed.
Outcome Measures
The clinical outcome of interest was receipt of TKR within 12 months after viewing the video and/or receipt of a recommendation for surgery from an orthopedic surgeon within 6 months of viewing the video. Research staff who were not involved in the intervention and were blinded to the study arm abstracted this information from the medical record.
Covariates
At baseline, participants were asked about their willingness to undergo TKR if recommended by the surgeon. Response options ranged from definitely not willing to definitely willing in a 5-category ordinal response scale. Sociodemographic characteristics, including age, sex, educational attainment, employment status, annual household income, marital status, and living situation, were also assessed at baseline. Severity of knee OA was assessed using the WOMAC index.27 Two subscales of the Arthritis Self-efficacy Scale were also reported.29 The pain subscale measures patients’ confidence that they can manage arthritis-related pain (range, 5–50, with higher scores indicating more confidence), and the function subscale measures patients’ confidence that they can perform specific daily activities (range, 9–90,with higher scores indicating more confidence). Medical comorbidity was assessed using an interviewer-based modification of the Charlson Comorbidity Index (range, 0–17, with higher scores indicating greater comorbidities).30,31 Overall quality of life was assessed using the 12-ItemShort Form Health Survey, version 2, from which the physical and mental component summary scores were calculated (range, 12–61 for the physical and 22–70 for the mental components, with higher scores indicating better physical and mental health).32
Statistical Analysis
Analyses were performed on a per-protocol basis, including patients who actually received the intervention, and an intention to-treat (ITT) basis, in which all randomized participants, whether or not they viewed the decision aid video for knee OA. Demographic and clinical characteristics were compared by intervention vs control groups using 2-tailed t tests for continuous variables and χ2 for categorical variables.
In our primary analysis, the clinical outcome of interest was the recommendation for TKR by an orthopedic surgeon at 6 months after the intervention and/or receipt of TKR surgery at 12 months after the intervention. This information was assessed separately, comparing the intervention and the control arms. Because of our ability to extract data for clinical outcome using the electronic medical record, we had complete data for all study participants regardless of whether they received the intended intervention.
Because the study participants were recruited from 3 different hospital systems in Philadelphia, we used logistic regression analysis to examine the effect of the intervention on a recommendation for TKR within 6months or receipt of TKR within 12 months. We first estimated the unadjusted (crude) odds ratio (OR) for each outcome. We then added into the model the site of care as a covariate. We reported results from both analyses.
Finally, we conducted additional exploratory analyses to assess whether particular subgroups of patients might benefit from the intervention to a greater degree than others. We postulated that patients might derive more or less benefit from the intervention based on sex, age, patient willingness at baseline, and disease-severity level. Accordingly, we used logistic regression models to evaluate the association between each of these patient variables and the 2 study outcomes separately to compare the intervention and control groups with site of care as an additional covariate. We included an interaction term for each variable with the treatment group to test for evidence of effect modification by each of the variables of interest. We report the P value for the interaction term, along with ORs and 95%CIs estimated within levels of each covariate. In formal tests for interaction, continuous variables were used whenever possible. Statistical significance was set with an α level of .05. All analyses were performed using SAS software (version 9.4; SAS Institute Inc).
Results
Participants and Baseline Characteristics
A total of 2194 individuals underwent assessment for the study (Figure 1). Of these, 1542 persons declined or were unable to be contacted for full screening, and 652 underwent full screening for the study. Of these, 312 individuals were ineligible. The remaining 340 participants consented to the study and underwent baseline (prerandomization) assessments of clinical and demographic characteristics as fully eligible. Four participants withdrew from the study after baseline assessments. Of the remaining 336 participants (101 men [30.1%]; 235women [69.9%]; mean [SD] age, 59.1 [7.2] years), 168 were randomized to the intervention (decision aid) arm and 168 to the control arm. Among those randomized to the intervention arm, 150 completed the intervention entirely. The rest did not receive the video intervention. Of those assigned to the control arm, 14 were unavailable for telephone follow-up. However, information on key clinical outcomes for all participants was abstracted from the medical record for full analysis (CONSORT diagram in Figure 1). Baseline participant clinical and demographic characteristics are summarized in the Table. Overall, we found no statistically significant differences in demographic or clinical characteristics between the intervention and control arms.
Table.
Baseline Demographic and Clinical Characteristics of the Study Samplea
| Study | ||||
|---|---|---|---|---|
|
|
||||
| ITT Analysis | Per-Protocol Analysis | |||
|
|
|
|||
| Characteristic | Control (n = 168) |
Intervention (n = 168) |
Control (n = 154) |
Intervention (n = 150) |
| Demographic | ||||
|
| ||||
| Age, mean (SD), y | 59.3 (7.5) | 58.9 (7.0) | 59.4 (7.7) | 58.8 (6.9) |
|
| ||||
| Sex male, No. (%) | 52 (31.0) | 49 (29.2) | 50 (32.5) | 47 (31.3) |
|
| ||||
| Educational attainment less than high school, No. (%) | 39 (23.2) | 48 (28.6) | 35 (22.7) | 41 (27.3) |
|
| ||||
| Currently employed, No. (%) | 43 (25.6) | 41 (24.4) | 40 (26.0) | 34 (22.7) |
|
| ||||
| Currently married, No. (%)b | 38 (22.6) | 41 (25.2) | 34 (22.7) | 36 (24.8) |
|
| ||||
| Living alone, No. (%) | 70 (41.7) | 66 (39.3) | 65 (42.2) | 61 (40.7) |
|
| ||||
| Annual household income <$15 000, No. (%)c | 63 (51.6) | 63 (48.8) | 57 (52.3) | 58 (49.2) |
|
| ||||
| Willing at baseline, No. (%) | 114 (67.9) | 108 (64.2) | 105 (68.2) | 97 (64.7) |
|
| ||||
| Clinical | ||||
|
| ||||
| WOMAC score, mean (SD)d | 62.09 (16.98) | 63.11 (16.26) | 61.66 (16.84) | 63.32 (15.70) |
|
| ||||
| Arthritis Self-efficacy Scale, mean (SD) | ||||
|
| ||||
| Pain subscalee | 24.02 (10.92) | 24.07 (11.15) | 23.88 (10.92) | 24.22 (11.02) |
|
| ||||
| Function subscalef | 52.79 (17.80) | 51.94 (18.19) | 52.04 (17.94) | 52.03 (17.92) |
|
| ||||
| Charlson Comorbidity Scale score, mean (SD)g | 2.98 (2.25) | 2.96 (2.15) | 2.97 (2.21) | 2.90 (2.04) |
|
| ||||
| SF-12 score, mean (SD) | ||||
|
| ||||
| Physical component h | 31.62 (8.78) | 31.24 (9.59) | 31.47 (8.87) | 30.86 (9.02) |
|
| ||||
| Mental component i | 44.74 (8.67) | 45.18 (8.78) | 44.96 (8.52) | 45.07 (8.88) |
Abbreviations: ITT, intention to treat; SF-12, 12-Item Short Form Health Survey; WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index.
We used 2-tailed t tests for continuous variables and χ2 tests for categorical variables. Differences were not statistically significant.
Responses were missing for 10 patients for ITT and 9 for per-protocol analyses.
Responses were missing for 185 patients for ITT and 77 for per-protocol analyses.
Scores range from 0 to 100, with higher scores indicating increased pain, stiffness, and functional limitations.
Scores range from 5 to 50, with higher scores indicating more confidence.
Scores range from 9 to 90, with higher scores indicating more confidence.
Scores range from 0 to 17, with higher scores indicating greater comorbidities.
Scores range from 12 to 61, with higher scores indicating better physical health.
Scores range from 22 to 70, with higher scores indicating better mental health.
Primary Outcomes
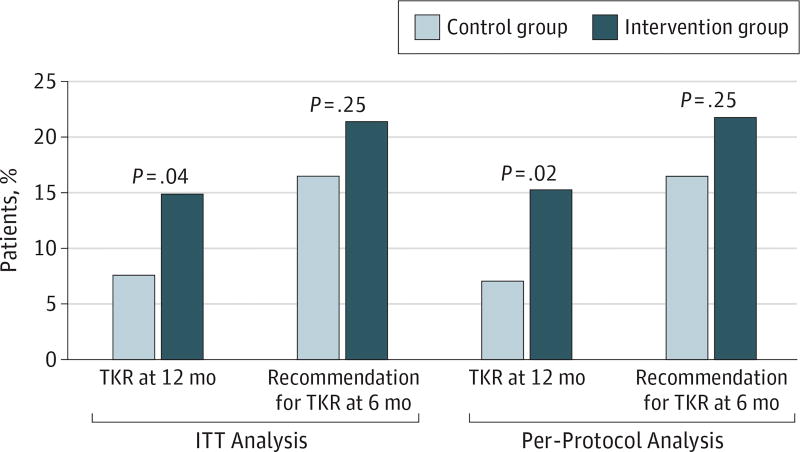
In the ITT analysis, 13 of 168 controls (7.7%) and 25 of 168 intervention patients (14.9%) underwent TKR within 12 months of the intervention (P = .04). This result represents a 70% increase in the receipt of TKR for the intervention group. For the per-protocol sample, receipt of surgery increased by 86% (11 of 154 [7.1%] vs 23 of 150 [15.3%]; P = .02). Twenty-six of the controls (15.5%) and 34 of the intervention patients (20.2%) in the ITT analysis received a recommendation for surgery within 6 months of intervention. However, this difference (30%) did not achieve statistical significance (P = .25). The numbers were very similar when we confined the analysis to the per-protocol sample (24 of 154 controls [15.6%] and 31 of 150 intervention patients [20.7%]; P = .25) (Figure 2). Although we did not assess the recommendation for surgery at 12 months, typically patients do not undergo surgery without first receiving a recommendation for surgery from an orthopedic surgeon.
Figure 2. Observed Proportions for Study Outcomes.
Data depict the patients in each study arm who received total knee replacement (TKR) surgery within 12 months or a recommendation for TKR surgery within 6 months. The control condition consisted of a booklet about osteoarthritis (OA) of the knee; the intervention, a video examining all treatment options for OA of the knee. ITT indicates intention to treat.
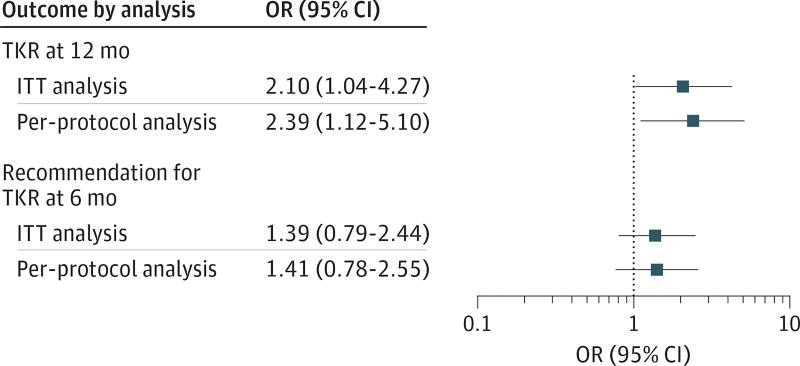
Effects of Study Site
Because the study participants were recruited from 3 different hospital systems in Philadelphia, we examined whether the site of care was related to the effect of the intervention on the recommendation for TKR within 6 months or receipt of TKR within 12 months. We calculated the site-adjusted ORs comparing study arms for the ITT and per-protocol analyses. After adjustment for study site, study findings were essentially identical and we report only results of the site-adjusted analyses. For receipt of TKR at 12 months, the adjusted ORs were 2.10 (95%CI, 1.04–4.27) for the ITT analysis and 2.39 (95%CI, 1.12–5.10) for the per-protocol analysis. For recommendation of TKR at 6months, the adjusted ORs were 1.39 (95%CI, 0.79–2.44) and 1.41 (95% CI, 0.78–2.55) (Figure 3).
Figure 3. Study Outcomes.
Site-adjusted odds ratios (ORs) compare the intervention and control arms for study outcomes.The control condition consisted of a booklet about osteoarthritis (OA) of the knee; the intervention, a video examining all treatment options for OA of the knee. TKR indicates total knee replacement.
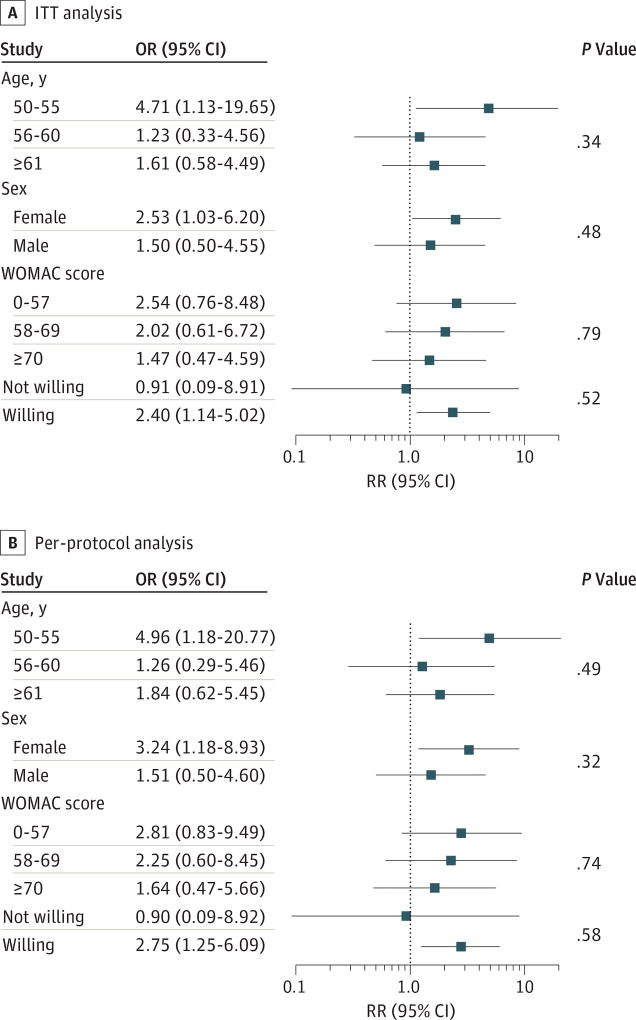
Subgroup Analysis
For patients who showed a statistically significant increase in the receipt of TKR, we conducted additional exploratory analyses to assess whether particular subgroups of patients might benefit from the intervention to a greater degree than others. The effect of the decision aid intervention on TKR at 12 months was similar among the subgroups(Figure 4).However, the intervention tended to be more effective than the control treatment for patients aged 50 to 55 years (OR,4.17;95%CI,1.13–19.65), patients who were willing to undergo surgery at baseline (OR, 2.40; 95% CI, 1.14–5.02), and women (OR, 2.54; 95%CI, 1.03–6.20).
Figure 4. Subgroup Analysis of Total Knee Replacement at 12 Months.
Odds ratios (ORs) are shown for the intervention vs control groups at each level of age, sex, Western Ontario McMaster Universities Osteoarthritis Index (WOMAC) score (range, 0–100, with higher scores indicating increased pain, stiffness, and functional limitations), and baseline willingness, adjusted for site. P values for interaction were calculated from logistic regression models including the study group, the covariates and their interaction, and site. Age and WOMAC score were continuous, and baseline willingness was ordinal. The control condition consisted of a booklet about osteoarthritis (OA) of the knee; the intervention, a video examining all treatment options for OA of the knee. ITT indicates intention to treat.
Discussion
In this sample of black patients who were referred to an orthopedic clinic for knee OA, our randomized clinical trial tested the effectiveness of a decision aid for OA of the knee on patients’ likelihood of undergoing TKR and/or receiving a recommendation for surgery from an orthopedic surgeon. We found that the decision aid resulted in an 85% increase in the receipt of TKR within 12 months among those who received the intervention compared with controls. The decision aid also increased by about 30% the receipt of a recommendation from an orthopedic surgeon within 6 months of the intervention. However, this association did not achieve statistical significance (P = .25). Finally, we found that the intervention was more likely to lead to surgery among those who at baseline were willing compared with those who were unwilling, for women compared with men, and for patients aged 50 to 55 years compared with older patients.
Disparities in TKR represent one of many types of racial and ethnic disparities that exist across various health care conditions and settings.33–40 The reasons for these disparities are complex and involve patient-level, physician-level, and system-level factors. One potential etiologic mechanism for disparities in elective treatment such as TKR is patient preference, an attitudinal disposition that is amenable to educational intervention.41 Patient preference has been reported to vary by race and ethnicity and to influence use of medical care.42–44 Black patients are less willing to consider joint replacement in general.45–47 In a study that examined willingness to pay for TKR among a sample of patients, black and white participants differed significantly in their willingness to pay for TKR, even after adjusting for age, income, educational level, and other factors.48
Although decision aids are used in clinical decision making and are increasingly available for patients’ education, their use to reshape patient preference and to empower patients, particularly minority patients in their pursuit of clinical care, is novel and innovative. Decision aids are conceptually framed by decision theories and cognitive behavioral theories49 and are designed as counseling tools, particularly for preference-sensitive medical conditions or treatments such as TKR. Decision aids provide high-quality information on treatment options while also clarifying the outcomes of treatment choice. In this way, they empower patients and facilitate communication and decision making. Decision aids are associated with increased patient knowledge, more realistic patient perceptions about the disease or treatment, less decisional conflict, fewer patients who are passive decision makers, fewer patients who remain indecisive after counseling, and improved concordance between patient values and treatment choices.50 The National Quality Forum cited shared decision making, which decision aids promote, as one of the 6 health care reforms with the greatest potential to reduce disparities.51 We used the decision aid in this study as a means to deliver high-quality, relevant, and timely information on OA of the knee and TKR.
In contrast to our findings, other studies have examined the use of decision aids as decision tools and found them to be associated with less use of elective invasive surgery such as joint replacement. For example, Arterburn et al52 published the findings of an observational study that showed decision aids to be associated with reduced use of joint replacement. Similarly, in a Cochrane review, Stacey et al53 reviewed studies involving the use of decision aids. They found decision aids to be associated with key patient outcomes, such as patient satisfaction with the treatment decision and reduced decisional conflict. In approximately a dozen of those studies, patients were also found to favor conservative treatment compared with major invasive surgery.53Our study differs from those studies in that we focused on black patients, who are traditionally skeptical about the use of joint replacement in the management of advanced OA of the knee and hip. The effect of the decision aid on patient access to elective surgery may vary according to where patients are along the treatment preference continuum. The review by Stacey et al53 indicated that patients with high preference for surgery at baseline might be nudged by the decision aid toward a lower preference for invasive surgery. However, patients who at baseline hold low preference for surgery may be more likely to be moved by the decision aid toward a higher level of preference and possibly higher rates of surgery.
One question that our study did not address directly is the mechanism by which the decision aid intervention leads to a higher rate of TKR. However, black patients who are candidates for TKR differ in their preferences for joint replacement, which are primarily shaped by differences in knowledge and understanding about the risks and benefits of the treatment.22,46 Furthermore, physician-patient communication for preference-sensitive treatments such as joint replacement is bidirectional, and the content of the communication and decisions are influenced by the patient’s baseline knowledge and ability to engage in the discussion. Evidence suggests that baseline differences in preference, knowledge, or expectations regarding joint replacement affect the quality of communication between black patients and orthopedic surgeons and consequently reduce black patients’ likelihood of receiving a recommendation for joint replacement.54,55
Limitations
Several limitations should be considered in interpreting our results. First, we did not evaluate the nonsurgical treatments our study participants may have received. Various nonsurgical treatment options exist for patients with OA of the knee, including viscosupplementation, intra-articular corticosteroid injections, and medication therapy with various analgesics.56 Proportions of patients using these OA treatments might have differed by study group at baseline and at any time before the 1-year follow-up, potentially confounding the effects of the intervention on patient treatment preferences. Second, we followed up patients for only 12 months. Given the long-term trajectory of OA of the knee, a longer follow-up may have resulted in a higher rate of surgery among those who received the intervention. Finally, our intervention was brief and occurred only once. A more frequent intervention and better access to a decision aid for patients would result in an even greater likelihood of receiving TKR among those for whom the treatment is clinically appropriate.
Conclusions
In this randomized clinical study of black patients who were referred to orthopedic surgery for OA of the knee, we found that a knee decision aid significantly increased the receipt of TKR within 12 months by 85% compared with those who received the educational pamphlet. The decision aid also increased the likelihood of receiving a recommendation for TKR from an orthopedic surgeon within 6 months of the intervention by 30%. However, this association did not achieve statistical significance. Although the interactions between the study group and the subgroups were not statistically significant, the findings for younger patients, women, and those willing at baseline to benefit more from the decision aid intervention are potentially interesting areas for future investigation. Finally, future research may be needed to also explain the mechanism by which the decision aid actually leads to greater uptake of surgery among black patients and whether this method could be used to address other treatment disparities.
Supplementary Material
Key Points.
Question
Does patient education with a decision aid improve access to total knee replacement surgery for black patients with end-stage osteoarthritis of the knee?
Findings
In this randomized clinical trial of 336 individuals, a patient-centered educational intervention using validated decision aid significantly increased receipt of total knee replacement surgery for black patients with end-stage osteoarthritis of the knee.
Meaning
Patient-centered educational tools such as decision aids might help reduce racial disparities in access to preference-sensitive surgical treatments such as total knee replacement.
Acknowledgments
Funding/Support: This study was supported by grant 1R01AR059615-0 from the National Institute of Arthritis and Musculoskeletal Skin Diseases, National Institutes of Health. Dr Ibrahim reports receiving Mid-Career Development Award K24AR055259 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases.
Role of the Funder/Sponsor: The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Ibrahim had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Ibrahim, Blum, Lee, Mooar.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Ibrahim, Collier.
Critical revision of the manuscript for important intellectual content: Ibrahim, Blum, Lee, Mooar, Medvedeva, Richardson.
Statistical analysis: Ibrahim, Medvedeva, Richardson.
Obtained funding: Ibrahim, Mooar.
Administrative, technical, or material support: Ibrahim, Blum, Lee, Mooar, Collier.
Study supervision: Ibrahim, Blum, Lee.
Conflict of Interest Disclosures: None reported.
References
- 1.Stoddard SJL, Ripple JM, Krause L. Chartbook on Work and Disability in the United States. Washington, DC: US National Institute on Disability and Rehabilitation; 1998. [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) Racial/ethnic differences in the prevalence and impact of doctor-diagnosed arthritis: United States,2002. MMWR Morb Mortal Wkly Rep. 2005;54(5):119–123. [PubMed] [Google Scholar]
- 3.Lawrence RC, Helmick CG, Arnett FC, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41(5):778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 4.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis Care Res. 1995;8(4):242–250. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 5.Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275(11):858–865. [PubMed] [Google Scholar]
- 6.Yelin E, Lubeck D, Holman H, Epstein W. The impact of rheumatoid arthritis and osteoarthritis: the activities of patients with rheumatoid arthritis and osteoarthritis compared to controls. J Rheumatol. 1987;14(4):710–717. [PubMed] [Google Scholar]
- 7.Rothfuss J, Mau W, Zeidler H, Brenner MH. Socioeconomic evaluation of rheumatoid arthritis and osteoarthritis: a literature review. Semin Arthritis Rheum. 1997;26(5):771–779. doi: 10.1016/s0049-0172(97)80044-3. [DOI] [PubMed] [Google Scholar]
- 8.Hochberg MC, Perlmutter DL, Hudson JI, Altman RD. Preferences in the management of osteoarthritis of the hip and knee: results of a survey of community-based rheumatologists in the United States. Arthritis Care Res. 1996;9(3):170–176. doi: 10.1002/1529-0131(199606)9:3<170::aid-anr1790090304>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 9.NIH Consensus Development Panel on Total Hip Replacement. NIH consensus conference: total hip replacement. JAMA. 1995;273(24):1950–1956. [PubMed] [Google Scholar]
- 10.Sharkness CM, Hamburger S, Moore RM, Jr, Kaczmarek RG. Prevalence of artificial hip implants and use of health services by recipients. Public Health Rep. 1993;108(1):70–75. [PMC free article] [PubMed] [Google Scholar]
- 11.Wilson MG, May DS, Kelly JJ. Racial differences in the use of total knee arthroplasty for osteoarthritis among older Americans. Ethn Dis. 1994;4(1):57–67. [PubMed] [Google Scholar]
- 12.Hoaglund FT, Oishi CS, Gialamas GG. Extreme variations in racial rates of total hip arthroplasty for primary coxarthrosis: a population-based study in San Francisco. Ann Rheum Dis. 1995;54(2):107–110. doi: 10.1136/ard.54.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dunlop DD, Manheim LM, Song J, Chang RW. Arthritis prevalence and activity limitations in older adults. Arthritis Rheum. 2001;44(1):212–221. doi: 10.1002/1529-0131(200101)44:1<212::AID-ANR28>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 14.Zhang W, Moskowitz RW, Nuki G, et al. OARSI recommendations for the management of hip and knee osteoarthritis, part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis Cartilage. 2008;16(2):137–162. doi: 10.1016/j.joca.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 15.Skinner J, Weinstein JN, Sporer SM, Wennberg JE. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349(14):1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 16.Katz BP, Freund DA, Heck DA, et al. Demographic variation in the rate of knee replacement: a multi-year analysis. Health Serv Res. 1996;31(2):125–140. [PMC free article] [PubMed] [Google Scholar]
- 17.Cisternas MG, Murphy L, Croft JB, Helmick CG, Centers for Disease Control and Prevention (CDC) Racial disparities in total knee replacement among Medicare enrollees: United States, 2000–2013;2006. MMWR Morb Mortal Wkly Rep. 2009;58(6):133–138. [PubMed] [Google Scholar]
- 18.Felson DT, Naimark A, Anderson J, Kazis L, Castelli W, Meenan RF. The prevalence of knee osteoarthritis in the elderly: the Framingham Osteoarthritis Study. Arthritis Rheum. 1987;30(8):914–918. doi: 10.1002/art.1780300811. [DOI] [PubMed] [Google Scholar]
- 19.Anderson JJ, Felson DT. Factors associated with osteoarthritis of the knee in the first National Health and Nutrition Examination Survey (HANES I): evidence for an association with overweight, race, and physical demands of work. Am J Epidemiol. 1988;128(1):179–189. doi: 10.1093/oxfordjournals.aje.a114939. [DOI] [PubMed] [Google Scholar]
- 20.Ibrahim SA, Burant CJ, Siminoff LA, Stoller EP, Kwoh CK. Self-assessed global quality of life: a comparison between African-American and white older patients with arthritis. J Clin Epidemiol. 2002;55(5):512–517. doi: 10.1016/s0895-4356(01)00501-7. [DOI] [PubMed] [Google Scholar]
- 21.Verbrugge LM, Gates DM, Ike RW. Risk factors for disability among US adults with arthritis. J Clin Epidemiol. 1991;44(2):167–182. doi: 10.1016/0895-4356(91)90264-a. [DOI] [PubMed] [Google Scholar]
- 22.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Differences in expectations of outcome mediate African American/white patient differences in "willingness" to consider joint replacement. Arthritis Rheum. 2002;46(9):2429–2435. doi: 10.1002/art.10494. [DOI] [PubMed] [Google Scholar]
- 23.Hausmann LRM, Mor M, Hanusa BH, et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010;25(9):982–988. doi: 10.1007/s11606-010-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ibrahim SA, Hanusa BH, Hannon MJ, Kresevic D, Long J, Kent Kwoh C. Willingness and access to joint replacement among African American patients with knee osteoarthritis: a randomized, controlled intervention. Arthritis Rheum. 2013;65(5):1253–1261. doi: 10.1002/art.37899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vina ER, Richardson D, Medvedeva E, Kent Kwoh C, Collier A, Ibrahim SA. Does a patient-centered educational intervention affect African-American access to knee replacement? a randomized trial. Clin Orthop Relat Res. 2016;474(8):1755–1764. doi: 10.1007/s11999-016-4834-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tepper S, Hochberg MC. Factors associated with hip osteoarthritis: data from the first National Health and Nutrition Examination Survey (NHANES-I) Am J Epidemiol. 1993;137(10):1081–1088. doi: 10.1093/oxfordjournals.aje.a116611. [DOI] [PubMed] [Google Scholar]
- 27.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–1840. [PubMed] [Google Scholar]
- 28.National Institute of Arthritis and Musculoskeletal and Skin Disorders. Handout on Health: Osteoarthritis. [Accessed September 26, 2016]; http://www.niams.nih.gov/Health_Info/Osteoarthritis/default.asp.
- 29.Lorig K, Chastain RL, Ung E, Shoor S, Holman HR. Development and evaluation of a scale to measure perceived self-efficacy in people with arthritis. Arthritis Rheum. 1989;32(1):37–44. doi: 10.1002/anr.1780320107. [DOI] [PubMed] [Google Scholar]
- 30.Chaudhry S, Jin L, Meltzer D. Use of a self-report-generated Charlson Comorbidity Index for predicting mortality. Med Care. 2005;43(6):607–615. doi: 10.1097/01.mlr.0000163658.65008.ec. [DOI] [PubMed] [Google Scholar]
- 31.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Med Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Ware JE, Jr, Kosinski M, Bjorner JB, Turner-Bowker DM, Gandek B, Maruish ME. User’s Manual for the SF-36 version 2 TM Health Survey. 2. Lincoln, RI: Quality Metric Inc; 2007. [Google Scholar]
- 33.Whittle J, Conigliaro J, Good CB, Lofgren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. 1993;329(9):621–627. doi: 10.1056/NEJM199308263290907. [DOI] [PubMed] [Google Scholar]
- 34.Peterson ED, Wright SM, Daley J, Thibault GE. Racial variation in cardiac procedure use and survival following acute myocardial infarction in the Department of Veterans Affairs. JAMA. 1994;271(15):1175–1180. [PubMed] [Google Scholar]
- 35.Goldberg KC, Hartz AJ, Jacobsen SJ, Krakauer H, Rimm AA. Racial and community factors influencing coronary artery bypass graft surgery rates for all 1986 Medicare patients. JAMA. 1992;267(11):1473–1477. [PubMed] [Google Scholar]
- 36.Blendon RJ, Aiken LH, Freeman HE, Corey CR. Access to medical care for black and white Americans: a matter of continuing concern. JAMA. 1989;261(2):278–281. [PubMed] [Google Scholar]
- 37.Ayanian JZ, Udvarhelyi IS, Gatsonis CA, Pashos CL, Epstein AM. Racial differences in the use of revascularization procedures after coronary angiography. JAMA. 1993;269(20):2642–2646. [PubMed] [Google Scholar]
- 38.Hannan EL, Kilburn H, Jr, O’Donnell JF, Lukacik G, Shields EP. Interracial access to selected cardiac procedures for patients hospitalized with coronary artery disease in New York State. Med Care. 1991;29(5):430–441. doi: 10.1097/00005650-199105000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Peterson ED, Shaw LK, DeLong ER, Pryor DB, Califf RM, Mark DB. Racial variation in the use of coronary-revascularization procedures: are the differences real? do they matter? N Engl J Med. 1997;336(7):480–486. doi: 10.1056/NEJM199702133360706. [DOI] [PubMed] [Google Scholar]
- 40.Conigliaro J, Whittle J, Good CB, et al. Understanding racial variation in the use of coronary revascularization procedures: the role of clinical factors. Arch Intern Med. 2000;160(9):1329–1335. doi: 10.1001/archinte.160.9.1329. [DOI] [PubMed] [Google Scholar]
- 41.Ashton CM, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services: bias, preferences, or poor communication? J Gen Intern Med. 2003;18(2):146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ayanian JZ, Cleary PD, Weissman JS, Epstein AM. The effect of patients’ preferences on racial differences in access to renal transplantation. N Engl J Med. 1999;341(22):1661–1669. doi: 10.1056/NEJM199911253412206. [DOI] [PubMed] [Google Scholar]
- 43.Hannan EL, van Ryn M, Burke J, et al. Access to coronary artery bypass surgery by race/ethnicity and gender among patients who are appropriate for surgery. Med Care. 1999;37(1):68–77. doi: 10.1097/00005650-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 44.Gardon HS, Paterniti DA, Wray NP. Impact of patient refusal on racial/ethnic variation in the use of invasive cardiac procedures. J Gen Intern Med. 2002;17(suppl 1):159. doi: 10.1111/j.1525-1497.2004.30131.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Variation in perceptions of treatment and self-care practices in elderly with osteoarthritis: a comparison between African American and white patients. Arthritis Rheum. 2001;45(4):340–345. doi: 10.1002/1529-0131(200108)45:4<340::AID-ART346>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 46.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Understanding ethnic differences in the utilization of joint replacement for osteoarthritis: the role of patient-level factors. Med Care. 2002;40((1)(suppl)):I44–I51. doi: 10.1097/00005650-200201001-00006. [DOI] [PubMed] [Google Scholar]
- 47.Figaro MK, Russo PW, Allegrante JP. Preferences for arthritis care among urban African Americans: "I don’t want to be cut". Health Psychol. 2004;23(3):324–329. doi: 10.1037/0278-6133.23.3.324. [DOI] [PubMed] [Google Scholar]
- 48.Byrne MM, O’Malley KJ, Suarez-Almazor ME. Ethnic differences in health preferences: analysis using willingness-to-pay. J Rheumatol. 2004;31(9):1811–1818. [PubMed] [Google Scholar]
- 49.O’Connor AM, Llewellyn-Thomas HA, Flood AB. Modifying unwarranted variations in health care: shared decision making using patient decision aids. Health Aff (Millwood) 2004;(suppl web exclusives):VAR63–VAR72. doi: 10.1377/hlthaff.var.63. [DOI] [PubMed] [Google Scholar]
- 50.O’Connor A, Stacey D, Entwistle V, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2003;(2):CD001431. doi: 10.1002/14651858.CD001431. [DOI] [PubMed] [Google Scholar]
- 51.Frosch DL, Singer KJ, Timmermans S. Conducting implementation research in community-based primary care: a qualitative study on integrating patient decision support interventions for cancer screening into routine practice. Health Expect. 2011;14(suppl 1):73–84. doi: 10.1111/j.1369-7625.2009.00579.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Arterburn D, Wellman R, Westbrook E, et al. Introducing decision aids at Group Health was linked to sharply lower hip and knee surgery rates and costs. Health Aff (Millwood) 2012;31(9):2094–2104. doi: 10.1377/hlthaff.2011.0686. [DOI] [PubMed] [Google Scholar]
- 53.Stacey D, Légaré F, Col NF, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev. 2014;(1):CD001431. doi: 10.1002/14651858.CD001431.pub4. [DOI] [PubMed] [Google Scholar]
- 54.Hausmann LR, Kresevic D, Cohen PZ, et al. Patient race and doctor-patient communication in the orthopedic setting. Paper presented at: Society of General Internal Medicine Annual Meeting; April 9, 2008; Pittsburgh, PA. [Google Scholar]
- 55.Hausmann LRM, Mor M, Hanusa BH, et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010;25(9):982–988. doi: 10.1007/s11606-010-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hochberg MC, Altman RD, April KT, et al. American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken) 2012;64(4):465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.