Summary
The management of morbid obesity and its metabolic complications among HIV-infected patients requires a multi-disciplinary approach, with surgical interventions as one option. We sought to assess the long-term durability of ART among HIV-infected patients undergoing bariatric procedures for the management of morbid obesity. During the study period, 7 patients underwent a bariatric surgery procedure for the management of morbid obesity: 3 patients underwent sleeve gastrectomy, 2 patients underwent laparoscopic banding, and 2 patients underwent Roux-en-Y gastric bypass surgery. Overall, the proportion of undetectable HIV viral load levels did not change after the bariatric procedures, although 2 patients did require temporary cessation of medications due to procedure-related complications. Sleeve gastrectomy and Roux-en-Y gastric bypass were safe and effective among morbidly obese HIV-infected patients in our clinic population.
Keywords: HIV, Antiretroviral therapy, Obesity, Bariatric surgery, Virologic failure
To the Editors
The prevalence of overweight/obesity among HIV-infected patients engaged in care in the U.S. is estimated to range between 30 and 40% overall [1]. Common metabolic conditions, including pre-diabetes, diabetes, dyslipidemia, and hypertension are also prevalent among HIV-infected patients, making bariatric surgery a potential option for the treatment of obesity and its related diseases in this population [2].
Surgical interventions for morbid obesity include restrictive procedures, such as adjustable gastric banding (AGB) and sleeve gastrectomy (SG), and gastrointestinal diversionary procedures, such as Roux-en-Y gastric bypass (RYGB) [3]. These interventions are associated with improvements in glycemic control among diabetic patients [4], which are driven in part by hormonal changes that are independent of weight loss [5]. Bariatric procedures among morbidly obese patients also improve quality-of-life measures [6].
There are limited data regarding the impact of bariatric procedures on oral antiretroviral therapy (ART) bioavailability, which may be different for each type of procedure. Some studies have demonstrated sub-therapeutic serum drug concentrations in HIV-infected patients after these procedures [7,8]. Regional delivery of oral ART medications to different portions of the upper gastrointestinal tract may influence systemic bioavailability [9], and the need for co-administered antacid therapy in the post-operative period may impair the gastrointestinal absorption of atazanavir [10]. Prior case series of HIV-infected patients undergoing bariatric procedures have demonstrated virologic efficacy of ART in the immediate post-operative period [11], and a single case series that included 6 patients receiving ART reported continued virologic efficacy after a median of 16 months follow-up time [9].
We performed a retrospective cohort study of HIV-infected patients who underwent bariatric surgery while receiving care at the Partnership Comprehensive Care Practice (PCCP), a multidisciplinary HIV clinic affiliated with Drexel University College of Medicine. We included all HIV-infected patients who underwent AGB, SG, or RYGB between the January 1, 2005, and July 1, 2014. We collected data from the electronic medical record regarding HIV viral load, CD4+ T cell count, weight, body mass index, metabolic parameters (random glucose, HbA1C, LDL, HDL), blood pressure, post-operative complications, use of acid suppression therapies, and changes in ART regimens. The Institutional Review Board at Drexel University College of Medicine approved the study.
During the study period, 7 patients (4 men and 3 women) underwent a bariatric surgery procedure for the management of morbid obesity: 3 underwent SG, 2 underwent AGB, and 2 underwent RYGB. The median age at the time of the procedure was 40 years (range 24—50 years) and the mean (SD) pre-operative BMI was 49.1 (12.2) kg/m2. The median CD4+ T cell count at the time of the procedure was 598 cells/µL (range 297—1857 cells/µL). The median follow-up time at the PCCP following the procedure was 27 months (range 10—60 months).
There were 2 patients with intolerance of oral medications in the post-operative period leading to prolonged time periods without ART administration. In both instances, undetectable HIV viral loads were again obtained after ART regimens were restarted. There were no significant changes in CD4+ T cell counts pre- and post-procedure (p = 0.35) or the proportion of undetectable HIV viral loads (p = 0.76).
There were no intra-operative complications for any patients. Subsequent to the procedure, 2 patients had their ART regimens changed for reasons other than patient preference. In both of these instances, the ART regimen change was prompted by the use of atazanavir in patients receiving antacid therapy. Other medication changes during the post-operative period included cessation of oral antihypertensive therapy (1 patient) and cessation of oral hypoglycemic therapy (1 patient), with therapeutic targets reached in the absence of medications.
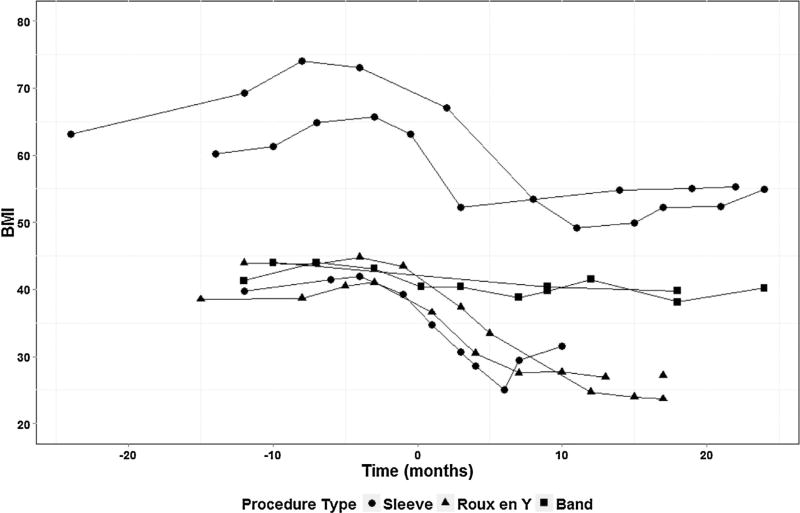
The mean BMI after surgery was 41.2 (11.7) kg/m2, which was significantly reduced from baseline (p < 0.01). Overall, the smallest reduction in BMI was observed after AGB, while larger reductions in BMI were observed after SG and RYGB (Fig. 1). Random glucose concentrations and HbA1c values were significantly reduced after surgery, whereas lipid parameters were essentially unchanged. Statistically significant decrements in both systolic and diastolic blood pressure were also observed (Table 1).
Figure 1.
Changes in BMI following bariatric procedures.
Table 1.
Changes in metabolic parameters before and after bariatric procedures.
| Parameter | Pre-procedure Mean (SD) |
Post-procedure Mean (SD) |
p-value* |
|---|---|---|---|
| BMI (kg/m2) | 49.1 (12.2) | 41.2 (11.7) | <0.01 |
| HbA1c (%) | 6.1 (0.7) | 5.6 (0.4) | <0.01 |
| Random glucose (mg/dL) | 97.5 (11.9) | 89.3 (12.3) | 0.01 |
| LDL (mg/dL) | 121.8 (34.7) | 123.0 (29.7) | 0.16 |
| HDL (mg/dL) | 47.3 (6.9) | 59.9 (15.1) | 0.07 |
| Systolic blood pressure (mm Hg) | 36.0 (16.1) | 130.4 (13.4) | <0.01 |
| Diastolic blood pressure (mm Hg) | 84.5 (7.2) | 80.8 (10.6) | 0.04 |
Within subject ANOVA for repeated measures.
Our study had several limitations. The sample size precluded the performance of adjusted statistical analyses, and we did not include a comparison group of morbidly obese patients that did not undergo bariatric procedures. Although our study was motivated by concerns regarding gastrointestinal absorption of ART medications post-surgery, we did not measure serum drug levels. Strengths of the study include the depth of clinical information obtained from the electronic medical record, and the performance of all bariatric procedures at a single centre.
In summary, SG and RYGB were safe and effective among morbidly obese HIV-infected patients in our clinic population. As more HIV-infected patients undergo these interventions, prospective studies will be required to determine whether bariatric procedures lead to changes in the gastrointestinal absorption and oral bioavailability of individual medications in ART regimens.
Acknowledgments
Dr. Vinnard is supported by NIAID (K23AI102639-02).
Footnotes
Authors contributions
SZ and CV conceived the study, SZ performed data collection, and all authors contributed to data interpretation and manuscript preparation.
Contributor Information
Steven Zivich, Department of Family Medicine, Drexel University College of Medicine, Philadelphia, USA.
Margaret Cauterucci, Division of Infectious Diseases & HIV Medicine, Department of Medicine, Drexel University College of Medicine, Philadelphia, USA.
Sara Allen, Division of Infectious Diseases & HIV Medicine, Department of Medicine, Drexel University College of Medicine, Philadelphia, USA.
Marion Vetter, Bristol Myers Squibb, Lawrenceville, USA.
Christopher Vinnard, Division of Infectious Diseases & HIV Medicine, Department of Medicine, Drexel University College of Medicine, Philadelphia, USA.
References
- 1.Keithley JK, Duloy AM, Swanson B, Zeller JM. HIV infection and obesity: a review of the evidence. J Assoc Nurses AIDS Care. 2009;20(4):260–74. doi: 10.1016/j.jana.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 2.Kral JG, Naslund E. Surgical treatment of obesity. Nat Clin Pract Endocrin Metab. 2007;3(8):574–83. doi: 10.1038/ncpendmet0563. [DOI] [PubMed] [Google Scholar]
- 3.Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, Mingrone G, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomized controlled trials. BMJ. 2013;347:f5934. doi: 10.1136/bmj.f5934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vetter ML, Ritter S, Wadden TA, Sarwer DB. Comparison of bariatric surgical procedures for diabetes remission: efficacy and mechanisms. Diabetes Spectr. 2012;25(4):200–10. doi: 10.2337/diaspect.25.4.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kaul A, Sharma J. Impact of bariatric surgery on comorbidities. Surg Clin N Am. 2011;91:1295–312. doi: 10.1016/j.suc.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 6.de Roche M, Siccardi M, Stoeckle M, Livio F, Back D, Battegay M, et al. Efavirenz in an obese HIV-infected patient — a report and an in vitro — in vivo extrapolation model indicating risk of underdosing. Antivir Ther. 2012;17(7):1381–4. doi: 10.3851/IMP2107. [DOI] [PubMed] [Google Scholar]
- 7.Razonable R, Estes L, Thompson G. Gastric bypass surgery and serum concentrations of zidovudine, lamivudine, and nelfinavir. Presented at the international conference on AIDS. 2002:14.
- 8.Fysekidis M, Cohen R, Bekheit M, Chebib J, Boussairi A, Khuong MA, et al. Sleeve gastrectomy is a safe and efficient procedure in HIV patients with morbid obesity: a case series with results in weight loss, comorbidity evolution, CD4 count, and viral load. Obes Surg. 2014 doi: 10.1007/s11695-014-1350-7. doi:10.1007. [DOI] [PubMed] [Google Scholar]
- 9.Kamimura M, Watanabe K, Kobayakawa M, Mihara F, Edamoto Y, Teruya K, et al. Successful absorption of antiretroviral drugs after gastrojejunal bypass surgery following failure of therapy through a jejunal tube. Intern Med. 2009;48(12):1103–4. doi: 10.2169/internalmedicine.48.1906. [DOI] [PubMed] [Google Scholar]
- 10.Falcon RW, Kakuda TN. Drug interactions between HIV protease inhibitors and acid-reducing agents. Clin Pharmacokinet. 2008;47(2):75–89. doi: 10.2165/00003088-200847020-00001. [DOI] [PubMed] [Google Scholar]
- 11.Selke H, Norris S, Osterholzer D, Fife K, DeRose B, Gupta S. Bariatric surgery outcomes in HIV-infected subjects: a case series. AIDS Patient Care STDs. 2010;24(9):545–50. doi: 10.1089/apc.2010.0132. [DOI] [PubMed] [Google Scholar]