Abstract
Background and purpose
Previous research has highlighted the importance of cognitive appraisal processes in determining the nature and effectiveness of coping with chronic pain. Two of the key variables implicated in appraisal of pain are catastrophizing and perceived injustice, which exacerbate the severity of pain-related distress and increase the risk of long-term disability through maladaptive behavioral responses. However, to date, the influences of these phenomena have not been examined concurrently, nor have they been related specifically to quality of life measures, such as life satisfaction.
Methods
Using data from an online survey of 330 individuals with chronic pain, structural path modeling techniques were used to examine the independent effects of pain catastrophizing, perceived injustice, and average pain intensity on life satisfaction. Two potential mediators of these relationships were examined: depressive symptoms and pain-related interference.
Results
Results indicated that depressive symptoms fully mediated the relationship between pain catastrophizing and life satisfaction, and pain interference fully mediated the relationship between pain intensity and life satisfaction. Both depressive symptoms and pain interference were found to significantly mediate the relationship between perceived injustice and life satisfaction, but perceived injustice continued to demonstrate a significant and negative relationship with life satisfaction, above and beyond the other study variables.
Conclusions
The current findings highlight the distinct affective and behavioral mediators of pain and maladaptive cognitive appraisal processes in chronic pain, and highlight their importance in both perceptions of pain-related interference and longer-term quality of life.
Keywords: Pain catastrophizing, perceived injustice, life satisfaction, pain interference, depression
Introduction
The role of cognitive appraisals in coping and overall adjustment to chronic pain has been well-documented (1, 2). Appraisals typically develop in a milieu of cultural orientations and justice principles (3), rendering socially-constructed justice principles of the pain experience (e.g. fairness of the experience), an emerging area of study. Perception of injustice, defined as an appraisal reflecting the severity and irreparability of injury- or disability-related loss, blame, and unfairness, has been identified as a significant barrier to effective recovery after acute injury (4–7), and predicts poorer outcomes in both acute pain and chronic pain populations (4, 6). For example, individuals who view their pain as unjust tend to report greater pain (8, 9) and depressive symptoms (10–12) and show greater susceptibility to maladaptive pain behaviors (13, 14). Perceived injustice may bias an individual’s appraisal process to loss and blame-related cues, thus limiting their coping repertoire.
In addition to injustice appraisals, other cognitive processes can complicate effective adaptation to chronic pain, most notably viewing pain as a catastrophic personal experience. Pain catastrophizing is a pattern of negative key appraisal process, defined as “exaggerated cognitive and affective reaction to an expected or actual pain experience” (15). It plays an important role in chronic pain and appears to be directly related to pain intensity, disability, emotional distress, and physical dysfunction (16–19). Pain catastrophizing narrows an individual’s cognitive focus to threat-related cues, which subsequently contributes to rigid and less effective coping styles (20, 21).
Variability in appraisal processes has been shown to be related to adjustment and recovery outcomes (22); however, the degree of overlap between these processes, as well as the mechanisms of effect, remain unclear. Of interest are mechanisms related to emotional distress and perceptions of daily life function, as they can facilitate targeted interventions and influence broader life outcomes. For example, depression in chronic pain may occur because pain impedes an individual’s motivation to achieve goals and engage in valued pursuits (23, 24) thereby reducing quality of life. Similarly, pain-related interference shows a longitudinal relationship with emotional distress (25) and low life satisfaction in some pain populations (26), highlighting the possibility that broader perceptions of pain as a barrier to function might mediate the relationship between appraisals of pain and quality of life outcomes.
It is notable that beyond the initial validation study that demonstrated some incremental predictive validity of a measure of perceived injustice above and beyond the effects of pain catastrophizing (6), perceived injustice and pain catastrophizing are rarely examined together in predictive models. The current study examined the direct effects of pain intensity, perceived injustice, and pain catastrophizing on life satisfaction in an Internet-based sample of 330 individuals with chronic pain. Based on the expectation that the effects of chronic pain-specific factors may influence life satisfaction through indicators of broader physical and psychosocial function, we expected that a significant degree of the effects of pain intensity, pain catastrophizing and perceived injustice on life satisfaction would be explained by the presence of depressive symptoms and pain-related interference.
Methods
Procedure
The current study constitutes a secondary data analysis of a questionnaire validation study (manuscript in preparation; results not reported here). Participants were asked to complete a set of Internet-based questionnaires. Participants were recruited via e-mails sent to prior participants from the Stanford Neuroscience and Pain Laboratory, and via an open recruitment link posted by the National Pain Report (www.nationalpainreport.com). Study measures were administered using the REDCap online survey system (27). All responses were anonymous, and participants were not compensated for their participation. As a result, the study was approved by the Stanford University Institutional Review Board as an exempt protocol. Participant consent was obtained through the REDCap system by clicking a link after being provided an information sheet on the online study; participants could not advance to completing study questionnaires without completing the online informed consent. Eligibility criteria were minimal: being 18 years of age or older, being able to read and write in English, and the presence of a chronic pain condition. As the initial target of the study was validation of a self-report measure containing an item pool of 35 items, a sample of at least 350 was considered optimal.
Participants
The initial online data collection included 497 people who completed the online consent; of these, 330 participants provided sufficient data to be included in the current analysis, which constituted the sample for analysis. The sample was 90% female and predominantly Caucasian (92.7% of the overall sample). Median age, which was assessed using a categorical variable reflecting 10-year increments, was between 40 and 49 years. Regarding marital status, 54.8% of the sample reported being married at the time of data collection. Median education level was a completed Associate’s Degree. Mean average pain intensity over the previous 30 days was 6.42 (SD = 1.53) out of 10, and mean pain duration was 15 years (SD = 6.42, range: 1 year to 60 years). Regarding psychological history, 43.6% of the sample reported a previous mental health diagnosis, 50.3% of the sample reported no prior mental health diagnosis, and 6.1% declined to answer this question. Pain diagnosis information was obtained via self-report, and was broadly categorized according to common causes of pain (e.g., nerve pain) or common pain diagnoses (e.g., fibromyalgia). Participants reported their prior pain diagnoses using a free-text entry, which was then coded by the lead author into 12 pain categories. Pain diagnosis categories were not mutually exclusive: 138 participants endorsed a single pain category, 103 participants endorsed 2 pain categories, 30 participants endorsed 3 or more pain categories, and 8 participants endorsed 4 or more pain categories. Full diagnosis information can be found in Table 1. The most commonly endorsed pain categories were fibromyalgia, musculoskeletal pain, nerve pain, pain associated with a rheumatic or autoimmune disease, and headaches or orofacial pain.
Table 1.
Pain diagnosis information
| Pain Group | N (% of Sample) |
|---|---|
| Central | 6 (1.8%) |
| Complex Regional Pain Syndrome | 17 (5.2%) |
| Ehlers-Danlos/Mixed Connective Tissue Disorder | 11 (3.3%) |
| Fibromyalgia | 155 (47.0%) |
| Gastrointestinal/Pelvic Pain | 20 (6.1%) |
| Headaches/Orofacial Pain | 35 (10.6%) |
| Musculoskeletal Pain | 76 (23.0%) |
| Myofascial Pain | 12 (3.6%) |
| Nerve Pain | 80 (24.2%) |
| Neurological Condition | 6 (1.2%) |
| Rheumatic/Autoimmune Condition | 39 (11.8%) |
| Vascular Condition | 3 (0.9%) |
| Unsure about diagnosis | 7 (2.1%) |
Measures
PROMIS Depression and Pain Interference
Depression and pain interference were assessed using 6-item short-form versions of the Patient-Reported Outcome Measurement Information System (PROMIS) Depression and Pain Interference instruments (28). PROMIS Depression items assess negative mood, negative views of the self, negative cognitions, and decreased positive emotion and engagement. PROMIS pain interference items assess the severity of pain-related interference in multiple domains of life, including social, recreational, cognitive, emotional, and overall physical functioning domains. All PROMIS assessments were converted from raw scores to t-scores, consistent with their initial publications. Higher scores on depression signified greater severity of these symptoms. Similarly, higher scores on PROMIS Pain Interference reflect greater pain-related interference. Questions were framed according the experience of symptoms or functioning over the past 7 days using a 5-point Likert scale from 1 (“Never”) to 5 (“Always). In this sample, both measures demonstrated high internal consistency (depression α = .929; pain interference α = .934).
Pain intensity
Average pain intensity over the previous 30 days was rated on an 11-point numerical rating scale (NRS) with 0 representing “no pain” and 10 representing “worst pain imaginable.” Use of numerical rating scale has been identified as a suitable assessment of pain intensity in acute and chronic pain populations in previous studies (29).
Life satisfaction
Life satisfaction was assessed using the 5-item Satisfaction with Life Questionnaire (SWLS). The 5-item measure assesses satisfaction with life as a whole. For each item, participants rate their satisfaction on a scale from 1 (strongly disagree) to 7 (strongly agree); scores are summed to calculate a total score that ranges from 5 to 35 (with higher scores reflecting greater life satisfaction). This scale shows discriminant validity from emotional well-being measures, good test-retest stability and sufficient sensitivity to detect changes (30). In this sample, this measure demonstrated adequate internal consistency (Cronbach’s α = .881).
Pain catastrophizing
Pain catastrophizing was assessed using the Pain Catastrophizing Scale (31), a 13-item self-report questionnaire widely used to assess catastrophizing tendencies in chronic pain research and clinical settings. The PCS directs respondents to consider how they tend to think and feel in the broad context of pain stimuli. A sample item from the PCS: “I become afraid that the pain will get worse”. Respondents rate their endorsement of frequency for each item using a 0–4 Likert scale 0 (not at all) to 4 (all the time). The PCS is comprised of three subscales: magnification, rumination, and feelings of helplessness. All items are summed to create a total score. The psychometric validity of the PCS has been demonstrated.(32, 33) In the current sample, the internal consistency of the PCS was high (Cronbach’s α = .943).
Perceived injustice
Perceived injustice was assessed using the Injustice Experience Questionnaire (IEQ)(6). The construct of perceived injustice encompasses two related domains: irreparability of loss and self-blame (6). The IEQ consists of 12 items, scored from 0 (never) to 4 (all the time); IEQ scores are computed as a sum score with a range from 0 to 48, with higher scores representing greater perceived injustice. The IEQ has demonstrated adequate psychometric properties (6), and been validated for use in both acute injury samples (6, 11) and chronic pain samples (34, 35). In the current sample, the internal consistency of the IEQ was high (Cronbach’s α = .904).
Analyses
Path models were estimated using Mplus software, Version 6.12 (36) to test the direct and indirect effects of average pain intensity, pain catastrophizing, and perceived injustice on life satisfaction through ratings of depression and pain interference. Missing data were handled using Full Information Maximum Likelihood (FIML) estimation, which is designed to include all available information. Indirect effects were estimated using a 1000-draw bootstrap-estimated product of coefficients (ab) approach, which is preferable to normal theory mediation analytic approaches due to greater statistical power and a lower risk of Type-I error (37). It should be noted that our use of the term “mediation” refers to the analytic approach of establishing a direct effect of an exogenous predictor (e.g., perceived injustice, pain intensity) on a mediator (the a path) and the effect of the mediator (e.g., pain interference, depressive symptoms) on an endogenous outcome (life satisfaction), above and beyond the effects of the predictor (the b path). This type of mediation analysis is concluded by testing the statistical significance of the product of the a and b path coefficients (38). However, there are other assumptions inherent within statistical mediation (i.e., assumptions of temporal precedence and strong causal inference regarding effects from each predictor to each mediator to each outcome) that cannot be satisfied with cross-sectional data analysis. It is therefore optimal to refer to “mediators” in cross-sectional models as “intervening variables” (38). With this caveat in mind, however, we continue to refer to mediation analysis for the sake of consistency throughout the manuscript. All model parameters are presented as standardized path coefficients to allow comparison across paths; as Mplus does not output significance values for standardized path coefficients in conjunction with bootstrapping procedures, these significance values are drawn from equivalent unstandardized path models. In addition to relative size of standardized beta coefficients, r2 variance statistics were used to determine the amount of variance accounted for in each endogenous variable (i.e., a variable that is modeled as an outcome in our model, including both mediators and outcomes) by each predictor when modeled separately, as well as the total amount of variance accounted for in the fully-specified model. Adequacy of model fit is represented by chi-square (χ2), the comparative fit index (CFI), the Tucker-Lewis Index (TLI), the root mean square of approximation (RMSEA), and the standardized root mean square residual (SRMR). Model fit was deemed to be adequate if CFI and TLI were greater than .90 and RMSEA and SRMR values were less than .05 (39).
Results
Descriptive statistics can be found in Table 2, correlations between study variables can be found in Table 3, and the total proportion of variance of the outcome variable (R2) accounted for in each model can be found in Table 4.
Table 2.
Descriptive Statistics
| Study variable | Mean (SD) |
|---|---|
| Pain Intensity | 6.42 (1.53) |
| Pain Catastrophizing | 23.3 (12.7) |
| Perceived Injustice | 30.0 (10.3) |
| Depression | 61.8 (8.19) |
| Pain Interference | 67.8 (6.20) |
| Life Satisfaction | 15.3 (7.65) |
Note: Depression and Pain Interference are t-scores (mean = 50, standard deviation = 10)
Table 3.
Correlations between study variables.
| Pain intensity | Pain catastrophizing | Perceived injustice | Depression | Pain interference | Life satisfaction | |
|---|---|---|---|---|---|---|
| Pain Intensity | 1 | .373 | .293 | .319 | .388 | −.242 |
| Pain Catastrophizing | 1 | .753 | .688 | .513 | −.491 | |
| Perceived Injustice | 1 | .608 | .493 | −.557 | ||
| PROMIS Depression | 1 | .532 | −.525 | |||
| PROMIS Pain Interference | 1 | −.438 | ||||
| Life Satisfaction | 1 |
PROMIS assessments are based on a mean of 50 with an SD of 10.
PROMIS, Patient-Reported Outcomes Measurement Information Systems
Note: All p-values significant at p < .01.
Table 4.
Variance Accounted for in the Fully Specified Model (R2)
| Pain intensity Main Effect | Pain Catastrophizing Main Effect | Perceived Injustice Main Effect | Fully Specified Model | |
|---|---|---|---|---|
| Life satisfaction | .061 | .241 | .310 | .377 |
| Depressive symptoms | .102 | .473 | .369 | .503 |
| Pain interference | .150 | .263 | .243 | .353 |
When the total effects of each study predictor were examined in a univariate model (i.e., without any other predictors in the model), higher levels of pain intensity (β = −.247, p < .001), pain catastrophizing (β = −.494, p < .001), and perceived injustice (β = −.558, p < .001) significantly predicted lower levels of life satisfaction. According to the r2 variance statistic, the main effect of perceived injustice accounted for the largest proportion of variance in life satisfaction, followed by pain catastrophizing, and pain intensity. In the initial specification of the path model, no relationship was specified between pain interference and depressive symptoms; however, the resulting fit indices indicated significant model misfit (χ2(3) = 35.08, p < .001; RMSEA = .181; CFI = .939; TLI = .755; SRMR = .048). These model fit indices suggest that a significant degree of covariance was not accounted for in this model specification. Consequently, it was assumed that this model misfit resulted from the lack of a modeled relationship between pain interference and depressive symptoms, which has been noted in prior studies (25, 40). As a result, exploratory models were estimated specifying either an effect of pain interference on depressive symptoms, or an effect of depressive symptoms on pain interference. The specified model appeared to better account for the covariance between variables when the model included an effect of depressive symptoms on pain interference, so this path was included in the final model.
The final specified model, which includes standardized beta coefficients for each path, is represented in Figure 1. In the final specified model, depressive symptoms, pain interference, and perceived injustice continued to show a significant relationship with life satisfaction. No significant effects of pain intensity and pain catastrophizing were noted on life satisfaction after inclusion of pain interference and depressive symptoms. Similarly, pain intensity was not found to predict depressive symptoms, nor did pain catastrophizing predict pain interference in the final model. As a result, these effects were not specified in the final estimated model. The fully-specified model yielded model fit indices that were suggestive of good model fit (χ2(4) = 5.45, p = .24; RMSEA = .033; CFI = .997; TLI = .992; SRMR = .017). Subsequent mediation analyses suggested that depressive symptoms accounted for a significant degree of the relationship between pain catastrophizing and life satisfaction (ab = −.131, p < .001) and accounted for a significant degree of the relationship between perceived injustice and life satisfaction (ab = −.052, p = .006). Similarly, pain interference was found to account for a significant degree of the variance in the relationship between perceived injustice and life satisfaction (ab = −.034, p = .018) and the relationship between pain intensity and life satisfaction (ab = .034, p = .019). Inclusion of all predictors and intervening variables in the model accounted for 37.7% of the variance in life satisfaction.
Figure 1.
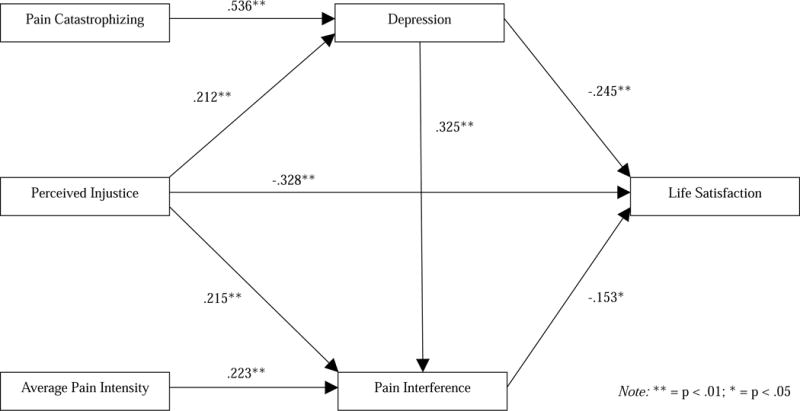
Depressive symptoms and pain interference as intervening variables of the effects of pain intensity, pain catastrophizing, and perceived injustice on life satisfaction.
Note: All path coefficients reflect standardized beta coefficients from the fully-specified model.
Discussion
The relationship between cognitive appraisals of pain and general life satisfaction is influenced by a complex interplay of emotional and physical factors. In a sample of 330 individuals with chronic pain, our analyses suggested significant bivariate relationships of both pain intensity and cognitive appraisals with life satisfaction, by which higher scores for pain catastrophizing, perceived injustice and pain intensity correlated with lower life satisfaction. Notably, our findings revealed more robust associations of perceived injustice and pain catastrophizing with life satisfaction, compared to effects of pain intensity. Our results support and extend previous findings demonstrating the role of psychological factors in coping and adjustment among individuals with chronic pain (1, 2). Specifically, injustice perceptions and catastrophic appraisal about pain appear to have stronger associations with life satisfaction than pain intensity.
Given the complex and multifactorial nature of psychological responses to chronic pain, we opted to estimate our hypothesized study model using a structural path modeling approach. These models, which allow for the simultaneous estimation of multivariate mediation models, also allow for more effective modeling of complex psychological phenomena. In this respect, our analyses revealed several indirect effects in the relationship between life satisfaction and both pain intensity and appraisals (catastrophizing and perceived injustice). Our results suggest that pain-related interference in daily life and depressive symptoms are related to broad pain-relevant variables (e.g., pain intensity, maladaptive appraisal patterns related to pain), but also appear to map more closely onto patterns of life satisfaction than these other pain-relevant variables.
Unsurprisingly, the indirect effects of the cognitive appraisal variables overlapped to some degree with the effects of pain, as perceived injustice in particular appeared to show an effect on life satisfaction through both pain interference and depressive symptoms. Further, these intervening variables were themselves linked; only by specifying a relationship between them was an adequate degree of model fit achieved. Despite the overlapping nature of these effects, a few distinctions are noteworthy: with both depressive symptoms and pain interference in the model, we found no remaining relationship between either pain catastrophizing or pain intensity with life satisfaction, suggesting that depressive symptoms and pain interference may act as more proximal factors (i.e., factors that track more closely with life satisfaction). The relative contributions of pain interference and depressive symptoms, compared to pain interference or catastrophizing, is a key finding, given prior research that both intensity and catastrophizing about pain are related to quality of life metrics in chronic pain (41). Although we cannot state that these effects follow any particular causal sequence, and despite the relatively high degree of overlap between these constructs, our analyses help to identify a few factors that most closely relate to concurrent ratings of life satisfaction (namely, pain interference and depressive symptoms).
Interestingly, perceived injustice continued to show an effect, above and beyond these other effects, suggesting that there may be other potential mediators that were not assessed in the current study that may connect these variables. For instance, feelings of social isolation and anger, which have shown significant conceptual and statistical relationships with perceived injustice in prior studies (9, 42) may be candidates for future mediation research. Perceived injustice has been conceptualized as a cognitive antecedent for anger (3), as both share in the common the experience of “being wronged” (43). Hence, anger could serve as a mechanism for the impact of perceived injustice on health outcomes; a finding supported by rehabilitation studies (35, 44). Further, strong beliefs of injustice or inequity related to pain appears to yield significant feelings of disconnection or social isolation from others, which correlates strongly with anger (42). As social relationships are considered to be a key determinant in quality of life (45–47), feelings of isolation or disconnection may be key factors that yield incremental gains in predicting quality of life in individuals with chronic pain.
The current findings highlight the distinct affective and behavioral mediators of pain and maladaptive cognitive appraisal processes in chronic pain, and highlight their importance in both perceptions of pain as a barrier to meaningful function and in longer-term quality of life. More importantly, we included perceived injustice in our models, a relatively new but important construct to consider when studying coping and function in the context of pain, which accounted for the largest proportion with life satisfaction when modeled as a main effect. We thus urge study of the consequences of both perceived injustice and pain catastrophizing, as both of these patterns of maladaptive cognitive appraisal may have interrelated and distinct consequences for quality of life for people living with chronic pain.
Limitations
Data used in the current analysis were collected from a single time point, which results in significant limitations in interpretability. The cross-sectional nature of our data precludes interpretations regarding temporal precedence or causality. Also, data were not collected on anger or social isolation, both of which show robust relationships with perceived injustice and has significant implications for pain and health-related outcomes (42, 48–51). It is also possible that other factors (e.g., behavioral avoidance, social conflict) may mediate this effect, though additional study is warranted. Additionally, the current study sample was overwhelmingly female and Caucasian; we underscore the need to replicate this work in samples with greater diversity.
It is also notable that the model we tested was nearly saturated, suggesting that there was significant covariance between each examined exogenous and endogenous variable (as indicated, for example, by the poor model fit when we did not free depression and pain interference to co-vary in our earlier model). In this respect, it should be noted that these variables are significantly related to one another and our examined mediation analyses allowed us only to examine the topology of effects; by including pain interference and depression as mediators, the residual direct effects of pain intensity and pain catastrophizing on life satisfaction were no longer significant. We do not claim that this proposed model reflects strictly unidimensional effects. Indeed, it stands to reason that for individuals who are more depressed or perceive greater pain-related interference in daily life, they may be more prone to catastrophizing or to report greater pain intensity, as there is some evidence that improvements in depressive symptoms may presage improvements in pain intensity and function (52). It is likely that these constructs are strongly mutually influential, and our results should be interpreted with this caveat in mind.
Additionally, chronic pain was loosely defined as an inclusion criterion, and showed considerable heterogeneity in sample. Despite strengths in generalizability, this heterogeneity precludes clear comparisons of these effects across different pain conditions. For instance, research shows that headaches have a neurological basis, and they are likely initiated by one of numerous pathways including nerve stimulation, irritation or disinhibition (53). This factor may influence patients’ attributions regarding the etiology of their conditions, which may impact their coping style and subsequent adjustment. Further, our use of broad self-reported pain categories, which was necessary due to the open-ended nature of our pain diagnosis question, may include some degree of error in terms of participants’ beliefs regarding the etiology of their pain. As a result, our pain diagnosis categories should be interpreted only as a broad-level description of the pain locations and characteristics of our mixed chronic pain sample. Identifying moderator variables including the etiology and physiological mechanisms of pain transmission may further clarify how these appraisal processes differ across pain conditions and, potentially, inform more targeted interventions.
Future Directions
As noted previously, our findings warrant replication and extension in longitudinal studies. As appraisal processes may vary across time due to general adaptation, changes in pain intensity or quality, or psychological intervention, examination of how these factors interrelate across time may yield additional information regarding causality and the temporal ordering of effects. Similarly, replication of these findings in clinical studies targeting pain intensity, pain catastrophizing, or perceived injustice may help to elucidate differential patterns of treatment response due to different participant characteristics. To date, there have been no published studies examining perceived injustice as a key mediator of treatment; indeed, the degree to which perceived injustice beliefs vary across time or may be changed via clinical intervention is unclear. However, our findings highlight that this variable may be a key target for interventionin terms of promoting better emotional well-being and overall quality of life.
Conclusions
The current study presents a cross-sectional path model representing distinct and overlapping effects of pain intensity, pain catastrophizing, and perceived injustice on life satisfaction, mediated by perceptions of pain-related interference and depressive symptomatology. The relative salience of perceived injustice as a potential determinant of quality of life in individuals with chronic pain suggests that this factor may be underappreciated, understudied and undertreated. Our results require replication and extension in specific pain populations across clinical and longitudinal studies, but continue to expand upon evidence of the highly complex and multifactorial nature of pain coping.
Highlights.
Pain intensity and cognitive factors contribute to reduced life satisfaction
These effects were fully mediated by pain interference and depressive symptoms
Perceived injustice predicted life satisfaction, above and beyond other variables
Acknowledgments
This work was supported by the National Institutes of Health (NIH) NIDA T32DA035165 (JAS, MSZ) and K24DA029262 (SCM), NCCIH R01AT008561 and P01AT006651 (BDD, SCM). The authors would like to offer their sincere thanks to The National Pain Report for their assistance with this project.
Disclosure statement: This work was supported by the National Institutes of Health (NIH) NIDA T32DA035165 (JAS, MSZ) and K24DA029262 (SCM), NCCIH R01AT008561 and P01AT006651 (BDD, SCM).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have no conflicts of interest to disclose.
Ethical Issues
The current study was conducted under an IRB-approved protocol for an observational study (a questionnaire validation study; study results not presented here). Participant consent was obtained using the online REDCap system by clicking a link after being provided an information sheet on the online study; participants could not advance to completing study questionnaires without completing the online informed consent. The study protocol was not registered with any organization outside of the institution where the study was conducted.
References
- 1.Esteve R, Ramirez-Maestre C, Lopez-Marinez AE. Adjustment to chronic pain: the role of pain acceptance, coping strategies, and pain-related cognitions. Ann Behav Med. 2007;33(2):179–88. doi: 10.1080/08836610701309724. [DOI] [PubMed] [Google Scholar]
- 2.Woby SR, Watson PJ, Roach NK, Urmston M. Adjustment to chronic low back pain–the relative influence of fear-avoidance beliefs, catastrophizing, and appraisals of control. Behav Res Ther. 2004;42(7):761–74. doi: 10.1016/S0005-7967(03)00195-5. [DOI] [PubMed] [Google Scholar]
- 3.Monden KR, Trost Z, Scott W, Bogart KR, Driver S. The unfairness of it all: Exploring the role of injustice appraisals in rehabilitation outcomes. Rehabil Psychol. 2016;61(1):44. doi: 10.1037/rep0000075. [DOI] [PubMed] [Google Scholar]
- 4.McParland JL, Eccleston C. “It’s Not Fair” Social Justice Appraisals in the Context of Chronic Pain. Curr Dir Psychol Sci. 2013;22(6):484–9. doi: 10.1177/0963721413496811. [DOI] [Google Scholar]
- 5.McParland JL, Eccleston C, Osborn M, Hezseltine L. It’s not fair: an interpretative phenomenological analysis of discourses of justice and fairness in chronic pain. Health. 2011;15(5):459–74. doi: 10.1177/1363459310383593. [DOI] [PubMed] [Google Scholar]
- 6.Sullivan MJ, Adams H, Horan S, Maher D, Boland D, Gross R. The role of perceived injustice in the experience of chronic pain and disability: scale development and validation. J Occup Rehabil. 2008;18(3):249–61. doi: 10.1007/s10926-008-9140-5. [DOI] [PubMed] [Google Scholar]
- 7.Sullivan MJ, Scott W, Trost Z. Perceived injustice: a risk factor for problematic pain outcomes. Clin J Pain. 2012;28(6):484–8. doi: 10.1097/AJP.0b013e3182527d13. [DOI] [PubMed] [Google Scholar]
- 8.Ferrari R, Russell AS. Perceived injustice in fibromyalgia and rheumatoid arthritis. Clin Rheumatol. 2014;33(10):1501–7. doi: 10.1007/s10067-014-2552-z. [DOI] [PubMed] [Google Scholar]
- 9.Scott W, Trost Z, Bernier E, Sullivan MJ. Anger differentially mediates the relationship between perceived injustice and chronic pain outcomes. PAIN®. 2013;154(9):1691–8. doi: 10.1016/j.pain.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 10.Scott W, Sullivan M. Perceived injustice moderates the relationship between pain and depressive symptoms among individuals with persistent musculoskeletal pain. Pain Res Manage. 2012;17(5):335–40. doi: 10.1155/2012/501260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trost Z, Agtarap S, Scott W, Driver S, Guck A, Roden-Foreman K, Reynolds M, Foreman ML, Warren AM. Perceived injustice after traumatic injury: Associations with pain, psychological distress, and quality of life outcomes 12 months after injury. Rehabil Psychol. 2015;60(3):213–21. doi: 10.1037/rep0000043. [DOI] [PubMed] [Google Scholar]
- 12.Yakobov E, Scott W, Tanzer M, Stanish W, Dunbar M, Richardson G, Sullivan MJL. Validation of the Injustice Experiences Questionnaire adapted for use with patients with severe osteoarthritis of the knee. J Arthritis. 2014;2014 doi: 10.4172/2167-7921.1000130. [DOI] [Google Scholar]
- 13.Sullivan MJ, Davidson N, Garfinkel B, Siriapaipant N, Scott W. Perceived injustice is associated with heightened pain behavior and disability in individuals with whiplash injuries. Psychol Inj Law. 2009;2(3–4):238–47. doi: 10.1007/s12207-009-9055-2. [DOI] [Google Scholar]
- 14.Yakobov E, Scott W, Stanish W, Dunbar M, Richardson G, Sullivan M. The role of perceived injustice in the prediction of pain and function after total knee arthroplasty. Pain. 2014;155(10):2040–6. doi: 10.1016/j.pain.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 15.Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17(1):52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Edwards RR, Cahalan C, Mensing G, Smith M, Haythornthwaite JA. Pain, catastrophizing, and depression in the rheumatic diseases. Nat Rev Rheumatol. 2011;7(4):216–24. doi: 10.1038/nrrheum.2011.2. [DOI] [PubMed] [Google Scholar]
- 17.Flor H, Behle DJ, Birbaumer N. Assessment of pain-related cognitions in chronic pain patients. Behav Res Ther. 1993;31(1):63–73. doi: 10.1016/0005-7967(93)90044-u. [DOI] [PubMed] [Google Scholar]
- 18.Sturgeon JA, Zautra AJ. State and trait pain catastrophizing and emotional health in rheumatoid arthritis. Ann Behav Med. 2013;45(1):69–77. doi: 10.1007/s12160-012-9408-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Westman AE, Boersma K, Leppert J, Linton SJ. Fear-avoidance beliefs, catastrophizing, and distress: a longitudinal subgroup analysis on patients with musculoskeletal pain. Clin J Pain. 2011;27(7):567–77. doi: 10.1097/AJP.0b013e318219ab6c. [DOI] [PubMed] [Google Scholar]
- 20.Crombez G, Eccleston C, Van Damme S, Vlaeyen JW, Karoly P. Fear-avoidance model of chronic pain: the next generation. Clin J Pain. 2012;28(6):475–83. doi: 10.1097/AJP.0b013e3182385392. [DOI] [PubMed] [Google Scholar]
- 21.Crombez G, Viane I, Eccleston C, Devulder J, Goubert L. Attention to pain and fear of pain in patients with chronic pain. J Behav Med. 2013;36(4):371–8. doi: 10.1007/s10865-012-9433-1. [DOI] [PubMed] [Google Scholar]
- 22.Sullivan MJ, Yakobov E, Scott W, Tait R. Perceived injustice and adverse recovery outcomes. Psychol Inj Law. 2014;7(4):325–34. doi: 10.1007/s12207-014-9209-8. [DOI] [Google Scholar]
- 23.Harris S, Morley S, Barton SB. Role loss and emotional adjustment in chronic pain. Pain. 2003;105(1–2):363–70. doi: 10.1016/s0304-3959(03)00251-3. [DOI] [PubMed] [Google Scholar]
- 24.Morley S, Davies C, Barton S. Possible selves in chronic pain: self-pain enmeshment, adjustment and acceptance. Pain. 2005;115(1–2):84–94. doi: 10.1016/j.pain.2005.02.021. [DOI] [PubMed] [Google Scholar]
- 25.Arola HM, Nicholls E, Mallen C, Thomas E. Self‐reported pain interference and symptoms of anxiety and depression in community‐dwelling older adults: Can a temporal relationship be determined? Eur J Pain. 2010;14(9):966–71. doi: 10.1016/j.ejpain.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 26.Oster G, Harding G, Dukes E, Edelsberg J, Cleary PD. Pain, medication use, and health-related quality of life in older persons with postherpetic neuralgia: results from a population-based survey. J Pain. 2005;6(6):356–63. doi: 10.1016/j.jpain.2005.01.359. [DOI] [PubMed] [Google Scholar]
- 27.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63(11):1179–94. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cook KF, Dunn W, Griffith JW, Morrison MT, Tanquary J, Sabata D, Victorson D, Carey LM, MacDermid JC, Dudgeon BJ, Gerson RC. Pain assessment using the NIH Toolbox. Neurology. 2013;80(11 Supplement 3):S49–S53. doi: 10.1212/wnl.0b013e3182872e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pavot W, Diener E. Review of the satisfaction with life scale. Psychol Assess. 1993;5(2):164–72. [Google Scholar]
- 31.Sullivan MJ, Bishop SR, Pivik J. The pain catastrophizing scale: development and validation. Psychol Assess. 1995;7(4):524. doi: 10.1037//1040-3590.7.4.524. [DOI] [Google Scholar]
- 32.Osman A, Barrios FX, Gutierrez PM, Kopper BA, Merrifield T, Grittmann L. The Pain Catastrophizing Scale: further psychometric evaluation with adult samples. J Behav Med. 2000;23(4):351–65. doi: 10.1023/a:1005548801037. [DOI] [PubMed] [Google Scholar]
- 33.Van Damme S, Crombez G, Bijttebier P, Goubert L, Van Houdenhove B. A confirmatory factor analysis of the Pain Catastrophizing Scale: invariant factor structure across clinical and non-clinical populations. Pain. 2002;96(3):319–24. doi: 10.1016/s0304-3959(01)00463-8. [DOI] [PubMed] [Google Scholar]
- 34.Rodero B, Luciano JV, Montero-Marin J, Casanueva B, Palacin JC, Gili M, del Hoyo YL, Serrano-Blanco A, Garcia-Campayo J. Perceived injustice in fibromyalgia: psychometric characteristics of the Injustice Experience Questionnaire and relationship with pain catastrophising and pain acceptance. J Psychosom Res. 2012;73(2):86–91. doi: 10.1016/j.jpsychores.2012.05.011. [DOI] [PubMed] [Google Scholar]
- 35.Scott W, Trost Z, Milioto M, Sullivan MJ. Further validation of a measure of injury-related injustice perceptions to identify risk for occupational disability: a prospective study of individuals with whiplash injury. J Occup Rehabil. 2013;23(4):557–65. doi: 10.1007/s10926-013-9417-1. [DOI] [PubMed] [Google Scholar]
- 36.Muthén L, Muthén B. Mplus statistical modeling software (Version 6.12) Los Angeles: Muthén & Muthén; 2011. [Google Scholar]
- 37.Mackinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behav Res. 2004;39(1):99. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83. doi: 10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 40.Sturgeon JA, Darnall BD, Kao MC, Mackey SC. Physical and psychological correlates of fatigue and physical function: A Collaborative Health Outcomes Information Registry (CHOIR) study. J Pain. 2015;16(3):291–8 e1. doi: 10.1016/j.jpain.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Börsbo B, Peolsson M, Gerdle B. Catastrophizing, depression, and pain: correlation with and influence on quality of life and health–a study of chronic whiplash-associated disorders. J Rehabil Med. 2008;40(7):562–9. doi: 10.2340/16501977-0207. [DOI] [PubMed] [Google Scholar]
- 42.Sturgeon JA, Carriere JS, Kao M-CJ, Rico T, Darnall BD, Mackey SC. Social disruption mediates the relationship between perceived injustice and anger in chronic pain: A Collaborative Health Outcomes Information Registry study. Ann Behav Med. 2016:1–11. doi: 10.1007/s12160-016-9808-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fernandez E, Wasan A. The anger of pain sufferers: Attributions to agents and appraisals of wrongdoings. Springer; 2010. pp. 449–64. (International Handbook of Anger). [Google Scholar]
- 44.Scott W, Trost Z, Milioto M, Sullivan MJ. Barriers to change in depressive symptoms after multidisciplinary rehabilitation for whiplash: the role of perceived injustice. Clin J Pain. 2015;31(2):145–51. doi: 10.1097/AJP.0000000000000095. [DOI] [PubMed] [Google Scholar]
- 45.Myers DG. 19 Close Relationships and Quality of Life. Well-being: Foundations of hedonic psychology. 2003:374. [Google Scholar]
- 46.Albrecht GL, Devlieger PJ. The disability paradox: high quality of life against all odds. Soc Sci Med. 1999;48(8):977–88. doi: 10.1016/s0277-9536(98)00411-0. [DOI] [PubMed] [Google Scholar]
- 47.Lynch EB, Butt Z, Heinemann A, Victorson D, Nowinski CJ, Perez L, Cella D. A qualitative study of quality of life after stroke: the importance of social relationships. J Rehabil Med. 2008;40(7):518–23. doi: 10.2340/16501977-0203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Conant LL. Psychological variables associated with pain perceptions among individuals with chronic spinal cord injury pain. J Clin Psychol Med Settings. 1998;5(1):71–90. [Google Scholar]
- 49.Craig A, Tran Y, Siddall P, Wijesuriya N, Lovas J, Bartrop R, Middleton J. Developing a model of associations between chronic pain, depressive mood, chronic fatigue, and self-efficacy in people with spinal cord injury. J Pain. 2013;14(9):911–20. doi: 10.1016/j.jpain.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 50.Summers JD, Rapoff MA, Varghese G, Porter K, Palmer RE. Psychosocial factors in chronic spinal cord injury pain. Pain. 1991;47(2):183–9. doi: 10.1016/0304-3959(91)90203-a. [DOI] [PubMed] [Google Scholar]
- 51.Wollaars MM, Post MW, van Asbeck FW, Brand N. Spinal cord injury pain: The influence of psychologic factors and impact on quality of life. Clin J Pain. 2007;23(5):383–91. doi: 10.1097/AJP.0b013e31804463e5. [DOI] [PubMed] [Google Scholar]
- 52.Lin EH, Katon W, Von Korff M, Tang L, Williams JW, Jr, Kroenke K, Hunkeler E, Harpole L, Hegel M, Arean P, Hoffing M. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290(18):2428–9. doi: 10.1001/jama.290.21.2803-a. [DOI] [PubMed] [Google Scholar]
- 53.Bogduk N, Mercer S. Biomechanics of the cervical spine. I: Normal kinematics. Clin Biomech. 2000;15(9):633–48. doi: 10.1016/s0268-0033(00)00034-6. [DOI] [PubMed] [Google Scholar]


