Abstract
Cutaneous leiomyosarcoma is a rare neoplasia, and its periorbital presentation is rather uncommon. We present a case of a male patient who was surgically treated, with the reconstruction performed with a frontal myocutaneous flap. The patient has been followed up for one year with adequate oncologic control and good aesthetic outcome.
Keywords: Leiomiossarcoma, Leiomyosarcoma, Sarcoma, Skin neoplasms, Surgical flaps
INTRODUCTION
Leiomyosarcomas represent approximately 7% of all soft tissue sarcomas, being more common on the abdomen and retroperitoneum. Cutaneous leiomyosarcoma (CLMS) is a rare neoplasia and is responsible for less than 3% of the superficial sarcomas.1 CLMS can appear on any part of the body, with predilection for the lower limbs (50 to 75%), and rarely affects the face (1 to 5%).2 Most literature data indicate a male (3:1) and Caucasian predilection, appearing more frequently in the fifth and sixth decades of life.2,3 CLMS is subdivided into dermal and subcutaneous. The former appears to originate in the piloerector smooth muscle, is locally aggressive (potential of recurrence of 30 to 50%), with little tendency to metastasize. The latter seems to arise from the muscle layeer of the vessels, has more chances of recurrence (50 to 70%) and metastasis.4,5 Enzinger considers to be CLMS only those tumors originated in the piloerector muscles, which are rarer than the subcutaneous type, that comes from the small vessels. This author further classifies as vascular leiomyosarcoma those arising from medium and large caliber vessels.1
CLMS presents clinically as a solitary nodule. The dermal variant is found adhered to the epidermis, covered by erythematous or brownish skin, tending to be smaller and present slower growth compared to the subcutaneous subtype, that is usually mobile and covered by normal skin. There can be pain on palpation, as well as pruritus, paresthesias and bleeding.1,5,6 Histologically, it is a smooth muscle cell tumor, with proliferation of spindle cells with a bulky, elongated cigar-shaped nucleus, besides pleomorphism and mitoses. The well differentiated areas of the tumor show a higher concentration of spindle cells, whereas the less well differentiated show giant, atypical cells with bizarre nuclei.2,5,6 The main immunohistochemistry markers are smooth muscle actin, desmin and vimentin.2,6
Surgical treatment is preferred, with margins of 1 cm or more, or Mohs micrographic surgery.3 We report this case due to its rarity and uncommon location, as well as its surgical treatment, that proved to be satisfactory from the oncological, functional and aesthetic point of view.
CASE REPORT
Thirty-four-year-old phototype IV male was referred for evaluation of a tumor on the medial corner of the left eye tha had been present for eight months. On dermatological examination, there was a firm, erythematous nodule, measuring 2.0 x 1.5 cm, adhered to the skin, with a central crust and located on the left nasojugal groove (Figure 1). There was pain on palpation. There were no palpable lymph nodes. An incisional biopsy was performed, and the histology revealed a poorly differentiated malignancy, with a spindle cell pattern, diffusely infiltrating the dermis (Figures 2 and 3). Immunohistochemistry was positive for specific muscle actin (HHF-35), smooth muscle actin (HUC-1) and Ki-67 in 10% of the tumor cells (Figure 4). Chest radiograph and abdominal ultrasound were normal. The patient underwent surgery with lateral, medial and inferior margins of 1.5 cm and 1 cm superior margin deep down to the periosteum. The defect was reconstructed with a frontal myocutaneous flap. Histology showed clear margins, and the patient has been followed up for one year now, with no recurrence.
Figure 1.
Firm, erythematous nodule, adhered and with central crust, measuring 2.0 x 1.5cm, located on the left nasojugal groove
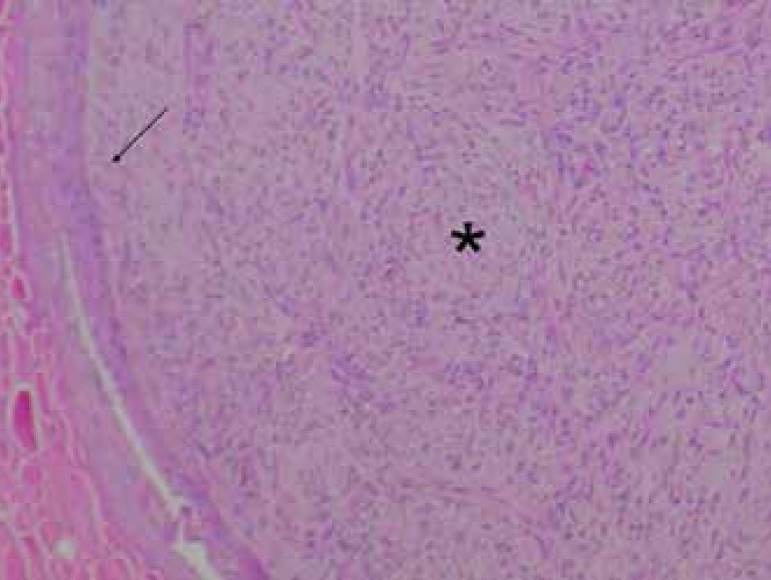
Figure 2.
Spindle cell neoplasia (*) diffusely infiltrating the dermis and epidermis (arrow) (Hematoxylin & eosin, X200)
Figure 3.
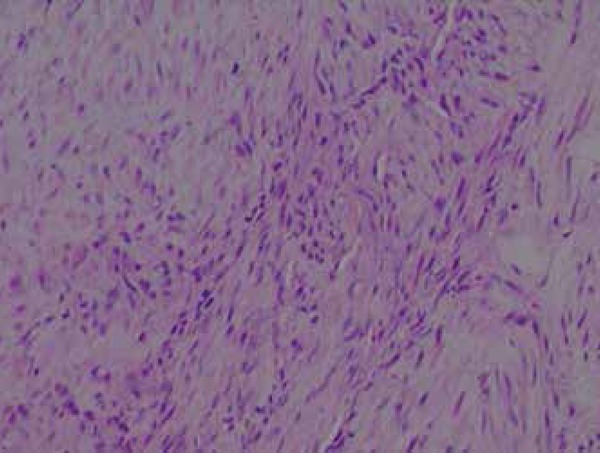
Detail of spindle cell with bulky, elongated, cigar-shaped nuclei (Hematoxylin & eosin, X400)
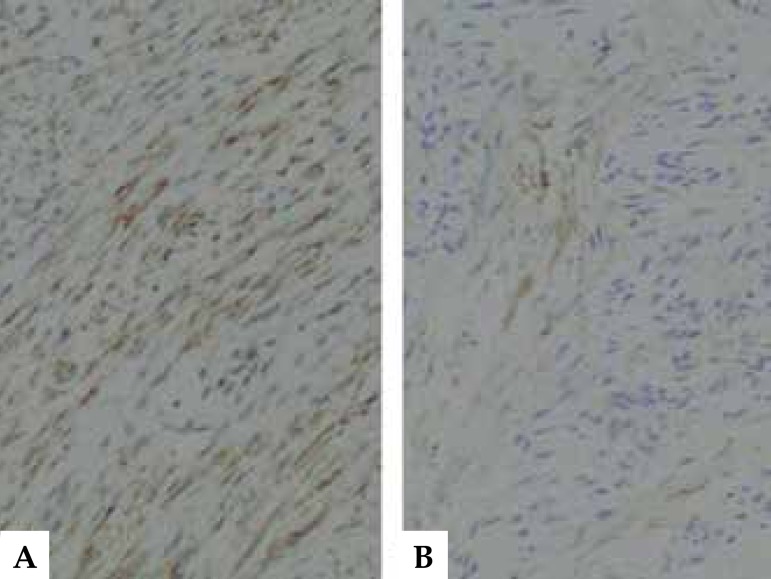
Figure 4.
Positive staining for HUC-1 (A) and desmin (B) (X200)
DISCUSSION
Leiomyosarcoma is an uncommon neoplasia, with clinical features similar to other skin tumors. In our case, the initial differential diagnoses proposed were dermatofibrosarcoma protuberans, basal cell carcinoma, squamous cell carcinoma and pilomatricoma. The final diagnosis was made after histological examination with hematoxylin and eosin (HE) in paraffin and complementary immunohistochemistry, key tests for this rare tumor.
The differentiation between dermal and subcutaneous CLMS is important because they have distinct clinical and prognostic features. The dermal type occurs in men on the fifth and seventh decades of life, has better prognosis, local recurrence rates of 14-50% and low metastatic potential; the subcutaneous type occurs in both genders equally, in a more advanced age (fifth and eighth decades of life), has a poorer prognosis with local recurrence rates that range between 40-60% and the likelihood of metastasis of 20-60%.7-9 According to Annest et al., the dermal type occurs predominantly on the head and neck, whereas the subcutaneous type favors the lower limbs.10 However, in a more recent study, the extremities were the most commonly affected area for both dermal and subcutaneous types (52% for both).7
Treatment is essentially surgical. Surgical excision with wide margins is the most used technique to treat this tumor. Despite the lack of consensus regarding the most adequate margins, studies suggest using a minimum 1cm margin.2,3,5 Mohs micrographic surgery has shown promising results, with high rates of cure and preservation of health tissue, but more cases need to be reported so that it can be considered the standard treatment technique. Chemotherapy and radiotherapy are controversial, but adjuvant radiotherapy has been used for high grade tumors, cases with positive margins, tumors larger than 5 cm and for those with extensive subcutaneous involvement.3
We report the case of a dermal CLMS, in a male, phototype IV patient, occurring at an early age and on an uncommon location. Our patient’s tumor has a better prognosis due to the lower rates of recurrence and few cases of metastasis found in the literature. In a study performed by Winchester et al, 5 out of 48 dermal CLMS cases developed metastasis, with 2 out of 5 cases resulting in death.7 We opted for a conventional surgical excision with wide margins since Mohs surgery is not available in our hospital. Adjuvant radiotherapy was not indicated because it is controversial and due to the risk of radiation induced cataracts, considering the lesion was on the periorbital area. The prognosis is favorable, considering the resection of the primary tumor showed tumor-free margins. The patient will be reviewed every six months for the first 5 years (the period with highest recurrence rates) and then annually to monitor possible recurrence and/or metastasis.10
Footnotes
Conflict of Interests: None.
Study conducted at Hospital Universitário Lauro Wanderley of the Universidade Federal da Paraíba (HULW-UFPB) - João Pessoa (PB), Brazil.
Financial Support: None.
REFERENCES
- 1.Enzinger FM, Weiss SW. Soft tissue tumors. 4th ed. St Louis, Missouri: Mosby; 2001. Leiomyosarcoma; pp. 491–508. [Google Scholar]
- 2.Fields JP, Helwig EB. Leiomyosarcoma of the skin and subcutaneous tissue. Cancer. 1981;47:156–169. doi: 10.1002/1097-0142(19810101)47:1<156::aid-cncr2820470127>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- 3.Deneve JL, Messina JL, Bui MM, Marzban SS, Letson GD, Cheong D, et al. Cutaneous leiomyosarcoma: treatment and outcomes with a standardized margin of resection. Cancer Control. 2013;20:307–312. doi: 10.1177/107327481302000408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Guillén DR, Cockerell CJ. Cutaneous and subcutaneous sarcomas. Clin Dermatol. 2001;19:262–268. doi: 10.1016/s0738-081x(01)00177-8. [DOI] [PubMed] [Google Scholar]
- 5.Bernstein SC, Roenigk RK. Leiomyosarcoma of the Skin - treatment of 34 cases. Dermatol Surg. 1996;22:631–635. doi: 10.1111/j.1524-4725.1996.tb00609.x. [DOI] [PubMed] [Google Scholar]
- 6.Fleury LFF Jr, Sanches JA Jr. Sarcomas cutâneos primários. An Bras Dermatol. 2006;81:207–221. [Google Scholar]
- 7.Winchester DS, Hocker TL, Brewer JD, Baum CL, Hochwalt PC, Arpey CJ, et al. Leiomyosarcoma of the skin: clinical, histopathologic, and prognostic factors that influence outcomes. J Am Acad Dermatol. 2014;71:919–925. doi: 10.1016/j.jaad.2014.07.020. [DOI] [PubMed] [Google Scholar]
- 8.Bernstein SC, Roenigk RK. Leiomyosarcoma of the skin: treatment of 34 cases. Dermatol Surg. 1996;22:631–635. doi: 10.1111/j.1524-4725.1996.tb00609.x. [DOI] [PubMed] [Google Scholar]
- 9.Snowden RT, Osborn FD, Wong FS, Sebelik ME. Superficial leiomyosarcoma of the head and neck: case report and review of the literature. Ear Nose Throat J. 2001;80:449–453. [PubMed] [Google Scholar]
- 10.Annest NM, Grekin SJ, Stone MS, Messingham MJ. Cutaneous leiomyosarcoma: a tumor of the head and neck. Dermatol Surg. 2007;33:628–633. doi: 10.1111/j.1524-4725.2007.33124.x. [DOI] [PubMed] [Google Scholar]