Abstract
Background:
The Chvostek sign—a contraction of ipsilateral facial muscles subsequent to percussion over the facial nerve—is considered a clinical indicator of hypocalcemia. I sought to evaluate the association between Chvostek sign and serum calcium levels.
Methods:
I performed a cross-sectional analysis of data gathered from a nationwide probability sample of 3,434 individuals, aged 25–74 years, in the First National Health and Nutrition Examination Survey, conducted from 1971 to 1975.
Results:
Increasing serum calcium levels were associated with an increased odds for a positive Chvostek sign. When compared to calcium levels in the lowest quartile (5.47–9.4 mg/dL), individuals with serum calcium levels of 9.4–9.6 mg/dL, 9.6–9.9 mg/dL, and 9.9–11.9 mg/dL had a 195% (95% confidence interval [CI] 23.3%–604%), 124% (95% CI −0.8% to 407%), and 159% (95% CI 33.8%–401%) increased odds—as opposed to the expected decreased odds—for a positive Chvostek sign. When adjusting for age, sex, and race, these increased odds were 220% (95% CI 32%–679%), 125% (95% 0.00%–409%), and 172% (35%–448%), respectively. For every 1 g/dL increase in serum calcium level, the odds for a positive Chvostek sign increased by 4% (95% CI 0.00%–8%).
Conclusions:
A positive Chvostek sign is informative of normal to increased serum calcium levels rather than hypocalcemia.
In 1876, Dr. Franz Chvostek,1 a Viennese surgeon, observed an increased mechanical irritability of the peripheral nerves in a patient with latent tetany. The increased irritability of the facial nerve, manifested by twitching of the ipsilateral facial muscles on percussion over the branches of the facial nerve, came to be known as Chvostek sign. This clinical finding has become widely accepted in the medical community as a sign of hypocalcemia.2,3
Despite this acceptance, the existing literature does not provide strong evidence for this association. Of the 54 studies written in English, and identified on PubMed with an inclusive search strategy, only 11 included data on positive Chvostek sign rates and serum calcium levels.4–14 Only 4 measured calcium levels in all evaluated patients, a minimum requirement for evaluating diagnostic accuracy.5–7,12 Sensitivities from these 4 studies ranged from 0% to 100% and specificities from 78.8% to 100%.
The association of Chvostek sign with normocalcemic diseases such as migraines and epilepsy further calls into question its role as an indicator of hypocalcemia.6 This study examined the association of Chvostek sign and serum calcium in the setting of the National Health and Nutrition Examination Survey I (NHANES I) and estimated the diagnostic accuracy of the sign for states of hypocalcemia. Data from NHANES I provided an opportunity to examine this association, as the survey evaluated the presence of a Chvostek sign in 3,854 individuals and measured serum calcium for all participants.
METHODS
Study population
NHANES I was conducted from 1971 to 1975 on a nationwide probability sample of 28,043 people from 65 locations across the United States. Participants were between the ages of 1 and 74 years and were noninstitutionalized individuals. Individuals at high risk for malnutrition, specifically low-income people, women, children, and the elderly, were oversampled. Adjusted sampling weights were provided along with the data to allow results drawn from the data to be applicable to reflect the general noninstitutionalized US population. A detailed description of the survey has been published.15 A subgroup of 3,854 individuals from the ages of 25 to 74 years underwent more detailed medical examinations, which included testing for the Chvostek sign. No oversampling was done when forming these subgroups. This study looked only at these individuals who received the more detailed examination.
Standard protocol approvals, registrations, and patient consents
Ethics approval was not obtained for this study, as it was an analysis of deidentified data.
Calcium levels
Venipuncture was done on the same day as the physical examination by nursing staff. Examinees did not receive any treatment in between venipuncture and the physical examination. Resultant specimens were centrifuged and the serum was removed, placed into vials, and frozen to −20°C. These vials were then packaged with solid-slab dry ice and shipped daily to the Center for Disease Control at Atlanta, Georgia, where serum calcium was measured using the SMA 12/60 calcium method. This method was chosen by the Centers for Disease Control and Prevention (CDC) and reflected the current laboratory practice for serum calcium measurement.16 Biochemistries were measured for all examinees where sufficient serum was collected. The number, training, and expertise of the people working in the laboratory with the SMA 12/60 method are not known. Individuals with calcium levels listed as unacceptable data, blank but applicable, or no test done were labeled as missing.
Ionized calcium is the gold standard for assessing hypocalcemia; however, as this was not measured in the NHANES survey, it could not be used for this study. Instead, total calcium adjusted for albumin levels was used. For many patients, total serum calcium is highly correlated with ionized calcium.17 However, albumin levels that differ greatly from the normal range can cause total serum calcium levels to be either falsely elevated or depressed. Therefore, it is a common practice in the clinical setting to correct serum calcium levels for the patient's serum albumin level. In this study, all serum calcium levels used in statistical analysis were first corrected for albumin level using the equation corrected calcium (mg/dL) = measured calcium (mg/dL) + 0.8 × (4 − measured albumin [g/dL]).17
Hypocalcemia was defined as an adjusted serum calcium level less than 8.4 mg/dL, normocalcemia as 8.5–10.2 mg/dL, and hypercalcemia as greater than 10.3 mg/dL. These definitions are consistent with those currently used in the medical community.2
While it seems unlikely that the technicians measuring serum calcium values at the CDC had access to the physical examination results, no information on this matter could be found, and therefore it is not known whether those performing the reference standard were blinded to the results of the index test.
Chvostek sign
The physical examinations were performed in one of 3 mobile examination centers by physicians who were given detailed, standardized instructions on how to perform and score each part, and who underwent 1–3 days of training. The total number of physicians conducting the physical examinations is not known; however, each examinee was examined by one physician. The Chvostek sign was evaluated by percussing the malar process of the temporal bone on both sides of the face with a percussion hammer. A positive Chvostek sign was defined as visible contraction of the ipsilateral perioral muscles.16 It was scored as either positive or negative.
The results of the serum calcium measurements were not available at the time that the physicians performed the physical examination, and therefore they were blinded to the results of the reference standard when they performed the index test.
Statistical analysis
The association between corrected serum calcium levels and the Chvostek sign, both adjusted and nonadjusted for covariates including race, age, and sex, were estimated using logistic regression models, which took into account the sampling design of NHANES I. Corrected serum calcium levels were modeled both as a continuous and a discrete variable. For the latter, corrected serum calcium levels were divided into quartiles, with the lowest quartile as the reference cell. A 2-tailed p value of <0.05 was considered to be significant.
The c statistic, which is equivalent to the area under the receiver operating characteristic curve, was calculated to evaluate model fit and discrimination.18 Measures of diagnostic accuracy and their 95% confidence intervals (CIs) were calculated accounting for sampling design; this included sensitivity, specificity, positive and negative predictive values, and likelihood ratios.19
RESULTS
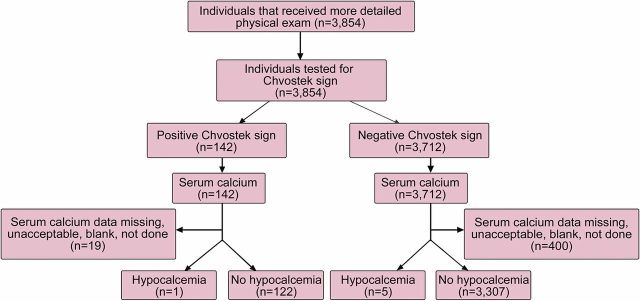
The population that underwent the more detailed physical examination numbered 3,854 individuals, with ages ranging from 25 to 74 years. A total of 419 individuals had missing serum calcium levels and were not included in the data analysis. In addition, one individual had an adjusted serum calcium level of 0.17 mg/dL, and due to the improbability of this value being compatible with life, this was assumed to be an error and was excluded from analysis. This left 3,434 observations to be analyzed. All 3,854 individuals were checked for the Chvostek sign, and had either a negative or a positive result. See figure 1 for flowchart. The average age of the 3,434 individuals was 46.2 years (95% CI 45.7–46.8 years). The average adjusted serum calcium level was 9.64 mg/dL (95% CI 9.62–9.65 mg/dL). The group had 47.65% (95% CI 45.92%–49.38%) men and 52.35% (95% CI 50.62%–54.08%) women, and was 89.46% (95% CI 87.8%–91.92%) white, 9.74% (95% CI 8.14%–11.34%) black, and 0.80% (95% CI 0.27%–1.33%) other.
Figure 1. Flow diagram of analyzed data.
Flow diagram of number of individuals receiving index and reference test, number of individuals with positive and negative index tests with the target condition present or absent, and number of individuals with missing data.
Serum calcium levels and Chvostek sign
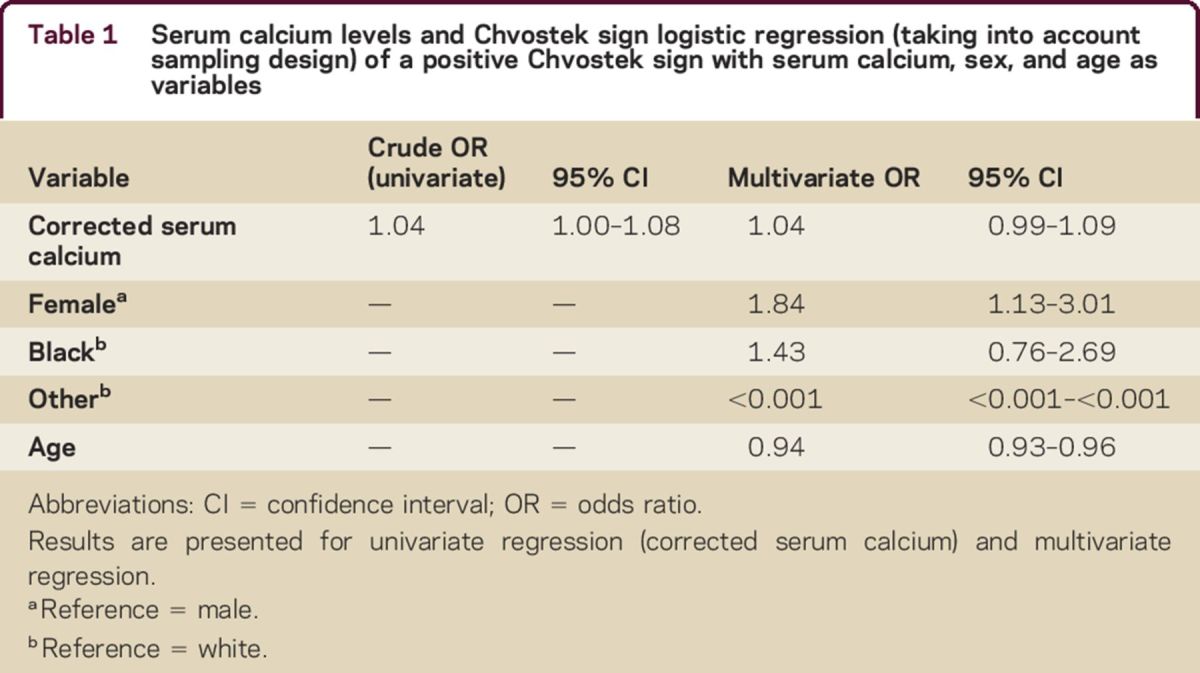
The univariate (nonadjusted) odds ratio (OR) for the association between a positive Chvostek sign and serum calcium was 1.04 (95% CI 1.00–1.08), with a c statistic of 0.55 (95% CI 0.51–0.60) (table 1). Thus, for every 1 g/dL increase in serum calcium level, the odds for a positive Chvostek sign increased by 4%. This association was opposite of what was expected and was significant. When the OR was adjusted for age, race, and sex, the association became nonsignificant (OR 1.04; 95% CI 0.99–1.09), with a c statistic of 0.70 (95% CI 0.66–0.74).
Table 1.
Serum calcium levels and Chvostek sign logistic regression (taking into account sampling design) of a positive Chvostek sign with serum calcium, sex, and age as variables
Analysis for quartiles of serum calcium levels
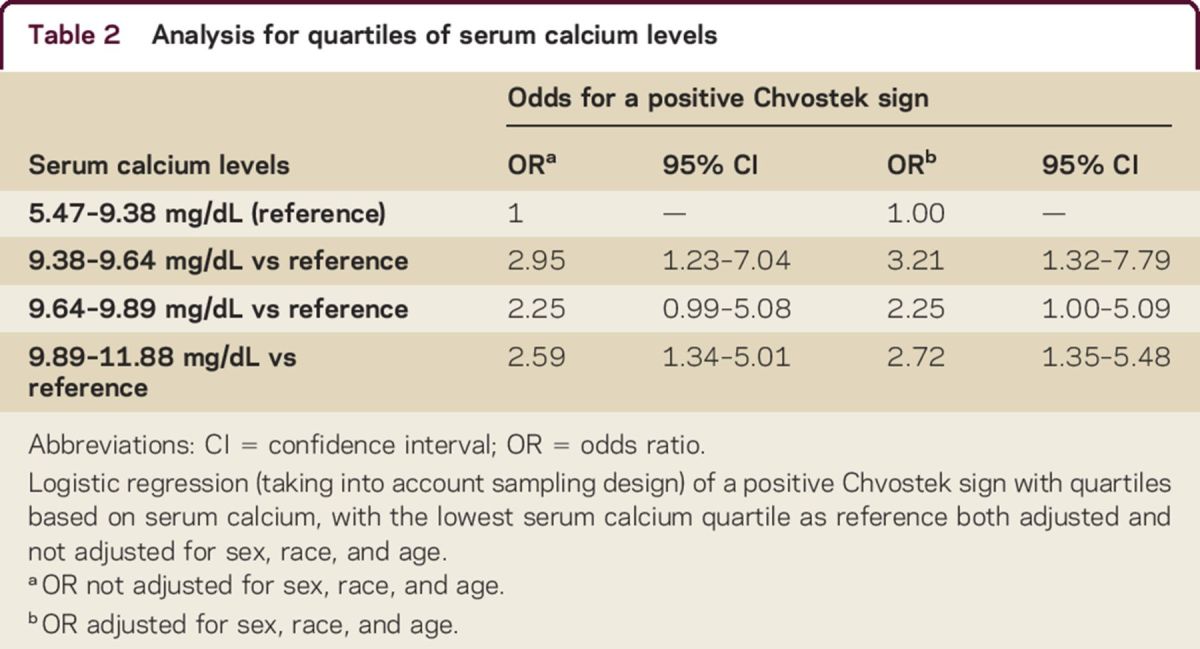
The 4 quartiles of serum calcium levels were 5.47 mg/dL to ≤9.38 mg/dL, 9.38 mg/dL to ≤9.64 mg/dL, 9.64 mg/dL to ≤9.89 mg/dL, and 9.89 mg/dL to ≤11.88 mg/dL (table 2). Each quartile, when compared to the lowest quartile of serum calcium level, had an increased odds for a positive Chvostek sign. The ORs calculated from the regression adjusting for age, sex, and race were 3.21 (95% CI 1.32–7.79) for the second quartile, 2.25 (95% CI 1.00–5.09) for the third quartile, and 2.72 (95% CI 1.35–5.48) for the fourth quartile. The c statistic for this model was 0.70 (95% CI 0.66–0.75). The ORs calculated from the regression not adjusting for age, sex, and race were 2.95 (95% CI 1.23–7.04) for the second quartile, 2.24 (95% CI 0.99–5.07) for the third quartile, and 2.59 (95% CI, 1.34–5.01) for the fourth quartile. The c statistic for this model was 0.56 (95% CI 0.51–0.61). The Wald χ2 for the 3 degrees of freedom for these 2 regressions was 9.65 (p < 0.02) and 9.16 (p < 0.03), respectively, indicating that the overall test was significant and that the pairwise comparisons were relevant.
Table 2.
Analysis for quartiles of serum calcium levels
Sensitivity, specificity, likelihood ratios, and positive and negative predictive values
Of the 3,434 individuals tested, there were 123 with a positive Chvostek sign and 5 with hypocalcemia. Of these 123 individuals with a positive Chvostek sign, only 1 had hypocalcemia. The remaining 4 individuals with hypocalcemia had a negative Chvostek sign. The calculated sensitivity was 25.63% (95% CI 0.00%–76.97%) and specificity was 96.29% (95% CI 95.30%–97.30%). The positive likelihood ratio was 6.90 (95% CI, 1.26–37.71) and the negative likelihood ratio was 0.77 (95% CI 0.47–1.27). The positive predictive value was 0.66% (95% CI 0.00%–1.93%) and the negative predictive value was 99.93% (95% CI 99.83%–100.00%).
Demographics and a positive Chvostek sign
Female participants were significantly more likely to have a positive Chvostek sign than male participants: adjusted OR 1.84 (95% CI 1.13–3.01) (table 1). Younger individuals were significantly more likely to have a positive Chvostek sign than older individuals, with an adjusted OR of 0.94 (95% CI 0.93–0.96). There was no association between race and the likelihood for a positive Chvostek sign.
DISCUSSION
Individuals with normocalcemia or hypercalcemia were significantly more likely to have a positive Chvostek sign than individuals with hypocalcemia. These findings are opposite of what is reported in standard reference works on the diagnostic significance of a positive Chvostek sign.2,3 One of the main strengths of this study was that it was based on data from a nationally representative sample of the United States on which a standardized physical examination, including the Chvostek sign, was performed, as well as serum calcium measurements. Additionally, with 3,434 individuals, it is the largest study to date examining both Chvostek sign and serum calcium level in all participants. The second largest study identified on PubMed had a sample size of 154.6
The NHANES survey data identified that a positive Chvostek sign was more likely among female patients and children. These findings may explain the reported high false-positive rates of the Chvostek sign in both female patients and children.5,9–11,20–22 Skepticism concerning the accuracy of the Chvostek sign is particularly prevalent in the field of pediatrics, and several studies have reported low sensitivity and specificity in children.5,9,10,20–22 One study identified a false-positive rate of 64% in neonates, 41% in children, and 8% in adults.14 Compared with age, there is less evidence regarding the effects of sex on Chvostek sign. Three studies, one carried out on the NHANES I data, have reported a higher but not significant prevalence of a false-positive Chvostek sign in women.9,10,21
The findings reported here support the hypothesis that hyperexcitability of the facial nerve, unrelated to serum calcium levels, may lead to a positive Chvostek sign. Chvostek1 speculated that the Chvostek sign was a direct result of stimulation of the facial nerve, and a study done by Kugelberg23 appears to support this hypothesis. Our findings suggest that this sensitivity of the facial nerve cannot be attributed to a hypocalcemic state. We hypothesize that a positive Chvostek sign results from neural and muscular hyperexcitability unrelated to serum calcium levels. This hypothesis is consistent with the reports that a positive Chvostek sign is associated with migraines and hypomagnesemia, 2 conditions unrelated to hypocalcemia.20 This hypothesis would also explain why female patients and younger individuals are more likely to have a positive Chvostek sign, as these 2 groups have been found to possess neural hyperexcitability.24
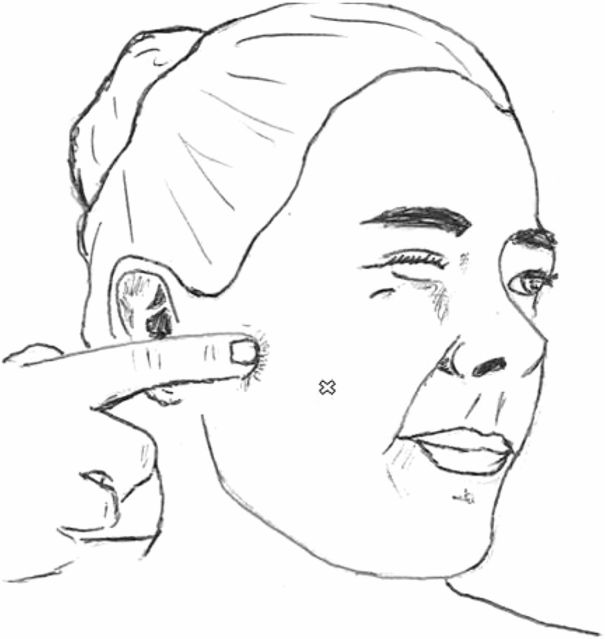
The exact location of percussion for the Chvostek sign varies in the literature, and different locations carry different likelihoods of causing a positive Chvostek sign.8,20 The 2 most common areas of percussion are anterior to the external meatus over the vertical ramus of the mandible and percussion on the soft tissues of the cheek, halfway between the earlobe and the corner of the mouth (figure 2). The rate of positive Chvostek sign for each location varies in the literature, with a recent review on Chvostek sign finding a range of 1%–50% positives for the former and 5%–29% positives for the latter location.20 One study comparing these 2 possible techniques speculated that percussion over the soft tissues may result in direct muscle stimulation and therefore not result in a true positive.8 No consensus exists in the literature on the proper technique to use. In this study, physicians were instructed to percuss over the malar process of the temporal bone. This region sits just before the auditory canal, along the zygomatic arch, where the facial nerve branches out to innervate the facial muscles. This location of percussion is most consistent with the technique of percussing over the vertical ramus, although it is slightly more anterior and superior. Due to the variability in reported techniques and their associated positive rates, the implications of the percussion location used in this study are difficult to assess.
Figure 2. Illustration of a positive Chvostek sign following percussion over the vertical ramus of the mandible.
There are variable techniques used to elicit the Chvostek sign, and the X marks one common location used to elicit the sign, located midway from the ear to the corner of the mouth. The finger is percussing over another common area, the vertical ramus of the mandible. The illustrated Chvostek sign represents what some would grade as a marked sign, as it involves the orbicularis oculi and ala nasi in addition to the orbicularis oris. A mild sign only involves contraction of the orbicularis oris muscle.
The definition of a positive Chvostek sign used in this survey was consistent with the literature: a positive sign being contraction of the ipsilateral facial muscles, in this case the orbicularis oris. Some studies grade the Chvostek sign, with a mild sign involving contraction of the orbicularis oris muscle, and a more marked sign involving the orbicularis oculi or the ala nasi muscles in addition to the orbicularis oris muscle.6,13,20 By defining a positive Chvostek sign as a contraction of the orbicularis oris, this survey encompassed all grades of a positive Chvostek sign.
There are several limitations of this study. The first is that the more detailed physical examination that included the Chvostek sign was performed only on individuals ranging from 25 to 74 years of age. This excludes younger age groups. The second is that the average serum calcium, 9.6 mg/dL, was in the normocalcemic range, and the prevalence of hypocalcemia in the studied population was very low (5 individuals out of 3,434). Therefore, the studied population was not representative of those who would undergo the Chvostek test in clinical practice. We cannot exclude the possibility of a bathtub-shaped association between a positive Chvostek sign and hypocalcemia, and that a positive Chvostek sign is indicative of an abnormally high or low calcium level. However, if such a bathtub-shaped association indeed existed, it would indicate that it would be dangerous to make clinical decisions based simply on a Chvostek sign. Another limitation is that there was potential variability in how physicians elicited the Chvostek sign, despite specific directions given to physicians on how to perform the test.
This study found that a positive Chvostek sign was associated with higher levels of serum calcium, the opposite of what is traditionally reported in medical reference works. The existing literature on Chvostek sign is sparse, and no studies could be identified that analyzed its diagnostic accuracy as a marker of hypocalcemia. The findings of this study confirm the low sensitivity and specificity and high false-positive rate, particularly in younger individuals and female patients, which have previously been identified in the literature. This finding has implications for the utility of this physical examination technique in clinical practice as a marker for hypocalcemia, as well as for hypotheses regarding the mechanism of the sign, which has been hypothesized to be due to causes unrelated to serum calcium.
ACKNOWLEDGMENT
The author thanks Dr. Philippe Hujoel for his assistance in statistical analysis and general guidance.
AUTHOR CONTRIBUTIONS
I.A. Hujoel is responsible for data analysis, the study concept and design, and drafting and revising the manuscript.
STUDY FUNDING
No targeted funding reported.
DISCLOSURES
I.A. Hujoel reports no disclosures. Full disclosure form information provided by the author is available with the full text of this article at Neurology.org/cp.
REFERENCES
- 1.Chvostek V. Beitrag zur Tetanie. Wein Med Presse 1876;17:1201–1204. [Google Scholar]
- 2.Godara H, Hirbe A, Nassif M, Otepka H, Rosenstock A, eds. The Washington Manual of Medical Therapeutics, 34th ed Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 3.Longo D, Fauci A, Kasper D, Hauser S, Jameson J, Loscalzo J, eds. Harrison's Principles of Internal Medicine, 18th ed New York: McGraw Hill Medical; 2011. [Google Scholar]
- 4.Méneret A, Guey S, Degos B. Chvostek sign, frequently found in healthy subjects, is not a useful clinical sign. Neurology 2013;80:1067. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal K, Baijal N, Tiwari L, Verma N, Sahni M, Puliyel J. Swan-neck sign of the big toe: association with hypocalcaemia. Trop Doct 2007;37:238–239. [DOI] [PubMed] [Google Scholar]
- 6.Ahmed M, Martinez A, Mariam S, Whitehouse W. Chvostek's sign and hypocalcaemia in children with seizures. Seizure 2004;13:217–222. [DOI] [PubMed] [Google Scholar]
- 7.Strickland P, Recabaren J. Are preoperative serum calcium, parathyroid hormone, and adenoma weight predictive of postoperative hypocalcemia? Am Surg 2002;68:1080–1082. [PubMed] [Google Scholar]
- 8.Hopkins I. Chvostek's sign and facial reflexes in normal newborn infants. Dev Med Child Neurol 1964;6:389–392. [DOI] [PubMed] [Google Scholar]
- 9.Hoffman E. Clinical evaluation of the Chvostek sign. Am Surg 1960;26:501–505. [PubMed] [Google Scholar]
- 10.Hoffman E. The Chvostek sign: a clinical study. Am J Surg 1958;96:33–37. [DOI] [PubMed] [Google Scholar]
- 11.Moller K, Soderling B. The significance of Chvostek's symptom in infants under 2 years of age. Acta Paediatr 1949;37:318–322. [DOI] [PubMed] [Google Scholar]
- 12.McGreal G, Kelly J, Hehir D, Brady M. Incidence of false positive Chvostek's sign in hospitalised patients. Ir J Med Sci 1995;164:56. [DOI] [PubMed] [Google Scholar]
- 13.Kotowicz J. Occurrence of Chvostek's sign in healthy people and its significance. Pol Med J 1969;8:440–443. [PubMed] [Google Scholar]
- 14.Krogh L, Wynne J, Cywes S. The value of Chvostek's sign in tetany. S Afr Med J 1968;42:846–847. [PubMed] [Google Scholar]
- 15.A statistical methodology for analyzing data from a complex survey: the first National Health and Nutrition Examination Survey [online]. Available at: http://www.cdc.gov/nchs/data/series/sr_02/sr02_092.pdf. Accessed March 8, 2015. [PubMed]
- 16.HANES: Examination Staff Procedures Manual for the Health and Nutrition Examination Survey, 1971–1973 [online]. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanesi/15a71_73.pdf. Accessed March 8, 2015.
- 17.Baird G. Ionized calcium. Clinica Chim Acta 2011;412:696–701. [DOI] [PubMed] [Google Scholar]
- 18.Agnelli R. Paper SA S404-2014: Examples of Logistic Modeling With the SURVEYLOGISTIC Procedure [online]. Available at: http://support.sas.com/resources/papers/proceedings14/SAS404-2014.pdf. Accessed February 19, 2016. [Google Scholar]
- 19.Simel DL, Samsa GP, Matchar DB. Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol 1991;44:763–770. [DOI] [PubMed] [Google Scholar]
- 20.Hasan Z, Absamara R, Ahmed M. Chvostek's sign in paediatric practice. Curr Pediatr Rev 2014;10:194–197. [PubMed] [Google Scholar]
- 21.Lowenstein F. Major nutritional findings from the first Health and Nutrition Examination Survey in the United States of America, 1971–1974. Bibl Nutr Dieta 1981;30:1–16. [DOI] [PubMed] [Google Scholar]
- 22.Veerappan D, Ahmed MAS. NMP034 Chvostek's sign in normal children. Eur J Paediatric Neurol 2007;11:114. [Google Scholar]
- 23.Kugelberg E. The mechanism of Chvostek's sign. AMA Arch Neurol Psychiatry 1951;65:511–517. [DOI] [PubMed] [Google Scholar]
- 24.McHugh J, Reilly R, Connolly S. Examining the effects of age, sex, and body mass index on normative median motor nerve excitability measurements. Clin Neurophysiol 2011;122:2081–2088. [DOI] [PubMed] [Google Scholar]