Abstract
Abdominal symptoms are a hallmark of Cystic fibrosis (CF). Yet, their association with morphological abnormalities of different abdominal organs is still poorly understood. Aim was therefore to relate these symptoms, assessed with a questionnaire, to findings in abdominal ultrasound (US). In 114 CF patients of all ages, findings in US considering seventeen specific parameters were related to abdominal symptoms compiled with our novel CF-specific 26-modal symptom score (CFAbd-Score). US abnormalities were detected in 95% of the patients. Most frequent findings were pancreatic lipomatosis (88%), liver steatosis (37%), hepatomegaly (31%), and thickened bowel walls (23%). Highest burden of GI-symptoms was clearly associated with pancreatic lipomatosis (p = 0.036). In detail, patients revealing this pathology reported higher rates of abdominal pain (p = 0.018), flatulence (p = 0.006), heartburn (p = 0.04), and reflux of stomach content (p = 0.006). Patients with pancreatic sufficiency had less US-findings (p = 0.033), which in turn was associated with lower rates of abdominal symptoms. The majority of them were carriers of class IV-VI or G551D mutations. Our approach gives new insights regarding the underestimated multi-organ abdominal involvement in CF. The new score can be of high interest e.g. as a complementary tool to assess the gastrointestinal effects of promising novel CF therapeutics.
Introduction
Whereas pulmonary involvement in cystic fibrosis (CF), the most frequent autosomal recessive lethal disorder in Caucasians, has been intensively studied, the abdominal manifestations in CF are still not sufficiently understood. Abdominal manifestations, which substantially contribute to the high burden of symptoms and to preliminary death in CF, include pancreatic insufficiency (PI), focal biliary cirrhosis, micro-gallbladder with sludge and concrements, meconium ileus (MI), intestinal prolapses and intussusception and, in higher ages, distal intestinal obstruction syndrome (DIOS)1. Dysfunction of the cystic fibrosis transmembrane conductance regulator (CFTR) in the pancreatic and biliary ducts and in intestinal epithelia results in viscous acidic secretions leading to lumen obstruction and impaired digestion. The resulting deficiency of nutrients and fat-soluble vitamins, failure to thrive and reduced body weight are strongly correlated to impaired pulmonary function and reduced survival2. Ultrasound (US) has a high value for detecting abdominal pathologies non-invasively and without exposition to radiation. In our center, US has been established as routine control, performed every 6 to 12 months in CF patients. It allows static and dynamic assessment of pathologies such as pancreatic lipomatosis and cystosis, liver abnormalities, and bowel wall thickness3.
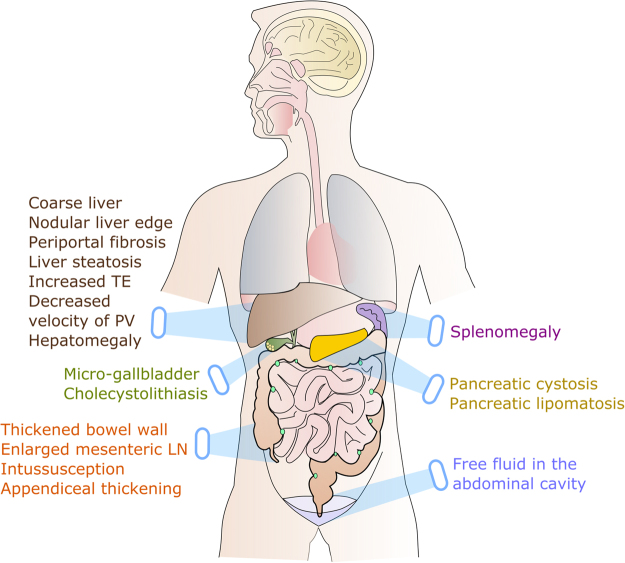
With our recently presented JenAbdomen-Score we showed that, among the complex symptoms, abdominal pain and distention, flatulence, lack of appetite and nausea, fatty stools, and diarrhea are most prominent4. Yet, the relation of these symptoms to morphological abnormalities of different abdominal organs is still poorly understood. Therefore, we recorded and quantified the complex GI symptoms with a revised, improved, and now 26-modal version of our questionnaire (CFAbd-Score) and related the calculated scores to morphological findings obtained with structured abdominal US, assessing seventeen parameters which are frequently abnormal in CF (Fig. 1).
Figure 1.
Seventeen abdominal abnormalities in cystic fibrosis detected with ultrasound. TE: transient elastography; PV: (maximal flow velocity in) portal vein; LN: lymph nodes.
Materials and Methods
Participants and Settings
The prospective study was performed consecutively including CF patients of all ages attended at the Jena University Hospital CF Center. Inclusion criteria were: (1) a diagnosis of CF determined by a sweat chloride of >60 mEq/L and/or (2) detection of 2 disease causing CFTR mutations with evidence of organ involvement. We considered patients of all ages who completed the self-reported or parent-proxy reported CFAbd-Score.
Ethical Statement
The study was approved by the Jena University ethics committee (registration number 4458-06/15) and done in adherence to ethical principles. All methods were performed in accordance with the relevant guidelines and regulations. All patients and parents of minors provided written informed consent.
Evaluation of abdominal symptoms
The CFAbd-Score was further developed from our recently presented JenaAbdomen-CF Score 1.04 with additional 9 items concerning GI symptoms-related quality of life (QoL), thus now consisting of 26 items. QoL items were: embarrassed, physical activity limitation, reduced productivity, fatigue, reduced concentration, frustrated/restless/irritable, sad, difficulty falling asleep, and waking up at night, measured with a 6-point Likert scale from ‘not at all’ (0 pts) to ‘always’ (5 pts).
In contrast to the first version, each item was reversely scored and linearly transformed to a 100-points scale (0 = 100, 1 = 80, 2 = 60, 3 = 40, 4 = 20, 5 = 0) with lower rates for increasing severity of GI symptoms. Only the domains with more than 50% of the items answered were included in the calculation. CFAbd-Score (26 items) was calculated as the sum of the items over the number of items answered in each domain.
Measurement of ultrasound abnormalities
The US examinations were performed in a single center using an ultrasound scanner (Philips; U22; Philips Healthcare, Best, the Netherlands) under standardized conditions. The findings were confirmed by and discussed with a second experienced radiologist in order to enhance the quality of the data. The abdominal US findings included evaluation of 17 parameters:
Bowel wall thickness (BWT) was measured in a longitudinal and transverse section. The measurement was taken from the central hyperechoic line of the lumen (representing the interface between content of the lumen and the mucosa) to the outer hyperechoic margin of the wall (representing the serosa). BWT was considered ‘normal’ up to 4 mm5.
Enlarged mesenteric lymph nodes were defined as greater than 5 mm in the shorter axis and larger than 10 mm in the long axis5.
Intussusception was defined as the invagination of a proximal segment of the intestine into an adjacent distal segment. In US, it appears as a mass with multiple concentric rings or doughnut signs on the short axis5.
Appendiceal thickening was defined as a diameter of more than 6 mm and/or an appendiceal wall thicker than 2 mm6.
Free fluid within the peritoneal cavity.
Pancreatic cystosis was defined as anechoic structures which are usually round and oval (cystic lesions) with sizes greater than 1 cm (macroscopic cysts)7.
Pancreatic lipomatosis was given when pancreatic echogenicity was partially or completely higher than liver (or the kidney in case of liver hyperechogenity)8.
Cholecystolithiasis was demonstrated by typical acoustic shadow in the gallbladder.
Micro-gallbladder was defined as less than 2–3 cm long and 0.5–1.5 cm wide9.
Coarseness of the hepatic parenchyma,
nodularity of the liver edge, and
periportal fibrosis (increased periportal echoes) were documented according to a scoring system established by Williams et al.10.
Liver steatosis criteria were increased echogenicity compared to renal parenchyma, vascular blurring, and deep attenuation of the US signal11.
The maximum velocity of flow in the portal vein (PV) was measured in cm/s and was considered decreased below 15 cm/s12.
Transient elastography (TE) was measured in kPa and was considered increased with a value above 7.1 kPa13.
Hepatomegaly was indicated when the liver span at the mid-clavicular line exceeded the upper limits according to height14.
Splenomegaly was indicated when spleen length (measured as the larger diameter through the hilum in a cranio-caudal axis) exceeded the upper limits according to age15.
These 17 parameters were scored either as absent (0 pts) or present (1 pt) with a maximal score of 17 points (US-17). In addition to US-17, the Williams score10 and TE were correlated separately to the CFAbd-Score.
In order to link the pancreatic status (pancreas sufficiency = PS/pancreas insufficiency = PI) to US abnormalities, doses of substituted enzymes quantified as intake of international units of pancreatic lipase per kg of body weight and day (IU/kg/d) were additionally factored in.
Measures of clinical data
The recently established pancreatic insufficiency prevalence (PIP) scores adapted from Ooi were used to measure the severity of specific CFTR mutations in regard to pancreatic function16. Patients carrying mutations which had not been included into the study from Ooi could not be attributed to a specific PIP score and thus were excluded from the PIP-genotype analysis (12/114 patients). CFTR-mutations were classified as I-III (severe) and IV-V (mild)17. An adequate visualization of the pancreas by US was present in 92% of the patients (105/114). TE could be performed in 99 of the 114 patients. CF-liver disease (CFLD) was defined according to Debray et al.18.
Data Analysis
Statistical analyses were performed using SPSS v.23.0. Median, lower (Q1) and upper (Q3) interquartiles of the score in relation to the respective US parameter are given as median [Q1;Q3]. To detect statistical differences between the US findings-associated symptom scores, Mann-Whitney-U test was chosen following Kolmogorov-Smirnov (K-S) testing of normal distribution. To evaluate the difference between two patient groups (e.g. PS vs. PI), the Hodges-Lehmann (HL) estimator (median of all pairwise differences) with 95% confidence interval (CI) was reported. Nominal data was compared with the Chi-square test or Fisher’s exact tests, as appropriate. Correlations between variables were examined using the Pearson’s correlation coefficient. A p-value ≤ 0.05 indicates a significant difference or correlation.
Results
One-hundred fourteen patients (52.6% females) were enrolled prospectively. The mean age was 19.8 ± 13.6 (1–75) years. Exocrine PI was present in 106 patients (93%, Table 1) at time of inclusion, 8 patients were PS and 9 patients (8%) had undergone bowel resection. CFTR mutations were identified on both alleles in all patients.
Table 1.
Characteristics of the included CF patients (n = 114).
| Variable | N (%) | |
|---|---|---|
| Sex | Female | 61 (52.6%) |
| Male | 53 (47.4%) | |
| Genotype | F508del/F508del | 48 (42.1%) |
| F508del/other | 53 (46.5%) | |
| G551D/other | 15 (13.0%) | |
| Other/other | 13 (10.7%) | |
| Age (yrs.) | 0–5 | 17 (14.9%) |
| 6–11 | 25 (21.9%) | |
| 12–17 | 14 (12.3%) | |
| ≥18 | 58 (50.9%) | |
| Therapy | Antibiotic therapy in the previous 3 months | 84 (73.7%) |
| Pancreatic enzymes intake | 107 (93.9%) | |
| Proton pump inhibitors (PPI) | 30 (36.3%) | |
| Comorbidities | Exocrine pancreatic insufficiency (EPI) | 106 (93.0%) |
| Meconium ileus (MI) | 9 (7.9%) | |
| Distal intestinal obstruction syndrome (DIOS) | 11 (9.6%) | |
| Rectal prolapse | 13 (11.4%) | |
| CF liver disease (CFLD) | 21 (18.4%) | |
| Small bowel resection | 9 (7.9%) | |
| Serum | Elevated† ALT | 60 (52.6%) |
| Elevated† AST | 25 (21.9%) | |
| Elevated† γ-GT | 12 (10.5%) | |
| Elevated† AP | 48 (42.1%) | |
| Platelet counts reduced | 5 (4.4%) |
†Elevated in regard to age and gender-related reference.
ALT: alanine aminotransferase; AST: aspartate aminotransferase; γ-GT: γ-glutamyl transpeptidase;
and AP: alkaline phosphatase.
Relation of US-findings to symptoms assessed with the CFAbd-Score
Ultrasound abnormalities detected in the included CF patients are listed in Table 2 and Fig. 2. Altogether, patients with pancreatic lipomatosis detected by abdominal US revealed lower values for CFAbd-Score (84 [76;91] vs. 94 [81;95]; p = 0.036) according to a higher burden of symptoms than those without pancreatic lipomatosis. In detail, they reported a higher burden of abdominal pain (AP) frequency (HL = 20 pts, 95% CI [0;20]; MWW p = 0.018), AP duration (HL = 0 pts, 95% CI [0;20]; MWW p = 0.046), and AP intensity (HL = 20 pts, 95% CI [10;30]; MWW p = 0.002) as well as flatulence (HL = 20 pts, 95% CI [0;20]; MWW p = 0.006), heartburn (HL = 0 pts, 95% CI [0;20]; MWW p = 0.04), and reflux of stomach content (HL = 0 pts, 95% CI [0;20]; MWW p = 0.006) (Supplementary Table S1). Furthermore, patients with micro-gallbladder detected in US reported higher rates of pain during bowel movements (HL = 10 pts, 95% CI [0;10]; MWW p = 0.014) whereas patients with liver steatosis more frequently suffered from fatty stools (HL = 0 pts, 95% CI [0;20]; MWW p = 0.031). At the same time, we did not detect significant differences in the CFAbd-Score with thickened bowel walls (n = 26/114), enlarged mesenteric lymph nodes (n = 10/114), appendiceal thickening (n = 7/114), free abdominal fluid (n = 11/114), pancreatic cystosis (n = 6/105), hepatic parenchymal abnormalities such as coarse/irregular parenchyma (n = 25/114), nodular liver edge (n = 7/114), periportal fibrosis (n = 19/114), as well as hepatomegaly (n = 35/114), splenomegaly (n = 12/114), decreased velocity of PV (n = 11/114) and increased TE (n = 7/99). Cholecystolithiasis (n = 3/114) and intussusception (n = 2/114) were not evaluated because of the small number of patients with these pathologies detected in US. In general, CFAbd-Score did not correlate with US-17 scores (r = 0.01; p = 0.92), maximum velocity of PV (r = 0.17; p = 0.08), TE values (r = 0.17; p = 0.09), or the Williams score (r = 0.02; p = 0.86).
Table 2.
Frequencies of detected abnormalities in abdominal ultrasound (US-17).
| Pathologies detected by abdominal US | N (%) |
|---|---|
| Pancreatic lipomatosis† | 92/105 (88) |
| Liver steatosis | 42/114 (37) |
| Hepatomegaly | 35/114 (31) |
| Thickened bowel wall (>4 mm) | 26/114 (23) |
| Coarse/irregular hepatic parenchyma | 25/114 (22) |
| Micro-gallbladder | 24/114 (21) |
| Periportal fibrosis | 19/114 (17) |
| Splenomegaly | 12/114 (11) |
| Free fluid in the abdominal cavity | 11/114 (10) |
| Decreased velocity of PV | 11/114 (10) |
| Enlarged mesenteric lymph nodes | 10/114 (9) |
| Increased TE* | 7/ 99 (7) |
| Appendiceal thickening | 7/114 (6) |
| Nodular liver edge | 7/114 (6) |
| Pancreatic cystosis† | 6/105 (6) |
| Cholelithiasis | 3/114 (3) |
| Intussusception | 2/114 (2) |
†Pancreas was adequately visualized in 105 of the 114 patients.
*Transient elastography (TE) was performed in 99 of the 114 patients.
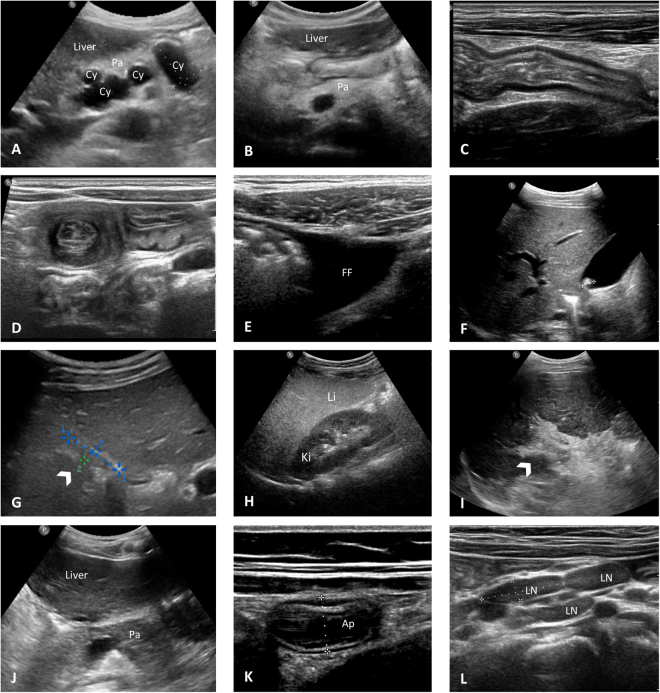
Figure 2.
Specific US abnormalities identified in the Jena University CF cohort. (A) Pancreatic cystosis in an asymptomatic 41-year-old female patient heterozygous for G551D showing a hyperechoic pancreas (Pa) containing multiple cysts (Cy) with sizes approximately of 21 × 34 × 20 mm and 21 × 40 × 24 mm. CFAbd-Score: 82 (*range: highest burden of symptoms [0 points] to no symptoms [100 points], respectively). (B) Hyperechoic pancreas (Pa) with fat replacement as typical for pancreatic lipomatosis in a 10-year-old female patient homozygous for F508del with pancreatic insufficiency (symptom score: 95). (C) Longitudinal US image of the bowel wall in the terminal ileum measuring approximately 5 mm in a context of thickened bowel wall in a 19-year-old patient homozygous for F508del (symptom score: 81). (D) Transversal section of the small bowel showing the classic target sign appearance of intussusception in a 3-year-old female asymptomatic patient homozygous for F508del (symptom score: 96). (E) Free fluid (FF) in the right lower quadrant in a 32-year-old male patient homozygous for F508del with severe liver disease (symptom score: 80). (F) Single gallstone in a 12-year-old male asymptomatic patient heterozygous for G551D (symptom score: 100). (G) Gallbladder (arrow) in a 11-year-old female patient heterozygous for G551D measuring 18 × 4 mm in a context of micro-gallbladder (symptom score: 88). (H) US image of liver steatosis in a 4-year-old male patient homozygous for F508del, showing diffused increased echogenicity of the right lobe of the liver (Li) relative to right kidney cortex (Ki) (symptom score: 85). I) Severe periportal fibrosis (arrow) in a 28-year-old male patient heterozygous for F508del/R347P with cystic fibrosis liver disease (CFLD) (symptom score: 87). (J) Isoechoic pancreas (Pa) relative to liver in a 18 year-old female patient heterozygous for G551D with pancreatic sufficiency (PS) in longitudinal sonogram at level of the pancreatic head (symptom score: 99). (K) US scan of the appendix (Ap) in a 10-year-old asymptomatic female patient homozygous for F508del. Note the thickened aspect of the appendix (diameter of 9 mm) (symptom score: 95). (L) Enlarged mesenteric lymph nodes (LN) greater than 18 mm in the larger axis in a 10-year-old asymptomatic patient homozygous for F508del, in a context of an inflammatory etiology (symptom score: 95).
Furthermore, we did not find differences in US-17 between sexes. Altogether, only 5.3% of the included CF patients (6/114) did not reveal any pathological US-finding, which in part also could have been caused by superposition of the pancreas or other organs with bowel gases (minimal abdominal US). Moreover, enzyme dose was not related to US abnormalities (Supplementary Table S2).
US-findings in relation to the pancreatic status
Comparison of ultrasound findings between PS and PI patients revealed pancreatic lipomatosis in 75% vs. 91%, (p = 0.034) and liver steatosis in 13% vs. 42% of patients, respectively (p = 0.021) (Supplementary Table S3). Accordingly, pancreatic sufficient patients showed an overall lower frequency of US-findings compared with patients with PI (1.5 [0;2] vs. 3 [2;4]; p = 0.033).
Correlations between CFTR genotype and ultrasound findings (US-17)
The number of US findings (US-17) showed a weak positive correlation with the PIP-score (r = 0.26; p < 0.01). Patients carrying at least one class IV to VI mutation revealed lower rates of pathologies in US-17 than patients carrying class I to III mutations (1 [1;2] vs. 3 [2;4]; p = 0.004). Thereby, patients carrying a G551D mutation (≈13% of the CF patients attended in the Jena University CF center) showed a lower number of US findings (US-Score) compared to those without this mutation (2 [1;3] vs. 3 [2;5]; p = 0.018). However, 8/15 of these patients received ivacaftor at the time of inclusion, so that we cannot determine whether this outcome is primary for patients with a G551D mutation or secondary due to therapy with the potent CFTR modulator.
Discussion
To our knowledge, this is the first study correlating the wide range of different findings in abdominal ultrasound in CF patients with the range of typical abdominal symptoms assessed with a second, revised version of our CF-specific score (CFAbd-Score). Thereby, we queried frequency, duration, and intensity of symptoms together with the related burden for the patient’s daily life. By using US measures we found that particularly pancreatic lipomatosis is associated with an increased abdominal symptom load. Altogether, pancreatic lipomatosis was detected in 88% (92/105) of the included CF patients. Overall, this accords well to the pancreatic status, as the majority of the included CF patients with pancreatic lipomatosis were pancreas insufficient (PI) (91%), and these US changes are a common finding in this subgroup13,19. By means of serial radiology, four states have been revealed in the course of the progression from PS to PI: normal pancreas, an atrophic state subsequent to recurrent pancreatitis, a lipomatous state in which pancreatic tissue is successively replaced by fat-dense tissue, and a macro- or microcystic pancreas with parietal calcifications20. Finally, many patients who initially were classified as PS will become PI. The finding of lipomatosis in our PS patients indicates an advanced stage in the progression from PS to PI. On the basis of a first and preliminary version of our score (JenAbdomen-CF Score 1.0) we demonstrated that PI-CF patients report significantly more GI symptoms compared to PS-CF patients4. A recent study using a symptom questionnaire developed as PI-specific patient-reported outcome measure (PROM) revealed that 84% of the patients reported experiencing abdominal pain21. This is quite similar to our finding that 79% of our CF patients (92% PI) recurrently and regularly suffer from abdominal pain. The most frequent locations of abdominal pain were the umbilical (83%) and epigastric regions (11%)4. Our finding on the impact of a pancreatic lipomatosis fits very well with the patients´ statements. The elevated rate of GI symptoms in PI patients may be caused by the combination of exocrine pancreatic deficiency to liberate enzymes, the failure to neutralize the acidic gastric contents, and intestinal inflammation22. Nevertheless, this finding should be taken carefully, as a smaller number of patients with elevated pancreatic echogenicity quoted as pancreatic lipomatosis still maintain residual pancreatic function according to a PS phenotype and vice versa. At the same time, US revealing a hypoechoic pancreas, which does not accord to pancreatic lipomatosis, could represent a fibrotic pancreas, as found in patients with PI19. However, these cases accounted for a minority of our cohort.
Interestingly, prominent US findings such as pancreatic cystosis, which was detected in 6/105 patients (6%), with cyst lesions measuring up to 40 mm did not significantly contribute to the burden of abdominal symptoms in these patients. However, this specific pathology might cause symptoms later, e.g. when further growth of cysts compress surrounding structures, as described in a single case report by deGruchy et al.: the 9 year old patient with pancreatic cystosis suffered from intense radiating abdominal pain23. Previously, Dietrich et al. reported that abdominal US reveals small pancreatic cysts with a mean diameter of 18 mm (7–27 mm) in up to 18% of CF patients (n = 12/67)9.
Thickened bowel walls, as detected in 26 of 114 patients (23%) of our CF cohort, were not significantly correlated with an increased burden of GI symptoms. Thereby, until now, etiology of bowel wall thickening in CF is not fully understood. A relation to intestinal inflammation, and possibly to dysbiosis has been discussed and also that in the long run it could lead to segmental submucosal fibrosis24. However, this assumption needs further evaluation in future studies. As previously reported, the dose of applied pancreatic enzymes did not correlate with the presence of thickened bowel walls24, even though such a correlation was discussed25.
The presence of an enlarged appendix was observed in 7 of the included CF patients (6%). This finding was not related to an increased burden of GI symptoms. Apparently, patients remain asymptomatic until occurrence of an appendiceal perforation or abscess formation6. Altogether, the appendix in CF has been reported to be usually filled with mucoid contents, which maintain the appendiceal lumen distended and less prone to total luminal occlusion and acute inflammation. Consequently, progress to acute appendicitis in CF appears to be rare, occurring in only 1–2% of patients26.
As suspected, hepatic abnormalities including coarse parenchyma, nodular edges, periportal fibrosis, organomegaly, increased TE, and decreased PV velocity was not correlated with an increased burden of GI symptoms. However, symptoms like upper GI hemorrhage and tarry stools may manifest with end-stage liver disease27. Such an acute hepatic decompensation, which is often associated with metabolic disorders, is rare and did not occur in our observational period.
In the present study, 42 patients (37%) revealed sonographic signs of liver steatosis, which is in accordance with previous ultrasound studies reporting steatosis in 23–75% of CF patients28. The most common abdominal symptom found in that subgroup was ‘fatty stools´, which was significantly more frequent in this group (p = 0.031). Interestingly, 41 out of these 42 patients were PI. As recently published, patients who underwent pancreatectomy are likely to develop hepatosteatosis due to maldigestion. This largely depended on the endo- and exocrine function of the remnant pancreas and a well-adjusted enzyme supplementation29. In non-CF patients, hepatosteatosis is closely linked to an impaired glucose metabolism30. It is conceivable that also in CF the development of a liver steatosis is promoted by insulin deficiency due to pancreatic insufficiency. Once in progress, the situation is worsened by an inadequate synthesis of hepatic phosphatidylcholine and apolipoprotein B, which results in impaired VLDL assembly and, subsequently, disturbed removal of triacylgycerols from the liver1,31,32. Moreover, deficiency of essential fatty acids and carnitine are factors discussed in the context of hepatosteatosis in CF33.
Enlarged abdominal lymph nodes, consistently with a reactive morphology, were detected in 10 of our patients (9%). This finding was not associated with elevated GI symptomatology. Likewise, detection of gallstones (found in 3% of patients) was not related to elevated symptoms. However, it is not unlikely to give rise to symptoms in the course of time.
Interestingly, PS patients carrying a mild genotype (class IV-VI) as well as patients with a G551D mutation had significantly lower rates of US abnormalities (US-17) compared to patients with class I-II mutations and PI, respectively. As a limitation, 8 of the 15 patients carrying a G551D mutation were treated with ivacaftor (IVA) at the time of inclusion. With higher patient numbers, it would be most interesting to assess changes of abdominal symptoms due to introduction of the potent CFTR modulator. According to recent publications, IVA improved many of the abdominal pathologies such as a hyperacidic gastric content and liver steatosis, and even restored exocrine pancreatic function to some extent in some patients34–36. Even more impressive, improvement of GI symptoms was observed in CF patients treated with orkambi, the combination of the CFTR corrector lumacaftor and the potentiator IVA, which was recently approved for CF patients homozygous for F508del in many countries. Here is where a differential score assessing the multimodal abdominal involvement in CF is of outstanding interest to sufficiently document and quantify such interesting effects. This would be one of many interesting fields for the application of a score like the present CFAbd-Score, which could bring substantial new insights as a PROM. As previously mentioned, the validation of this PROM is still in progress and, just like the JenAbdomen-CF Score 1.0, the second version presented herein is preliminary4. Nevertheless, we show that especially pancreatic lipomatosis was well reflected by self-reported elevated GI-symptoms. Our data may contribute to the still little understanding of the abdominal involvement in CF.
Electronic supplementary material
Acknowledgements
The authors especially thank the patients who participated in this study. This research was supported by the German Academic Exchange Service (DAAD, Grant: 57130097) to HT. The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author Contributions
Conceptualization: H.T., J.G.M., C.A. Funding acquisition: H.T., J.G.M. Project administration: C.A., A.J., J.G.M. Recruitment: J.G.M., M.L., R.K.M., Investigation: H.T., J.G.M., D.M.R., M.L., R.K.M. Data acquisition: D.M.R., H.T., C.A. Formal analysis: H.T., A.J., T.L. Resources: J.G.M., H.J.M. Supervision: J.G.M., H.J.M. Draft writing - original draft: H.T., A.J., J.G.M. Drawing: H.T., A.J.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Harold Tabori, Anke Jaudszus, Diane M. Renz and Jochen G. Mainz contributed equally to this work
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-017-17302-4.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kelly T, Buxbaum J. Gastrointestinal Manifestations of Cystic Fibrosis. Digestive diseases and sciences. 2015;60:1903–1913. doi: 10.1007/s10620-015-3546-7. [DOI] [PubMed] [Google Scholar]
- 2.Steinkamp G, Wiedemann B. Relationship between nutritional status and lung function in cystic fibrosis: cross sectional and longitudinal analyses from the German CF quality assurance (CFQA) project. Thorax. 2002;57:596–601. doi: 10.1136/thorax.57.7.596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Liong SY, Awad D, Jones AM, Sukumar SA. The adult cystic fibrosis patient with abdominal pain: what the radiologist needs to know. Clinical radiology. 2011;66:132–139. doi: 10.1016/j.crad.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Tabori H, et al. Abdominal symptoms in cystic fibrosis and their relation to genotype, history, clinical and laboratory findings. PloS one. 2017;12:e0174463. doi: 10.1371/journal.pone.0174463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maconi, G., Bianchi Porro G (eds.). Ultrasound of the Gastrointestinal Tract., (Springer-Verlag, 2013).
- 6.Lardenoye SW, Puylaert JB, Smit MJ, Holscher HC. Appendix in children with cystic fibrosis: US features. Radiology. 2004;232:187–189. doi: 10.1148/radiol.2321030363. [DOI] [PubMed] [Google Scholar]
- 7.Berrocal T, Pajares MP, Zubillaga AF. Pancreatic cystosis in children and young adults with cystic fibrosis: sonographic, CT, and MRI findings. AJR. American journal of roentgenology. 2005;184:1305–1309. doi: 10.2214/ajr.184.4.01841305. [DOI] [PubMed] [Google Scholar]
- 8.Worthen NJ, Beabeau D. Normal pancreatic echogenicity: relation to age and body fat. AJR. American journal of roentgenology. 1982;139:1095–1098. doi: 10.2214/ajr.139.6.1095. [DOI] [PubMed] [Google Scholar]
- 9.Dietrich, C. F. et al. Sonographic findings of the hepatobiliary-pancreatic system in adult patients with cystic fibrosis. Journal of ultrasound in medicine: official journal of the American Institute of Ultrasound in Medicine 21, 409–416; quiz417 (2002). [DOI] [PubMed]
- 10.Williams SG, et al. An ultrasound scoring system for the diagnosis of liver disease in cystic fibrosis. Journal of hepatology. 1995;22:513–521. doi: 10.1016/0168-8278(95)80444-7. [DOI] [PubMed] [Google Scholar]
- 11.Williams CD, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140:124–131. doi: 10.1053/j.gastro.2010.09.038. [DOI] [PubMed] [Google Scholar]
- 12.Kuo CH, Changchien CS, Tai DI, Chen JJ. Portal vein velocity by duplex Doppler ultrasound as an indication of the clinical severity of portal hypertension. Changgeng yi xue za zhi. 1995;18:217–223. [PubMed] [Google Scholar]
- 13.Friedrich-Rust M, et al. Non-invasive measurement of liver and pancreas fibrosis in patients with cystic fibrosis. Journal of cystic fibrosis: official journal of the European Cystic Fibrosis Society. 2013;12:431–439. doi: 10.1016/j.jcf.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 14.Lawson EE, Grand RJ, Neff RK, Cohen LF. Clinical estimation of liver span in infants and children. American journal of diseases of children (1960) 1978;132:474–476. doi: 10.1001/archpedi.1978.02120300034005. [DOI] [PubMed] [Google Scholar]
- 15.Rosenberg HK, et al. Normal splenic size in infants and children: sonographic measurements. AJR. American journal of roentgenology. 1991;157:119–121. doi: 10.2214/ajr.157.1.2048509. [DOI] [PubMed] [Google Scholar]
- 16.Ooi CY, et al. Type of CFTR mutation determines risk of pancreatitis in patients with cystic fibrosis. Gastroenterology. 2011;140:153–161. doi: 10.1053/j.gastro.2010.09.046. [DOI] [PubMed] [Google Scholar]
- 17.Ahmed N, et al. Molecular consequences of cystic fibrosis transmembrane regulator (CFTR) gene mutations in the exocrine pancreas. Gut. 2003;52:1159–1164. doi: 10.1136/gut.52.8.1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Debray D, Kelly D, Houwen R, Strandvik B, Colombo C. Best practice guidance for the diagnosis and management of cystic fibrosis-associated liver disease. Journal of cystic fibrosis: official journal of the European Cystic Fibrosis Society. 2011;10(Suppl 2):S29–36. doi: 10.1016/S1569-1993(11)60006-4. [DOI] [PubMed] [Google Scholar]
- 19.Engjom T, et al. Ultrasound echo-intensity predicts severe pancreatic affection in cystic fibrosis patients. PloS one. 2015;10:e0121121. doi: 10.1371/journal.pone.0121121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feigelson J, et al. Imaging changes in the pancreas in cystic fibrosis: a retrospective evaluation of 55 cases seen over a period of 9 years. Journal of pediatric gastroenterology and nutrition. 2000;30:145–151. doi: 10.1097/00005176-200002000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Johnson CD, et al. Qualitative Assessment of the Symptoms and Impact of Pancreatic Exocrine Insufficiency (PEI) to Inform the Development of a Patient-Reported Outcome (PRO) Instrument. The patient. 2017 doi: 10.1007/s40271-017-0233-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hart PA, Conwell DL. Challenges and Updates in the Management of Exocrine Pancreatic Insufficiency. Pancreas. 2016;45:1–4. doi: 10.1097/MPA.0000000000000457. [DOI] [PubMed] [Google Scholar]
- 23.deGruchy S, Lee EY. Pancreatic cystosis in a child with cystic fibrosis. Pediatric radiology. 2008;38:1142. doi: 10.1007/s00247-008-0968-9. [DOI] [PubMed] [Google Scholar]
- 24.Dialer I, Hundt C, Bertele-Harms RM, Harms HK. Sonographic evaluation of bowel wall thickness in patients with cystic fibrosis. Journal of clinical gastroenterology. 2003;37:55–60. doi: 10.1097/00004836-200307000-00014. [DOI] [PubMed] [Google Scholar]
- 25.Smyth RL. Fibrosing colonopathy in cystic fibrosis. Archives of disease in childhood. 1996;74:464–468. doi: 10.1136/adc.74.5.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shields MD, Levison H, Reisman JJ, Durie PR, Canny GJ. Appendicitis in cystic fibrosis. Archives of disease in childhood. 1991;66:307–310. doi: 10.1136/adc.66.3.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Colombo C. Liver disease in cystic fibrosis. Current opinion in pulmonary medicine. 2007;13:529–536. doi: 10.1097/MCP.0b013e3282f10a16. [DOI] [PubMed] [Google Scholar]
- 28.Flass T, Narkewicz MR. Cirrhosis and other liver disease in cystic fibrosis. Journal of cystic fibrosis: official journal of the European Cystic Fibrosis Society. 2013;12:116–124. doi: 10.1016/j.jcf.2012.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hata T, et al. Clinical Characteristics and Risk Factors for the Development of Postoperative Hepatic Steatosis After Total Pancreatectomy. Pancreas. 2016;45:362–369. doi: 10.1097/MPA.0000000000000462. [DOI] [PubMed] [Google Scholar]
- 30.Lewis JR, Mohanty SR. Nonalcoholic fatty liver disease: a review and update. Digestive diseases and sciences. 2010;55:560–578. doi: 10.1007/s10620-009-1081-0. [DOI] [PubMed] [Google Scholar]
- 31.Vaughan WJ, Lindgren FT, Whalen JB, Abraham S. Serum lipoprotein concentrations in cystic fibrosis. Science (New York, N.Y.) 1978;199:783–786. doi: 10.1126/science.203033. [DOI] [PubMed] [Google Scholar]
- 32.Grothe J, et al. Plasma phosphatidylcholine alterations in cystic fibrosis patients: impaired metabolism and correlation with lung function and inflammation. Cellular physiology and biochemistry: international journal of experimental cellular physiology, biochemistry, and pharmacology. 2015;35:1437–1453. doi: 10.1159/000373964. [DOI] [PubMed] [Google Scholar]
- 33.Treem WR, Stanley CA. Massive hepatomegaly, steatosis, and secondary plasma carnitine deficiency in an infant with cystic fibrosis. Pediatrics. 1989;83:993–997. [PubMed] [Google Scholar]
- 34.Hayes D, Jr., Warren PS, McCoy KS, Sheikh SI. Improvement of hepatic steatosis in cystic fibrosis with ivacaftor therapy. Journal of pediatric gastroenterology and nutrition. 2015;60:578–579. doi: 10.1097/MPG.0000000000000765. [DOI] [PubMed] [Google Scholar]
- 35.Rowe SM, et al. Clinical mechanism of the cystic fibrosis transmembrane conductance regulator potentiator ivacaftor in G551D-mediated cystic fibrosis. American journal of respiratory and critical care medicine. 2014;190:175–184. doi: 10.1164/rccm.201404-0703OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elborn JS, et al. Efficacy and safety of lumacaftor/ivacaftor combination therapy in patients with cystic fibrosis homozygous for Phe508del CFTR by pulmonary function subgroup: a pooled analysis. The Lancet. Respiratory medicine. 2016;4:617–626. doi: 10.1016/S2213-2600(16)30121-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.