Abstract
Purpose
To determine patients’ and parents’ perceptions of transitioning education as well as their attitudes and perceived barriers to transfer to adult oriented care.
Methods
A self-report survey was administered to patients (16–25 years old) with various childhood onset chronic diseases. A similar survey was administered to their parents/guardians.
Results
A total of 155 patients and 104 parents participated in the study. The mean age of patients was 18.9±2.3 years; 57% were female. Although most patients and parents reported receiving information and training about their medical condition, significant gaps in “transitioning education” were identified. These included stated deficiencies in education regarding unprotected intercourse, health of future offspring, birth control, pregnancy, illicit drug use, and future career or vocation counseling. Commonly named barriers to transfer were emotional attachments and lack of adult medicine specialty providers; however, the majority anticipated being ready to transfer to adult oriented care by age 25 years.
Conclusion
Current transitioning education delivery appears to result in significant gaps in transfer of information and training, as perceived by patients and their parents. Standardization of transitioning education may help ensure that patients obtain the necessary skills for self-care in adulthood and successful transfer to adult oriented care.
Keywords: Health Care Transition, Self-Care Management, Pediatric onset chronic disease
The overwhelming majority of patients with pediatric onset chronic disease, such as congenital heart disease, cancer, organ transplantation, cystic fibrosis, sickle cell disease, hemophilia, diabetes and inflammatory bowel disease, are expected to live well into adulthood (1). Providing these patients with the necessary skills for healthcare self-management in adulthood is increasingly recognized as an integral component of improved quality of life, enhanced physical and emotional functioning and decreased morbidity. A recent expert consensus statement from the American Academy of Pediatrics suggests that high-quality preparation for transition should be deemed a “basic standard of care;” however, this type of effort has not had “wide spread implementation” (2). Although many clinicians believe they provide patients with transitioning (self-care management) education, most provide this type of education without a standardized approach or without the use of validated transition knowledge assessment tools (3). In addition, several studies restricted to specific pediatric chronic diseases have demonstrated a lack of patient and parental knowledge of basic components of transition education, including general disease knowledge and the need for lifelong uninterrupted health surveillance (4–9). To assess the quality of transition education and identify deficiencies in the provision of transitioning education both patients, with a variety of pediatric chronic diseases receiving care at a tertiary children’s hospital, as well as their parents were surveyed. Barriers to transfer to adult oriented medical care and perceptions of criteria for transfer readiness were also assessed.
METHODS
Survey design
A survey of patients and parents at a 396-bed tertiary care pediatric hospital was conducted. To date, this hospital does not have a strict policy regarding timing of transfer to adult oriented care. In addition, the provision of transitioning education is highly variable depending on the clinic, department and healthcare team and is usually provided informally (3). Patients 16–25 years of age with pediatric onset chronic medical conditions, as well as their parents, were invited to participate in the study. Recruitment occurred in 8 subspecialty outpatient clinics, except the oncology clinic where eligible patients and parents were invited to participate in the survey via mail due to on-site recruitment restrictions; oncology patients presenting to other outpatient clinics were recruited at those locations. Inclusion criteria were presence of a pediatric onset chronic condition that would likely require lifelong medical care surveillance, ongoing care in one of the hospital’s outpatient clinics for at least two years and parental and patient report of age-appropriate cognitive development.
Survey Tool
The survey tools were developed over a 12-month time frame through a working group of 10 clinician-researchers with an interest in health care transition together with patient advocate representation (members of the hospital based Family Advisory Council). Questions were developed based on a review of the health care transition literature, including a recent national survey (10), and guided by a survey methodologist (SZ). Consideration was given to ensure that the survey content and language was age appropriate. The final survey was piloted by members of the hospital based Teen Advisory Council.
The final patient survey tool included 30 multi-choice questions and one open-ended question which asked if there was anything else the respondents would like to share regarding the transition and transfer process. The first section of the survey covered specific questions about the delivery of health care transition education with the option to answer “yes”, “no” or “don’t know” for each question. Patients were asked to choose “yes” even if their healthcare team provided only one discussion about the transition topic. Patients were asked if their health care team had explained to them their healthcare condition and their medications and why they take them, along with potential side effects. They were asked if their healthcare team had spoken to them about the type of symptoms that require urgent evaluation the impact their disease might have on the health of their future children, as well as the risks of smoking tobacco, using illegal drugs and alcohol and the risk of unprotected sex. In addition, they were asked if their health care team had spoken to them about their future education or career. Female respondents were also asked if their healthcare team had spoken to them about birth control or the risks of becoming pregnant. The second section of the survey explored timing and barriers to transfer to adult oriented care. Patients were asked at what age they thought they would be ready to transfer to a hospital or healthcare provider that cares for adults. Patients were then asked what they perceive as barriers to transfer to a hospital or healthcare provider that cares for adults. The survey provided several potential barriers based on the review of the literature and included adult physicians not understanding their medical condition, health insurance issues as well as emotional attachment of the provider, themselves or their parent. There was also an opportunity for subjects to list other barriers that they perceived.
The parallel parent survey addressed the same questions from a parent’s perspective. It specifically asked whether the transitioning education topics listed above were being delivered to their child. As in the patient survey, parents had the open of choosing “yes”, “no” or “don’t know” and were instructed to choose “yes” even if their healthcare team provided only one discussion to their child about the transition topic. Parents were also asked at what age they thought their child would be ready to transfer to an adult hospital or adult care provider, and their perception of impediments as listed on the patient survey. The parental survey also included additional questions regarding allocation of resources. Parents were asked if they thought the hospital should provide resources to improve the delivery of self-care management education to patients and if the hospital should provide resources to streamline the transfer process. Parents provided their demographic information including their parental role, race, ethnicity, highest level of education and type of insurance. Patient age, diagnosis and gender were obtained by review of available medical records.
DATA ANALYSIS
Descriptive analyses were summarized using means and standard deviations for continuous variables and proportions for categorical variables. Demographic differences were analyzed using Pearson’s chi-square or Fisher’s exact test for categorical variables and ANOVA for continuous variables. Barriers to, and estimates of timing of the transfer of patients into adult care were ranked and differences were assessed using chi square analyses. Survey results were reported in aggregate to ensure confidentiality. A two-sided p value <0.05 was considered to indicate statistical significance. All analyses were performed using SPSS software version 18 (Chicago, IL).
A content analysis approach to the qualitative data interpretation was employed (11, 12). The free-text comments about the participants’ perceptions regarding their experiences constituted the units of analysis. The text was separated into meaning units that were condensed, summarized and labeled with a code. These codes were reviewed for similarities and differences, sorted into categories, and then studied for underlying meanings threaded through the whole as themes. The project was approved by the Boston Children’s Hospital Center for Clinical Investigation.
Results
A total of 155 patients and 104 parents agreed to study participation; 93 (76%) were patient-parent/guardian pairs. Participation rate for patients (N=132) and parents (N=83) recruited in the outpatient clinics were 97% and 93% respectively. Participation rates for oncology patients (N=23) and parents (N=21) recruited by mail the participation rate were 19% and 20% respectively. Patient and parental characteristics are displayed in Table 1. The mean age of the patients was 18.9±2.3 years; 57% were female. Most parental respondents (89%) reported that they usually brought their child to their medical visit. The majority of parents were highly educated (68% with ≥ an associate degree) and had private healthcare insurance (80%).
Table 1.
Patient and Parent Characteristics
| Parents | Patients | p value | |
|---|---|---|---|
|
| |||
| Total Responses | N=104 | N=155 | |
| Age (yrs) | |||
| Mean±SD | 18.8±2.3 | ||
|
| |||
| Gender | <0.001 | ||
|
| |||
| Female | 80% | 57% | |
|
| |||
| Patients’ Diagnosis (n, %) | 0.510 | ||
|
| |||
| Cancer | 21 (20%) | 23 (15%)* | |
| Type 1 diabetes | 10 (10%) | 25 (16%) | |
| Congenital heart disease | 13 (13%) | 21 (13%)* | |
| Juvenile rheumatoid arthritis | 10 (10%) | 20(13%) | |
| Hematologic disorder | 16 (15%) | 15 (10%) | |
| Inflammatory bowel disease | 12 (11%) | 16 (10%) | |
| Cystic fibrosis | 5 (5%) | 11 (7%) | |
| Solid organ transplant | 6 (6%) | 7 (4%) | |
| Genetic disorders | 5 (5%) | 5 (3%) | |
| Renal disease requiring dialysis | 0 (0%) | 4 (3%) | |
| Other | 6 (5%) | 9 (6%) | |
|
| |||
| Hispanic | |||
|
| |||
| Yes | 5.8% | ||
|
| |||
| Race | |||
|
| |||
| White | 86.5% | ||
|
| |||
| Education level | |||
|
| |||
| Lower than 12th grade | 3.0% | ||
| Graduated high school | 29.3% | ||
| Associate’s degree | 17.2% | ||
| Bachelor’s degree | 28.3% | ||
| Master’s/doctoral degree | 22.3% | ||
|
| |||
| Insurance | |||
|
| |||
| Private insurance | 79.8% | ||
| State Aid | 22.1% | ||
One patient had both complex congenital heart disease and cancer
Delivery of Transitioning (Self Care) Education and Assessment
A comparison of the patient and parental perceptions regarding the delivery of transitioning education can be found in Table 2. The overwhelming majority of patients and their parents perceived that education regarding the patient’s medical condition was appropriately delivered (92% and 94% respectively). However, less than half of patients and parents reported receiving any education regarding reproductive health (specifically, unprotected intercourse), impact of disease on future offspring, birth control, and risks of pregnancy. Patients were more likely than their parents to state that education regarding unprotected intercourse (43% versus 18%, p<0.001), and birth control (45% versus 23%, p=0.009) was received. Similarly, patients were more likely to indicate that education regarding the risk of alcohol (61% versus 38%, p<0.001) and illicit drug use (48% versus 34%, p=0.019) was received. Only a small number of respondents reported receiving education regarding impact of disease on future career/vocation (28% and 31% respectively).
Table 2.
A comparison of patient and parental perceptions regarding the delivery of transitioning education by their healthcare team
| Educational Topic | Patient | Parent | p value |
|---|---|---|---|
| Patient’s disease | 92% | 94% | NS |
| Patient’s medications | 90% | 100% | 0.001 |
| Medication side effects | 79% | 69% | NS |
| Symptoms requiring urgent evaluation | 77% | 79% | NS |
| Unprotected intercourse | 43% | 18% | <0.001 |
| Impact of disease on future offspring | 32% | 39% | NS |
| Birth control considerations and risk | 45% | 23% | 0.009 |
| Risk of pregnancy to patient | 33% | 31% | NS |
| Risk of alcohol to patient | 61% | 38% | <0.001 |
| Risk of tobacco use to patient | 52% | 51% | NS |
| Risk of illicit drug use to patient | 48% | 34% | 0.019 |
| Impact of disease on patient’s future education | 60% | 60% | NS |
| Impact of disease on patient’s future career/vocation | 28% | 31% | NS |
Timing of Transfer
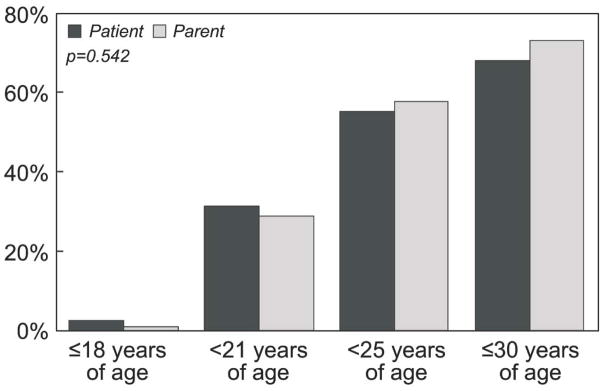
Over 50% of patients and their parents anticipated a readiness for transfer from pediatric to adult oriented care before age 25 years (56% and 58% respectively; see Figure 1). Few patients and parents stated they were unsure about the timing of readiness (17% and 15%) and 12% of patients and 9% of parents did not think that transfer readiness would be achievable regardless of age. Of note, there was no significant difference in the patients’ or their parents’ perceived readiness for transfer to adult oriented care based on the patient age, gender or diagnostic group, or the parental ethnicity, race, level of education, type of insurance or relationship to the child.
Figure 1.
Patients’ and parents’ perceived age at readiness for transfer to adult-oriented care.
Barriers to Transfer
A comparison of the patient and parental perceptions regarding the most commonly perceived barriers to transfer are found in Table 3. Emotional attachment to the patient’s base medical institution or pediatric subspecialty care provider and perceived attachment of the pediatric subspecialty provider to the patient and family were the most common identified barriers. Parents were more likely than patients to perceive parental attachment issues as barriers to transition, including to the pediatric institution (53% versus 19%, p<0.001) and pediatric provider (48% versus 23%, p<0.001). This emotional attachment did not appear to impact readiness to transfer to adult oriented care by age 25 years. Parents were more likely than their participating children to perceive the lack of adult subspecialty providers as a barrier to adult oriented care (40% versus 26%, p=0.013).
Table 3.
Barriers to adult oriented care: A comparison of patient and parental perceptions
| Perceived Barrier | Patient | Parent | p value |
|---|---|---|---|
| Patient attachment pediatric institution | 48% | 50% | NS |
| Patient attachment to the provider | 45% | 44% | NS |
| Pediatric provider attachment to patient and family | 40% | 37% | NS |
| Lack of provider in specialty | 26% | 40% | 0.013 |
| Parent attachment to the provider | 23% | 48% | <0.001 |
| Parent attachment to pediatric institution | 19% | 53% | <0.001 |
| Health insurance | 19% | 15% | NS |
Perceived barriers to adult oriented care appeared to be influenced by underlying diagnosis. Patients with congenital heart disease were far more likely to perceive a lack of adult subspecialty care providers as a barrier to adult oriented care, as compared to patients with diseases from other diagnostic group (60% versus 21%, p<0.001). Patients with cancer, inflammatory bowel disease and type 1 diabetes were more likely to note parental attachment to the pediatric medical provider as a barrier to adult oriented care when compared to other tested patient groups (44% versus 20%, p=0013; 41% versus 16%, p=0.012; 32% versus 15%, p=0.044 respectively). Female patients were more likely to identify their own attachment to their pediatric providers as a barrier to care transfer, as compared to male patients (52% versus 34%, p=0.023).
Resources
Most parents (73%) supported the allocation of resources to increase the delivery of transitioning education and assessment. Almost all (95%) parents supported the allocation of resources to improve and streamline the transfer process of patients from pediatric- to adult-oriented care.
Qualitative Results
A total of 22/166 (13%) of the patient respondents and 30/104 (29%) of the parent respondents replied to the open-ended question inviting further input regarding the transition and transfer processes. Two major themes, emerged, namely “success”, and “fear”. Both patients and their parents expressed positive feelings towards relationships developed with their pediatric providers and many described a sense of accomplishment by overcoming physical and emotional hurdles. The concept of transitioning to adult oriented care and from adolescence to adulthood was associated with some level of fear both by parents and patients. Parents were more likely to express this fear than patients and had additional concerns about “letting go” and feeling excluded from their adult child’s medical decisions because of HIPPA regulations. Some parents expressed strategies that could help alleviate their fears, such as utilizing the resources of a pediatric provider who could assist/mediate part of the effectiveness of transitioning by working together with adult providers and building patients’/parents’ transitioning support groups.
Discussion
This single-institution study assessing perceptions about transitioning education we found that adolescents and young adults with a variety of pediatric onset chronic diseases, and as well as their parents, perceived that education about their lifelong disease and its treatment were provided. However, the potential consequences of their specific disease on several aspects of their adult health were frequently perceived as lacking, in particular, issues of reproductive health, high-risk health behaviors, and employment/vocation. Emotional attachment to pediatric providers and concerns over the lack of specialty internal medicine adult providers were identified as common barriers to transfer. Nevertheless, the majority of patients and parents perceived readiness for transfer by patient age 25 years, albeit with lingering concerns and anxiety about transition. Of note, these findings were consistent among all disease groups.
Provision of Transitioning (Self-Care) Education/Assessment
Education regarding patient-specific disease appeared to be the only transitioning educational area that was perceived to be provided on a consistent basis. Patients and parents frequently perceived a lack of education related to unprotected intercourse, impact of disease on future offspring and the potential risks of birth control and pregnancy in female patients. Fewer than 50% of the patients surveyed stated that they recalled a single discussion about these topics by their subspecialty provider. This gap in education was observed across all diagnostic groups and older patients were no more likely to perceive this education than younger patients. This reported lack of education is consistent with previously published reports in patients with congenital heart disease and in childhood cancer survivors (13, 14). This reported lack of education, if representative of true lack of successful transfer of health-related information, could have deleterious consequences since many patients with pediatric onset chronic diseases are at increased risk of maternal and fetal adverse events during pregnancy (15). Patients may be at increased risk for anomalies in their offspring, and counseling and education may assist both in guiding parental oversight and pregnancy. Moreover, some lifelong diseases or their associated therapies can result in infertility; counseling regarding specific adversities can help effected individuals better understand the longer-term implications of therapeutic choices made during times of acute or sub-acute medical worsening (16, 17).
Education regarding contraception, pregnancy risk, and the impact of disease on offspring appears essential to ensuring that patients are equipped with the necessary information to make informed decisions about their bodies and their future. Data suggest that these conversations need to begin in early adolescence, since nearly 50% of adolescents in the general population have engaged in sexual intercourse (18). Adolescents with pediatric onset disorders appear to follow similar general population trends; as 28% of sickle cell patients and 51% of cystic fibrosis patients between the ages of 12 to 19 years have been shown to be engaging in sexual intercourse (19).
Education regarding high-risk behaviors such as alcohol, tobacco and illicit drug use were reported by approximately half of the patients. Previous studies suggest that patients with pediatric onset chronic disease do participate in high-risk activities, with behavioral patterns that are often similar to the general population. (20, 21). Primary care providers can give general counsel regarding these behaviors, but specialist involvement may be important because high-risk activities may have implications for the chronic disease or its treatment that are better known to the subspecialty team.
The patients and parents in this study frequently reported not receiving education regarding the impact of disease on future education and career/vocation. While primary care providers also need to ensure that conversations occur that help patients and their families with “envisioning a future” (22), specialty clinicians may have unique perspectives regarding the realistic capabilities or individuals with specific chronic conditions.
Perceived Readiness and Barriers to Transfer to Adult Oriented Care
Patients and parents expressed a spectrum of views regarding readiness to transfer to adult oriented care, with no detectable trend based on age, gender or diagnostic group. Despite the call for transfer from pediatric to adult oriented care by age 21 years by many institutions, nearly ¾ of the patients and parents in our study did not believe they would be ready to transfer by this age. However, more than half envisioned readiness for transfer before age 25 years. A slightly older age at transfer may improve readiness for transfer but many adolescents feel that age should not be the only determinant (23). The addition of a more objective measure of readiness such as the Transition Readiness Assessment Questionnaire (24) might improve perceived readiness. In addition, allowing the adolescent to participate in the plan for transition appears to be desirable (23) and may improve patient satisfaction. Although some patients and their parents might never feel ready for transfer, preparation beginning in early adolescence and a flexible yet structured plan for transition and transfer may help alleviate some anxiety and fear. Emotional attachment or bond between patient, parent, and provider was noted by 45% of patients and 44% of parents in our study. Although this has been previously reported as a barrier to adult oriented care (22, 25) this appears to be less common that what is perceived by pediatric providers (3, 23).
The perceived lack of adult specialty providers did not correlate with the patients’ or the parents’ anticipated readiness to transfer to adult oriented care by age 25 years. Patients with congenital heart disease were far more likely to express concerns over the lack of adult care providers than patients with disease from other diagnostic groups. While underlying reasons remain to be clarified, the location and provision of adult congenital heart disease care can remain unclear to patients and families (26, 27). Although training pathways and accreditation are being addressed, current adult congenital heart disease specialists are self-described (cardiologists with either pediatric cardiology or general adult cardiology training or both) without standardization of training or certification (28, 29). These factors may contribute to the apprehension expressed by patients and parents, which may be lessened with improved transition educational programming.
The self-reported barriers to transfer to adult oriented care appear multi-factorial and include emotional attachment, perceived lack of providers, and fear on the part of both the parents and the patients facing lifelong medical disease. These fears should also be addressed in transitioning education programs that facilitate a gradual shift from parent directed to patient-directed (and as appropriate, parent-supported) care management. Reassurance that a child possesses the skills to successfully manage his or her health care can ease parental fears of “letting go.” In addition, ensuring that patients and their parents will have access to qualified adult subspecialists can help alleviate fears of abandonment. Pediatric subspecialists should avoid messages implying that they are the only qualified clinicians capable of providing appropriate care, as has been noted in previous studies (30). Given the increasing number of adult survivors of pediatric onset chronic disease and projected shortage of pediatric subspecialty providers (31) it is unlikely that pediatric institutions will have the required resources to care for the rapidly growing population of adults with chronic pediatric-onset diseases. In addition, as this population continues to age, the onset of adult internal medicine co-morbidities involve areas of expertise that extend beyond the training of most pediatric subspecialists as well as pediatric hospital nurses, and ancillary staff. There is an urgent need for multi-disciplinary teams to engage adult subspecialty providers and establish a system that allows for a gradual transition of care, while providing patients and their families with confidence that all members of the care team are competent and qualified.
Limitations
The population of patients and parents studied was derived from a single pediatric institution, and as such, results may not be generalizable to other health care settings. In particular, several programs are available in local adult centers to accept young adults transitioning with particular chronic diseases, potentially accounting for our observation that concern about lack of adult providers was far less than in previous studies. Exclusion of patients with cognitive impairment precludes extrapolations of the findings to this high-risk population. The results reflect self-reporting and are, therefore, subject to potential social desirability response bias, which may result in an over- or underestimation of prevalence estimates. Having only one open-ended survey question may result in leading question bias. Finally, the cross-sectional nature of this study does not allow for inferences regarding cause-and-effect relationships
Conclusion
Transitioning (self-care management) education is an integral and important component of high quality health care for patients with pediatric onset chronic disease, and is now deemed standard of care. Despite this recognition, transitioning education is most often provided on an inconsistent and informal basis. Our results suggest that, regardless of whether or not clinicians are providing this education, patients and their parents across a wide spectrum of pediatric onset chronic disease report significant gaps in this type of education. Optimal delivery of transitioning education remains to be defined but may include initiation early in adolescence with standardized and validated tools to formalize and monitor the process. In addition, this data suggests that clinicians and key healthcare stakeholders should engage policy makers to ensure that the added time and effort required providing transitioning education is reimbursable by third party payers.
Acknowledgments
The authors would like to acknowledge the contributions to this project by the hospital’s Family and Teen Advisory Councils; Mathieu Clair, M.D.; Laura Risch, B.S.; Douglas-Jarrett Turno, Nathan Demars; Susan Shanske, LCSW; Rhonda Fritz, NP; Richard C. Antonelli, M.D. and Emily Harris. This research was funded in part by the Boston Children’s Hospital Program for Patient Safety and Quality and the Dunlevie Foundation.
Footnotes
There are no relationships with industry.
References
- 1.Reiss J, Edwards L, Daniel P, Wood DL. Healthcare Transition for Youth with Special Healthcare Needs. Northeast Florida Medicine. 2008;59(4):10–6. [Google Scholar]
- 2.American Academy of Pediatrics AAoFP, American College of Physicians TCRAG. Supporting the Health Care Transition From Adolescence to Adulthood in the Medical Home. Pediatrics. 2011 Jul 1;128(1):182–200. doi: 10.1542/peds.2011-0969. [DOI] [PubMed] [Google Scholar]
- 3.Fernandes SM, Fishman L, O’Sullivan-Oliveira J, Ziniel S, Melvin P, Khairy P, et al. Current practices for the transition and transfer of patients with a wide spectrum of pediatric-onset chronic diseases: Results of a clinician survey at a free-standing pediatric hospital. International Journal of Child and Adolescent Health. 2010;3(4):507–15. [Google Scholar]
- 4.Fredericks EM, Dore-Stites D, Well A, Magee JC, Freed GL, Shieck V, et al. Assessment of transition readiness skills and adherence in pediatric liver transplant recipients. Pediatric Transplantation. 2010;14(8):944–53. doi: 10.1111/j.1399-3046.2010.01349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benchimol EI, Walters TD, Kaufman M, Frost K, Fiedler K, Chinea Z, et al. Assessment of knowledge in adolescents with inflammatory bowel disease using a novel transition tool. Inflammatory Bowel Diseases. 2011;17(5):1131–7. doi: 10.1002/ibd.21464. [DOI] [PubMed] [Google Scholar]
- 6.Clarizia NA, Chahal N, Manlhiot C, Kilburn J, Redington AN, McCrindle BW. Transition to adult health care for adolescents and young adults with congenital heart disease: Perspectives of the patient, parent and health care provider. Canadian Journal of Cardiology. 2009;25(9):317–22. doi: 10.1016/s0828-282x(09)70145-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernandes SM, Verstappen A, Ackerman K, Adams EE, Barton C, Breitinger P, et al. Parental Knowledge Regarding Lifelong Congenital Cardiac Care. Pediatrics. 2011 Dec 1;128(6):e1489–e95. doi: 10.1542/peds.2010-3068. [DOI] [PubMed] [Google Scholar]
- 8.Lawson EF, Hersh AO, Applebaum MA, Yelin EH, Okumura MJ, Scheven Ev. Self-management skills in adolescents with chronic rheumatic disease: A cross-sectional survey. Pediatric Rheumatology. 2011;9(1):35. doi: 10.1186/1546-0096-9-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deyk KV, Pelgrims E, Troost E, Goossens E, Budts W, Gewillig M, et al. Adolescents’ Understanding of Their Congenital Heart Disease on Transfer to Adult-Focused Care. The American Journal of Cardiology. 2010;106(12):1803–7. doi: 10.1016/j.amjcard.2010.08.020. [DOI] [PubMed] [Google Scholar]
- 10.McLaughlin SE, Diener-West M, Indurkhya A, Rubin H, Heckmann R, Boyle MP. Improving Transition From Pediatric to Adult Cystic Fibrosis Care: Lessons From a National Survey of Current Practices. Pediatrics. 2008 May 1;121(5):e1160–6. doi: 10.1542/peds.2007-2217. [DOI] [PubMed] [Google Scholar]
- 11.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- 12.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–12. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Vigl M, Kaemmerer M, Seifert-Klauss V, Niggemeyer E, Nagdyman N, Trigas V, et al. Contraception in Women With Congenital Heart Disease. American Journal of Cardiology. 2010;106(9):1317–21. doi: 10.1016/j.amjcard.2010.06.060. [DOI] [PubMed] [Google Scholar]
- 14.Hohmann C, Borgmann-Staudt A, Rendtorff R, Reinmuth S, Holzhausena S, Willich SN, et al. Patient Counselling on the Risk of Infertility and Its Impact on Childhood Cancer Survivors: Results from a National Survey. Journal of Psychosocial Oncology. 2011;29(3):274–85. doi: 10.1080/07347332.2011.563344. [DOI] [PubMed] [Google Scholar]
- 15.Fernandes SM, Arendt KW, Landzberg MJ, Economy KE, Khairy P. Pregnant women with congenital heart disease: cardiac, anesthetic and obstetrical implications. Expert Review of Cardiovascular Therapy. 2010;8(3):439–48. doi: 10.1586/erc.09.179. [DOI] [PubMed] [Google Scholar]
- 16.Kenney LB, Cohen LE, Shnorhavorian M, Metzger ML, Lockart B, Hijiya N, et al. Male Reproductive Health after Childhood, Adolescent, and Young Adult Cancer: a report from the Children’s Oncology Group. Journal of Clinical Oncology. 2012 doi: 10.1200/JCO.2011.38.6938. Epub May 29, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Green DM, Sklar CA, JDB, Mulvihill JJ, Whitton JA, Stovall M, et al. Ovarian Failure and Reproductive Outcomes After Childhood Cancer Treatment: Results From the Childhood Cancer Survivor Study. Journal of Clinical Oncology. 2009;27(14):2374–81. doi: 10.1200/JCO.2008.21.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, et al. Youth Risk Behavior Surveillance. Washington, DC: Department Of Health And Human Services, Centers for Disease Control and Prevention; 2009. [Google Scholar]
- 19.Britto MT, Garrett JM, Dugliss MAJ, CWD, Johnson CA, Leigh MW, et al. Risky Behavior in Teens With Cystic Fibrosis or Sickle Cell Disease: A Multicenter Study. Pediatrics. 1998;101(2):250–6. doi: 10.1542/peds.101.2.250. [DOI] [PubMed] [Google Scholar]
- 20.Reid GJ, Webb GD, McCrindle BW, Irvine MJ., MD, SCS Health Behaviors among Adolescents and Young Adults with Congenital Heart Disease. Congenital Heart Disease. 2008;3(1):16–25. doi: 10.1111/j.1747-0803.2007.00161.x. [DOI] [PubMed] [Google Scholar]
- 21.Klosky JL, Howell CR, Li Z, Foster RH, Mertens AC, Robison LL, et al. Risky Health Behavior Among Adolescents in the Childhood Cancer Survivor Study Cohort. Journal of Pediatric Psychology. 2012 doi: 10.1093/jpepsy/jss046. Epub March 16, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reiss JG, Gibson RW, Walker LR. Health Care Transition: Youth, Family and Provider Perspectives. Pediatrics. 2005;115(112):112–20. doi: 10.1542/peds.2004-1321. [DOI] [PubMed] [Google Scholar]
- 23.Tong A, Wong G, Hodson E, Walker R, Tjaden L, Craig J. Adolescent views on transition in diabetes and nephrology. Eur J Pediatr 2013. 2013 Mar 01;172(3):293–304. doi: 10.1007/s00431-012-1725-5. English. [DOI] [PubMed] [Google Scholar]
- 24.Sawicki G, Lukens Bull K, Yin X, Demars N, Huang IC, Livingood W, et al. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ--Transition Readiness Assessment Questionnaire. Journal of Pediatric Psychology. 2011;36(2):160–71. doi: 10.1093/jpepsy/jsp128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lugasi T, Achille M, Stevenson M. Patients’ Perspective on Factors That Facilitate Transition From Child-centered to Adult-centered Health Care: A Theory Integrated Metasummary of Quantitative and Qualitative Studies. Journal of Adolescent Health. 2011 May;48(5):429–40. doi: 10.1016/j.jadohealth.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 26.Kogon BE, Plattner Courtney, Leong T, Kirshbom PM, Kanter KR, McConnell M, et al. Adult CongenitalHeart Surgery: Adult or Pediatric Facility? Adult or Pediatric Surgeon? The Annals of Thoracic Surgery. 2009;87(3):833–40. doi: 10.1016/j.athoracsur.2008.12.027. [DOI] [PubMed] [Google Scholar]
- 27.Fernandes SM, Landzberg MJ. Transitioning the young adult with congenital heart disease for life-long medical care. Pediatric Clinics of North America. 2004;51(6):1739–48. doi: 10.1016/j.pcl.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 28.Gurvitz MZ, Chang R-K, Ramos FJ, Allada V, Child JS, Klitzner TS. Variations in Adult Congenital Heart Disease Training in Adult and Pediatric Cardiology Fellowship Programs. Journal of the American College of Cardiology. 2005;46(5):893–8. doi: 10.1016/j.jacc.2005.05.062. [DOI] [PubMed] [Google Scholar]
- 29.Williams RG, Pearson GD, Barst RJ, Child JS, Nido Pd, Gersony WM, et al. Report of the National Heart, Lung, and Blood Institute Working Group on Research in Adult Congenital Heart Disease. Journal of the American College of Cardiology. 2006;47(4):701–7. doi: 10.1016/j.jacc.2005.08.074. [DOI] [PubMed] [Google Scholar]
- 30.O’Sullivan-Oliveira J, Fernandes SM, Borges LF, Fishman LN. Pediatric Nursing. 2012. Transition of Pediatric Patients to Adult Care: An Analysis of Provider Perceptions across Discipline and Role. (Pending Publication) [PubMed] [Google Scholar]
- 31.Jewett EA, Anderson MR, Gilchrist GS. The Pediatric Subspecialty Workforce: Public Policy and Forces for Change. Pediatrics. 2005;116(5):1192–202. doi: 10.1542/peds.2004-2339. [DOI] [PubMed] [Google Scholar]