Abstract
Objective
The purpose of this study was to examine the co-occurrence of posttraumatic stress disorder (PTSD) and dissociation in a clinical sample of trauma-exposed adolescents, first evaluating evidence for the depersonalization/derealization dissociative subtype of PTSD as defined by the DSM-5, and then examining a broader set of dissociation symptoms.
Method
A sample of treatment-seeking, trauma-exposed adolescents ages 12 to 16 (N=3,081) from the National Child Traumatic Stress Network Core Data Set was used to meet the study objectives. Two models of PTSD/dissociation co-occurrence were estimated using latent class analysis, one with two dissociation symptoms and the other with ten dissociation symptoms. After model selection, groups within each model were compared on demographics, trauma characteristics, and psychopathology.
Results
Model A, the depersonalization/derealization model, had five classes: (1) dissociative subtype/high PTSD; (2) high PTSD; (3) anxious arousal; (4) dysphoric arousal; and (5) a low symptom/reference class. Model B, the expanded dissociation model, identified an additional class characterized by dissociative amnesia and detached arousal.
Conclusion
These two models provide new information about the specific ways PTSD and dissociation co-occur and illuminate some differences between adult and adolescent trauma symptom expression. A dissociative subtype of PTSD can be distinguished from PTSD alone among adolescents, but assessing a wider range of dissociative symptoms is needed in order to fully characterize adolescent traumatic stress responses.
Keywords: PTSD, dissociation, adolescent, maltreatment
INTRODUCTION
Trauma exposures during early childhood can impair child development, disrupt attachment security and self-regulatory processes, and lead to poor physical and mental health outcomes in childhood and across the lifespan.1 During or after traumatic experiences, children may display posttraumatic stress responses including dissociation that require clinical intervention to mitigate risk for these long-term adverse outcomes.2, 3 Understanding the relationship between trauma, posttraumatic stress, and dissociation is particularly important for children, for whom trauma exposures and responses can impair healthy development. Dissociation is a “disruption of and/or discontinuity in the normal, subjective integration of one or more aspects of psychological functioning, including—but not limited to—memory, identity, consciousness, perception, and motor control.”4(p826) It is a psychobiological process that develops in response to traumatic or other overwhelming experiences as a coping mechanism to attenuate distress.5 By automating and compartmentalizing certain psychobiological functions, trauma-related threats and distress can be separated from conscious awareness and produce alterations in consciousness that promote coping and survival in the face of overwhelming traumatic stressors.2, 5
Maltreatment and complex trauma exposures involving direct harm, such as sexual or physical abuse, as well as less overt types of maltreatment such as emotional abuse, neglect, and frightening or unpredictable parenting, can all lead to the development of long-term dissociative coping in children.6 Dissociation may also be more acute in what is known as peritraumatic dissociation, which occurs during or immediately after a traumatic event in the form of altered perceptions, memory, and awareness related to the trauma experience.7 Peritraumatic dissociation suggests that the trauma is being experienced as severe and overwhelming, and it is a strong risk factor for the development of posttraumatic stress disorder (PTSD).7 Although dissociation can be protective and even adaptive for attenuating distress during a traumatic experience in childhood when there are no other options for escape, it can interfere with child learning and development and becomes maladaptive when it persists into adulthood and is deployed in the face of ordinary, everyday stressors that do not pose a significant threat.8–10 Trauma-related dissociation can disrupt the development of self-regulatory processes in stress response systems, interpersonal relationships, affect and impulses, and self-perception and lead to the development of chronic self-dysregulation.11 Adults with maladaptive dissociative tendencies may not be able to distinguish situations that are genuinely threatening or dangerous and often have trouble tolerating and self-regulating intense emotions, particularly those that accompany trauma-related flashbacks, intrusion, and arousal.8–11
Although the evidence base for complex trauma sequelae, including dissociation, has grown, a specific complex PTSD was not included as a formal diagnosis in the DSM-5.12 However, a dissociative subtype of PTSD was established, defined by symptoms of depersonalization and derealization in addition to symptoms of PTSD.13 The subtype was noted to possibly capture the subset of individuals with more severe trauma histories, complex posttraumatic stress sequelae, and unique treatment needs.13 Although controversy in the field remains about whether or not complex PTSD should be a formal diagnosis, this change in the DSM-5 reflects the growing evidence base demonstrating that trauma, dissociation, and posttraumatic stress frequently co-occur in survivors of maltreatment.
There have been several adult studies of the dissociative subtype of PTSD that provide evidence for the subtype and characterize the ways trauma, PTSD, and dissociation are expressed in trauma survivors. Depersonalization and derealization emerged in these studies as the two dissociation symptoms that characterized a unique, high-severity subset of PTSD cases, and individuals with the dissociative subtype more frequently endorsed childhood trauma and adult sexual trauma.14, 15 Additionally, women in the dissociative subtype group had higher levels of avoidant and borderline personality disorder behaviors.14, 15 Prevalence estimates of the dissociative subtype range from 12% to 50% of PTSD cases.16–18
As evidence for the relationships between complex trauma exposure, dissociation, and PTSD has accumulated among veteran and adult populations, a gap in the literature remains for how these phenomena affect children and adolescents, as well as how patterns of co-occurring PTSD and dissociation change during development and across the lifespan. Although there is a need to study these phenomena across childhood, adolescence is a particularly important developmental epoch to capture because it will help bridge what is known about adults to children and clarify the life course of traumatic stress symptomatology. Adolescent PTSD tends to look similar to adult PTSD, but adolescents are more likely to display aggression, poor impulse control, and traumatic reenactment.19 There are some differences in the expression of dissociative symptomatology when comparing adolescents and adults as well. Dissociative symptoms in adolescents are often subtler and may be mistaken for inattentiveness, as adolescents tend to display less dramatic changes in voice, mood, and mannerisms, and briefer trance states.20, 21 Adolescents also often lack insight that dissociated parts or voices the adolescent is experiencing are not normal.19 These differences from adults are consistent with the normal developmental tasks and transitions associated with adolescence.22 Studies of the new PTSD criteria with samples of adolescents have provided evidence of complex posttraumatic stress sequelae in response to severe trauma, but the dissociative subtype has received little attention as it relates to child development.23, 25 In a recent study of trauma-exposed adolescents involved in juvenile justice, an 83% prevalence rate for PTSD dissociative subtype (PTSD-D) was found as well as evidence for a three-factor dimension of posttraumatic dissociation including depersonalization/derealization, amnesia, and loss of conscious control.25 However, additional study of this topic is needed in light of the known differences in the effects of and responses to childhood trauma exposure versus other trauma exposure, as well as the potential life course changes in expression of dissociation over time. The purpose of this study was to examine the co-occurrence of PTSD and dissociation for a clinical sample of trauma-exposed adolescents, first evaluating evidence for the depersonalization/derealization dissociative subtype of PTSD as defined by the DSM-5, and then examining a broader set of dissociation symptoms. This study replicates the approach and methodology of an adult study of the dissociative subtype of PTSD with a sample of veterans that used latent class modeling to explore evidence for the dissociative subtype of PTSD.15 The adult study found evidence for a subgroup of individuals affected by PTSD with more severe PTSD symptomatology and co-occurring depersonalization/derealization.15 The current study used a similar methodological approach with a trauma-exposed, treatment-seeking sample of adolescents to evaluate developmental differences in the dissociative subtype of PTSD.
METHOD
Design and Sample
A secondary analysis of the National Child Traumatic Stress Network (NCTSN) Core Data Set (CDS) was used to answer the research questions for this study.26, 27 This dataset contains clinical data from over 14,000 trauma-exposed children ages 0 to 21 from 57 NCTSN sites in the US, collected from 2010 to 2014. Children in the CDS sample were seeking assessment and treatment services secondary to trauma exposure. Data for this study were collected at intake (prior to the initiation of treatment). Data were collected by clinicians at NCTSN sites from the child and his or her caregiver. Additional information about the CDS is reported elsewhere.28, 29 A subset of the full CDS was selected for this study. Individuals in the CDS were included in the subset if they were adolescents ages 12 to 16, had baseline data available, experienced at least one type of trauma exposure, and were not missing assessments of PTSD and dissociation. The age range was chosen to capture the specific developmental epoch of adolescence to facilitate some comparisons to adults. The final sample used in the analysis included 3,081 adolescents. The University of Michigan Institutional Review Board reviewed and approved this study.
Measures
Demographics
Demographic data available in the CDS were age in years, gender, race/ethnicity (White, Black, Hispanic, Other), residence (with parents, with other relatives, foster care, residential treatment, other), and insurance status (private, public, both, neither). In prior studies with the CDS, insurance status has been used as a proxy variable for socioeconomic risk.28, 30
Trauma
The CDS General Trauma Information Form was used to assess 20 different types of trauma exposures and the age(s) when the trauma occurred. Trauma variables used for this analysis were a total trauma exposure count, a maltreatment trauma count, individual variables for each of four maltreatment types (physical abuse, sexual abuse, emotional abuse, neglect), and whether the trauma occurred before or after age 6. Six years was chosen as a cutoff age to denote early childhood maltreatment, which can lead to more complex posttraumatic stress.2, 3
PTSD
The University of California Los Angeles PTSD Reaction Index for DSM-IV (UCLA PTSD-RI) is a 48-item pediatric measure of trauma exposure and PTSD, administered in an interview or in self-report form.31–34 The 20 PTSD symptom items and 2 associated features of PTSD items (trauma-related guilt, fear of trauma recurrence) were used for this study (Table 1). This measure contains additional items for some symptoms (C6, emotional numbing; C7, foreshortened future; D2, anger/irritability), two questions for criterion A, and items assessing the presence of two PTSD associated features, trauma-related guilt and fear of trauma recurrence.34 The UCLA PTSD-RI was used to determine PTSD diagnosis, the number of PTSD symptoms using scores of 2 or greater as a positive endorsement, and the DSM-IV to make a PTSD diagnosis (at least one B cluster item, at least three C cluster items, and at least two D cluster items; this diagnosis did not consider level of functional impairment).31 The internal consistency reliability for the current sample on the UCLA PTSD-RI was 0.93.
Table 1.
Posttraumatic Stress Disorder Symptoms by Cluster
| Re-experiencing |
|---|
| B1: Intrusive recollections of trauma |
| B2: Distressing dreams about trauma |
| B3: Feeling of trauma recurrence |
| B4: Psychological distress when reminders of trauma occur |
| B5: Physiologic reactivity when reminders of trauma occur |
| Avoidance |
| C1: Avoiding talking, thinking, or having feelings about trauma |
| C2: Avoiding people, places, or things that are reminders of trauma |
| C3: Trouble remembering important parts of trauma |
| C4: Diminished interest in important activities or friendships |
| C5: Feelings of detachment or distance from others |
| C6a: Restricted positive affect |
| C6b: Restricted negative affect |
| C7a: Sense of foreshortened future |
| C7b: Feeling pessimistic or negative about the future |
| Arousal |
| D1: Trouble falling or staying asleep |
| D2a: Irritability or anger |
| D2b: Arguments or physical fights |
| D3: Trouble concentrating or attention difficulties |
| D4: Hypervigilance |
| D5: Heightened startle response |
| Associated features |
| AFa: Trauma-related guilt |
| AFb: Fear of trauma recurrence |
Dissociation
The Trauma Symptom Checklist for Children-Alternate Version (TSCC-A) is a 44-item measure of traumatic stress symptoms designed for children ages 8 to 16 years.35 The TSCC-A was another measure included in the CDS assessment protocol. The present study only used items from the dissociation subscale of the TSCC-A used. The dissociation scale has ten items and two subscales, overt dissociation and fantasy. Dissociation was defined according to the DSM-5 PTSD dissociative subtype symptoms, depersonalization and derealization, and thus we used two items from the TSCC-A specifically assessing these symptoms.12 Studies of the dimensionality of dissociation with trauma-exposed youth have found a depersonalization/ derealization construct that effectively distinguishes youth with and without PTSD and youth with and without the dissociative subtype of PTSD.25 These two dissociation symptoms were considered present for scores of 2 or higher on a 0 (never) to 3 (almost all of the time) scale. The internal consistency reliability for only these two items was 0.69. The overall internal consistency reliability for the TSCC-A was 0.97.
Behavioral Symptoms
The Child Behavior Checklist for Ages 6 to 18 (CBCL) internalizing and externalizing behavior broadband scales were used to measure emotional and behavioral problems.36–37 The CBCL broadband scales were included in the analysis as indicators of level of dysfunction. The behavioral items are rated on 3-point Likert scales (0/not true, 2/very true or often true) by caregivers, and for this analysis, and raw scores for internalizing and externalizing behavior problems were used. These scores are the sum of the numbered responses for each item in the scale.37 The internalizing behavior subscale internal consistency reliability was 0.90. The externalizing behavior subscale internal consistency reliability was 0.92.
Analysis
All analyses were conducted using Mplus and R, version 3.2.3, and p-values were set at .05. Data were missing in low proportions (<10% per variable) with no distinguishable patterns of missingness. Because this analysis used a clinical dataset, missing trauma history and symptom data were coded as “no” responses, consistent with the medical-legal presumption that clinicians must note such information relevant to making treatment decisions in clinical records.38 Individuals who were missing all data on PTSD and dissociation were not eligible for inclusion in the study sample, as described previously. Frequencies and descriptive statistics were examined for all variables used in the analysis. Latent class analysis (LCA) was used to examine the dissociative subtype of PTSD in two separate models distinguished by the way dissociation was operationalized. Latent class analysis is a statistical technique used to identify unobserved (latent) heterogeneity in a population from categorical data.39 This technique was selected to replicate an adult study of the dissociative subtype of PTSD that used latent profile analysis (LPA) to look for evidence of an unobserved dissociative subtype of PTSD.15 These two approaches to latent variable identification are identical except that they use different types of data to derive the latent grouping variable. Latent class analysis uses categorical data to derive a categorical latent variable, while in latent profile analysis, continuous data are used to derive a continuous latent variable.39 This study used latent class analysis with variables indicating the presence or absence of symptoms based on a predetermined cutoff because the study was focused on diagnosis rather than intensity of PTSD and dissociation.
In the first model (Model A), 22 PTSD items from the UCLA PTSD-RI representing the B, C, and D symptom clusters plus 2 PTSD associated features (trauma-related guilt, fear of trauma recurrence; the associated features are now part of Criterion D in the DSM-5) and 2 dissociative subtype items (depersonalization and derealization) from the TSCC-A were used to derive latent classes (24 items total).12, 35 In the second model (Model B), the dissociation component was expanded. The same 24 PTSD and PTSD-associated feature items and 10 dissociation items (depersonalization and derealization plus all other items from the dissociation scale of the TSCC-A) were used to derive latent classes (32 items total) in the second model. For each model, first, a 2-class model was estimated. Then, the number of latent classes was incrementally increased, comparing the fit of each new model to the previous model. Several statistical fit indices were used to compare models and select the most parsimonious model that fit the data best, including Bayesian Information Criterion (BIC), sample size-adjusted Bayesian Information Criterion (SSABIC), Akaike Information Criterion (AIC), and the Vuong-Lo-Mendel-Rubin (VLMR) likelihood ratio test.40 Lower BIC or AIC values indicate that the model fit is improved by adding a class. The VLMR likelihood ratio test compares a model with k classes to a model with k + 1 classes. It generates a test statistic and p-value, and if the p-value is less than .05, the model fit is improved by adding a class. To determine the distinctness of the latent classes, entropy values and substantively meaningful characteristics of the classes were assessed by the investigators. Entropy values range from 0 to 1, and values closer to 1 indicate better differentiation and separation between classes.40 After selecting the best-fit latent class model and assigning cases in the sample to their most likely latent classes, two multinomial logistic regression models, one for Model A and one for Model B, were estimated with latent class as the outcome variable and demographic and trauma history characteristics as the predictor variables. Analysis of variance tests with pairwise follow-up tests were used to examine differences between latent classes for each of the two models on level of dysfunction, as indicated by the CBCL internalizing and externalizing broadband scales, and overall trauma count, number of PTSD symptoms, and number of dissociation symptoms. For these five analyses, the p-value was set at .01 to adjust for multiple comparisons.
Finally, after deriving the two sets of latent classes, the sample was divided into four groups according to their trauma-related symptomology to assess agreement between DSM-5 diagnosis of the dissociative subtype and latent classes: (1) PTSD only, (2) dissociation only, (3) both PTSD and dissociation, which represents the dissociative subtype of PTSD (PTSD-D), and (4) neither. A 3-step approach of modal maximum likelihood was used to examine agreement between this DSM-5 grouping variable and the latent classes.41 This approach adjusts for misclassification bias in assigning latent class membership fitting a multinomial logistic regression model with the maximum likelihood function adjusted for the uncertainly of class membership probabilities.
RESULTS
Sample
The mean age of the sample was 14.5 years (SD = 1.45). The sample was 60.5% girls and 39.5% boys. The racial proportions of the sample were 32.4% White or Caucasian, 22.9% Black or African American, 36.9% Hispanic, and 6.0% other. Public insurance status was considered a proxy variable for socioeconomic risk, and 61.2% of the sample had public insurance. A majority of the sample (62.5%) resided with their parents, while 11.8% were living with other relatives, 8.9% were in foster care, 7.1% were in residential treatment, and 4.0% had another living situation. The sample had a mean of 3.9 overall trauma exposures (SD = 2.42, minimum = 1, maximum = 14) and a mean of 1.1 maltreatment trauma exposures (SD = 1.28, minimum = 0, maximum = 4).
Model Selection
Model A: DSM-5 Dissociation Model
After evaluating several fit indices and model quality both statistically and substantively, a 5-class model was selected as the best fit for the data (Table 2). This model was favored by the VLMR likelihood ratio test. The information criterion values favored 6 or 7 class models. However, ultimately, the 5-class model was selected because it was both statistically supported and substantively interpretable; the 5-class model reflects the 5-factor structure of PTSD found previously with the NCTSN sample.32
Table 2.
Statistical Fit Indices for Model A
| Model A | ||||||
|---|---|---|---|---|---|---|
| Classes | BIC | SSA BIC | AIC | VLMR LRT | AdLMR LRT | Entropy |
| 2 Class | 80543.4 | 80387.7 | 80247.7 | −46870.3** | 13523.5** | 0.90 |
| 3 Class | 78264.9 | 78029.7 | 77818.4 | −40074.9** | 2467.0** | 0.85 |
| 4 Class | 77886.9 | 77575.4 | 77289.7 | −38835.2** | 575.9** | 0.80 |
| 5 Class | 77613.9 | 77219.9 | 76865.8 | −38545.8** | 471.5** | 0.77 |
| 6 Class | 77543.5 | 77543.5 | 76644.6 | −38308.9 | 269.9 | 0.75 |
| 7 Class | 77595.6 | 77042.7 | 76545.8 | −38173.3 | 148.0 | 0.74 |
| Model B | ||||||
| Classes | BIC | SSA BIC | AIC | VLMR LRT | AdLMR LRT | Entropy |
| 2 Class | 103576.2 | 103369.7 | 103184.1 | −59809.5** | 16502.7** | 0.92 |
| 3 Class | 100746.4 | 100435.0 | 100155.2 | −51527.0** | 3083.3** | 0.87 |
| 4 Class | 100040.1 | 99623.9 | 99249.8 | −49979.6** | 967.7** | 0.83 |
| 5 Class | 99463.4 | 98942.3 | 98474.0 | −49493.9** | 838.6** | 0.82 |
| 6 Class | 99281.1 | 98655.2 | 98092.6 | −49073.0** | 445.7** | 0.79 |
| 7 Class | 99249.0 | 98518.2 | 97861.4 | −48849.3 | 296.1 | 0.78 |
Note: AdLMR LRT = Adjusted Lo-Mendel-Rubin Likelihood Ratio Test; AIC = Akaike Information Criterion; BIC = Bayesian Information Criterion; SSA = sample size-adjusted; VLMR LRT = Vuong-Lo-Mendel-Rubin Likelihood Ratio Test.
Value is significant at the .05 level
Value is significant at the .01 level
Model B: Expanded Dissociation Model
A 5-class model was selected for Model B to make comparisons with the Model A (Table 2). Although statistical fit indices would have favored a 6 or 7 class model, substantive comparison and interpretation of the 5-class model versus the 6- and 7-class models indicated that the 5-class model represented the data well, allowed for comparisons with Model A, and had theoretical validity, agreeing with previous studies with this sample.32 The 6-class model presented a complex mixture of arousal and dissociation symptom profiles that lacked clear interpretability. Additionally, the decreases in BIC between the 5-, 6-, and 7-class models were not as dramatic, implying that the BIC was leveling off. In light of the purpose of the study, we prioritized substantive evaluation of the models over the statistical indicators.
Model A: DSM-5 Dissociation Model
Description of Latent Classes
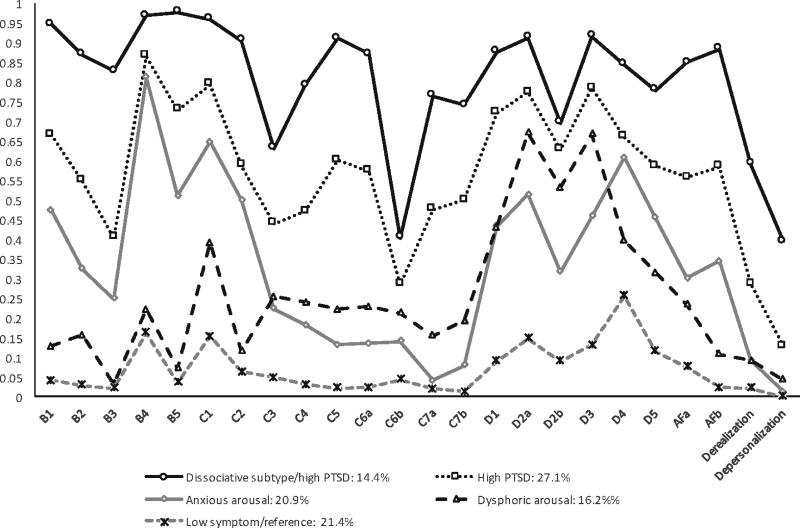
This model classified 14.4% of the sample in a dissociative subtype/high PTSD class (mean class membership probability = 0.90) characterized by higher probability of PTSD symptoms in all clusters and the highest probability of depersonalization (0.40) and derealization (0.59) symptoms of all the groups. The next class, high PTSD, contained 27.1% of the sample (mean class membership probability = 0.85) and was similar to the dissociative subtype/high PTSD class, but with an overall lower probability of each PTSD and dissociation symptom. The third class, anxious arousal, contained 20.9% of the sample (mean class membership probability = 0.81) and had a symptom profile that reflected the anxious arousal symptom cluster (high relative probability of D4 and D5; 0.61 and 0.40, respectively) of PTSD consistent with previous findings with this sample.30 A dysphoric arousal class (16.2% of the sample; mean class membership probability = 0.80) reflected the dysphoric arousal factor (high relative probability of D1, D2, and D3; 0.43, 0.67, 0.53, respectively).30 The remainder of the sample (21.4%) fell into a low symptom/reference class (mean class membership probability = 0.90), having relatively low probabilities of all symptoms. Figure 1 shows the probability profiles for each class in Model A.
Figure 1.
Latent class probability profiles for model A. Note: This figure shows the probability of each posttraumatic stress disorder (PTSD) and dissociation symptom in model A by latent class. See Table 1 for symptom descriptions.
Comparison of Latent Classes
The differences in overall number of trauma exposures (difference = 0.37, p = .06) and number of maltreatment trauma exposures (difference = 0.07, p = .89) were not significant between the dissociative subtype/high PTSD class and the high PTSD class. In the logistic regression model, neglect decreased odds of membership in the dissociative subtype/high PTSD class and high PTSD class (OR= 0.46; OR= 0.50, respectively). Girls had higher odds of membership in these two groups (OR = 3.89; OR = 2.32, respectively) compared to boys, and adolescents living in a residential treatment center (OR = 2.16; OR = 1.92, respectively) had higher odds of membership in the same two classes compared to living with parents. Adolescents in the dissociative subtype/high PTSD class had the highest mean number of PTSD symptoms (mean = 16.9) of all the groups, followed by the high PTSD class (mean of 12.2) (difference = 4.7; p < .001). There were no significant group differences on externalizing behavior.
Model B: Expanded Dissociation Model
Description of Latent Classes
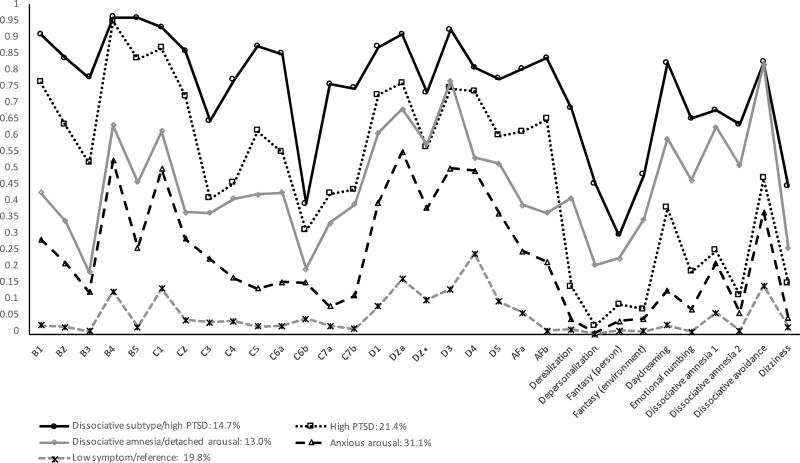
The dissociative subtype/high PTSD class (14.7% of the sample; mean class membership probability = 0.92) had the highest probabilities of all PTSD and all dissociation symptoms of the 5 groups, as well as characteristics of dysphoric arousal. This group was distinct from other classes in that it had the highest probability of derealization (0.68), depersonalization (0.46), and daydreaming (0.82). The second class, a high PTSD class (21.4%; mean class membership probability = 0.86) had an elevated profile of probabilities of PTSD symptoms, but with a markedly lower dissociation probability profile compared with the dissociative subtype/high PTSD class. The dissociative subtype/high PTSD class differed from the high PTSD class in that it had higher probability of B5 (0.96 v. 0.83), a higher avoidance symptom probability profile, and displayed anxious (items D4 and D5) rather than dysphoric arousal (items D1, D2a/b, D3). The third class, dissociative amnesia/detached arousal (13.0%; mean class membership probability = 0.84), was lower than either of the previous classes in terms of its PTSD profile, but had a much higher probability of dissociation items than the high PTSD class. This class had a high probability of dissociative amnesia (0.63) and dissociative avoidance (0.82) relative to other within-group dissociation symptoms. It also had dysphoric arousal characteristics and a low probability of flashbacks (B1; 0.43), nightmares (B2; 0.34), PTSD avoidance symptoms (C cluster; range of 0.20 to 0.42), trauma-related guilt (AFa; 0.39), and fear or trauma recurrence (AFb; 0.37). The fourth class, anxious arousal, (31.1%; mean class membership probability = 0.88) had a low avoidance symptom profile, anxious arousal, a low dissociation symptom profile, and minimal emotional numbing/dysphoria symptoms. As was the case with the previous model, a low symptom/reference class (19.8%; mean class membership probability = 0.91) had the lowest symptom profile of any group. Figure 2 shows the probability profiles for each class in Model B.
Figure 2.
Latent class probability profiles for model B. Note: This figure shows the probability of each posttraumatic stress disorder (PTSD) and dissociation symptom in model B by latent class. See Table 1 for symptom descriptions.
Comparison of Latent Classes
The dissociative subtype/high PTSD class was slightly older than the others (mean age = 14.74, SD = 1.38), though not significantly. Girls had increased odds of membership in the dissociative subtype/high PTSD class (OR = 3.70) and high PTSD class (OR = 3.06). Race and insurance status were not significant predictors of group membership. Adolescents living in residential treatment centers had higher odds of membership in the dissociative subtype/high PTSD class (OR = 2.18), and those living in foster care had decreased odds of membership in the dissociative amnesia/detached arousal class (OR = 0.52) (see Table 3).
Table 3.
Multinomial Logistic Regression Model for Model B Classes
| Outcome (reference= Low symptom/reference) |
Dissociative Subtype/High PTSD |
High PTSD | Dissociative Amnesia/ Detached Arousal |
Anxious Arousal | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Trauma exposures | ||||||||
| Number | 1.31* | 1.22, 1.41 | 1.24* | 1.16, 1.33 | 1.20* | 1.11, 1.30 | 1.14* | 1.07, 1.22 |
| Age of trauma (reference= After 6 yo) | ||||||||
| Before 6 years | 0.85 | 0.60, 1.19 | 0.76 | 0.56, 1.03 | 0.96 | 0.68, 1.37 | 0.81 | 0.61, 1.08 |
| Maltreatment exposures | ||||||||
| Sexual abuse | 1.23 | 0.89, 1.71 | 1.80* | 1.34, 2.41 | 1.25 | 0.89, 1.76 | 1.18 | 0.89, 1.56 |
| Physical abuse | 1.36 | 0.97, 1.88 | 1.31 | 0.97, 1.77 | 1.12 | 0.79, 1.59 | 1.16 | 0.88, 1.53 |
| Emotional abuse | 1.19 | 0.87, 1.64 | 1.37* | 1.03, 1.84 | 1.21 | 0.87, 1.68 | 1.14 | 0.88, 1.48 |
| Neglect | 0.45* | 0.31, 0.64 | 0.57* | 0.41, 0.79 | 0.71 | 0.49, 1.04 | 0.79 | 0.59, 1.05 |
| Gender (reference= Boys) | ||||||||
| Girls | 3.70* | 2.79, 4.91 | 3.06* | 2.39, 3.92 | 2.02* | 1.53, 2.67 | 1.54* | 1.25, 1.91 |
| Age | ||||||||
| Number | 1.09* | 1.00, 1.20 | 1.06 | 0.98, 1.15 | 1.05 | 0.96, 1.15 | 1.06 | 0.98, 1.13 |
| Race (reference= White) | ||||||||
| Black | 1.04 | 0.73, 1.50 | 0.98 | 0.71, 1.32 | 1.08 | 0.75, 1.55 | 1.11 | 0.83, 1.47 |
| Hispanic | 0.99 | 0.72, 1.36 | 0.88 | 0.66, 1.18 | 0.84 | 0.60, 1.17 | 1.02 | 0.78, 1.32 |
| Other | 1.21 | 0.73, 2.01 | 0.97 | 0.60, 1.56 | 1.18 | 0.70, 1.98 | 1.15 | 0.75, 1.76 |
| Insurance (reference= None) | ||||||||
| Private | 1.43 | 0.91, 2.28 | 1.07 | 0.70, 1.63 | 1.46 | 0.91, 2.35 | 1.24 | 0.84, 1.82 |
| Public | 0.88 | 0.65, 1.20 | 0.78 | 0.59, 1.03 | 1.00 | 0.73, 1.37 | 1.05 | 0.82, 1.34 |
| Both | 0.63 | 0.19, 2.18 | 0.55 | 0.18, 1.67 | 1.14 | 0.37, 3.50 | 0.64 | 0.23, 1.78 |
| Residence (reference= Parents) | ||||||||
| Relatives | 0.87 | 0.56, 1.33 | 0.94 | 0.65, 1.38 | 0.82 | 0.53, 1.27 | 0.97 | 0.69, 1.35 |
| Foster care | 0.92 | 0.57, 1.50 | 0.83 | 0.53, 1.22 | 0.52* | 0.30, 0.90 | 0.72 | 0.48, 1.07 |
| Residential treatment | 2.18* | 1.23, 3.89 | 1.72 | 0.99, 2.99 | 0.79 | 0.39, 1.61 | 1.45 | 0.85, 2.48 |
| Other | 0.67 | 0.43, 1.05 | 0.46* | 0.30, 0.70 | 0.79 | 0.51, 1.22 | 0.80 | 0.56, 1.12 |
Note: PTSD = posttraumatic stress disorder
Value is significant at 0.05 level.
The dissociative subtype/high PTSD class had the highest number of total trauma exposures (mean= 4.3, SD= 3.0), but it did not differ significantly from the high PTSD class (mean= 4.1, SD= 3.0) on this variable. Looking at the count of maltreatment only, the high PTSD class had the highest mean number of maltreatment exposures (mean= 1.44, SD= 1.37), but this number was not significantly different than the dissociative subtype/high PTSD class average (mean= 1.31, SD= 1.32). Experiencing maltreatment trauma before age six was not significantly associated with membership in any particular class. Sexual abuse and emotional abuse increased odds of membership in the high PTSD class (OR= 1.80; OR= 1.37, respectively), while neglect decreased odds of membership in the dissociative subtype/high PTSD class and high PTSD class (OR= 0.45; OR= 0.57, respectively).
The dissociative subtype/high PTSD class had the highest mean number of PTSD symptoms (mean= 16.3, SD= 2.0), followed by the other four classes in order (see Table 4). The differences between all class pairings were all statistically significant. The same pattern held true for dissociation symptoms. Each class differed significantly on dissociation symptoms from each other class, except for the comparison of the high PTSD class with the dissociative amnesia/detached arousal class, which had a mean of 2.7 more dissociation symptoms (p= <.001). Comparing level of dysfunction as measured by behavioral symptoms, the dissociative subtype/high PTSD class had more internalizing behavior symptoms (mean= 20.95, SD= 11.92) than the high PTSD class (mean = 17.15; SD= 10.28; difference= 3.8; p≤.001). The same pattern held true for externalizing behaviors; the dissociative subtype/high PTSD class had a mean of 21.39 symptoms (SD=12.96), and the high PTSD class had a mean of 18.16 (SD=12.11) symptoms (difference= 3.2, p= .003).
Table 4.
Latent Class Group Comparisons for Model B
| N(%) | Overall 3081 (100.0) |
Dissociative subtype/high PTSD 453 (14.7) |
High PTSD 658 (21.4) |
Dissociative amnesia/detached arousal 401 (13.0) |
Anxious arousal 958 (31.1) |
Low symptom/ reference 611 (19.8) |
F |
|---|---|---|---|---|---|---|---|
| Trauma count, M(SD) | 3.85 (2.4) | 4.25 (3.0) | 4.12 (3.0) | 3.63 (3.0) | 3.47 (3.0) | 2.78 (1.5) | 37.80*** |
| PTSD symptom count, M(SD) | 8.41 (5.4) | 16.34 (2.0) | 12.7 (2.3) | 9.19 (2.4) | 6.04 (2.1) | 1.42 (1.2) | 4379.00*** |
| Dissociation count, M(SD) | 2.28 (2.4) | 6.05 (1.9) | 1.91 (1.2) | 4.66 (1.6) | 1.05 (1.0) | 0.32 (0.6) | 1871.00*** |
| Externalizing behavior, M(SD) | 18.52 (12.34) | 21.39 (12.96) | 18.16 (12.11) | 19.5 (12.97) | 19.05 (12.25) | 15.22 (11.13) | 12.19*** |
| Internalizing behavior, M(SD) | 15.77 (10.28) | 20.95 (11.92) | 17.15 (10.28) | 16.8 (10.26) | 14.37 (9.06) | 11.94 (9.24) | 42.88*** |
Note: PTSD = posttraumatic stress disorder.
p < .001
Model A and Model B Comparison
Both models demonstrated relatively low probabilities of PTSD symptoms B3, C3, and C6b, as well as depersonalization, for all classes (see Table 1 for symptom descriptions). For the additional items on the UCLA PTSD-RI, scores did not seem to differ within each pair of C and D symptoms in either model, with the exception of item C6a, which better differentiated the high-severity classes in both models than C6b. There was a consistent high probability of PTSD symptoms B4, C1, and D2a across all classes in both models. In Model B when additional dissociation symptoms were accounted for, the anxious and dysphoric arousal groups were not clearly differentiated as in Model A. However, the two high dissociation groups (dissociative subtype/high PTSD and dissociative amnesia/detached arousal) reflected dysphoric arousal symptoms, while the two low dissociation groups (high PTSD and anxious arousal) demonstrated more anxious arousal symptoms. Model A classified 83.4% of PTSD-D cases in the dissociative subtype/high PTSD class, but classified both PTSD-only (62.9%) and dissociation-only (61.1%) cases into the same class (high PTSD). These groups were better differentiated in Model B. The dissociative subtype/high PTSD class contained 89.2% of PTSD-D cases, the high PTSD class contained 74.0% of PTSD-only cases, and the dissociative amnesia/detached arousal class contained 66.9% of dissociation-only cases.
DISCUSSION
This study evaluated two latent class models of co-occurring PTSD and dissociation symptoms, one with the two DSM-5 PTSD dissociative subtype items of depersonalization and derealization, and one with an expanded set of ten dissociation symptoms.12 These two models provide new information about the specific ways PTSD and dissociation co-occur and illuminate differences between adult and adolescent trauma symptom expression. Latent class models identified distinct subgroups in a national sample of adolescents seeking trauma treatment services based on profiles of PTSD and dissociative symptoms. When only the dissociative symptoms in the dissociative subtype of PTSD (depersonalization and derealization) were considered, a dissociative PTSD class and a PTSD without dissociative features class were identified, as well as two additional classes characterized by subsets of PTSD symptoms (anxious arousal, dysphoric arousal), and a relatively low symptom class. When additional dissociative symptoms were included, similar subgroups were identified, but the dysphoric arousal class also was characterized by dissociative amnesia and detached arousal. These findings support the extension of the primarily adult-based PTSD-dissociative subtype to traumatized adolescents, while also suggesting that a wider range of dissociative symptoms than the PTSD-D depersonalization and derealization symptoms should be considered when assessing and treating traumatized adolescents who are dysphoric but do not report PTSD flashbacks, nightmares, avoidance, guilt, or fear symptoms.
Model A demonstrated some of the ways the dissociative subtype of PTSD characterized by depersonalization and derealization manifests differently for adolescent populations than for adult populations. Adult studies of the subtype found that individuals in the dissociative group had more flashbacks, childhood sexual abuse, and adult sexual trauma than individuals in the high PTSD alone group.14 In the current study, the two high PTSD classes (dissociative subtype/high PTSD and high PTSD) did not differ significantly on number of trauma exposures or number of maltreatment trauma exposures and had similar rates of exposure to each maltreatment type. The dissociative subtype/high PTSD class had more somatic symptoms, avoidance of people, places, or things that were reminders of the trauma, sense of foreshortened future, and trauma-related guilt. This class also had more overall PTSD symptoms, dissociation symptoms, and internalizing behavior symptoms than any other class and contained 83.4% of cases of the PTSD dissociative subtype. The PTSD symptom profile for adolescents with the PTSD dissociative subtype appears to differ from that of adults, and number and characteristics of trauma exposures were not a significant variable in class differences the way they were for adults.
In Model B, the expanded conceptualization of dissociation co-occurring with PTSD captured several more nuanced dissociative subgroups, including a dissociative amnesia/detached arousal class and a dissociative subtype/high PTSD class with depersonalization and derealization playing relatively minor roles in characterizing the group compared with other dissociation symptoms. These two high dissociation classes did not differ on maltreatment exposure count, but the dissociative subtype/high PTSD class had more overall trauma exposures than the dissociative amnesia/detached arousal class and an average of seven more PTSD symptoms. Both the dissociative subtype/high PTSD class and high PTSD class—the two high PTSD groups—had more trauma exposures and maltreatment exposures and lower odds of neglect than the dissociative amnesia/detached arousal class. However, this class was unique in that it was characterized by higher relative probability of dissociative amnesia symptoms. This finding might lend support to the hypothesis that dissociation in some youth functions to obscure recall of traumatic experiences, in addition to attenuating distress. Previous studies have found severe dissociation in survivors of severe childhood maltreatment in the absence of affect dysregulation or PTSD.42 Additionally, there is evidence that amnesia for severe trauma experiences such as sexual abuse or chronic trauma experiences such as emotional neglect can occur during childhood.43, 44 This effect has been noted in studies of adult samples and is consistent with conceptualizations of the function dissociation serves in the trauma response.43–45 Although additional studies are needed to confirm this explanation, it is possible that highly dissociative youth have unrecalled trauma histories and thus require trauma-specific treatment and trauma-informed care.45
Model A demonstrates that including the two dissociative symptoms of depersonalization and derealization elucidates the dissociative subtype/high PTSD class identified with adults and that depersonalization and derealization should continue to be studied with youth.15 This model also indicated that the moderate PTSD subgroup (anxious arousal class and dysphoric arousal class) is best separated into two classes distinguished by anxiety versus dysphoria.32 Model B demonstrates that the high PTSD subgroup (dissociative subtype/high PTSD class and high PTSD class) should be separated into two classes distinguished by a wide array of dissociative symptoms, not only depersonalization and derealization—and that the more moderate PTSD subgroup may be better characterized by two classes that represent anxious arousal but are distinguished by dysphoria including dissociative amnesia, emotional detachment, and numbing.
There are strengths and limitations to this study that require consideration in interpreting the results. The study findings were consistent with prior studies demonstrating that depersonalization and derealization are less common among children than adults, possibly due to the difficulty of describing these phenomena, and that dissociation is a common coping mechanism for trauma-exposed children that becomes less common across child development and ultimately over the lifespan.46–48 The study used a large, ethnoracially diverse sample of trauma-exposed adolescents. The study was limited in that it did not include older adolescents ages 17 or 18 and that it used a DSM-IV measure of PTSD due to constraints of the dataset, which was constructed prior to the publication of the DSM-5.12, 31 It also did not elucidate how dissociation may appear in youth under age 12, another important age group to consider in future research studies.
This study demonstrates that while the DSM-5 dissociative subtype of PTSD captures an important subset of PTSD cases, there are additional prominent dissociation symptoms—some of which are more prominent than depersonalization/derealization—that would be optimal to assess for in adolescents. While PTSD-D can be distinguished from PTSD alone in adolescents, a wider range of dissociative symptoms is needed to fully characterize the co-occurrence and expression of PTSD and dissociative symptoms. Important symptoms of dissociation in the models were daydreaming, dissociative amnesia, and dissociative avoidance. There was a unique subgroup of adolescents (dissociative amnesia/detached arousal) that was symptomatic for dissociation and in particular dissociative amnesia, but less symptomatic for PTSD and behavioral symptoms. The role of dissociation in auto-attenuating trauma-related distress and obscuring recall of trauma experiences requires further study in the future. Research and clinical focus on this phenomenon may be valuable since the presence of both dissociation and PTSD results in the highest burden of symptoms and residence outside the home for adolescents. If adolescence represents a crucial moment in the life history of pathological traumatic stress responses, it may be a pivotal point for intervention.
Clinical Guidance.
Dissociation co-occurs with PTSD commonly among adolescents. Clinicians treating trauma-exposed adolescents should include assessments of dissociative symptomatology, along with assessment for PTSD.
Dissociation should be conceptualized broadly and assessed comprehensively, beyond just the dissociative subtype of PTSD, which includes depersonalization and derealization. Dissociative amnesia and dissociative avoidance may also be important symptoms.
There appears to be a unique subgroup of adolescents who are symptomatic for dissociation, particularly dissociative amnesia, and less symptomatic for PTSD and behavioral symptoms, but who still could benefit from trauma-specific treatment.
Acknowledgments
This research project was supported by the Rita & Alex Hillman Foundation, Hillman Scholars Program in Nursing Innovation (predoctoral fellowship) and the Eunice Kennedy Shriver National Institutes of Child Health and Human Development (NICHD) at the National Institutes of Health (NIH) through an individual National Research Service Award (NRSA) (1F31HD088091-01). This project was developed (in part) under grant number 2U79SM054284 from the Center for Mental Health Services (CMHS), Substance Abuse and Mental Health Services Administration (SAMHSA), U.S. Department of Health and Human Services (HHS). The views, policies, and opinions expressed are those of the authors and do not necessarily reflect those of the above funding sources.
Mr. Lee served as the statistical expert for this research.
The authors would like to acknowledge the 56 sites within the NCTSN that have contributed data to the Core Data Set as well as the children and families that have contributed to our growing understanding of child traumatic stress. Tracy Bethel, MPH, Carrie Purbeck-Trunzo, MHA, CPHQ, and Courtney Fleck, data technician, of the National Center for Child Traumatic Stress (NCCTS) at Duke University School of Medicine, facilitated access to the dataset used in this project and provided technical assistance throughout the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure: Dr. Ford is a co-owner of Advanced Trauma Solutions, Inc., which is the sole distributor of the copyrighted TARGET model by the University of Connecticut. Drs. Choi, Seng, Briggs-King, Munro-Kramer, Graham-Bermann, and Mr. Lee report no biomedical financial interests or potential conflicts of interest.
Contributor Information
Dr. Kristen R. Choi, University of California, Los Angeles.
Dr. Julia S. Seng, University of Michigan, Ann Arbor.
Dr. Ernestine C. Briggs, Duke University, Durham, NC.
Dr. Michelle L. Munro-Kramer, University of Michigan, Ann Arbor.
Dr. Sandra A. Graham-Bermann, University of Michigan, Ann Arbor.
Mr. Robert C. Lee, Duke University, Durham, NC.
Dr. Julian D. Ford, University of Connecticut, Mansfield.
References
- 1.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 2.Herman J. Trauma and Recovery. New York: Basic Books, Perseus Book Group; 1992. [Google Scholar]
- 3.van der Kolk BA, Pynoos RS, Cicchetti D, et al. [Accessed June 21, 2017];Proposal to include a developmental trauma disorder diagnosis for children and adolescents in DSM-5. 2009 http://www.traumacenter.org/announcements/DTD_NCTSN_official_submission_to_DSM_V_Final_Version.pdf.
- 4.Spiegel D, Loewenstein RJ, Lewis-Fernández R, et al. Dissociative disorders in DSM-5. Depression and anxiety. 2011;28:826. doi: 10.1002/da.20874. [DOI] [PubMed] [Google Scholar]
- 5.Putnam F. Psychobiology of Dissociation. In: Lerer B, Gershon S, editors. in New Directions Affective Disorders. New York: Springer-Verlag; 1989. pp. 463–465. [Google Scholar]
- 6.Teicher MH, Andersen SL, Polcari A, Anderson CM, Navalta CP. Developmental neurobiology of childhood stress and trauma. Psychiatr Clin North Am. 2002;25:397–426. doi: 10.1016/s0193-953x(01)00003-x. [DOI] [PubMed] [Google Scholar]
- 7.Briere J, Scott C, Weathers F. Peritraumatic and persistent dissociation in the presumed etiology of PTSD. Am J Psychiatry. 2005;162:2295–301. doi: 10.1176/appi.ajp.162.12.2295. [DOI] [PubMed] [Google Scholar]
- 8.Briere J, Runtz M, Eadie E, Bigras N, Godbout N. Disengaged parenting: structural equation modeling with child abuse, insecure attachment, and adult symptomatology. Child Abuse Negl. 2017;67:260–270. doi: 10.1016/j.chiabu.2017.02.036. [DOI] [PubMed] [Google Scholar]
- 9.Dorahy MJ, Middleton W, Seager L, Williams M, Chambers R. Child abuse and neglect in complex dissociative disorder, abuse-related chronic PTSD, and mixed psychiatric samples. J Trauma Dissociation. 2016;17:223–236. doi: 10.1080/15299732.2015.1077916. [DOI] [PubMed] [Google Scholar]
- 10.Schimmenti A, Caretti V. Linking the overwhelming with the unbearable: developmental trauma, dissociation, and the disconnected self. Psychoanal Psychol. 2016;33:106–128. [Google Scholar]
- 11.Courtois CA, Ford JD. Treating Complex Traumatic Stress Disorders: An Evidence-Based Guide. New York: Guilford Press; 2009. [Google Scholar]
- 12.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 13.Friedman MJ. Finalizing PTSD in DSM-5: Getting here from there and where to go next. J Trauma Stress. 2013;26:548–556. doi: 10.1002/jts.21840. [DOI] [PubMed] [Google Scholar]
- 14.Wolf EJ, Lunney CA, Miller MW, Resick PA, Friedman MJ, Schnurr PP. The dissociative subtype of PTSD: a replication and extension. Depress Anxiety. 2012a;29:679–688. doi: 10.1002/da.21946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolf EJ, Miller MW, Reardon AF, Ryabchenko KA, Castillo D, Freund R. A latent class analysis of dissociation and posttraumatic stress disorder: evidence for a dissociative subtype. Arch Gen Psychiatry. 2012b;69:698–705. doi: 10.1001/archgenpsychiatry.2011.1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Armour C, Karstoft KI, Richardson JD. The co-occurrence of PTSD and dissociation: differentiating severe PTSD from dissociative-PTSD. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1297–1306. doi: 10.1007/s00127-014-0819-y. [DOI] [PubMed] [Google Scholar]
- 17.Choi KR, Ford JD, Briggs EC, Munro-Kramer ML, Graham-Bermann SA, Seng JS. Relationships between maltreatment, posttraumatic symptomatology, and the dissociative subtype of PTSD among adolescents. Under Review. doi: 10.1080/15299732.2019.1572043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stein DJ, Koenen KC, Friedman MJ, et al. Dissociation in posttraumatic stress disorder: evidence from the world mental health surveys. Biol Psychiatry. 2013;73:302–312. doi: 10.1016/j.biopsych.2012.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.International Society for the Study of Trauma and Dissociation. [Accessed June 21];Child/adolescent FAQs. http://www.isst-d.org/default.asp?contentID=100.
- 20.Hamblen J, Barnett E. PTSD in children and adolescents. [Accessed June 21];National Center for PTSD. 2016 https://www.ptsd.va.gov/professional/treatment/children/ptsd_in_children_and_adolescents_overview_for_professionals.asp.
- 21.Dalenberg CJ, Brand BL, Gleaves DH, et al. Evaluation of the evidence for the trauma and fantasy models of dissociation. Psychol Bull. 2012;138:550–588. doi: 10.1037/a0027447. [DOI] [PubMed] [Google Scholar]
- 22. [Accessed June 21, 2017];Centers for Disease Control and Prevention Teenagers (15–17 years of age): Developmental milestones. https://www.cdc.gov/ncbddd/childdevelopment/positiveparenting/adolescence2.html.
- 23.Perkonigg A, Höfler M, Cloitre M, Wittchen HU, Trautmann S, Maercker A. Evidence for two different ICD-11 posttraumatic stress disorders in a community sample of adolescents and young adults. Eur Arch Psychiatry Clin Neurosci. 2016;266:317–28. doi: 10.1007/s00406-015-0639-4. [DOI] [PubMed] [Google Scholar]
- 24.Modrowski CA, Bennett DC, Chaplo SD, Kerig PK. Screening for PTSD among detained adolescents: implications of the changes in the DSM-5. Psychol Trauma. 2017;9:10–17. doi: 10.1037/tra0000156. [DOI] [PubMed] [Google Scholar]
- 25.Kerig PK, Charak R, Chaplo SD, et al. Validation of the factor structure of the adolescent dissociative experiences scale in a sample of trauma-exposed detained youth. Psychol Trauma. 2016;8:592. doi: 10.1037/tra0000140. [DOI] [PubMed] [Google Scholar]
- 26.National Child Traumatic Stress Network. [Accessed June 21]; NCCTS Leadership: The Core Data Set. 2009 http://www.nctsnet.org/nctsn_assets/pdfs/CoreDataSet_InfoBrief_FINAL.pdf.
- 27.Steinberg AM, Pynoos RS, Briggs EC, et al. The National Child Traumatic Stress Network Core Data Set: emerging findings, future directions, and implications for theory, research, practice, and policy. Psychol Trauma. 2014;(S1):S50. [Google Scholar]
- 28.Briggs EC, Greeson JK, Layne CM, Fairbank JA, Knoverek AM, Pynoos RS. Trauma exposure, psychosocial functioning, and treatment needs of youth in residential care: preliminary findings from the NCTSN Core Data Set. J Child Adolesc Trauma. 2012;5:1–15. [Google Scholar]
- 29.Greeson JK, Briggs EC, Layne CM, et al. Traumatic childhood experiences in the 21st century: broadening and building on the ACE studies with data from the National Child Traumatic Stress Network. J Interpers Violence. 2014;29:536–56. doi: 10.1177/0886260513505217. [DOI] [PubMed] [Google Scholar]
- 30.Kiser LJ, Stover CS, Navalta CP, et al. Effects of the child-perpetrator relationship on mental health outcomes of child abuse: it’s (not) all relative. Child Abuse Negl. 2014;38:1083–1093. doi: 10.1016/j.chiabu.2014.02.017. [DOI] [PubMed] [Google Scholar]
- 31.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 32.Elhai JD, Layne CM, Steinberg AM, et al. Psychometric properties of the UCLA PTSD reaction index. part II: investigating factor structure findings in a national clinic-referred youth sample. J Trauma Stress. 2013;26:10–18. doi: 10.1002/jts.21755. [DOI] [PubMed] [Google Scholar]
- 33.Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles post-traumatic stress disorder reaction index. Curr Psychiatry Rep. 2004;6:96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- 34.Steinberg AM, Brymer MJ, Kim S, et al. Psychometric properties of the ULCA PTSD reaction index: part 1. J Trauma Stress. 2013;26:1–9. doi: 10.1002/jts.21780. [DOI] [PubMed] [Google Scholar]
- 35.Briere J. Trauma Symptom Checklist for Children: Professional Manual. Odessa, FL: Psychological Assessment Resources, Inc; 1996. [Google Scholar]
- 36.Achenbach TM. Manual for Child Behavior Checklist/4–18 and 1991 Profile. Burlington, VT: University of Vermont, Department of Psychiatry; 1991. [Google Scholar]
- 37.Achenbach TM, Rescorla LA. Manual for the ASEBA School-Age Forms and Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- 38.Low LK, Seng JS, Miller JM. Use of the Optimality Index-United States in perinatal clinical research: a validation study. J Midwifery Womens Health. 2008;53:302–309. doi: 10.1016/j.jmwh.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 39.McCutcheon AL. Latent class analysis. Los Angeles: Sage; 1987. [Google Scholar]
- 40.Nylund KL, Asparouhov T, Muthén BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct Equ Modeling. 2007;14:535–569. [Google Scholar]
- 41.Asparouhov T, Muthén B. Auxiliary variables in mixture modeling: three-step approaches using M plus. Struct Equ Modeling. 2014;21:329–341. [Google Scholar]
- 42.Putnam FW. Ten-year research update review: child sexual abuse. J Am Acad Child Adolesc Psychiatry. 2003;42:269–78. doi: 10.1097/00004583-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Briere J, Conte J. Self-reported amnesia for abuse in adults molested as children. J Trauma Stress. 1993;6:21–31. [Google Scholar]
- 44.Chu JA, Frey LM, Ganzel BL, Matthews JA. Memories of childhood abuse: dissociation, amnesia, and corroboration. Am J Psychiatry. 1999;156:749–55. doi: 10.1176/ajp.156.5.749. [DOI] [PubMed] [Google Scholar]
- 45.Seng JS, D’Andrea W, Ford JD. Complex mental health sequelae of psychological trauma among women in prenatal care. Psychol Trauma. 2014;6:41. doi: 10.1037/a0031467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brunner R, Parzer P, Schuld V, Resch F. Dissociative symptomatology and traumatogenic factors in adolescent psychiatric patients. J Nerv Ment Dis. 2000;188:71–7. doi: 10.1097/00005053-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 47.Coons PM. Depersonalization and derealization. In: Michelson LK, Ray WL, editors. Handbook of Dissociation. New York: Springer US; 1996. pp. 291–305. [Google Scholar]
- 48.Shimizu M, Sakamoto S. Depersonalization in early adolescence. Psychiatry Clin Neurosci. 1986;40:603–608. doi: 10.1111/j.1440-1819.1986.tb03174.x. [DOI] [PubMed] [Google Scholar]