Abstract
This study aimed to examine the early impact of the Program of Comprehensive Assistance for Family Caregivers (PCAFC) on Veteran health care utilization and costs. A pre-post cohort design including a nonequivalent control group was used to understand how Veterans’ use of Veteran Affairs health care and total health care costs changed in 6-month intervals up to 3 years after PCAFC enrollment. The control group was an inverse probability of treatment weighted sample of Veterans whose caregivers applied for, but were not accepted into, PCAFC. Veterans in PCAFC had similar acute care utilization postenrollment when compared with those in the control group, but significantly greater primary, specialty, and mental health outpatient care use at least 30, and up to 36, months postenrollment. Estimated total health care costs for PCAFC Veterans were $1,500 to $3,400 higher per 6-month interval than for control group Veterans. PCAFC may have increased Veterans’ access to care.
Keywords: informal care, family caregivers, primary care, mental health outpatient care, emergency department, inpatient hospitalization, Veterans health care utilization
Introduction
Wounded Veterans have significant care needs: 1.1 million Veterans who served in the post-9/11 era receive care from a family member or friend in the home (Ramchand et al., 2014). The Caregivers and Veterans Omnibus Health Services Act of 2010 (Public Law: 111–163) enacted legislation that stipulated landmark services for family caregivers of severely injured post-9/11 era Veterans including training, services, and other types of assistance. The Program of Comprehensive Assistance for Family Caregivers (PCAFC) supports caregivers of Veterans from the post-9/11 era who need assistance with Activities of Daily Living (ADLs) or supervision or protection because of the residual effects of their injuries sustained in the line of duty.
Family caregiver support in the United States for non-Veterans has been limited to modest tax credits offered by a few states, moderately funded National Family Caregiver Support Program training and services provided through Area Agencies on Aging (Feinberg, Newman, Feinberg, & Newman, 2006; The Lewin Group, 2016), limited state programs that pay family caregivers, and supports through Medicaid Home and Community-based Waiver funds (Alliance for the Betterment of Citizens with Disabilities, 2016), in which half of states allow patients to pay family caregivers instead of a formally trained provider to meet their care needs (Foster, Dale, & Brown, 2007; LaPlante, Kaye, & Harrington, 2007). In contrast to the programs described above, PCAFC is a substantial, comprehensive program, requiring caregivers to complete a training curriculum and meet other eligibility requirements in order to participate. Participating caregivers, who must be a relative or a coresiding friend, receive a monthly tax-free stipend. Unlike in Medicaid waiver programs that allow patients to pay family caregivers, the stipend is not intended to replace professionally provided formal home health care already being received by the Veteran. Furthermore, the PCAFC stipend is a clinical benefit paid directly to the caregiver, for the purpose of supporting the Veteran’s recovery process. The caregiver decides how to use the stipend. Stipend amounts range between $600 and $2,300 per month and are based on an assessment of the Veteran’s care needs as determined by the Veteran’s health care team at the local Veteran Affairs (VA) medical center. The stipend amount is awarded according to a three-tier system, aligned with an estimated average number of hours of caregiving each week, not to exceed 40 hours. The hourly rate is based on the Bureau of Labor Statistics–adjusted hourly salary of a home health aide in the geographic area where the Veteran resides.
The caregiver training required as part of the application for PCAFC represents the largest, systematic effort to train family caregivers in U.S. history; as of October 2016, more than 35,000 caregivers have taken this training. Caregivers are offered a choice of taking the training online (in English or Spanish) or using a workbook (English or Spanish). The curriculum covers the following topics: caregiver self-care (e.g., nutrition, exercise, stress management), caregiving skills (taking vital signs, infection control, wound care/pressure sores, medication management, pain management), Veteran’s personal care (supporting the Veteran in ADLs and instrumental ADLs and promoting independence, home accessibility, and assistive devices), home safety (falls prevention, emergency preparedness), managing challenging behaviors (associated with posttraumatic stress disorder, traumatic brain injury, depression, suicide, substance abuse), and information on the caregiver as advocate and resources to support both the caregiver and Veteran (including VA programs, benefits, support groups, respite, and legal and financial information).
The PCAFC also provides a menu of other benefits and services: health care insurance coverage for the caregiver through the Civilian Health and Medical Program of the Department of Veteran Affairs if a caregiver has no health insurance; reimbursed travel expenses when attending required training or accompanying the Veteran for treatment, respite care services, mental health services for the caregiver, and continued monitoring of Veteran and caregiver well-being through quarterly assessments (Miller, Kabat, Henius, & Van Houtven, 2015).
Whereas the above services are available only to PCAFC participants, PCAFC and non-PCAFC caregivers in the VA have access to other resources, including the Caregiver Support Line (1-855-260-3274), a caregiver listserv, and an interactive website (www.caregiver.va.gov). PCAFC and non-PCAFC caregivers can also participate in caregiver self-care classes. Self-care class topics include “Managing Stress,” “Problem Solving/Effective Communication,” “Taking Care of Yourself,” and “Utilizing Technology.” Since November 2013, these classes have been taken by nearly 4,000 caregivers. Importantly, non-PCAFC caregivers are eligible for respite care services and mental health services when part of the Veteran’s treatment plan. These resources and services altogether can be thought of as usual care for VA caregivers.
Caregiver support coordinators (CSCs) in each VA medical center (VAMC) serve as the primary local point of contact for all VA caregivers and oversee all aspects of the multistep application process for PCAFC. In addition, CSCs counsel caregivers, lead caregiver support groups, conduct follow-up home visits, and organize caregiver training activities. CSCs are responsible for offering services and trainings to PCAFC and non-PCAFC caregivers.
PCAFC was implemented rapidly across all VAMCs; when the program began accepting applications in May 2011, there was at least one CSC in each of VA’s 152 Medical Centers. By September 30, 2014, the number of CSCs had grown to 240. PCAFC enrollment far exceeded expectations. A recent Government Accountability Office report found that while VA had expected to receive a total of 4,000 applications for PCAFC, more than 37,000 applications were received between May 11, 2011, and September 30, 2014 (Government Accountability Office, 2014). As of September 2015, over 27,000 family caregivers were enrolled in PCAFC and outlays totaled more than $1 billion. Stipend payments to caregivers account for 81% of total program costs; the remaining funds cover program delivery costs, including staff and CSC salaries, caregiving training, and caregiver program benefits and program monitoring.
Expected annual outlays have been higher than expected due to substantial demand. Therefore, the impact of PCAFC is of immediate interest to the Caregiver Support Program (CSP) and stakeholders. More broadly, policy makers and the research community seek to understand how supports for family caregivers, who serve as the backbone of the long-term care system in the United States, affect patient outcomes and service use and what implications family caregiver support has on system-level outcomes, such as health care costs. Understanding whether comprehensive support for family caregivers is an effective means of increasing access to outpatient care and decreasing acute care is the first step in understanding how broader health outcomes could be affected by support for family caregivers. The VA experience can inform other payers and health care systems in the United States such as Medicare and Medicaid administered by the Centers for Medicare and Medicaid Services or states such as California, which has begun pilot efforts to support family caregivers (Newcomer, Kang, & Doty, 2012).
New Contributions
This study is part of a larger effort to examine the effect of the PCAFC on Veteran health service use, Veteran and caregiver well-being, and caregiver perspectives about the use and value of the PCAFC. Articles that address the latter aspects of this evaluation are forthcoming. This study tests the following hypotheses:
Hypothesis 1: Whether PCAFC is associated with reduced Veteran VA and VA-purchased inpatient hospitalizations or emergency department (ED) visits (acute care).
Hypothesis 2: Whether PCAFC is associated with an increased ability to access care that facilitates well-being and higher functioning, such as primary care, outpatient specialty care, and outpatient mental health care (outpatient care).
Hypothesis 3: Whether PCAFC is associated with increased or decreased total Veteran health care costs.
The conceptual model in Figure 1 suggests that PCAFC could affect Veteran health care utilization by influencing the activities that caregivers provide: their clinical care activities (e.g., quality of caregiving), psychological activities (e.g., managing problem behaviors, coping), their support-seeking activities (e.g., obtaining resources for the Veteran), and the quantity of care provided (Van Houtven, Voils, & Weinberger, 2011). Specifically, PCAFC could affect Veteran health care utilization in the following ways: The training received by a Veteran’s caregiver may improve the ability of a caregiver to navigate the VA health care system, seek timely outpatient care for the Veteran, and improve the quality of caregiving at home. Prompt outpatient care and heightened caregiving quality may in turn help Veterans avoid an unnecessary visit to the ED. Similar to the concept of potentially avoidable hospitalizations, if quality of caregiving increases through PCAFC training and support, acute care could go down because of receipt of timely preventive and primary care in the home and clinic (Starfield, Shi, & Macinko, 2005). Similarly, the stipend may allow the caregiver to have the time and resources to accompany the Veteran to outpatient appointments and gain a better understanding of the Veteran’s treatment plan. Considering that PCAFC participation is expected to decrease acute care (Hypothesis 1) and increase outpatient care (Hypothesis 2), it is not clear a priori whether total Veteran health care costs would increase or decrease from PCAFC participation (Hypothesis 3). Even with support for both Hypotheses 1 and 2, PCAFC may increase total Veteran costs if the cost savings in acute care are less than the increases in outpatient care use among participating Veterans.
Figure 1. Conceptual model of caregiver support and Veteran utilization.
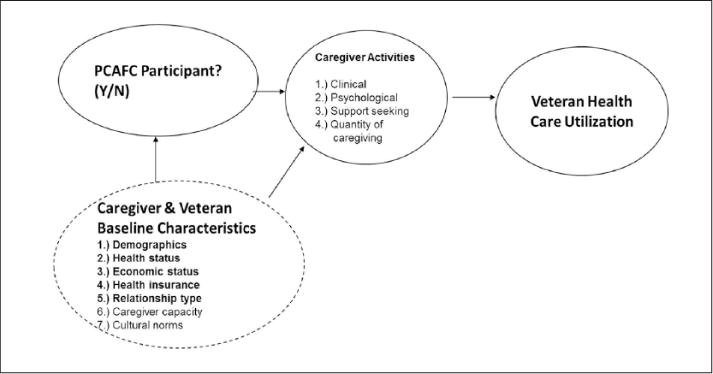
Source. Model adapted from Van Houtven et al. (2011).
Method
Design and Study Population
As the goal of this study was to examine the effect of the PCAFC on Veteran health care utilization and costs, we estimated the average treatment effect among the treated (ATT; Imbens, 2004) using a pre–post two-group retrospective cohort design. The ATT measures the effect of PCAFC on Veteran health care utilization and costs among those Veterans whose caregivers were ever enrolled in the program. Primary interest was in the policy perspective of the decision maker and stakeholders. Therefore, outcomes after enrollment were examined from an intent-to-treat perspective, regardless of whether the dyad remained in the PCAFC or left the program for any reason (e.g., graduated, died, dropped out).
The treatment group consisted of Veterans whose caregivers applied to and were ever approved for participation in PCAFC since its inception (May 2011) through March 31, 2014. Caregivers had to be enrolled in the program for at least 90 consecutive days, to ensure a minimum dose of the intervention. The nonequivalent control group consisted of all Veterans whose caregivers applied to PCAFC by March 31, 2014, and were never approved. Enrollment into the program is determined using a multistep, team-based, clinical approach to assess the Veteran’s needs and the home environment related to the Veteran’s overall level of functioning. As such, enrollment is based on clinical assessments and/or observations made by a trained, multidisciplinary team, which may include social workers, mental health providers, nurses, physicians, and therapists. The two most common reasons for denied entry into the program for our cohort were administrative as opposed to clinical; these reasons included the following: caring for a Veteran injured before 9/11 or caring for Veteran with an illness not related to military service (the law stipulates injury). Veterans and caregivers not approved for the program received standard VA benefits, including case management, and/or home and community-based services if clinically eligible, as well as the services and supports from VA CSP already described as usual care.
The study cohort included 15,836 Veterans in the treatment group and 9,106 Veterans in the control group. Exclusion criteria included (Figure 2): Veterans whose identification number could not be matched to VA data, who were older than 65 years as of September 11, 2011, who were aged 68 years or older on the application date, who died within 90 days of the application date, who had a home zip code outside the 50 states or Puerto Rico at time of application, or who had a missing comorbidity score. Baseline was defined using the application date and represented the end of the preperiod and the beginning of the postperiod in the empirical models described below. For the treatment group, baseline was the application date of the first approved application to PCAFC. For the control group, baseline was the first application date to PCAFC. Figure 3 illustrates the relationship between application date and the number of outcomes intervals for three fictional cases. For example, applying on September 30, 2011, means there can be up to six outcomes intervals (Patient 3a), whereas applying on March 30, 2014, means there can be only one outcome interval (Patient 3c).
Figure 2.
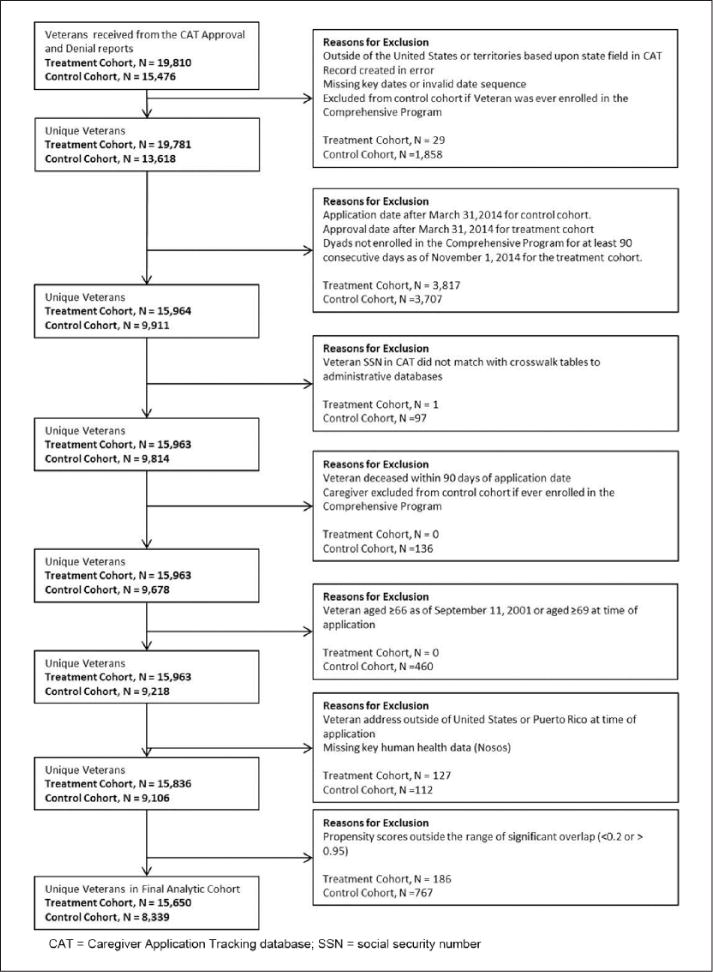
Flowchart of sample exclusions by treatment assignment of the dyad.
Figure 3.
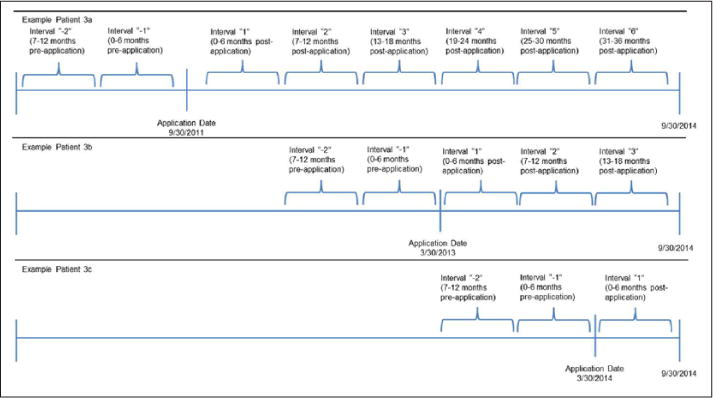
Application date and number of outcome intervals for three example patients.
Data Sources
Application date, program eligibility determination, and caregiver relationship with the Veteran were obtained from the Caregiver Application Tracker, the database used by the VA CSP to record all applications. Outcomes and explanatory variables in the VA electronic health record data were abstracted from the Corporate Data Warehouse, the Assistant Deputy Under Secretary for Health for Policy & Planning Enrollment files, and The Vital Status Mini file. Specifically, utilization outcomes were constructed using the Managerial Cost Accounting (MCA) System National Data Extracts Outpatient, Discharge, Treating Specialty, and Observation Treating Specialty SQL tables, and the Medical SAS® VA-purchased care files (also called Fee Basis) Inpatient and Outpatient files.
The Medical SAS Inpatient Datasets (Acute Care [main], Observation Care [main], non-VA Care [main], Extended Care [main]), Medical SAS Outpatient Event Dataset, and Fee Basis files provided additional information, including clinical information such as diagnosis codes, for creating explanatory variables and for delineating inpatient stays found in the MCA Discharge file into hospitalizations and extended care (e.g., nursing home care). Total health care costs were constructed from the MCA files and Fee Basis files. Date of death was obtained from the Vital Status Mini file, along with other demographic characteristics (e.g., date of birth, gender).
Outcomes
Utilization and total cost of VA services were categorized into 6-month outcome intervals based on the application date to PCAFC. Application dates varied, so the number of outcome intervals differed per Veteran. Each Veteran had at least one 6-month interval postapplication as well as two 6-month intervals prior to application; Veterans who applied at program inception had as many as 6 intervals postapplication, whereas Veterans who applied to the program in March 2014 only had 1 interval postapplication (end date September 30, 2014). Inclusion of utilization in the preapplication period allowed for evaluation of the success to which the propensity score weighting methods balanced observed characteristics of the treated and control groups prior to application.
Acute Care
Acute care included any ED care and any inpatient stay and was measured across VA and VA-purchased care. VA-purchased care is care provided in the community by non-VA providers. ED care was defined as at least one ED encounter, regardless of whether it resulted in an inpatient admission. Inpatient hospitalization was defined as an overnight inpatient stay for any reason, including observation stays. If an inpatient stay crossed two distinct 6-month outcome intervals, each distinct interval was counted.
Outpatient Care
There were four main categories of VA outpatient care examined: (a) total number of VA outpatient clinic visits in a 6-month interval, (b) receipt of any VA primary care visit, (c) receipt of any VA specialty care visit, and (d) receipt of any VA mental health care visit. All outpatient clinic stop codes (“clinic stop codes” classify type of outpatient care in the VA) were included in the count of outpatient clinic visits with a few exceptions that are not considered typical outpatient care, such as clinical pharmacy and home-based primary care. Primary care was defined by having a primary care clinic stop code; home-based primary care, which is often coded as an eligibility visit for PCAFC, and occurs in the home not the clinic, was not included in the definition of primary care. VA specialty outpatient care was defined as a visit to a medical specialty clinic such as neurology service, amputation follow-up, oncology, gastroenterology, hepatology, and many others (for a full list, contact the corresponding author).
VA mental health care was identified by clinic stop codes for mental health, with select outpatient clinic visits also requiring a mental health diagnosis code in the associated record to be considered a mental health visit (McCarthy & Blow, 2004). To examine the role of non-VA providers in VA-purchased mental health care specifically, another composite outpatient mental health measure was created (i.e., any mental health outpatient visits in a VA or a VA-purchased care setting). Mental health outpatient care in a VA-purchased care setting was identified by a mental health diagnosis code appearing in a record. Any VA or VA-purchased mental health use and number of days with any VA or VA-purchased mental health care were both examined.
Total Health Care Costs
A total health care cost measure was created which included all VA-financed Veteran health care; specifically, Veteran inpatient, extended care (e.g., nursing home care), outpatient (including ED and home-based primary care), and pharmacy costs across VA and VA-purchased sites of care (including VA-purchased home health care) were aggregated using procedures recommended by the VA Health Economics Resource Center (Phibbs, Scott, Flores, & Barnett, 2010; Wagner, Chow, & Barnett, 2009). For inpatient claims, an average daily cost based on the treatment dates was calculated. If all of a given claim’s treatment dates were within a 6-month interval, its cost was attributed to that single interval. If the treatment dates for one inpatient stay occurred over multiple 6-month intervals, costs were assigned to the appropriate 6-month interval via average daily costs. Costs were presented in 2014 dollars (Agency for Healthcare Research and Quality, 2016).
Inverse Probability of Treatment Weights
Because Veterans who qualify for PCAFC have a legal right to participate, Veterans could not be randomized to not receive PCAFC. Therefore, systematic differences may have existed between the treatment and control groups at time of application. The group of Veterans who were likely to be most similar to those who received PCAFC services were those whose caregivers applied for, but were not accepted into the program. However, the potential for confounding still exists. To address possible confounding due to such selection bias we applied inverse probability of treatment (IPT) weights that were constructed using propensity scores (Lunceford & Davidian, 2004). IPT weights were chosen over matching on the propensity score due to the relatively small number of Veterans in the control group compared with the number enrolled in PCAFC. Propensity scores—the predicted probably of ever being enrolled in PCAFC—were estimated for each individual using logistic regression. All available variables that were likely associated with Veteran-level health needs that might have driven decisions about program enrollment were included in the propensity scores.
Because interest was in estimation of the ATT, each Veteran in the treatment group received a weight of 1.0, while for each Veteran in the control group, a propensity score was used to create weights to balance explanatory variables between the treatment and control groups. The weights were constructed such that, after applying these weights, a pseudopopulation was created where the distribution of the explanatory variables was independent of whether a caregiver was enrolled in the program. Through this weighting process, Veterans in the control group with characteristics commonly seen in the treatment group but poorly represented in the control group were given proportionately higher weights (Austin, 2011; Rosenbaum, 1987). After applying these weights, covariate balance between the treatment and control groups was evaluated using standardized differences, which are insensitive to sample size. Standardized differences less than 10 indicate reasonable covariate balance (Austin, 2009). To ensure that the treatment and control groups have similar ranges of propensity scores for comparison (Stuart, 2010), Veterans with propensity scores lower than 0.2 or greater than 0.95 were trimmed from the analytic sample. This excluded 186 treated and 767 control group Veterans, creating a final analytic sample of 15,650 treatment group and 8,339 control group Veterans.
Importantly, because caregivers applied from the program’s inception from May 2011 to March 31, 2014, outcomes data were available for the full cohort in the 1- to 6-month outcome interval, but the available years of follow-up decreased for those who applied later in the study period (Table 1). For example, 19,553 Veterans (13,966 in treatment, 5,587 in control group) had 12 months of follow-up and only 2,381 Veterans (2,056 in treatment and 325 in control group) had a full 3 years of follow-up. Except for death, there was no loss to follow-up otherwise. This study was designed to detect early impacts of PCAFC on Veteran health care utilization and costs.
Table 1.
Duration of Follow-Up by Treatment Arm.
| Postapplication time interval |
Application date to PCAFC |
Overall
|
Treatment
|
Control
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N |
N (%) Deceased |
N Censoreda |
N |
N (%) Deceased |
N Censoreda |
N |
N (%) Deceased |
N Censoreda |
||
| 0–6 Months | 5/2011–3/2014 | 23,989 | 44 (0.2) | 4,392 | 15,650 | 13 (0.1) | 1,671 | 8,339 | 31 (0.4) | 2,721 |
| 7–12 Months | 5/2011–9/2013 | 19,553 | 74 (0.4) | 5,824 | 13,966 | 44 (0.3) | 3,452 | 5,587 | 30 (0.5) | 2,372 |
| 13–18 Months | 5/2011–3/2013 | 13,655 | 48 (0.4) | 4,497 | 10,470 | 29 (0.3) | 2,970 | 3,185 | 19 (0.6) | 1,527 |
| 19–24 Months | 5/2011–9/2012 | 9,110 | 34 (0.4) | 3,955 | 7,471 | 28 (0.4) | 3,014 | 1,639 | 6 (0.4) | 941 |
| 25–30 Months | 5/2011–3/2012 | 5,121 | 19 (0.4) | 2,721 | 4,429 | 17 (0.4) | 2,356 | 692 | 2 (0.3) | 365 |
| 31–36 Months | 5/2011–9/2011 | 2,381 | 4 (0.2) | 2,056 | 1 (0.0) | 325 | 3 (0.9) | |||
Note. PCAFC = Program of Comprehensive Assistance for Family Caregivers.
Number of nondeceased Veterans censored at end of time interval.
Explanatory Variables in the Logistic Propensity Score Model
Baseline explanatory variables were used to control for sociodemographics, access to care factors and comorbidities that may have affected both acceptance into PCAFC as well as Veteran health care utilization (Table 2). Variables chosen were carefully selected for the propensity score model as all those believed to be potential confounders on which we could obtain data (Brookhart et al., 2006; VanderWeele & Shpitser, 2011). Veteran age, gender, race, and relationship to the caregiver were included as well as service connection and distance to VA care. Comorbidities common in post-9/11 combat Veterans included posttraumatic stress disorder, traumatic brain injury, musculoskeletal conditions, and others, based on literature (Stroupe, Smith, Hogan, & St Andre, 2013). Veteran enrollment priority, means test status, preapplication rates of primary and mental health care utilization, as well as the Nosos comorbidity score, were included. Akin to a Diagnostic Cost Group score (Ash et al., 2000), Nosos reflects expected use based on past diagnoses, inpatient care, outpatient care, pharmacy utilization, and demographics (Wagner et al., 2016). Facility-level characteristics of Veterans Integrated Service Network and complexity level of the VAMC closest to the Veteran’s home address at time of application were also included to control for local facility and regional market-level factors at baseline. Propensity score specification was carefully tested, with the need for higher order terms or interactions assessed by visual inspection of the estimated distributions of propensity scores and the level of balance achieved via standardized differences.
Table 2.
Baseline Descriptive Characteristics of Unweighted and Weighted VA Caregiver Support Program Treatment Group and Control Group Veterans (%).
| Baseline characteristics | Unweighted cohorta
|
Inverse probability of treatment weighted cohort |
||||
|---|---|---|---|---|---|---|
| Control group |
Treatment group |
Std. diff.b | Control group |
Treatment group |
Std. diff.b | |
| Gender, % | ||||||
| Female | 10.9 | 7.6 | −11.5 | 7.8 | 7.6 | −0.7 |
| Age, M (SD) | 38.6 (10.3) | 36.2 (8.9) | −25.1 | 35.8 (11.7) | 36.2 (8.9) | 3.6 |
| Homelessc, % | 6.6 | 6.1 | −2.3 | 6.4 | 6.1 | −1.4 |
| Marital status, % | ||||||
| Married | 66.2 | 68.8 | 5.5 | 68.4 | 68.8 | 0.9 |
| Never married/single/widowed | 17.0 | 18.1 | 3.0 | 18.4 | 18.1 | −0.8 |
| Divorced/separated | 12.9 | 11.2 | −5.4 | 11.5 | 11.2 | −1.0 |
| Unknown | 3.9 | 1.9 | −12.3 | 1.7 | 1.9 | 1.5 |
| Race, % | ||||||
| White | 58.5 | 69.2 | 22.8 | 71.0 | 69.2 | −3.8 |
| Black | 29.1 | 18.3 | −26.4 | 17.1 | 18.3 | 3.0 |
| Other | 5.8 | 6.8 | 4.1 | 6.6 | 6.8 | 0.7 |
| Unknown | 6.6 | 5.7 | −3.9 | 5.2 | 5.7 | 1.9 |
| Ethnicity, % | ||||||
| Non-Hispanic/Latino(a) | 86.0 | 83.0 | −8.3 | 83.0 | 83.0 | −0.1 |
| Hispanic/Latino(a) | 10.0 | 13.6 | 11.1 | 13.3 | 13.6 | 0.7 |
| Unknown | 4.0 | 3.5 | −3.1 | 3.7 | 3.5 | −1.2 |
| Service connected, % | ||||||
| High (≥70%) | 64.0 | 72.3 | 18.2 | 72.2 | 72.3 | 0.3 |
| Medium high (50%–69%) | 14.8 | 11.9 | −8.7 | 11.5 | 11.9 | 1.1 |
| Medium low (10%–49%) | 8.3 | 5.5 | −11.4 | 5.6 | 5.5 | −0.3 |
| Low (<10%) or missing | 12.9 | 10.3 | −8.3 | 10.7 | 10.3 | −1.4 |
| Means test status, % | ||||||
| Copay required | 12.1 | 11.4 | −2.1 | 11.8 | 11.4 | −1.1 |
| Copay not required | 65.0 | 69.2 | 8.9 | 70.1 | 69.2 | −1.8 |
| Unknown | 22.8 | 19.3 | −8.7 | 18.1 | 19.3 | 3.1 |
| Enrollment priority group, % | ||||||
| Group 1 | 79.8 | 85.1 | 14.2 | 84.7 | 85.1 | 1.0 |
| Groups 2–4 | 11.4 | 9.0 | −8.0 | 9.2 | 9.0 | −0.7 |
| Groups 5–8 or missing | 8.8 | 5.9 | −11.4 | 6.1 | 5.9 | −0.7 |
| Non-VA insurance, % | 10.5 | 15.2 | 13.6 | 16.0 | 15.2 | −2.3 |
| Number of mental health visitsd, M (SD) | 4.2 (8.4) | 5.5 (9.5) | 14.6 | 5.7 (13.6) | 5.5 (9.5) | −1.7 |
| Number of VA primary care clinic stopsd, M (SD) | 1.3 (1.6) | 1.6 (1.7) | 12.8 | 1.6 (2.4) | 1.6 (1.7) | −0.6 |
| Nosos score, M (SD) | 1.2 (1.7) | 1.5 (2.0) | 13.1 | 1.5 (2.8) | 1.5 (2.0) | −2.4 |
| Diagnoses, % | ||||||
| Physical comorbidities | ||||||
| Musculoskeletal disorders/diseases | 58.9 | 64.8 | 12.3 | 64.8 | 64.8 | 0.03 |
| Pain, not including back or joint | 39.8 | 47.7 | 15.9 | 48.4 | 47.7 | −1.4 |
| Joint pain, not including back | 35.7 | 39.9 | 8.7 | 39.3 | 39.9 | 1.1 |
| Hyperlipidemia | 28.0 | 28.1 | 0.3 | 27.2 | 28.1 | 2.0 |
| Hypertension | 26.3 | 24.4 | −4.5 | 23.6 | 24.4 | 1.8 |
| TBI | 18.9 | 32.5 | 30.7 | 33.8 | 32.5 | −2.7 |
| Obesity | 17.6 | 19.1 | 3.8 | 19.5 | 19.1 | −1.0 |
| Headache | 15.1 | 20.1 | 13.1 | 19.9 | 20.1 | 0.7 |
| Hearing: loss, pain, other | 14.6 | 18.5 | 10.4 | 18.8 | 18.5 | −0.8 |
| Diabetes | 10.3 | 7.9 | −8.6 | 7.1 | 7.9 | 2.8 |
| Neoplasm | 7.5 | 7.1 | −1.5 | 7.1 | 7.1 | −0.1 |
| Chest pain/acute myocardial infarction | 6.9 | 7.2 | 1.2 | 7.0 | 7.2 | 0.9 |
| Mental health comorbidities, % | ||||||
| PTSD | 60.2 | 73.7 | 29.4 | 74.2 | 73.7 | −1.1 |
| Depression | 45.7 | 52.1 | 12.7 | 53.3 | 52.1 | −2.3 |
| Anxiety | 24.1 | 25.9 | 4.2 | 26.7 | 25.9 | −1.8 |
| Tobacco use | 19.7 | 22.9 | 7.7 | 23.1 | 22.9 | −0.4 |
| Alcohol or substance abuse | 19.2 | 20.9 | 4.2 | 22.3 | 20.9 | −3.4 |
| Other mental health | 14.1 | 17.3 | 8.6 | 18.3 | 17.3 | −2.8 |
| Adjustment reaction | 9.8 | 10.2 | 1.3 | 9.8 | 10.2 | 1.2 |
| Bipolar disorder | 9.2 | 10.9 | 5.5 | 11.3 | 10.9 | −1.2 |
| Miles to closest VAMCe, M (SD) | 39.9 (33.0) | 38.8 (35.4) | −3.2 | 39.6 (48.2) | 38.8 (35.4) | −1.9 |
| Caregiver’s relationship to Veteran, % | ||||||
| Spouse/partner | 77.5 | 81.8 | 10.8 | 80.9 | 81.8 | 2.3 |
| Mother or father | 7.8 | 8.9 | 3.9 | 9.7 | 8.9 | −2.9 |
| Other relative | 6.9 | 5.1 | −7.7 | 5.1 | 5.1 | −0.1 |
| Other nonrelative/not available | 7.8 | 4.2 | −15.7 | 4.3 | 4.2 | −0.2 |
| Caregiver is a Veteran, % | 11.3 | 11.8 | 1.3 | 10.7 | 11.8 | 3.4 |
Note. Control group = Veterans of caregivers who applied to but were denied entry into PCAFC; treatment group = Veterans of caregivers approved into PCAFC; Std. diff. = standardized difference; VA = Veteran Affairs; TBI = traumatic brain injury; PTSD = posttraumatic stress disorder; VAMC = Veterans Affairs Medical Center. Percentages in table may not add to 100% due to rounding. Veterans Integrated Service Network indicator variables (1–21) and complexity of the medical facility (1a, 1b, 1c, 2, 3) also assessed (not shown; Veterans Health Administration, 2012).
Analytic cohort: N = 8,339 and N = 15,650 Veterans in the control and treatment groups, respectively.
Assessed in the year prior to and including application date.
Number of visits in the 6 months prior to and including application date.
Closest VAMC or Independent Outpatient Clinic at time of application, based on distance from Veteran’s zip code.
Statistical Analysis
The impact of PCAFC enrollment on Veterans was evaluated on eight different utilization outcomes and total health care costs in the weighted cohorts. Generalized linear models (GLMs) fit via generalized estimating equations (GEEs) were employed with a logit link for dichotomous outcomes. For count outcomes, GLMs were fit with GEEs using a log link with an assumption that the variance was proportional to the mean. Additionally, for count outcomes, an offset was included for the number of days the Veteran was “at risk” for having this utilization in each 6-month interval. For example, if a deceased Veteran contributed days “at risk” for a partial interval, only days alive were considered “at risk.” For cost, model specification was thoroughly tested as recommended by Manning and Mullahy (2001). The program impact on costs was estimated via a GLM fit with GEEs using the optimal specification based on fit tests, a square root link with an assumption that the variance was proportional to the mean. To account for overdispersion seen in the data, empirical sandwich standard errors were employed for all utilization outcomes and for mean cost estimates; these standard errors are robust to variance misspecification in large sample sizes (Kauermann & Carroll, 2001; Royall, 1986). Confidence intervals for differences in mean costs were bootstrapped using 1,000 samples.
To allow for nonlinear trends over time, each time interval was dummy coded and interactions with an indicator of enrollment in PCAFC were included at all time points. Specifically, the model estimated was as follows:
where μij is the mean outcome for individual i at time j, g(·) is the link function, t−1 to t6 represent 0 to 6 months prior to application to 31 to 36 months postapplication, respectively, with 7 to 12 months prior to application serving as the reference level, and TRTi is an indicator of whether individual i was enrolled in the PCAFC.
All analyses were planned a priori with a statistical significance level set at a 0.05 level and conducted in SAS 9.4 and SAS Enterprise Guide 7.1 (SAS Institute Inc, Cary, NC). As a VA quality improvement project, this work was not subject to institutional review board approval.
Results
Descriptive Results
Table 2 displays the characteristics of the unweighted and weighted samples classified by Veteran treatment or control group status (e.g., enrolled or not). The columns labeled “Unweighted” present the baseline characteristics of treated (n = 15,650) and control (n = 8,339) Veterans. The large (>10) standardized differences observed in the unweighted cohort demonstrate that Veterans who were enrolled were different from Veterans who were not. In the unweighted cohort, treatment group Veterans were a lower proportion female (7.6% vs. 10.9%) and were on average 2.4 years younger than control group Veterans. A higher proportion of Veterans in the treatment group were White race and Hispanic/Latino ethnicity, while a higher proportion in the control group were Black race. After applying IPT weighting, balance between treatment and control groups was achieved as evidenced by small standardized differences <10 (Austin, 2009).
Impact of PCAFC on Veteran Utilization and Cost
Acute Care
Enrollment in PCAFC was not associated with Veteran ED use across VA and VA-purchased care in any time period following the application date (Figure 4). There was a decrease in the proportion of Veterans having any ED visit over time for both the treatment and control groups, with an estimated 25% of Veterans having an ED visit in the first 6-month interval, and falling to approximately 20% at 25 to 30 months postapplication date. Similarly, PCAFC was not associated with having an inpatient hospitalization at any time period after the application date. In the first 6 months after the application date, an estimated 9% to 10% of Veterans in both treatment and control groups had an inpatient hospitalization; 31 to 36 months after the application date, the estimated proportion was 7% to 10% (Figure 4).
Figure 4. Any emergency department and any hospitalization.
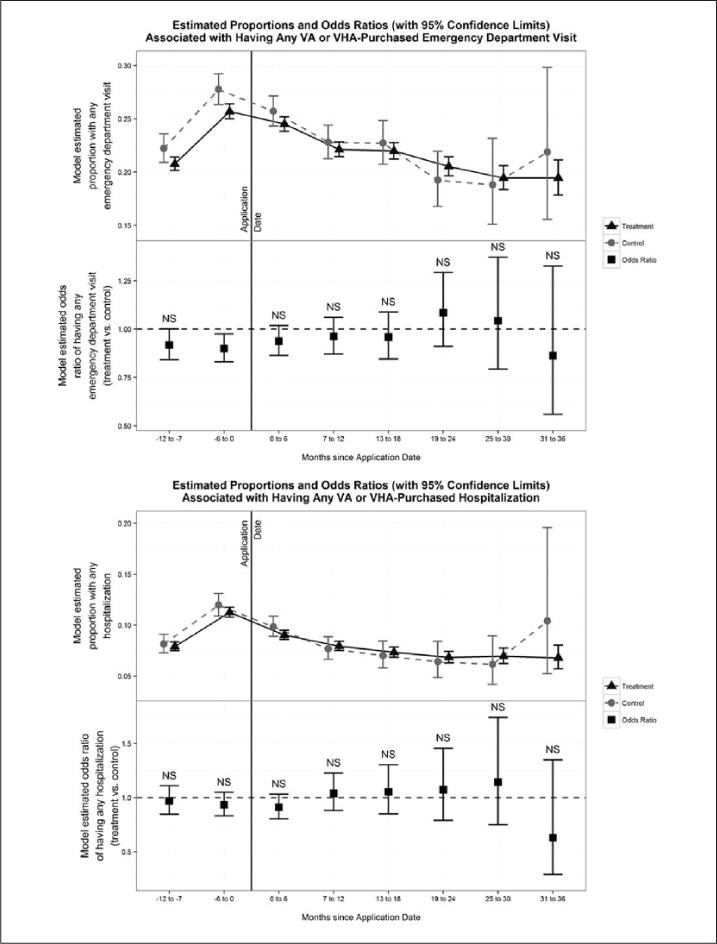
Note. The top panel of each figure represents the model-estimated proportion in each group (treatment and control) receiving any of the specified type of care at each 6-month interval, with 95% confidence intervals at each time point. The bottom panel of the figures represents the model-estimated odds ratios, comparing the odds of someone in the treatment group receiving that type of care compared with a similar individual in the control group. An odds ratio of 1.0 indicates no difference between groups; 95% confidence intervals are provided at each time point, and periods without statistically significant differences are denoted with “NS.”
Outpatient Care
PCAFC was associated with increased use of VA outpatient care across all categories following application: total VA outpatient care visits, receipt of any VA primary, receipt of any VA specialty, and receipt of any VA mental health care (Figure 5). First, the quantity of total VA outpatient visits was estimated to be statistically significantly different across groups. Veterans in the treatment group had on average 6.6 more outpatient visits in the first 6 months postapplication, 6.1 more in the 7 to 12 months postapplication, and 4 to 6 more outpatient visits per 6-month period in the subsequent 2 years (Figure 5, top left). Second, 0 to 6 months after application, an estimated 85% of treatment group Veterans accessed VA primary care compared with 73% of control group Veterans (Figure 5, top right). In the second time interval, 7 to 12 months after the application date, the estimated probability of receiving any VA primary care fell for both treatment and control group Veterans, yet remained higher for treated Veterans (75% and 63% for treated and control Veterans, respectively). Over time, treated Veterans had about a 10 percentage point higher probability of receiving any VA primary care compared with control group Veterans. Third, PCAFC also was associated with an increased probability of using any VA specialty care, with a 75% estimated probability for treated Veterans compared with a 64% estimated probability for control group Veterans in the first 6 months after the application date (Figure 5, bottom left). By 31 to 36 months, the difference was not statistically significant.
Figure 5. VA outpatient, primary care, specialty care, and mental health care.
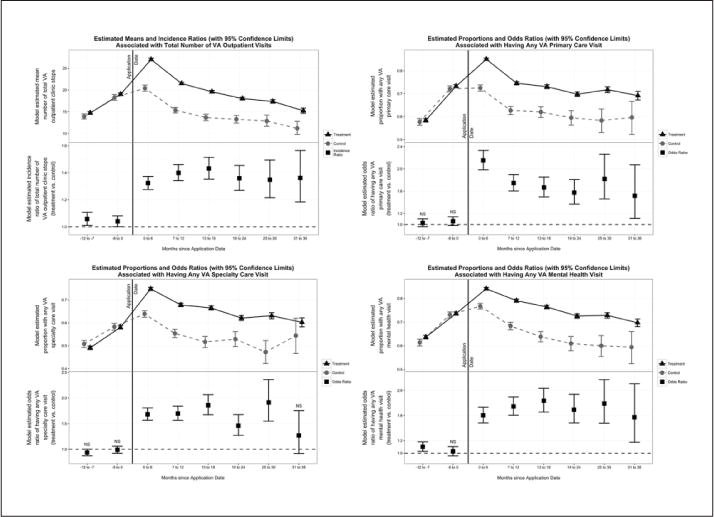
Note. VA = Veteran Affairs. The top panel of the top left figure represents the model-estimated mean visit count in each group (treatment and control) at each 6-month interval, with 95% confidence intervals at each time point. The bottom panel of the figures represents the model-estimated incidence density ratio, or rate ratio, comparing the mean number of visits of someone in the treatment group receiving that type of care compared with a similar individual in the control group. An incidence density ratio of 1.0 indicates no difference between groups; 95% confidence intervals are provided at each time point, and periods without statistically significant differences are denoted with “NS.” All other figures can be interpreted as those in Figure 4.
Finally, PCAFC was also associated with increased use of VA mental health care, with treatment group Veterans having an 84% estimated probability of any mental health visit in the 6 months after the application date, compared with a 77% estimated probability for control group Veterans. This probability dropped to 79% in the 7 to 12 months after the application date for treated Veterans, but a statistically significant difference of 10.7 percentage points remained. In the subsequent 2 years, statistically significant differences of an estimated 10 to 13 percentage points remained between groups (Figure 5, bottom right). The same pattern applied to VA-purchased mental health care and VA mental health care. Treatment group Veterans had an estimated 85% probability of any mental health visit in the first 6 months after the application date, compared with an approximately 77% probability for Veterans in the control group (Figure 6, top). Treatment group Veterans had a higher number of days with VA and VA-purchased mental health visits as well, with on average 1 more day of mental health care in each 6-month time interval, from 0 to 6 months through 25 to 30 months. There was no significant difference in number of total VA + VA-purchased days with mental health care at 31 to 36 months (Figure 6, bottom).
Figure 6. VA or VHA-purchased mental health care.
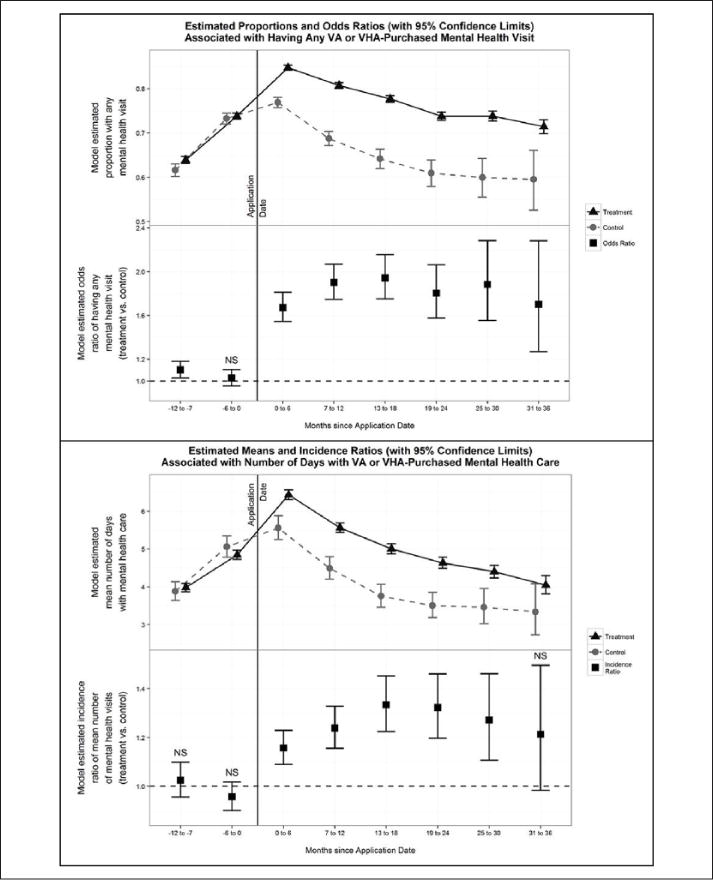
Note. VA = Veteran Affairs. To interpret the top half of the figure: The top panel of the figure represents the model-estimated proportion in each group (treatment and control) receiving any VA or VA-purchased mental health care at each 6-month interval, with 95% confidence intervals at each time point. The bottom panel of the top half represents the model-estimated odds ratios, comparing the odds of someone in the treatment group receiving such care compared with a similar individual in the control group. To interpret the bottom half of the figure: The top panel of the bottom figure represents the model-estimated mean visit count in each group (treatment and control) at each 6-month interval, with 95% confidence intervals at each time point. The bottom panel of the bottom figure represents the model-estimated incidence density ratio, or rate ratio, comparing the mean number of visits of someone in the treatment group receiving VA or Veterans Health Administration–purchased mental health care compared with a similar individual in the control group.
Total Health Care Costs
Enrollment in PCAFC was associated with higher estimated total VA and VA-purchased health care costs in all 6-month intervals after the application date (Figure 7). The estimated total cost for treated Veterans was $13,026 in the first 0 to 6 months compared with $10,773 for control group Veterans. Total VA costs fell over time for both groups, but they remained significantly higher for treated Veterans compared with control group Veterans. For example, at 19 to 24 months following the application date, total VA and VA-purchased health care costs were estimated to be $9,541 versus $7,857 for treated and control Veterans, respectively.
Figure 7. Total VA health care costs (VA and VHA-purchased care).
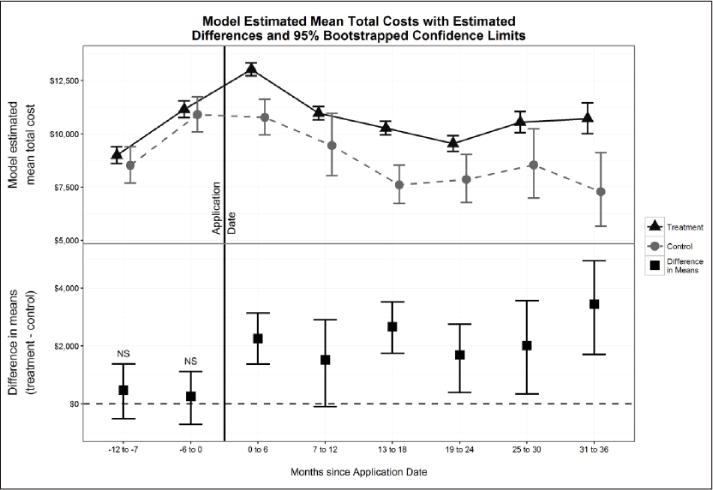
Note. VA = Veteran Affairs. The top panel of the figure represents the model-estimated mean total VA health care costs in each group (treatment and control) at each 6-month interval, with 95% confidence intervals at each time point. The bottom panel of the figure represents the model-estimated difference in mean total VA health care costs (treatment-control). A difference of 0 indicates no difference between the groups; 95% Bootstrapped confidence intervals are provided at each time point, and periods without statistically significant differences are denoted with “NS.” All dollars expressed in 2014 dollars using the GDP deflator.
Conclusion
Results show there was no significant difference between Veterans in the treatment and control groups with regard to utilization of acute care—ED or hospital inpatient care (Hypothesis 1). However, we find support for an association between caregiver enrollment in PCAFC and increased Veteran utilization of primary care, mental health care, and specialty care (Hypothesis 2). VA and VA-purchased total health care costs were also higher for Veterans of enrolled caregivers compared with Veterans of non-enrolled caregivers receiving usual care (Hypothesis 3), suggesting that PCAFC may have increased Veterans’ access to care in the short term.
Increasing access to care for Veterans is a priority of the Department of Veterans Affairs, as detailed in its Blueprint for Excellence (Veterans Health Administration, 2014). The increased outpatient health care utilization by Veterans with caregivers in the program requires further study to understand its drivers. Possible explanations for increased outpatient care include the following: (a) training and support offered by the program may increase caregiver confidence in navigating the VA health care system, including improved communication with the health care team, or increase the caregiver’s ability to recognize treatment needs; (b) the stipend may directly free the caregiver from the need to be employed or assist with the cost of child care, thus enabling the caregiver to make and accompany the Veteran to appointments; (c) caregiver access to health insurance could allow the caregiver to address her or his own physical and mental health care needs, and, being in better health, the caregiver may have more time and energy to help the Veteran access his or her care; and (d) quarterly assessment visits required over time by the program to monitor the well-being of the Veteran and caregiver may have led to increased outpatient visits or referrals for additional outpatient care.
An alternative explanation for the increased outpatient utilization observed among treatment group Veterans may be that, despite IPT weighting to control for confounding, Veterans of enrolled caregivers were sicker than Veterans of caregivers not enrolled and therefore used more outpatient services. Relative balance in utilization prior to application suggests such differences were likely not present at baseline. However, without further contextual information, these competing explanations—increased access versus unobserved indicators of increased need—remain untestable.
Several additional potential limitations must be acknowledged. First, the analysis is most robust in the 6-month and 1-year intervals postapplication date due to having outcomes on nearly all applicants up to 1 year, so they are truly informing the short-term impacts of the program. There are fewer outcome intervals (i.e., not the full 36 months) available for applicants who applied to the program later in the study time frame. Therefore, later periods following the application date could reflect changes in sample characteristics from the full cohort of treated Veterans to the early entry Veterans. Second, careful thought went into identifying commonly used codes for program-required home visits and health care use with these codes was systematically eliminated (specifically, home-based primary care). However, due to lack of standardized use of unique codes for program-required visits, study outcomes might include program-related care, which would lead to overstating the estimated increase in outpatient use. The average estimated difference between treatment and control groups ranged from 4.0 to 6.6 outpatient clinic visits across all 6-month outcome intervals. By contrast, two program-related visits are required in a 6-month period, so the estimated difference is unlikely to be fully attributed to program-driven care. Third, this study did not assess organizational features of program implementation (measures of readiness, model fidelity) by focusing on population impacts using health care claims. Fourth, we are able to inform impact on health care–specific costs but we do not consider costs of delivering the PCAFC program, such as the outlays on the stipend, health insurance, and staff. Such inclusion would be needed for a full cost-effectiveness analysis of the PCAFC, as well as broader consideration of “health effects” beyond health care impacts on Veterans.
Finally, and fifth, a nonequivalent control group of Veterans whose caregivers applied to, but were not accepted into PCAFC was used. A propensity score approach was utilized to address nonrandom selection across treatment and control groups based only on observed differences across groups. The use of propensity score weights led to excellent balance across groups on observed covariates; however, even though we controlled for site-level, individual access, and health characteristics, there may be unobserved differences that remain after propensity score weighting, such that residual confounding in the estimated average treatment effects ATT remains. Instrumental variable estimation to control for unobserved confounding was considered, but with no theoretically valid instrument (e.g., “distance to a VAMC” predicts treatment and utilization outcomes), propensity score methods were the most rigorous approach. The relative balance in utilization prior to application suggests such unobserved differences were likely not present at baseline, ameliorating concerns that unobserved differences were affecting the outcome (Brooks & Ohsfeldt, 2013). Nevertheless, as is true in all quasiexperimental studies, it is untestable whether estimated associations, such as Veteran outpatient utilization, were caused by PCAFC or associated with PCAFC due to such external factors affecting both outcomes and selection into PCAFC.
It is also important to acknowledge that even though PCAFC was initiated as a clinical intervention to actively support caregivers in order to help Veterans in their recovery process, there are countervailing incentives associated with PCAFC that may motivate individuals to remain in the program. Specifically, the most economically vulnerable families may want to remain in the program regardless of the caregiving they provide and regardless of Veteran recovery because of the stipend component. These incentives may also affect utilization patterns by influencing the Veteran/caregiver’s degree of engagement with the health care system. This analysis does not address these countervailing incentives, as we took the policy perspective of decision makers to understand the impact of enrollment for at least 90 days on utilization and costs. Therefore, we purposefully do not account for time in the program or utilization by whether a Veteran graduates or remains in the program (or whether other factors changed, such as a change in caregiver, a change in living situation, etc.). These types of inquiries could be answered in the future when the program has had time to mature and more Veterans and caregivers have graduated. Examination of longer term outcomes in the future also could provide a better picture of the return on investment to the VA and on Veteran health outcomes, as the short-term return on investment shows increased use of outpatient care and higher Veteran health care costs. We also do not consider health care services utilization outside of the VA health care system, which could differ across treated and control group Veterans (e.g., Medicaid, private pay services). Future research that takes a broader societal perspective rather than the VA perspective, could inform the full picture of program impacts on health care utilization.
This analysis is part of a larger examination of the PCAFC’s impact on caregiver outcomes and how caregivers use and value PCAFC services. The analysis presented here uses rigorous comparative effectiveness methods to provide the first evidence in the United States of how a comprehensive program of support for family caregivers of Veterans targeted directly to the caregiver affects an important process outcome measure of the care recipient—health care utilization. Given current policy traction to formally support family caregivers, these findings are relevant beyond the VA to other health care systems in the United States. Our findings suggest that comprehensive supports for family caregivers can increase patient engagement in outpatient care in the short term, which may enhance long-term health outcomes of vulnerable patients. Proposals to expand paid family leave for workers who have family caregiving duties could increase caregiver activities and have real consequences for care recipient outcomes if they also enhance care recipient engagement in outpatient care. Additionally, the PCAFC includes tenets of consumer-directed care that have been expanding in United States and VA in the past decade, but with a twist that has not been seen in the U.S. context: Payments go directly to family caregivers with no expectation that these payments replace formal care use. Thus, this study contributes knowledge about whether a consumer-directed approach to enhance quality of life reduces costs in the short term (Buntin et al., 2006). Finally, although examination of this and other proposed programs would need a tailored comparative effectiveness design based on its characteristics, the rigorous methods used in the PCAFC evaluation presented here, specifically carefully constructing the best available control group and how to minimize selection bias, could be useful to guide future assessment efforts.
Acknowledgments
We thank Merritt Schnell for programming support, Ted Berkowitz for graphical design, attendees at AcademyHealth Annual Research Meeting (2016), the International Long-Term Care Policy Network Conference attendees (2016), and Josephine Jacobs for helpful comments. The contents of this report are solely the responsibility of the authors and do not necessarily represent the official views of the Department of Veterans Affairs. We would like to thank two anonymous reviewers for helpful comments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project is funded by the Department of Veterans Affairs, CSP, and Quality Enhancement Research Initiative (PEC 14-272); support was also received from the Center of Innovation for Health Services Research in Primary Care (CIN 13-410) and Geriatrics Research Education and Clinical Center. Megan Shepherd-Banigan is supported by a VA OAA HSR&D PhD Fellowship TPP 21-027.
Footnotes
Reprints and permissions: sagepub.com/journalsPermissions.nav
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Agency for Healthcare Research and Quality. Using appropriate price indices for analyses of health care expenditures or income across multiple years. 2016 Retrieved from https://meps.ahrq.gov/about_meps/Price_Index.shtml.
- Alliance for the Betterment of Citizens with Disabilities. Supporting family caregiving via the federal waiver. 2016 Retrieved from http://www.abcdnj.org/publications/community-based-services/supporting-family-caregiving-via-the-federal-waiver/
- Ash AS, Ellis RP, Pope GC, Ayanian JZ, Bates DW, Burstin H, Yu W. Using diagnoses to describe populations and predict costs. Health Care Financing Review. 2000;21(3):7–28. [PMC free article] [PubMed] [Google Scholar]
- Austin P. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Statistics in Medicine. 2009;28:3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin P. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Sturmer T. Variable selection for propensity score models. American Journal of Epidemiology. 2006;163:1149–1156. doi: 10.1093/aje/kwj149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks JM, Ohsfeldt RL. Squeezing the balloon: Propensity scores and unmeasured covariate balance. Health Services Research. 2013;48:1487–1507. doi: 10.1111/1475-6773.12020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buntin MB, Damberg C, Haviland A, Kapur K, Lurie N, McDevitt R, Marquis MS. Consumer-directed health care: Early evidence about effects on cost and quality. Health Affairs (Millwood) 2006;25:w516–w530. doi: 10.1377/hlthaff.25.w516. [DOI] [PubMed] [Google Scholar]
- Feinberg LF, Newman SL, Feinberg LF, Newman SL. Preliminary experiences of the states in implementing the National Family Caregiver Support Program: A 50-state study. Journal of Aging & Social Policy. 2006;18:95–113. doi: 10.1300/J031v18n03_07. [DOI] [PubMed] [Google Scholar]
- Foster L, Dale SB, Brown R. How caregivers and workers fared in Cash and Counseling. Health Services Research. 2007;42:510–532. doi: 10.1111/j.1475-6773.2006.00672.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government Accountability Office. VA health care: Actions needed to address higher-than-expected demand for the family caregiver program. Washington, DC: Author; 2014. [Google Scholar]
- Imbens G. Nonparametric estimation of average treatment effects under exogeneity: A review. The Review of Economics and Statistics. 2004;86:4–29. [Google Scholar]
- Kauermann G, Carroll R. A note on the efficiency of sandwich covariance matrix estimation. Journal of the American Statistical Association. 2001;96:1387–1396. [Google Scholar]
- LaPlante MP, Kaye HS, Harrington C. Estimating the expense of a mandatory home-and community-based personal assistance services benefit under Medicaid. Journal of Aging & Social Policy. 2007;19:47–64. doi: 10.1300/J031v19n03_04. [DOI] [PubMed] [Google Scholar]
- The Lewin Group. Process evaluation of the older Americans Act Title III-E National Family Caregiver Support Program: Final report. 2016 Retrieved from https://aoa.acl.gov/Program_Results/docs/NFCSP_Final_Report-update.pdf.
- Lunceford J, Davidian M. Stratification and weighting via the propensity score in estimation of causal treatment effects: A comparative study. Statistics in Medicine. 2004;23:2937–2960. doi: 10.1002/sim.1903. [DOI] [PubMed] [Google Scholar]
- Manning WG, Mullahy J. Estimating log models: To transform or not to transform? Journal of Health Economics. 2001;20:461–494. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- McCarthy JF, Blow FC. Older patients with serious mental illness: Sensitivity to distance barriers for outpatient care. Medical Care. 2004;42:1073–1080. doi: 10.1097/00005650-200411000-00006. [DOI] [PubMed] [Google Scholar]
- Miller K, Kabat M, Henius J, Van Houtven C. Engaging, supporting, and sustaining the invisible partners in care: Young caregivers of veterans from the post-9/11 era. North Carolina Medical Journal. 2015;76:320–322. doi: 10.18043/ncm.76.5.320. [DOI] [PubMed] [Google Scholar]
- Newcomer RJ, Kang T, Doty P. Allowing spouses to be paid personal care providers: Spouse availability and effects on Medicaid-funded service use and expenditures. The Gerontologist. 2012;52:517–530. doi: 10.1093/geront/gnr102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phibbs C, Scott J, Flores N, Barnett P. HERC’s outpatient average cost data-set for VA care: Fiscal year 2009 update. Palo Alto, VA: Health Economics Resource Center; 2010. [Google Scholar]
- Ramchand R, Tanielian T, Fisher M, Vaughan C, Trail T, Batka C, Ghosh-Dastida B. Hidden heroes: America’s military caregivers. Santa Monica, CA: RAND; 2014. [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum P. Model-based direct adjustment. Journal of the American Statistician. 1987;82:387–394. [Google Scholar]
- Royall R. Model robust confidence intervals using maximum likelihood estimators. International Statistical Review. 1986;54:221–226. [Google Scholar]
- Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Quarterly. 2005;83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroupe KT, Smith BM, Hogan TP, St Andre JR. Healthcare utilization and costs of Veterans screened and assessed for traumatic brain injury. Journal of Rehabilitation Research & Development. 2013;50:1047–1068. doi: 10.1682/JRRD.2012.06.0107. [DOI] [PubMed] [Google Scholar]
- Stuart EA. Matching methods for causal inference: A review and a look forward. Statistical Science. 2010;25:1–21. doi: 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Houtven C, Voils C, Weinberger M. An organizing framework for informal caregiver interventions: Detailing caregiving activities and caregiver and care recipient outcomes to optimize evaluation efforts. BioMed Central-Geriatrics. 2011;11:77. doi: 10.1186/1471-2318-11-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanderWeele TJ, Shpitser I. A new criterion for confounder selection. Biometrics. 2011;67:1406–1413. doi: 10.1111/j.1541-0420.2011.01619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veterans Health Administration. 2012 VHA facility quality and safety report. Office of informatics and business analytics. Department of Veterans Affairs; VHA, US: 2012. [Google Scholar]
- Veterans Health Administration. Blueprint for excellence. 2014 Retrieved from https://www.va.gov/health/docs/VHA_Blueprint_for_Excellence.pdf.
- Wagner T, Chow A, Barnett P. HERC’s average cost datasets for VA inpatient care FY1998–FY2008. Palo Alto, VA: Health Economics Resource Center; 2009. [Google Scholar]
- Wagner T, Upadhyay A, Cowgill E, Sterfos T, Moran E, Asch S, Almenoff P. Risk adjustment tools for learning health systems: A comparison of DxCG and CMS-HCC V21. Health Services Research. 2016;51:2002–2019. doi: 10.1111/1475-6773.12454. [DOI] [PMC free article] [PubMed] [Google Scholar]


