Abstract
The minority stress process of internalized homophobia (IH) has been associated with a range of adverse health outcomes among gay and bisexual men (GBM). However, evidence is mixed regarding the effect of IH on drug use, suggesting the potential role of multiple mediated pathways. Researchers have linked depression, sexual anxiety, and gay community attachment with IH. Depression, sexual anxiety, and gay community attachment have also been linked with drug use and drug-related problems suggesting potential mediating roles. A U.S. national sample of 1,071 HIV-negative GBM completed at-home surveys, including measures of sociodemographic characteristics, IH, depression, sexual anxiety, gay community attachment, and drug use and associated problems. Adjusting for sociodemographic characteristics, depression mediated the association between IH and recent drug use. IH was positively associated with depression, and depression was positively associated with recent drug use. Gay community attachment partially mediated drug-related problems. IH had a positive direct association with drug-related problems and a negative direct association with gay community attachment. Gay community attachment had a positive association with drug-related problems. IH was positively associated with sexual anxiety, but sexual anxiety was not associated with either drug outcome. Efforts to reduce IH among HIV-negative GBM are likely to have a positive impact on mental health problems, as well as reduce risk for drug use and drug-related problems. Gay communities could provide the social support necessary for reducing IH; however, emphasis on community level interventions that address factors that increase risk for drug-related problems remains important.
Keywords: gay and bisexual men, internalized homophobia, depression, sexual anxiety, gay community, drug use
INTRODUCTION
Gay and bisexual men (GBM) living in the U.S. are 1.4–1.9 times more likely to meet criteria for a lifetime drug use disorder compared to heterosexual men (Kerridge et al., 2017). Disparities in drug use among GBM may result from the influence of minority stress (Hatzenbuehler, Jun, Corliss, & Austin, 2015; Meyer, 2003); the minority stress model posits that GBM experience unique and chronic stress because of the stigma associated with their sexual orientation. Sexual minority stressors range from distal objective stressors (e.g., victimization, harassment, and discrimination) to more proximal subjective stressors, which relate to self-identification as a sexual minority (e.g., concealment, expectations of rejection, and internalized homophobia). Presumably, the additive effect of sexual minority stress combined with other, non-minority, stressors serves to increase the risk of adverse health outcomes, including drug use. Evidence suggests GBM use drugs to cope with high levels of stress (Hamilton & Mahalik, 2009; Rosario, Schrimshaw, & Hunter, 2006) and associations between drug use and structural stigma (Hatzenbuehler et al., 2015), experiences of gay related harassment and victimization (McCabe, Bostwick, Hughes, West, & Boyd, 2010), and expectations of rejection (Pachankis, Hatzenbuehler, & Starks, 2014) have been observed.
Internalized homophobia (IH) is the most proximal minority stress process and is defined as the internalization of negative societal attitudes regarding homosexuality (Meyer & Dean, 1998). Other terms have been proposed to describe the internalization of these stigmatizing attitudes and the associated negative self-regard, including internalized homonegativity, internalized heterosexism, and internalized sexual stigma (Herek, Gillis, & Cogan, 2009; Shoptaw et al., 2009). In addition to negative self-regard, IH involves global anti-gay attitudes, isolation from other sexual minority group members, and discomfort with sexual-identity disclosure and same-sex acts (Meyer & Dean, 1998). IH and drug use are likely associated because early experiences of homophobia, both internal and external, likely teach GBM that their needs and feelings are unacceptable, need to be suppressed, and kept invisible from others. This results in the frequent use of coping strategies that involve the suppression or avoidance of natural feelings and provide an escape from their homophobic reality (Cabaj, 2000). As young GBM emerge into adulthood, they may utilize drugs to reduce negative affect associated with IH (Mays, Cochran, & Zamudio, 2004; McCabe et al., 2010).
Although IH has been found to correlate with a range of negative physical and mental health outcomes (Herek et al., 2009; Lick, Durso, & Johnson, 2013; Meyer, 2003), research on the association between IH and drug use has produced mixed results (Brubaker, Garrett, & Dew, 2009). Inconsistencies in the operationalization of drug use and drug-related problems may explain some of the mixed findings. Research suggests that IH is associated with use but different directions of effects have been observed by type of drug use. For example, two studies observed positive associations with any street drug use (excluding marijuana; Shoptaw et al., 2009; Quinn, et al, 2015) but another study observed a negative association with “club drug” use (Lea, de Wit, & Reynolds, 2014) suggesting the way drug use is operationalized may influence study findings. In the study by Quinn and colleagues (2015), IH was positively associated with street drug use but not with the number of use days which is consistent with other research and suggests an association between IH and any use but not frequency of use (Brubaker, Garrett, & Dew, 2009).
Studies have utilized popular screening measures to assess for problems related to drug abuse (e.g., Livingston, Oost, Heck, & Cochran, 2015). For dependence, measures mapping onto diagnostic criteria have often been used (e.g., Diagnostic Interview Schedule) and there is variability in whether dependence was assessed for a single substance (e.g., cocaine dependence; Hequembourg & Dearing, 2013) or a combination of substances (e.g., club drug dependence; Hequembourg & Dearing, 2013; Lea et al., 2014). Studies that have distinguished between use and problematic use have produced mixed results (Lea et al., 2014). For example, in a study of young gay, lesbian, and bisexual adults IH was associated with recent club drug use but was not associated with club drug dependence (Lea et al., 2014). This suggests that future research should simultaneously examine associations for both use and problematic use.
The presence of indirect pathways may also explain the mixed findings of previous research. Non-significant direct effects can arise when there are multiple competing pathways linking two variables and the direction of these pathways are variable (A. F. Hayes, 2009). Some studies have examined potential mediating factors between IH and substance use in mixed samples of lesbian, gay, and bisexual individuals, including psychological distress and closeness with the lesbian, gay, and bisexual community (e.g., D’Augelli, Grossman, Hershberger, & O’Connell, 2001; Igartua, Gill, & Montoro, 2003). Although these studies did not model indirect effects, the findings from these studies support positive asssociations between IH and these factors and between these factors and substance use when included in the same model. One study has examined the indirect association between IH and substance use. In this study of HIV-positive GBM, the authors found that stimulant use (frequent use compared to less frequent use) mediated the association between IH and sexual risk behavior, and negative affect mediated the association between IH and stimulant use (M. O. Johnson, Carrico, Chesney, & Morin, 2008). There is a need for additional research that investigates multiple indirect pathways, through which IH may influence drug use, simultaneously.
The association between IH and psychological distress among GBM is well-documented (Burns, Kamen, Lehman, & Beach, 2012; Frost & Meyer, 2009; Gold, Marx, & Lexington, 2007; Morandini, Blaszczynski, Ross, Costa, & Dar-Nimrod, 2015; Wagner, Brondolo, & Rabkin, 1997). A recent meta-analysis of studies on sexual minorities revealed small to moderate positive correlations between IH and clinical symptoms of depression and anxiety (Newcomb & Mustanski, 2010). An association between psychological distress and drug use has also been observed (Ibañez, Purcell, Stall, Parsons, & Gómez, 2005; M. O. Johnson et al., 2008; Kessler, 2003; Traube, Schrager, Holloway, Weiss, & Kipke, 2013). This literature suggests that negative affect is associated with avoidant coping and that avoidant coping is associated with drug use (McKirnan, Vanable, Ostrow, & Hope, 2001; Wagner et al., 1997). Specifically, IH has been positively associated with depression (Igartua et al., 2003; Morandini et al., 2015), and positive associations between depression and illicit drug use (Kecojevic, Wong, Corliss, & Lankenau, 2015; Mimiaga et al., 2010; Traube et al., 2013), as well as increased risk for drug dependence (Reisner et al., 2010; Traube et al., 2013), have been observed. Most anxiety research has focused on the association between IH and generalized anxiety but some evidence suggests IH is associated with sexual anxiety, defined here as worrisome thoughts or uneasy feelings surrounding the sexual aspects of one’s own life, among GBM (Dupras, 1994; Weiss & Hope, 2011). Similar to depression, sexual anxiety may also be associated with drug use (Rosario et al., 2006) as evidenced by associations between general anxiety symptoms and drug-related problems (Igartua et al., 2003). GBM may turn to drug use as an effective strategy for reducing uncomfortable self-awareness in sexual situations (e.g., HIV-transmission risk), to assist in narrowing their focus to the current situation (McKirnan et al., 2001), to reduce anxiety about sex induced by IH (Cabaj, 2000; Cheng, 2003) and to improve sexual functioning that may be impacted by negative affect (Barlow, 1986).
Community plays an important role in identity formation as it may be helpful in reconciling conflicting beliefs and values (Meyer, 2003). For GBM, attachment to the gay community is associated with lower levels of sexual minority stress (Carpiano, Kelly, Easterbrook, & Parsons, 2011; Meyer, 2003). However, connection to the gay community may promote unhealthy behaviors through submersion into a subculture that promotes drug use and provides easier access to drugs. Gay bars and clubs remain primary social outlets for GBM and attendance at these venues is associated with increased drug use (Greenwood et al., 2001; Halkitis, Fischgrund, & Parsons, 2005), perhaps as a mechanism to increase belonging with the gay community (Green & Feinstein, 2012; Klitzman, Greenberg, Pollack, & Dolezal, 2002). Thus, IH may be directly associated with increased drug use, but gay community attachment may constitute an indirect path where IH is negatively associated with drug use.
The present study sought to examine the association between IH and two drug use outcomes: 1) recent drug use and 2) drug-related problems (among those who report recent use) in a large-scale online cohort study of GBM living in the U.S. In addition to examining direct associations, we tested the hypotheses that depression, sexual anxiety, and gay community attachment would partially mediate these associations. Specifically, we hypothesized that IH would have positive direct associations with depression and sexual anxiety and a negative association with gay community attachment and that IH would have a positive indirect associations through both depression and sexual anxiety and a negative indirect association through gay community attachment for both drug outcomes.
METHOD
The [blind for review] cohort is a longitudinal study prospectively following a U.S. national sample of GBM for a period of three years [blind for review]. Analyses for the present manuscript use data collected at baseline in 2014.
Participants and Procedures
Recruitment and baseline incentive procedures have been described in detail elsewhere [blind for review]. In brief, participants were identified via Community Marketing and Insights, Inc. (CMI) panel of over 45,000 LGBT individuals, over 22,000 of which are GBM throughout the U.S. CMI draws panelists from over 200 sources ranging from LGBT events to social media and email broadcasts distributed by LGBT organizations, and includes non-gay identified venues/mediums such to maintain a robust and diverse panel of participants from across the U.S. CMI targeted individuals based on pre-specified characteristics and invited them to participate in our study. Our goal was to recruit a sample of GBM who represented the diversity and distribution of GBM at the U.S. population level. In so doing, we used data from the U.S. Census regarding same sex households, and racial and ethnic composition to populate our recruitment parameters. CMI identified participants from their panel and screened them for eligibility. Those deemed preliminary eligible had their responses and contact information shared with the research team, and we then independently pursued participants for full enrollment and longitudinal assessment.
To be preliminarily eligible for [blind for review], participants had to reside in the U.S., be at least 18 years of age, be biologically male and currently identify as male, identify as gay or bisexual, report having sex with a man in the past year, self-identify as HIV-negative, be willing to complete at-home self-administered rapid HIV antibody testing (those testing positive at baseline were not included in the [blind for review] cohort), be willing to complete self-administered home-based testing for urine and rectal Chlamydia/gonorrhea, be able to complete assessments in English, have access to the Internet so as to complete at-home online assessments, have access to a device that was capable of taking a digital photo (e.g., camera phone, digital camera), have an address to receive mail that was not a P.O. Box, and be residentially stable (i.e., have not moved more than twice in the past 6 months). All procedures were reviewed and approved by the Institutional Review Board of the [blind for review].
Measures
Data were collected using measures administered during the screening survey and baseline online survey which was programmed and administered via Qualtrics. The present study included measures of demographic characteristics, IH, depression, sexual anxiety, gay community attachment, and drug use and related problems.
Demographic characteristics
Participants reported their age, race and ethnicity, income, education, sexual orientation, and relationship status. Participants also provided their zip code, which was used to create a population density rank-ordered variable based on recent census data.
Internalized homophobia
The Internalized Homophobia Scale (IHS; Martin & Dean, 1988; Meyer, 1995) is a 9-item scale that measures internalized stigma associated with having a non-heterosexual sexual orientation. Responses to all nine items were averaged (range 1 to 4) with higher average scores indicating greater IH (Cronbach’s α = .86).
Depression
The 20-item Center for Epidemiological Studies-Depression scale (CESD; Radloff, 1977) was administered during the baseline CASI to assess depressive symptomology in the past three months. Scores were summed to form an overall score (range 0–60) and higher scores indicated greater levels of depressive symptoms in the past three months (Cronbach’s α = .93).
Sexual Anxiety
Participants completed the 5-item sexual anxiety subscale of the Multidimensional Sexuality Questionnaire (Snell, 1998) which assesses anxiety surrounding the sexual aspects of the participant’s life (e.g., “I feel anxious when I think about the sexual aspects of my life” and “I usually worry when I think about the sexual aspects of my life”). Responses were averaged (range 0–5) with higher scores indicating greater anxiety surrounding the sexual aspects of the participant’s life (Cronbach’s α = .88).
Gay Community Attachment
Participants answered five questions that assessed their connectedness to the gay community (Carpiano et al., 2011) (e.g., “I have a strong sense of belonging to the gay/bisexual community” and “I am happy that I am a member of the gay/bisexual community”). Responses were averaged across all five items (range 1–4) with higher scores indicating stronger attachment to the gay community (Cronbach’s α = .90).
Recent drug use
Participants reported the number of substance using days (range 0–90) in the past 3 months for cocaine, crack, crystal meth, ecstasy, GHB, heroin/opiates, ketamine, and recreational use of prescription drugs. A dichotomous recent drug use variable was created with scores of 0 indicating no use of any of these drugs in the past 90 days and 1 indicating any use of at least one of these drugs in the past 90 days.
Drug-related problems
Among those who reported recent use of any drug listed, the 10-item Drug Abuse Screening Test (DAST-10; Skinner, 1982) was administered to assess the degree of problems associated with recreational use of any illicit drugs other than alcohol, marijuana, and poppers in the past 3 months. Responses were summed to create a DAST-10 score (range 0–10; Cronbach’s α = .73) with higher scores indicating more problems related to drug use.
Analytic Plan
Analyses were done using Mplus 7.0. Given that individuals who reported the recent use of drugs reported on drug use associated problems, we utilized a two-step modeling procedure (Coxe, West, & Aiken, 2009). This procedure involves the use of two dependent variables modeled simultaneously: a binary variable indicating whether the individual reported recent drug use and a continuous variable indicating the severity of drug related problems among those who reported recent drug use. In order to examine the influence of indirect effects on the direct effect estimates, we calculated two models. In the first model, the direct effects of IH on recent drug use and drug-related problems were evaluated simultaneously controlling for age, race, population density, income, education, and relationship status. In the second model, a path model was specified, which included depression, sexual anxiety, and gay community attachment as mediators between IH and recent drug use and drug-related problems. Indirect effects of IH on the outcomes (through depression, sexual anxiety, and gay community attachment) were evaluated using bootstrapping tests of significance with 1000 boot-strapping draws. All models utilized weighted least squares means and variances estimation, which permits the use of bootstrapping tests of mediation. Our plan of analysis is consistent with the method for testing both direct and indirect effects recommended by Hayes (2009). Hayes argues that testing the indirect effects using bootstrapping provides greater power for detecting the presence of a true indirect effect compared to the commonly used causal step approach outlined by Baron and Kenny (1986).
RESULTS
The screening and baseline survey was completed by 1,268 men. Of those men, 1,071 (84.5%) also completed at home HIV and STI testing and were enrolled in the [blind for review] cohort. The demographic characteristics of the sample are provided in Table 1. The average age of the sample was 40.24 years (range = 18–79; SD = 13.83). The majority of participants identified as gay (95.0%), White, non-Hispanic (71.2%), had at least a 4-year college degree or more (55.7%), and earned $30,000 or more a year (68.8%). Drug use in the previous 90 days was reported by 192 participants (17.9%).
Table 1.
Demographic Characteristics of the Sample (N = 1,071)
| n | % | |
|---|---|---|
| Sexual Orientation | ||
| Gay | 1017 | 95.0 |
| Bisexual | 54 | 5.0 |
| Race/Ethnicity | ||
| White | 763 | 71.2 |
| Black/African American | 83 | 7.7 |
| Latino | 135 | 12.6 |
| Other/Multiracial | 90 | 8.4 |
| Relationship Status | ||
| Single | 549 | 51.3 |
| Partnered | 522 | 48.7 |
| Education | ||
| High School, GED, or less | 77 | 7.2 |
| Some college, associates degree | 397 | 37.1 |
| 4-year degree or more | 597 | 55.7 |
| Income | ||
| Less than $30,000/year | 334 | 31.2 |
| $30,000 a year or more | 737 | 68.8 |
| Geographic Region | ||
| South | 377 | 35.2 |
| West | 297 | 27.7 |
| Northeast | 204 | 19.0 |
| Midwest | 192 | 17.9 |
| Recent Drug Use (not including marijuana) | ||
| Yes (past 90 days) | 192 | 17.9 |
| No (past 90 days) | 879 | 82.1 |
| Drugs Used | ||
| Recreational Prescription Drugs | 124 | 11.6 |
| Cocaine | 56 | 5.2 |
| Ecstasy/MDMA | 43 | 4.0 |
| Methamphetamine | 25 | 2.3 |
| Heroin | 17 | 1.6 |
| GHB | 14 | 1.3 |
| Ketamine | 9 | 0.8 |
| Crack | 5 | 0.5 |
| M | SD | |
|
|
||
| Age (Range: 18 –79; Median = 39) | 40.24 | 13.8 |
Table 2 contains bivariate associations among observed variables as well as the means and standard deviations of our continuous variables. Older age, greater population density, higher income, higher education, and being in a relationship were associated with lower depression scores. Older age and being in a relationship were associated with lower sexual anxiety scores. Greater population density, greater income, and being in a relationship were all associated with greater gay community attachment. Participants who reported being White, non-Hispanic also reported greater gay community attachment. Those who reported any recent drug use were less likely to self-identify as White, non-Hispanic. Likelihood of recent drug use was also higher among those younger in age and living in more densely populated areas. In regards to problems related to drug use, those who reported having more income reported fewer problems related to drug use.
Table 2.
Bivariate associations between the psychosocial constructs and drug outcomes
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | – | |||||||||||
| 2. Race | .24*** | – | ||||||||||
| 3. Population Density | −.02 | −.15*** | – | |||||||||
| 4. Income | .28*** | .04 | .16*** | – | ||||||||
| 5. Education | .11*** | .05 | .19*** | .24*** | – | |||||||
| 6. Relationship Status | .06* | .05 | −.04 | .11*** | .06 | – | ||||||
| 7. Internalized Homophobia | −.14*** | −.09** | −.12*** | −.09** | −.05 | −.10*** | – | |||||
| 8. Gay Community Attachment | .05 | .08** | .14*** | .07* | .02 | .08** | −.45*** | – | ||||
| 9. Depression | −.17*** | −.03 | −.10*** | −.23*** | −.12*** | −.14*** | .24*** | −.22*** | – | |||
| 10. Sexual Anxiety | −.15*** | −.02 | −.04 | −.06* | −.00 | −.12*** | .33*** | −.20*** | .36*** | – | ||
| 11. Recent Drug Use (not including marijuana) | −.14*** | −.11*** | .07* | −.04 | −.02 | −.01 | .02 | −.02 | .09** | .05 | – | |
| 12. DAST score | −.12 | .11 | −.02 | −.15* | −.08 | −.11 | .19** | .08 | .15* | .15* | – | – |
|
| ||||||||||||
| M | 1.36 | 3.11 | 1.36 | 16.46 | – | 1.90 | ||||||
| SD | 0.48 | 0.66 | 0.48 | 11.61 | – | 1.90 | ||||||
Note. N = 1071.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Table 3 contains the results of the analyses examining the direct effects of IH on recent drug use and drug-related problems. After adjusting for demographic factors, IH was unrelated to the odds of reporting recent drug use; however, among those who reported recent drug use, IH was positively associated with drug-related problems.
Table 3.
Direct Effect of Internalized Homophobia on Odds of Recent Drug and Drug-related Problems
| Recent Drug Usea
|
Drug-related Problems (n=192)
|
||||||
|---|---|---|---|---|---|---|---|
| B | 95% CI | AOR | β | B | 95% CI | β | |
| Age | −0.01 | [−0.02, 0.01] | 0.99 | −0.17*** | −0.01 | [−0.03, 0.01] | −0.08 |
| Race (Ref: Non-White) | −0.23 | [−0.44, −0.03] | 0.79 | −0.10* | 0.58 | [0.04, 1.12] | 0.14* |
| Population Density | 0.10 | [−0.00, 0.20] | 1.10 | 0.09† | 0.05 | [−0.25, 0.34] | 0.03 |
| Income (Ref: Less than 30K) | −0.03 | [−0.25, 0.19] | 0.97 | −0.01 | −0.52 | [−1.12, 0.08] | −0.13† |
| Education (Ref: Less than BA) | −0.05 | [−0.23, 0.14] | 0.96 | −0.02 | −0.07 | [−0.68, 0.55] | −0.02 |
| Relationship Status (Ref: Single) | 0.02 | [−0.17, 0.21] | 1.02 | 0.01 | −0.28 | [−0.80, 0.24] | −0.08 |
| Internalized Homophobia | 0.02 | [−0.18, 0.21] | 1.02 | 0.01 | 0.69 | [0.10, 1.27] | 0.17* |
Note. N = 1071.
p ≤ .10.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Referrent group for recent drug use was no drug use in the past 90 days
Figure 1 depicts a path model with depression, sexual anxiety, and gay community attachment incorporated as potential mediators. Table 4 contains information for all regression parameters incorporated into the model. With respect to mediators, IH was positively associated with depression. In contrast, age, income, and being in a relationship were negatively associated with depression. Similarly, IH was positively associated with sexual anxiety, and age and being in a relationship were negatively associated with sexual anxiety. IH was negatively associated with gay community attachment whereas being White, non-Hispanic and greater population density were positively association with gay community attachment. With respect to outcomes, population density was positively associated with the odds of recent drug use. In contrast, age and identifying as white were negatively associated with odds of recent drug use. For every one-unit increase in depression score, odds of reporting recent drug use increased by 2%. For drug-related problems, race/ethnicity and IH were significantly associated with drug-related problems. Drug using men who reported having a White, non-Hispanic identity reported significantly more drug-related problems compared to racial/ethnic minority men. Both IH and gay community attachment were significantly associated with greater drug-related problems.
Figure 1.
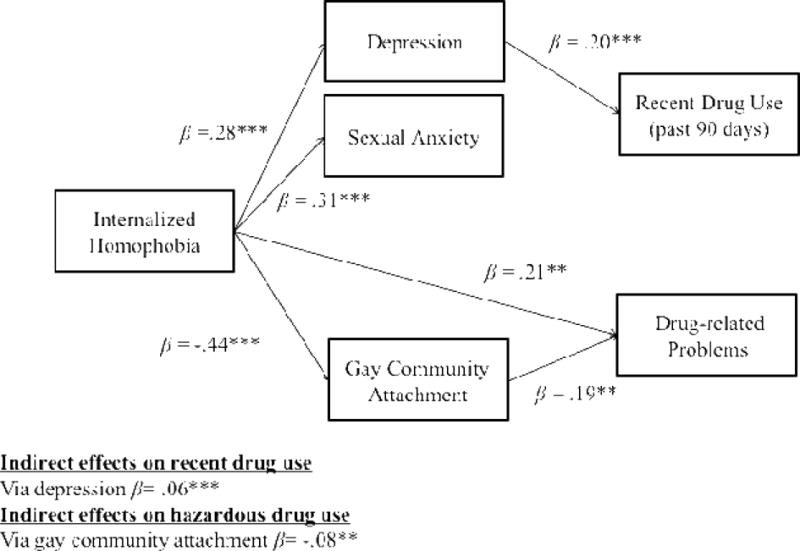
Internalized homophobia, mediators, and recent and drug-related problems: Path model results.
Table 4.
Path Coefficients
| Depression
|
Sexual Anxiety
|
Gay Community Attachment
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | β | B | 95% CI | β | B | 95% CI | β | |
| Age | −0.05 | [−0.10, 0.00] | −0.06† | −0.01 | [−0.01, −0.00] | −0.11*** | 0.00 | [−0.00, 0.00] | −0.03 |
| Race (Ref: Non-White) | −0.12 | [−1.61, 1.37] | −0.01 | 0.08 | [−0.04, 0.20] | 0.04 | 0.09 | [0.01, 0.18] | 0.07* |
| Population Density | −0.29 | [−0.95, 0.36] | −0.03 | −0.01 | [−0.06, 0.05] | −0.01 | 0.06 | [0.03, 0.10] | 0.10*** |
| Income (Ref: Less than 30K) | −5.22 | [−6.84, −3.60] | −0.21*** | 0.00 | [−0.14, 0.13] | 0.00 | 0.03 | [−0.06, 0.12] | 0.02 |
| Education (Ref: Less than BA) | −0.92 | [−2.27, 0.44] | −0.04 | 0.06 | [−0.06, 0.18] | 0.03 | −0.03 | [−0.11, 0.04] | −0.03 |
| Relationship (Ref: Single) | −2.33 | [−3.57, −1.08] | −0.10*** | −0.17 | [−0.28, −0.07] | −0.09** | 0.05 | [−0.02, 0.12] | 0.04 |
| Internalized Homophobia | 6.72 | [5.08, 8.37] | 0.28*** | 0.62 | [0.50, 0.75] | 0.31*** | −0.61 | [−0.70, −0.51] | −0.44*** |
| Recent Drug Usea | Drug-related Problems (n=192)b | ||||||
|---|---|---|---|---|---|---|---|
| B | 95% CI | AOR | β | B | 95% CI | β | |
| Age | −0.01 | [−0.02, −0.00] | 0.99 | −0.16** | −0.01 | [−0.03, 0.01] | −0.07 |
| Race (Ref: Non-White) | −0.23 | [−0.43, −0.03] | 0.79 | −0.10* | 0.53 | [0.00, 1.05] | 0.13* |
| Population Density | 0.11 | [0.01, 0.20] | 1.11 | 0.10* | 0.02 | [−0.27, 0.31] | 0.01 |
| Income (Ref: Less than 30K) | 0.07 | [−0.15, 0.29] | 1.07 | 0.03 | −0.44 | [−1.03, 0.16] | −0.11 |
| Education (Ref: Less than BA) | −0.03 | [−0.22, 0.15] | 0.97 | −0.02 | −0.04 | [−0.65, 0.57] | 0.01 |
| Relationship (Ref: Single) | 0.07 | [−0.11, 0.26] | 2.10 | 0.04 | −0.24 | [−0.77, 0.28] | −0.06 |
| Internalized Homophobia | −0.17 | [−0.41, 0.07] | 0.84 | −0.08 | 0.81 | [0.18, 1.44] | 0.21* |
| Depression | 0.02 | [0.01, 0.03] | 1.02 | 0.20*** | 0.02 | [−0.01, 0.04] | 0.12 |
| Sexual Anxiety | 0.06 | [−0.04, 0.16] | 1.06 | 0.06 | −0.11 | [−0.19, 0.41] | 0.06 |
| Gay Community Attachment | −0.04 | [−0.20, 0.11] | 0.96 | −0.03 | 0.53 | [0.14, 0.91] | 0.19** |
Note. N = 1071.
p ≤.10.
p ≤ .05.
p ≤ .01.
p ≤ .001.
Referrent group for recent drug use was no drug use in the past 90 days.
Based upon the pattern of observed direct effects, the indirect effect on recent drug use through depression and the indirect effects on drug-related problems through gay community attachment were tested. Bootstrapping tests suggested that IH has a significant indirect effect on recent drug use through depression (B = 0.056, SE = 0.014, p < .001). We also observed significant negative indirect effects through gay community attachment for drug-related problems (B = −0.081, SE = 0.030, p = .008).
DISCUSSION
Results from this study illustrate two critical factors in understanding the association between IH and drug use outcomes. First, distinguishing between the prediction of recent use and hazardous use among those who are using was meaningful. Depression mediated the association between IH and recent drug use, but gay community attachment, not depression, mediated the association between IH and drug-related problems. Second, these results suggest that both positive and negative indirect pathways link IH with drug use among GBM. The indirect pathway through depression on recent drug use was positive but the indirect pathway through gay community attachment on drug-related problems was negative.
The finding that IH is associated with drug use through a pathway mediated by depression is consistent with previous research. Positive associations between IH and depression among GBM have been observed elsewhere (Newcomb & Mustanski, 2010). In addition, depression has also been linked with drug use and associated problems in previous studies involving GBM, often in consideration of syndemic factors related to health disparities and HIV infection (Mustanski, Andrews, Herrick, Stall, & Schnarrs, 2013; Parsons, Grov, & Golub, 2012; Stall et al., 2001). Interestingly, while depression predicted whether a person engaged in recent drug use, depression was not significantly associated with drug-related problems. Previous studies have documented associations between depression and drug use disorders (J. H. Lee et al., 2015). It is plausible that sample composition accounts for this difference. In the current study, only 18% of participants reported recent drug use and provided information on the number of problems they experienced related to their use. Samples comprised of a higher concentration of participants using drugs may be better able to examine differences in problem severity predicted by other mental health factors among those who use. However, most of the current knowledge regarding drug use among GBM stems from studies where elevations in risk (e.g., recent drug use; sexual risk behavior) were included as part of eligibility criteria or from studies that used localized samples (e.g., large urban cities). The minority stress literature emphasizes that despite the sexual-orientation based stress GBM experience, a majority of the men in this community lack any significant physical or mental health problems, including problems with substance use (Hatzenbuehler, 2009; Meyer, 2003). The findings from the present study fill an important gap in the literature and speak to the nature of association between depression and drug problems among a predominately-healthy nationwide sample of HIV-negative GBM.
Alternatively, research has demonstrated differential effects of depression on substance use among GBM. For example, one study found that depression was associated with lower use of opioids but increased use of stimulants (Kecojevic et al., 2015). These findings suggest that depression may have differential associations depending on the type of drug use examined. In the present study, we were underpowered to examine individual classes of drugs but given the evidence to suggest the associations between depression and IH and drug use differ depending on the type of drug examined future research should examine these associations by type of drug. This research should also aim to understand the nuance of drug-related problems experienced by GBM for different types of drugs.
Sexual anxiety did not link IH and drug use outcomes in this sample. Nonetheless, the direct association between IH and sexual anxiety was consistent with previous studies in that we found a significant positive association (Dupras, 1994). However, unlike some previous studies demonstrating an association between general anxiety symptoms and drug use among GBM (Lelutiu-Weinberger et al., 2013; Rosario et al., 2006), there was no evidence of an association between sexual anxiety and drug outcomes in the current sample. One potential explanation for the non-significant findings is that these studies examined anxiety and substance use among young GBM and drugs may be relied on more to cope with current stressors. As GBM get older, they may develop more adaptive coping strategies. Another possible explanation is that the measure of sexual anxiety used here was a general measure of anxiety associated with the sexual aspects of a person’s life. Other, more specific measures of sexual anxiety, particularly measures of anxiety in the context of sexual behavior, may have an influence on the association between IH and drug outcomes (McKirnan, Ostrow, & Hope, 1996). For example, drugs may be used to counteract anxieties stemming from fear of rejection from sexual partners, fear of HIV-infection, and worries about sexual performance (Cochran, Sullivan, & Mays, 2003; Hirshfield et al., 2010; Starks, Millar, Tuck, & Wells, 2015). Another potential explanation is that other forms of anxiety may explain the association between IH and drug use. Several studies have documented associations between IH and anxiety surrounding peer evaluation and rejection (Burns et al., 2012; Feinstein, Goldfried, & Davila, 2012).
Research among sexual minorities suggests the adverse effects of sexual minority stress may also be influenced by the level of connectedness to the gay community (Meyer, 2003). Our findings are consistent with previous research on IH and connectedness to the gay community and suggest that gay communities play an important role in identity formation and self-acceptance. There is mixed evidenced on the direction of the association between gay community connectedness and drug use (Carpiano et al., 2011; D’Augelli et al., 2001; Lelutiu-Weinberger et al., 2013) and the findings from the present study suggest connectedness to the gay community is associated with greater risk for drug-related problems. High levels of IH may serve as a barrier to engagement with the gay community by GBM thereby also serving as a barrier from community level factors that lead to greater substance use. The present study provides some support for a negative indirect association between IH and hazardous substance use. Future research should examine the influence of perceived social norms and expectancies surrounding drug use (Hatzenbuehler, Corbin, & Fromme, 2008).
It is important to note that the direct effect between IH and drug-related problems was statistically significant in the both models with and without the proposed mediators. IH could have a direct influence on the risk for developing a drug use disorder. Alternatively, additional indirect pathways may exist involving other unmeasured variables. As mentioned above, other forms of anxiety may play a role as well as perceived social norms and substance use expectancies (Burns et al., 2012; Hatzenbuehler et al., 2008; Hirshfield et al., 2010). Factors, such as coping and emotion dysregulation (e.g., poor emotional awareness), self-esteem, and social isolation (Brubaker et al., 2009; Hatzenbuehler, 2009), require further consideration.
These results have the potential to inform the development and provision of clinical treatments aimed at improving mental health through the development of adaptive coping skills among GBM. Drug use has been characterized as an avoidant coping strategy (Barrett et al., 1995; Collins et al., 2001) and GBM may engage in drug use as a way to manage negative thoughts and feelings associated with IH and depression (Cabaj, 2000; Weber, 2008). Although our study did not examine coping style, IH has been found to be associated with greater use of avoidant coping (Nicholson & Long, 1990). A challenge with avoidant coping is that it does not allow for the resolution of stressors and it precludes new learning which inhibits the development of adaptive coping. This has important implications for treatment given that reducing drug use may reveal stressors related to IH that will need attention. Our findings suggest that affirmative therapies that address the negative ideations surrounding sexual orientation and promotes self-acceptance and self-compassion may serve to benefit GBM. Drug use among GBM may be positively influenced by therapies that aim to affirm non-heterosexual identities while addressing associated stigma (e.g., Gay Affirmative Therapy, Langdridge, 2007). Acceptance and Commitment Therapy (S. C. Hayes, Luoma, Bond, Masuda, & Lillis, 2006) may also benefit mental health and drug outcomes for GBM by improving psychological flexibility in an effort to move clients away from avoidance driven cognitions and behaviors to cognitions and behaviors that are helpful and positive (e.g., mindfulness and acceptance). Furthermore, motivational interviewing, a collaborative and participant-centered approach (Miller & Rollnick, 2012), has been shown to be effective in reducing drug use among GBM (Parsons, Lelutiu-Weinberger, Botsko, & Golub, 2014). Incorporation of motivational interviewing into affirmative therapies may help facilitate change in drug use as well as other risk behaviors among GBM.
Our findings for drug-related problems emphasize the continuing importance of community level interventions that address substance use in the gay community. Acceptance of the gay community has continued to increase and as a result there may be less of a need for gay specific venues and neighborhoods in order for GBM to socialize and feel safe (Carpiano et al., 2011). However, the development of a gay social network appears to be important in reconciling internalized stigma and potentially reducing internalizing psychopathology (Newcomb & Mustanski, 2010). Our findings suggest that interventions that address permissive norms and expectations surrounding drug and alcohol abuse in the gay community remain important.
Limitations
These findings should be considered in light of some limitations. Data are cross-sectional and mediation analyses using cross-sestional data have the potential to produces biased estimates depending on the stability of independent and mediating variables in the model (Maxwell & Cole, 2007). Longitudinal studies are needed to evaluate whether elevations in IH, depression and gay community attachment precede changes in drug use and how these variables change over time. Participants were recruited from nearly all 50 states; a large majority of the sample self-identified as White, non-Hispanic and had high levels of education and income. It should be noted, however, that a larger proportion of Black and Latino men were ineligible for the study due to self-report that they were HIV-positive, which is consistent with established racial disparities in HIV prevalence (A. S. Johnson et al., 2014). We did observe some racial/ethnic differences in drug use and drug-related problems in our sample. Men of color were more likely to report recent drug use but White, non-Hispanic drug using men reported significantly more drug-related problems. This may be differences in rates of drug use of specific substances. For example, White GBM may be more likely to use stimulants which have a greater risk of dependence compared to some other drugs (Grov, Bimbi, Nanin, & Parsons, 2006). Having a greater representation of the racial/ethnic minorities as well as men lower in education and income would have allowed additional meaningful comparisons and increased generalizability.
Although CMI actively seeks out individuals via non-gay sources, almost all of the participants in the current sample self-identified as gay and were open enough about their sexual orientation to be a part of an LGBT marketing panel. Previous research has documented higher levels of IH among those who have same-sex attraction but may not identify as gay (Wolitski, Jones, Wasserman, & Smith, 2006). These findings may not generalize to other MSM, and samples that include a greater proportion of bisexual men and include MSM who do not identify as gay could potentially produce larger effects (Schrimshaw, Siegel, Downing, & Parsons, 2013). The present study relied on a self-report measure of IH and some evidence suggests that implicit measures of IH differ from explicit measures (Hatzenbuehler, Dovidio, Nolen-Hoeksema, & Phills, 2009) and that associations with psychosocial outcomes may be different depending on the type of measurement. Future research should examine whether the magnitude of these associations remains the same using implicit measures such as the Implicit Association Test (Greenwald, McGhee, & Schwartz, 1998).
Rates of drug use were low in the present study and consistent with other research we only examined drug use and drug-related problems among users of illicit drugs other than marijuana (Quinn et al., 2015). Psychological distress has been associated with increased marijuana usage (Rosario, Schrimshaw, & Hunter, 2009) and marijuana usage has been associated with increased risk of drug use disorders (Degenhardt, Hall, & Lynskey, 2001). This suggests we may have had greater variability in our drug related problems outcome had we included marijuana usage, and we may have observed different results. Only individuals who had reported using drugs in the previous 90-days reported on problems related to their drug use and we may be missing some of the population with a history of problematic drug use. We were also underpowered to analyze individual drugs and previous research suggests differential associations between stress and drug use based on the type of drug examined (Lea et al., 2014; Quinn et al., 2015).
Finally, the generalizability of these findings to HIV-positive GBM is limited. HIV-positive GBM may be at increased risk of negative health outcomes due to compounding stigma associated with being HIV-positive and having sex with men (Cramer, Colbourn, Gemberling, Graham, & Stroud, 2015; R. S. Lee, Kochman, & Sikkema, 2002). Future research should examine the role of IH, internalized HIV-stigma, depression, gay community attachment, and drug use to see if these findings are consistent with the present study.
Conclusions
Limitations notwithstanding, these findings have important implications in the prevention and treatment of mental health problems and drug use and abuse among GBM. Despite increased visibility and acceptance of the LGBT community, GBM continue to experience minority stress associated with having a non-heterosexual orientation and identity. Addressing the internalization of negative societal attitudes regarding same-sex attraction, behavior, and identity remains an important target for efforts aimed at improving the health of these men (Pachankis, 2015). Treatments that focus on self-acceptance of a sexual minority identity may reduce risk of depression, sexual anxiety, and problematic drug use. Given our findings on the mediating role of depression, treatments for depression are likely to benefit GBM at risk of drug use (Safren et al., 2012). Overall, our findings suggest that IH negatively impacts GBM in regards to drug-related outcomes but the presence of competing indirect effects may diminish the combined impact of IH. Our findings on the role of gay community attachment speak to the need of both individual and community level interventions that address social norms and expectancies surrounding drug use.
Acknowledgments
The One Thousand Strong study was funded by a research grant from the National Institute on Drug Abuse (R01 DA036466: Jeffrey T. Parsons & Christian Grov, MPIs). Raymond Moody’s effort was funded by a supplement to the parent grant (R01 DA036466-S2). Special thanks to the other members of the One Thousand Strong study team (Tyrel Starks, Ana Ventuneac, H. Jonathon Rendina, Mark Pawson, Michael Castro, Ruben Jimenez, Chloe Mirzayi, Brett Millar, Thomas Whitfield, and Jonathan Lassiter) and other staff from the Center for HIV/AIDS Educational Studies and Training (Chris Hietikko, Andrew Cortopassi, Brian Salfas, Doug Keeler, Qurrat-Ul Ain, Chris Murphy, and Carlos Ponton). Thank you to the staff at Community Marketing, Inc. (David Paisley, Heather Torch, and Thomas Roth) as well as Patrick Sullivan, Jessica Ingersoll, Deborah Abdul-Ali, and Doris Igwe at the Emory Center for AIDS Research (P30 AI050409). Finally, a special thanks to Jeffrey Schulden and Pamela Goodlow at NIDA. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Sources of Funding: One Thousand Strong was funded by the National Institutes of Health (R01 DA 036466: Parsons & Grov). Raymond L. Moody’s effort was funded by the National Institute of Drug Abuse (R01 DA 036466-S2; Parsons & Grov).
Footnotes
Conflict of Interest: Raymond L. Moody declares that he has not conflict of interest. Tyrel J. Starks declares that he has not conflict of interest. Christian Grov declares he has not conflict of interest. Jeffrey T. Parsons declares he has no conflict of interest.
COMPLIANCE WITH ETHICAL STANDARDS:
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent: Informed consent was obtained from all individual participants included in this study.
References
- Amadio DM. Internalized heterosexism, alcohol use, and alcohol-related problems among lesbians and gay men. Addictive Behaviors. 2006;31(7):1153–1162. doi: 10.1016/j.addbeh.2005.08.013. http://dx.doi.org/10.1016/j.addbeh.2005.08.013. [DOI] [PubMed] [Google Scholar]
- Barlow DH. Causes of sexual dysfunction: The role of anxiety and cognitive interference. Journal of consulting and clinical psychology. 1986;54(2):140–148. doi: 10.1037/0022-006X.54.2.140. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51(6):1173–1182. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barrett DC, Bolan G, Joy D, Counts K, Doll L, Harrison J. Coping strategies, substance use, sexual activity, and HIV sexual risks in a sample of gay male STD patients. Journal of Applied Social Psychology. 1995;25(12):1058–1072. doi: 10.1111/j.1559-1816.1995.tb00617.x. [DOI] [Google Scholar]
- Brubaker MD, Garrett MT, Dew BJ. Examining the relationship between internalized heterosexism and substance abuse among lesbian, gay, and bisexual individuals: A critical review. Journal of LGBT Issues in Counseling. 2009;3(1):62–89. doi: 10.1080/15538600902754494. [DOI] [Google Scholar]
- Burns MN, Kamen C, Lehman KA, Beach SR. Minority stress and attributions for discriminatory events predict social anxiety in gay men. Cognitive therapy and research. 2012;36(1):25–35. [Google Scholar]
- Cabaj RP. Substance abuse, internalized homophobia, and gay men and lesbians: Psychodynamic issues and clinical implications. Journal of Gay & Lesbian Psychotherapy. 2000;3(3–4):5–24. doi: 10.1300/J236v03n03_02. [DOI] [Google Scholar]
- Carpiano RM, Kelly BC, Easterbrook A, Parsons JT. Community and drug use among gay men the role of neighborhoods and networks. Journal of Health and Social Behavior. 2011;52(1):74–90. doi: 10.1177/0022146510395026. [DOI] [PubMed] [Google Scholar]
- Cheng Z. Issues and standards in counseling lesbians and gay men with substance abuse concerns. Journal of Mental Health Counseling. 2003;25(4):323–336. doi: 10.17744/mehc.25.4.nb107j9cqdc5j7ld. [DOI] [Google Scholar]
- Cocco KM, Carey KB. Psychometric properties of the Drug Abuse Screening Test in psychiatric outpatients. Psychol Assess. 1998;10(4):408. [Google Scholar]
- Cochran SD, Sullivan JG, Mays VM. Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of consulting and clinical psychology. 2003;71(1):53. doi: 10.1037//0022-006x.71.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL, Kanouse DE, Gifford AL, Senterfitt JW, Schuster MA, McCaffrey DF, Wenger NS. Changes in health-promoting behavior following diagnosis with HIV: Prevalence and correlates in a national probability sample. Health Psychology. 2001;20(5):351–360. doi: 10.1037/0278-6133.20.5.351. [DOI] [PubMed] [Google Scholar]
- Coxe S, West SG, Aiken LS. The analysis of count data: A gentle introduction to Poisson Regression and its alternatives. Journal of personality assessment. 2009;91(2):121–136. doi: 10.1080/00223890802634175. [DOI] [PubMed] [Google Scholar]
- Cramer RJ, Colbourn SL, Gemberling TM, Graham J, Stroud CH. Substance-related coping, HIV-related factors, and mental health among an HIV-positive sexual minority community sample. AIDS care. 2015:1–6. doi: 10.1080/09540121.2015.1024097. [DOI] [PubMed] [Google Scholar]
- D’Augelli AR, Grossman AH, Hershberger SL, O’Connell TS. Aspects of mental health among older lesbian, gay, and bisexual adults. Aging and Mental Health. 2001;5(2):149–158. doi: 10.1080/713650002. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M. Alcohol, cannabis and tobacco use among Australians: A comparison of their associations with other drug use and use disorders, affective and anxiety disorders, and psychosis. Addiction. 2001;96(11):1603–1614. doi: 10.1080/09652140120080732. [DOI] [PubMed] [Google Scholar]
- Dupras A. Internalized homophobia and psychosexual adjustment among gay men. Psychological Reports. 1994;75(1, Pt 1):23–28. doi: 10.2466/pr0.1994.75.1.23. [DOI] [PubMed] [Google Scholar]
- Feinstein BA, Goldfried MR, Davila J. The relationship between experiences of discrimination and mental health among lesbians and gay men: An examination of internalized homonegativity and rejection sensitivity as potential mechanisms. Journal of consulting and clinical psychology. 2012;80(22823860):917–927. doi: 10.1037/a0029425. [DOI] [PubMed] [Google Scholar]
- Frost DM, Meyer IH. Internalized homophobia and relationship quality among lesbians, gay men, and bisexuals. Journal of Counseling Psychology. 2009;56(1):97–109. doi: 10.1037/a0012844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold SD, Marx BP, Lexington JM. Gay male sexual assault survivors: The relations among internalized homophobia, experiential avoidance, and psychological symptom severity. Behaviour Research and Therapy. 2007;45(3):549–562. doi: 10.1016/j.brat.2006.05.006. http://dx.doi.org/10.1016/j.brat.2006.05.006. [DOI] [PubMed] [Google Scholar]
- Green KE, Feinstein BA. Substance use in lesbian, gay, and bisexual populations: an update on empirical research and implications for treatment. Psychol Addict Behav. 2012;26(2):265–278. doi: 10.1037/a0025424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: The implicit association test. Journal of personality and social psychology. 1998;74(6):1464–1480. doi: 10.1037/0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- Greenwood GL, White EW, Page-Shafer K, Bein E, Osmond DH, Paul J, Stall RD. Correlates of heavy substance use among young gay and bisexual men: The San Francisco Young Men’s Health Study. Drug Alcohol Depend. 2001;61(11137274):105–112. doi: 10.1016/s0376-8716(00)00129-0. [DOI] [PubMed] [Google Scholar]
- Grov C, Bimbi DS, Nanin JE, Parsons JT. Exploring racial and ethnic differences in recreational drug use among gay and bisexual men in New York City and Los Angeles. Journal of Drug Education. 2006;36(2):105–123. doi: 10.2190/1G84-ENA1-UAD5-U8VJ. [DOI] [PubMed] [Google Scholar]
- Halkitis PN, Fischgrund BN, Parsons JT. Explanations for methamphetamine use among gay and bisexual men in New York City. Substance Use & Misuse. 2005;40(9–10):1331–1345. doi: 10.1081/JA-200066900. [DOI] [PubMed] [Google Scholar]
- Hamilton CJ, Mahalik JR. Minority stress, masculinity, and social norms predicting gay men’s health risk behaviors. Journal of Counseling Psychology. 2009;56(1):132–141. doi: 10.1037/a0014440. [DOI] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychological Bulletin. 2009;135(19702379):707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, Fromme K. Trajectories and determinants of alcohol use among LGB young adults and their heterosexual peers: results from a prospective study. Developmental psychology. 2008;44(1):81. doi: 10.1037/0012-1649.44.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Dovidio JF, Nolen-Hoeksema S, Phills CE. An implicit measure of anti-gay attitudes: Prospective associations with emotion regulation strategies and psychological distress. Journal of Experimental Social Psychology. 2009;45(6):1316–1320. doi: 10.1016/j.jesp.2009.08.005. http://dx.doi.org/10.1016/j.jesp.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Jun HJ, Corliss HL, Austin SB. Structural stigma and sexual orientation disparities in adolescent drug use. Addictive Behaviors. 2015;46:14–18. doi: 10.1016/j.addbeh.2015.02.017. http://dx.doi.org/10.1016/j.addbeh.2015.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. doi: 10.1080/03637750903310360. [DOI] [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, Lillis J. Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy. 2006;44(1):1–25. doi: 10.1016/j.brat.2005.06.006. http://dx.doi.org/10.1016/j.brat.2005.06.006. [DOI] [PubMed] [Google Scholar]
- Hequembourg AL, Dearing RL. Exploring shame, guilt, and risky substance use among sexual minority men and women. Journal of homosexuality. 2013;60(4):615–638. doi: 10.1080/00918369.2013.760365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, Gillis JR, Cogan JC. Internalized stigma among sexual minority adults: Insights from a social psychological perspective. Journal of Counseling Psychology. 2009;56(1):32. [Google Scholar]
- Hirshfield S, Chiasson MA, Wagmiller RL, Jr, Remien RH, Humberstone M, Scheinmann R, Grov C. Sexual dysfunction in an Internet sample of U.S. men who have sex with men. The Journal Of Sexual Medicine. 2010;7(9):3104–3114. doi: 10.1111/j.1743-6109.2009.01636.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibañez GE, Purcell DW, Stall R, Parsons JT, Gómez CA. Sexual risk, substance use, and psychological distress in HIV-positive gay and bisexual men who also inject drugs. AIDS. 2005;19:S49–S55. doi: 10.1097/01.aids.0000167351.00503.92. [DOI] [PubMed] [Google Scholar]
- Igartua KJ, Gill K, Montoro R. Internalized homophobia: a factor in depression, anxiety, and suicide in the gay and lesbian population. Canadian Journal of Community Mental Health. 2003;22(2):15–30. doi: 10.7870/cjcmh-2003-0011. [DOI] [PubMed] [Google Scholar]
- Johnson AS, Hall HI, Hu X, Lansky A, Holtgrave DR, Mermin J. Trends in diagnoses of HIV infection in the United States, 2002–2011. JAMA. 2014;312(4):432–434. doi: 10.1001/jama.2014.8534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MO, Carrico AW, Chesney MA, Morin SF. Internalized heterosexism among HIV-positive, gay-identified men: implications for HIV prevention and care. Journal of Consulting Clinical Psychology. 2008;76(5):829–839. doi: 10.1037/0022-006x.76.5.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kecojevic A, Wong CF, Corliss HL, Lankenau SE. Risk factors for high levels of prescription drug misuse and illicit drug use among substance-using young men who have sex with men (YMSM) Drug and alcohol dependence. 2015;150:156–163. doi: 10.1016/j.drugalcdep.2015.02.031. http://dx.doi.org/10.1016/j.drugalcdep.2015.02.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerridge BT, Pickering RP, Saha TD, Ruan WJ, Chou SP, Zhang H, Hasin DS. Prevalence, sociodemographic correlates and DSM-5 substance use disorders and other psychiatric disorders among sexual minorities in the United States. Drug and alcohol dependence. 2017;170:82–92. doi: 10.1016/j.drugalcdep.2016.10.038. http://dx.doi.org/10.1016/j.drugalcdep.2016.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R. The impairments caused by social phobia in the general population: implications for intervention. Acta Psychiatrica Scandinavica. 2003;108(s417):19–27. doi: 10.1034/j.1600-0447.108.s417.2.x. [DOI] [PubMed] [Google Scholar]
- Klitzman RL, Greenberg JD, Pollack LM, Dolezal C. MDMA (‘ecstasy’) use, and its association with high risk behaviors, mental health, and other factors among gay/bisexual men in New York City. Drug and alcohol dependence. 2002;66(2):115–125. doi: 10.1016/s0376-8716(01)00189-2. [DOI] [PubMed] [Google Scholar]
- Langdridge D. Gay Affirmative Therapy: A theoretical framework and defence. Journal of Gay & Lesbian Psychotherapy. 2007;11(1/2):27–43. doi: 10.1300/J236v11n01_03. [DOI] [Google Scholar]
- Lea T, de Wit J, Reynolds R. Minority stress in lesbian, gay, and bisexual young adults in Australia: Associations with psychological distress, suicidality, and substance use. Archives of Sexual Behavior. 2014;43(8):1571–1578. doi: 10.1007/s10508-014-0266-6. [DOI] [PubMed] [Google Scholar]
- Lee JH, Gamarel KE, Kahler CW, Marshall BDL, van den Berg JJ, Bryant K, Operario D. Co-occurring psychiatric and drug use disorders among sexual minority men with lifetime alcohol use disorders. Drug and alcohol dependence. 2015;151:167–172. doi: 10.1016/j.drugalcdep.2015.03.018. http://dx.doi.org/10.1016/j.drugalcdep.2015.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee RS, Kochman A, Sikkema K. Internalized stigma among people living with HIV-AIDS. AIDS and Behavior. 2002;6(4):309–319. doi: 10.1023/A:1021144511957. [DOI] [Google Scholar]
- Lelutiu-Weinberger C, Pachankis JE, Golub SA, Walker JNJ, Bamonte AJ, Parsons JT. Age cohort differences in the effects of gay-related stigma, anxiety and identification with the gay community on sexual risk and substance use. AIDS and Behavior. 2013;17(22038078):340–349. doi: 10.1007/s10461-011-0070-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lick DJ, Durso LE, Johnson KL. Minority stress and physical health among sexual minorities. Perspectives on Psychological Science. 2013;8(5):521–548. doi: 10.1177/1745691613497965. [DOI] [PubMed] [Google Scholar]
- Livingston NA, Oost KM, Heck NC, Cochran BN. The role of personality in predicting drug and alcohol use among sexual minorities. Psychology of Addictive Behaviors. 2015;29(2):414–419. doi: 10.1037/adb0000034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin JL, Dean LL. Unpublished technical report. New York: Columbia University; 1988. The Impact of AIDS on Gay Men: A Research Instrument, 1988. [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12(1):23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- Mays VM, Cochran SD, Zamudio A. HIV prevention research: Are we meeting the needs of African American men who have sex with men? Journal of Black Psychology. 2004;30(1):78–105. doi: 10.1177/0095798403260265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Bostwick WB, Hughes TL, West BT, Boyd CJ. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. American Journal of Public Health. 2010;100(10):1946–1952. doi: 10.2105/AJPH.2009.163147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe SE, Boyd CJ, Cranford JA, Morales M, Slayden J. A modified version of the Drug Abuse Screening Test among undergraduate students. Journal of Substance Abuse Treatment. 2006;31(3):297–303. doi: 10.1016/j.jsat.2006.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKirnan DJ, Ostrow DG, Hope B. Sex, drugs and escape: a psychological model of HIV-risk sexual behaviours. AIDS care. 1996;8(6):655–669. doi: 10.1080/09540129650125371. [DOI] [PubMed] [Google Scholar]
- McKirnan DJ, Vanable PA, Ostrow DG, Hope B. Expectancies of sexual “escape” and sexual risk among drug- and alcohol-involved gay and bisexual men. Journal of Substance Abuse. 2001;13(1–2):137–154. doi: 10.1016/s0899-3289(01)00063-3. http://dx.doi.org/10.1016/S0899-3289(01)00063-3. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Minority stress and mental health in gay men. Journal of Health and Social Behavior. 1995;36(7738327):38–56. [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin. 2003;129(5):674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Dean L. Internalized homophobia, intimacy and sexual behaviour among gay and bisexual men. In: Herek G, editor. Stigma and Sexual Orientation. Thousand Oaks, CA: Sage Publications; 1998. pp. 160–186. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Helping people change. Guilford press; 2012. [Google Scholar]
- Mimiaga MJ, Reisner SL, Fontaine YM, Bland SE, Driscoll MA, Isenberg D, Mayer KH. Walking the line: Stimulant use during sex and HIV risk behavior among Black urban MSM. Drug and alcohol dependence. 2010;110(1–2):30–37. doi: 10.1016/j.drugalcdep.2010.01.017. http://dx.doi.org/10.1016/j.drugalcdep.2010.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morandini JS, Blaszczynski A, Ross MW, Costa DSJ, Dar-Nimrod I. Essentialist beliefs, sexual identity uncertainty, internalized homonegativity and psychological wellbeing in gay men. Journal of Counseling Psychology. 2015;62(3):413–424. doi: 10.1037/cou0000072. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Andrews R, Herrick A, Stall R, Schnarrs PW. A syndemic of psychosocial health disparities and associations with risk for attempting suicide among young sexual minority men. American Journal of Public Health. 2013;104(2):287–294. doi: 10.2105/AJPH.2013.301744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Mustanski B. Internalized homophobia and internalizing mental health problems: A meta-analytic review. Clinical Psychology Review. 2010;30(20708315):1019–1029. doi: 10.1016/j.cpr.2010.07.003. [DOI] [PubMed] [Google Scholar]
- Nicholson WD, Long BC. Self-esteem, social support, internalized homophobia, and coping strategies of HIV+ gay men. Journal of consulting and clinical psychology. 1990;58(6):873–876. doi: 10.1037/0022-006X.58.6.873. [DOI] [PubMed] [Google Scholar]
- Pachankis JE. A transdiagnostic minority stress treatment approach for gay and bisexual men’s syndemic health conditions. Archives of Sexual Behavior. 2015;44(7):1843–1860. doi: 10.1007/s10508-015-0480-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Starks TJ. The influence of structural stigma and rejection sensitivity on young sexual minority men’s daily tobacco and alcohol use. Social science & medicine. 2014;103(24507912):67–75. doi: 10.1016/j.socscimed.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Grov C, Golub SA. Sexual compulsivity, co-occurring psychosocial health problems, and HIV risk among gay and bisexual men: Further evidence of a syndemic. American Journal of Public Health. 2012;102(1):156–162. doi: 10.2105/AJPH.2011.300284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parsons JT, Lelutiu-Weinberger C, Botsko M, Golub SA. A randomized controlled trial utilizing motivational interviewing to reduce HIV risk and drug use in young gay and bisexual men. Journal of consulting and clinical psychology. 2014;82(1):9–18. doi: 10.1037/a0035311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn K, Dickson-Gomez J, DiFranceisco W, Kelly JA, St Lawrence JS, Amirkhanian YA, Broaddus M. Correlates of internalized homonegativity among black men who have sex with men. AIDS Education & Prevention. 2015;27(3):212–226. doi: 10.1521/aeap.2015.27.3.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Reisner SL, Mimiaga MJ, Bland S, Skeer M, Cranston K, Isenberg D, Mayer KH. Problematic alcohol use and HIV risk among Black men who have sex with men in Massachusetts. AIDS care. 2010;22(5):577–587. doi: 10.1080/09540120903311482. [DOI] [PubMed] [Google Scholar]
- Rosario M, Schrimshaw EW, Hunter J. A model of sexual risk behaviors among young gay and bisexual men: Longitudinal associations of mental health, substance abuse, sexual abuse, and the coming-out process. AIDS Education & Prevention. 2006;18(17067255):444–460. doi: 10.1521/aeap.2006.18.5.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario M, Schrimshaw EW, Hunter J. Disclosure of sexual orientation and subsequent substance use and abuse among lesbian, gay, and bisexual youths: Critical role of disclosure reactions. Psychology of Addictive Behaviors. 2009;23(19290704):175–184. doi: 10.1037/a0014284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safren SA, O’Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: A randomized controlled trial. Journal of consulting and clinical psychology. 2012;80(3):404–415. doi: 10.1037/a0028208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrimshaw EW, Siegel K, Downing MJ, Jr, Parsons JT. Disclosure and concealment of sexual orientation and the mental health of non-gay-identified, behaviorally bisexual men. Journal of consulting and clinical psychology. 2013;81(1):141–153. doi: 10.1037/a0031272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoptaw S, Weiss RE, Munjas B, Hucks-Ortiz C, Young SD, Larkins S, Gorbach PM. Homonegativity, substance use, sexual risk behaviors, and HIV status in poor and ethnic men who have sex with men in Los Angeles. Journal of Urban Health. 2009;86(Suppl 1(19526346)):77–92. doi: 10.1007/s11524-009-9372-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA. The drug abuse screening test Addictive Behaviors. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Snell WE. The multidimensional sexual self-concept questionnaire. In: Davis CM, Yarber WL, Bauseman R, Schreer G, Davis SL, editors. Handbook of sexuality-related measures. Newbury Park: Sage; 1998. pp. 521–524. [Google Scholar]
- Stall R, Paul JP, Greenwood G, Pollack LM, Bein E, Crosby GM, Catania JA. Alcohol use, drug use and alcohol-related problems among men who have sex with men: The Urban Men’s Health Study. Addiction. 2001;96(11):1589–1601. doi: 10.1046/j.1360-0443.2001.961115896.x. [DOI] [PubMed] [Google Scholar]
- Starks TJ, Millar BM, Tuck AN, Wells BE. The role of sexual expectancies of substance use as a mediator between adult attachment and drug use among gay and bisexual men. Drug and alcohol dependence. 2015;153:187–193. doi: 10.1016/j.drugalcdep.2015.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Traube DE, Schrager SM, Holloway IW, Weiss G, Kipke MD. Environmental risk, social cognition, and drug use among young men who have sex with men: Longitudinal effects of minority status on health processes and outcomes. Drug and alcohol dependence. 2013;127(1–3):1–7. doi: 10.1016/j.drugalcdep.2012.06.007. http://dx.doi.org/10.1016/j.drugalcdep.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner G, Brondolo E, Rabkin J. Internalized homophobia in a sample of HIV+ gay men, and its relationship to psychological distress, coping, and illness progression. Journal of homosexuality. 1997;32(2):91–106. doi: 10.1300/J082v32n02_06. [DOI] [PubMed] [Google Scholar]
- Weber GN. Using to numb the pain: Substance use and abuse among lesbian, gay and bisexual individuals. Journal of Mental Health Counseling. 2008;30(1):31–48. [Google Scholar]
- Weiss BJ, Hope DA. A preliminary investigation of worry content in sexual minorities. Journal of Anxiety Disorders. 2011;25(2):244–250. doi: 10.1016/j.janxdis.2010.09.009. http://dx.doi.org/10.1016/j.janxdis.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitski R, Jones K, Wasserman J, Smith J. Self-identification as “down low” among men who have sex with men (MSM) from 12 US cities. AIDS and Behavior. 2006;10(5):519–529. doi: 10.1007/s10461-006-9095-5. [DOI] [PubMed] [Google Scholar]


