Summary
Bile duct injuries often occur because of surgeon spatial disorientation. The psychological concept of cognitive map misplacement is a useful explanation of how this disorientation and injury occurs. Surgeons may find that using a “bile duct time out” is a helpful way to orient. Based on the mnemonic B-SAFE, they can use 5 subhepatic landmarks (B, bile duct; S, sulcus of Rouviere; A, hepatic artery; F, umbilical fissure; E, enteric/duodenum) to correctly place their cognitive map.
Despite ongoing attention, the incidence of bile duct injuries during cholecystectomy remains high. New understanding in the field of cognitive psychology offers a possible explanation and solution to this vexing problem.
Maintaining spatial orientation during surgery is an ongoing psychological task. To be safe, surgeons must identify and maintain landmarks throughout the operation. During the process of “knowing” their environment, a surgeon accumulates spatial knowledge. The construction of a cognitive map serves the organization of this knowledge. It involves a series of psychological transformations that acquire, encode, store, recall, decode and then utilize spatial information.1 A surgeons’ map is not just a simple route. It is a complex collage of information rich in meaning. It carries with it an inherent risk assessment for various areas, an understanding of tissues and how they separate, and various options for forward moves. The development of a useful cognitive map may require years of training and may then be used in a largely subconscious, intuitive way.
A surgeons’ use of cognitive maps to perform surgery has received little attention. Most cognitive map studies deal with large-scale environments; however, the principles are the same for the surgeons’ small-scale environment. The use of a cognitive map is a heuristic (mental shortcut). Surgeons may place their cognitive maps on the presenting surgical environment based on fixed landmarks. This mental imagery fills in perceptual blanks and sorts ambiguous anatomy so that the operation can proceed rapidly. Not every structure must be meticulously explored, as the map makes assumptions about their nature. However, cognitive maps are not a perfect representation of reality; they “appear to be fragmented, schematized, inconsistent and multimodal.”2 They are also subject to their own set of biases, such as remembering things being more organized than they really are.2 Placement of a cognitive map in the wrong location is an ongoing risk for every surgeon.
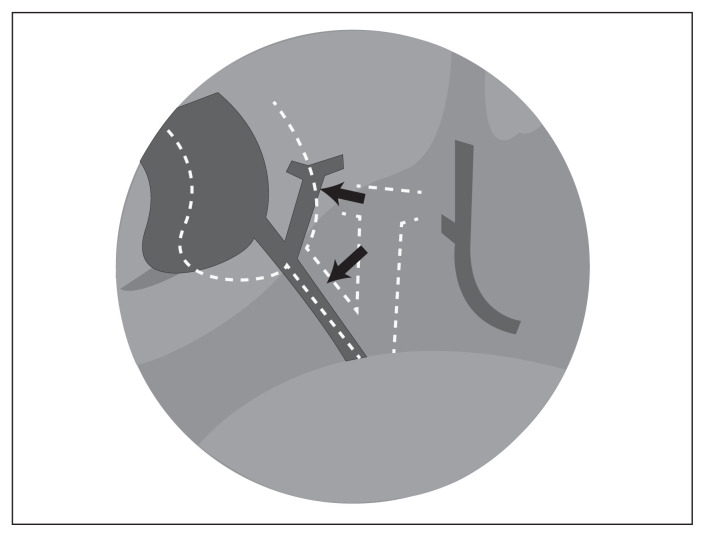
Spatial disorientation has been recognized as a major cause of bile duct injuries.3 The following of a misplaced cognitive map further explains how the error in a classical bile duct injury proceeds. Traction on the infundibulum (Hartmann pouch) may line up the common bile duct and cystic duct in the same axial plane and create an angle between the common bile duct and common hepatic duct that may appear like the angle between the cystic duct and gallbladder wall. This creates an illusion that convinces the operator to fix his or her cognitive map medially and inferiorly in the “porta hepatis” triangle rather than the hepatobiliary triangle (Fig. 1). Inflammation may obscure and close the hepatobiliary triangle; the tissues and anatomy in the porta hepatis triangle may also appear remarkably similar. The common bile duct is clipped and divided as if the cystic duct (Fig. 1, lower arrow), and the left side of the hepatic duct is followed to the liver as if it was the gallbladder wall. Cautery is then used to divide the common hepatic duct at or above the hilum as if separating the gallbladder from the liver (Fig. 1, higher arrow). It is the following of the map that results in the second division of the bile duct. The fact that this second division puts the operator back into the correct map location explains why most of these injuries are not recognized at the time of surgery.4
Fig. 1.
Retraction of the Hartmann pouch aligns the common bile duct with the cystic duct and creates a mid–bile duct angle (illusion). The surgeons’ cognitive map (dotted white lines) is placed in the “porta hepatis triangle,” and the dissection follows the map and proceeds to divide the bile duct twice (arrows).
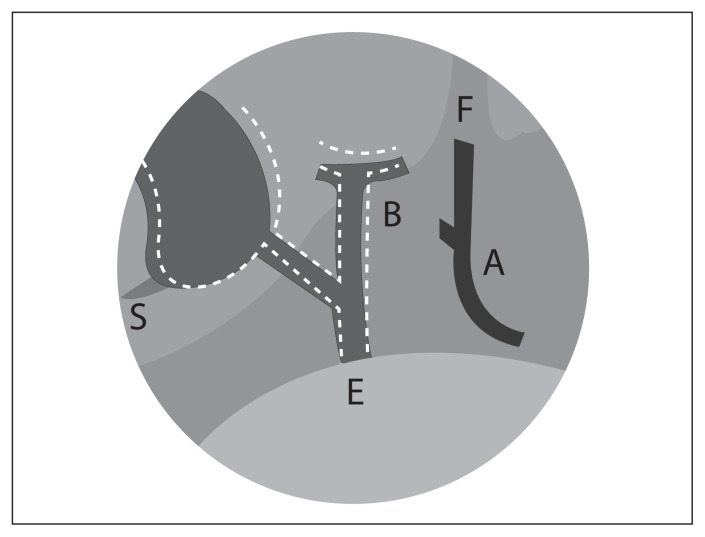
Five landmarks around the gallbladder can cue the surgeon to his or her spatial location (Fig. 2). First, the bile duct (B) itself can often be seen either just above the duodenum or at the hilum. The sulcus of Rouviere (S) in some form is usually present on the undersurface of the right side of the liver.4 The pulsations of the hepatic artery (A) can be seen on the left side of the porta hepatis. Also on the left side, the umbilical fissure (F) can be visualized. Inferiorly, one can use the enteric (E) stomach/duodenum to orient vertical position. By using these 5 landmarks — the B-SAFE mnemonic — the operator can orient in space and accurately set a cognitive map of the operation before starting.5
Fig. 2.
B-SAFE landmarks (B, bile duct; S, sulcus of Rouviere; A, hepatic artery; F, umbilical fissure; E, enteric/duodenum) to cue the surgeon to his or her spatial location.
Using timeouts is a cognitive strategy for debiasing our decisions. It is a forcing rule that, in a specific situation, makes us move from an intuitive (fast) thinking mode to a more reliable, analytic (slow) thinking mode. A bile duct time out can do this before the dissection commences and before division of any structure. The operator should stop, back the camera up, lift segment 4 of the liver and identify the 5 landmarks (B-SAFE) to be sure their map is correctly placed. It takes only seconds, and allows the surgeon to confirm spatial orientation.
Although completely eliminating bile duct injuries may be impossible, an improved understanding of the psychological basis from which surgeons operate offers new ways to improve outcome.
Footnotes
Competing interests: None declared.
Contributors: Both authors contributed substantially to the conception, writing and revision of this article and approved the final version for publication.
References
- 1.Downs RM, Stea D. Cognitive maps and spatial behavior: process and products. In: Downs RM, Stea D, editors. Image and Environment. Chicago (IL): Aldine Publishing Company; 1973. pp. 8–26. [Google Scholar]
- 2.Tversky B. Functional significance of visuospatial representation. In: Shah P, Miyake A, editors. Handbook of higher-level visuospatial thinking. Cambridge (UK): Cambridge University Press; 2005. pp. 1–34. [Google Scholar]
- 3.Way LW, Stewart L, Gantert W, et al. Causes and prevention of laparoscopic bile duct injuries: analysis of 252 cases from a human factors and cognitive psychology perspective. Ann Surg. 2003;237:460–9. doi: 10.1097/01.SLA.0000060680.92690.E9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hugh TB. New strategies to prevent laparoscopic bile duct injury-surgeons can learn from pilots. Surgery. 2002;132:826–35. doi: 10.1067/msy.2002.127681. [DOI] [PubMed] [Google Scholar]
- 5.Sutherland F, Ball C. The psychology and heuristics of bile duct injuries. In: Dixon E, Vollmer C, May G, editors. Management of benign biliary stenosis and Injury: A comprehensive guide. Toronto (ON): Springer; 2015. pp. 191–8. [Google Scholar]