Abstract
Background
This study evaluated the clinical application of high-frequency color Doppler ultrasonography (HFCDU) in the diagnosis, treatment, and rehabilitation of Achilles tendon injury.
Material/Methods
A total of 68 patients with suspected Achilles tendon injury were examined by HFCDU. There were 42 Achilles tendon injury patients who underwent surgery, and they were randomly divided into a routine treatment group (n=21) and a rehabilitation group (n=21). HFCDU was performed at weeks 1, 3, 6, and 9, and months 3, 6, 9, 12, and 24 after the operation. The thickness of the injured Achilles tendon, echo, blood flow, and tissue adhesion were compared to those of the uninjured side.
Results
Of the 68 patients, 14 had normal ultrasound presentation with strong echo; 7 had laceration, presenting as swelling and decreased echo; 26 had partial tear, presenting as discontinued rupture with no or low echo; 19 had complete rupture, presenting as discontinued fibers with hypoechoic hemorrhage and hyperechoic fat tissue between ends; 1 had plantar tendon rupture and periapical hemorrhage; and 1 had acute Achilles tendonitis. The postoperative tendon thickness decreased over time, echo turned homogeneous, blood flow and adhesions decreased, and these results were consistent with clinical symptoms. Patient condition and ultrasound recovery were better in the rehabilitation group, and the diameter of the injured tendon increased compared with the uninjured side.
Conclusions
HFCDU can determine the types and extent of tendon injuries, and can help in the diagnosis, treatment, and rehabilitation of Achilles tendon injury.
MeSH Keywords: Diagnosis; Rehabilitation; Ultrasonography, Doppler
Background
The Achilles tendon is one of the most powerful tendons of the human body and it can withstand great forces. In recent years, Achilles tendon injury usually occurs during public sports and recreational activities. Achilles tendon injuries can be categorized as open injury or closed injury. The open injury is easier to diagnose, while the closed injury is harder to diagnose, and the diagnosis of the latter depends more on experience and is prone to misdiagnosis. Early diagnosis reduces the incidence of post-trauma complications and maximizes the motor function [1,2], and therefore is vital for subsequent treatment.
X-ray evaluation of Achilles tendon injury has relatively low sensitivity and specificity (possibly due to its low resolution), and is often used in auxiliary examination or in bone-damage exclusion for patients with acute trauma. MRI examination has the advantage of high soft tissue resolution, showing not only the site and degree of the Achilles tendon injury, but also the edema and bleeding in surrounding soft tissues. However, MRI examination is time-consuming and expensive and is therefore not widely used in evaluating Achilles tendon injury. High-frequency color Doppler ultrasonography (HFCDU) can provide high-resolution images of soft tissues [3] to clearly distinguish subcutaneous tissue, Achilles tendon, aponeurosis, and surrounding connective tissue. It also gives details of Achilles tendon injuries, such as location and injury scope. Therefore, HFCDU may reduce the clinical misdiagnosis and evaluate Achilles tendon recovery after treatment, serving as an effective, affordable, noninvasive, and easy to perform examination method. This study evaluated the efficacy of HFCDU in the diagnosis, treatment, and rehabilitation of Achilles tendon injury.
Material and Methods
Subjects
A total of 68 patients with Achilles tendon injury were recruited, including 48 males and 20 females, with the mean age of 31.2 years (with a standard deviation of 7.9 years) ranging from 18 to 50 years. The main clinical symptoms were ipsilateral leg pain, swelling, and limited ankle mobility. All of them had closed injury as confirmed by MRI examination or surgery. The study was approved by the Medical Ethics Board of Liaocheng People’s Hospital. Informed consent was obtained from all patients or their families.
Ultrasound evaluation with HFCDU
Patients were in lateral position for vertical and horizontal scanning of the Achilles tendon. The ankle joint was passively stretched, and the triceps were squeezed for dynamic observation. The scan images were compared with that of the healthy side. The ultrasound was performed using a Philips iu22 and GE color Doppler ultrasound apparatus with probe frequency of 5–10 Mhz. Two ultrasound physicians evaluated and measured the ultrasound and another 2 physicians followed up the patients and performed statistical analysis.
Surgery treatment
Surgery was performed based on the results of HFCDU and Kuwade [4] classifications. Type I: patients with partial fracture less than 50% can choose non-surgery or surgery treatment; Type II: patients with complete injury and defects less than 3 cm can choose staged suture; Type III: patients with complete injury and defects of 3–6 cm can choose reinforcement sutures of plantar tendon or flip gastrocnemius tendon; Type IV: patients with complete injury and defects greater than 6 cm can choose reversed gastrocnemius tendon suture repair or free tendon transplantation. A total of 42 patients received surgical treatment and the other 26 patients were treated with the routine procedure. According to the methods of rehabilitation after surgery, these 42 patients were randomly divided into 2 groups by Urn randomization: a routine treatment group (21 patients) and a rehabilitation treatment group (21 patients). The rehabilitation program included fixation (0–4 weeks), activity and muscle strength practice (4–12 weeks), and consolidation period (13–24 weeks).
Treatment evaluation
HFCDU was performed at weeks 1, 3, 6, and 9, and at months 3, 6, 9, 12, and 24 after the operation. The changes in the Achilles tendon were recorded, including the thickness (percentage of follow-up thickness vs. postoperative thickness), echo (degree and uniformity), blood flow (the blood flow signal with the same blood flow speed, gain, and depth), and the sliding distance with plantar flexion at 15°. The scores of Achilles tendon recovery are shown in Table 1. The scores were categorized into 4 scales: excellent (9–12 points), very good (6–8 points), good (3–5 points), and poor (0–2 points).
Table 1.
The ultrasound evaluation of Achilles tendon in recovery.
| Score | Thickness (percentage) | Echo | Blood signal strips (amount) | Degree of adhesion (sliding distance (mm)) |
|---|---|---|---|---|
| 0 | 100% | Low, uneven | >5 | 0 |
| 1 | 90%–99% | Low, uneven | 3–5 | 0–1 |
| 2 | 80%–89% | High, uneven | 1–2 | 1–2 |
| 3 | <80% | High, even | 0 | >2 |
Achilles tendon recovery was evaluated in comparison with the uninjured side, using the Amer-Lindholm evaluation method, as follows. 1) Excellent efficacy: patients can walk normally without discomfort or abnormal muscle strength; patient can raise heels; calf circumference decreased less than 1 cm; dorsiflexion or plantar flexion angle reduced less than 5°. 2) Satisfactory efficacy: patients can walk with slight difficulty, discomfort, and mild muscle strength; patient can raise heels with efforts; calf circumference decreased less than 3 cm; dorsiflexion reduced between 5 to 10°; plantar flexion angle reduced between 5 to 15°. 3) Poor efficacy: patients can walk with severe difficulty, discomfort, and weak muscle strength; patient cannot raise heels; calf circumference decreased more than 3 cm; dorsiflexion reduced more than 10°; plantar flexion angle reduced more than 15°.
Statistical analysis
The data were analyzed using SPSS 16.0 (IBM, USA). The measurement data are expressed as mean ± standard deviation. The t test and ANOVA were used to compare differences between the 2 groups. P<0.05 was considered statistically significant.
Results
Imaging features of Achilles tendon injury on HFCDU before surgery
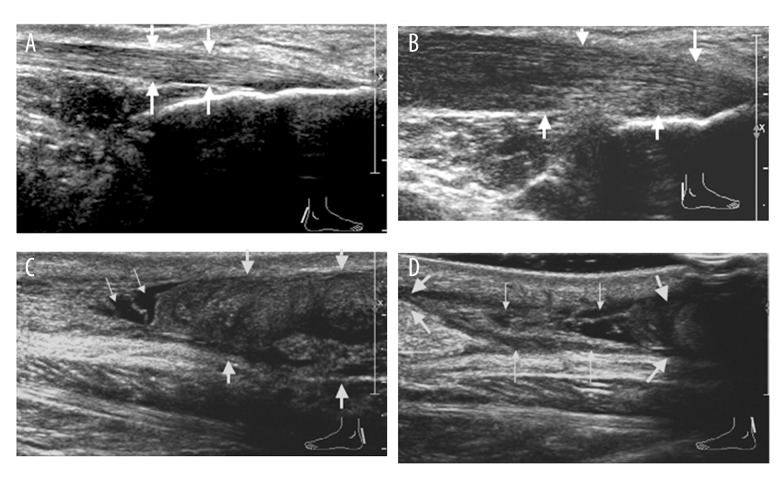
The features of Achilles tendon injury on HFCDU are shown in Figure 1. Normal Achilles tendon showed strong echo with fine homogeneity on longitudinal section (Figure 1A). It was connected with the gastrocnemius, soleus, and calcaneus, with clear upper and lower boundaries. On the cross-section, the starting, middle, and end points of the Achilles tendon presented as oval, round, and crescent-shaped homogeneous strong echo, respectively. As shown in Figure 1B, in Achilles tendon laceration, Achilles tendon was swollen and thickened, with reduced echo, blurred fiber texture, and no significant fiber loss. For partial tear of Achilles tendon (Figure 1C), Achilles tendon fibers were partially discontinuous with low or no echo in the torn area, no smooth edges, irregular ends, and echo-free area around the tear. For complete injury of Achilles tendon (Figure 1D), Achilles tendon was discontinuous with hypoechoic hemorrhage or hyperechoic high-fat adipose tissues in the gap between the proximal and distal ends, and swollen and thickened retracted tendon tissues.
Figure 1.
Imaging features of Achilles tendon injury on HFCDU before surgery. (A) Normal Achilles tendon with clear fiber texture (arrow) of the right foot of a 27-year-old male. (B) Achilles tendon after contusion of the right foot of a 29-year-old male: swelling, thickening, reduced echo, and no significant fiber loss (arrow). (C) Partial tear of Achilles tendon of the left foot of a 50-year-old female: discontinued fiber, hypoechoic area, and irregular edges (thin arrow); swollen and contracted ends (thick arrow). (D) Discontinued Achilles tendon fibers and retracted tendon ends of the left foot of a 42-year-old female (thick arrow); hypoechoic hemorrhage and hyperechoic fat tissues between ends (thin arrow).
Diagnostic evaluation
To evaluate the diagnostic value of HFCDU, the sensitivity, specificity, and accuracy were compared. Of the 68 suspected Achilles tendon injury cases, 53 cases showed abnormal ultrasound presentations and 15 cases were normal. Of the 15 cases with normal ultrasound presentations, 1 was Achilles tendon rupture. As shown in Table 2, of the 53 cases with abnormal ultrasound presentations, 25 cases were with partial tear (including 1 case had plantar tendon rupture and periapical hemorrhage and 1 case had acute Achilles tendonitis); 20 cases were with complete rapture (including 1 case had partial tear); and 8 cases were with laceration (including 1 case had Achilles tendon rupture). The tear sites of Achilles tendon were about 2–6 cm above the calcaneal attachment point. Compared with surgery or MRI results (Table 2), there were 49 cases of true-positive, 4 cases of false-positive, 14 cases of true-negative, and 1 case of false-negative. The sensitivity was 98% (49/50), specificity was 78% (14/18), and accuracy was 93% (63/68), suggesting that HFCDU has high diagnostic sensitivity, specificity, and accuracy in the diagnosis of Achilles tendon injury.
Table 2.
Ultrasound evaluations of Achilles tendon injury.
| Injury type | Number of cases | True positive | False positive |
|---|---|---|---|
| Laceration | 8 | 7 | 1 |
| Partial tear | 25 | 23 | 2 |
| Rupture | 20 | 19 | 1 |
| Total | 53 | 49 | 4 |
Imaging features of Achilles tendon injury on HFCDU after surgery
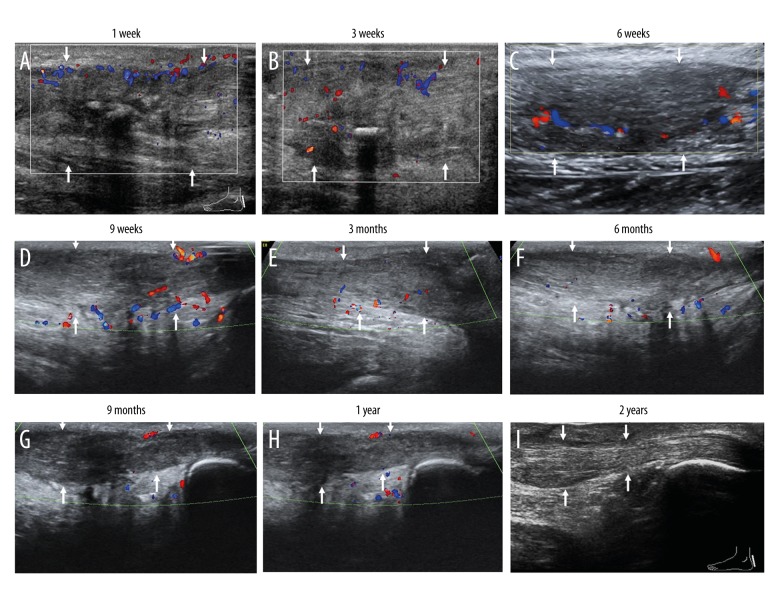
HFCDU was performed at weeks 1, 3, 6, and 9 and at months 3, 6, 9, 12, and 24 after the operation. Representative images are shown in Figure 2. The ultrasound at week 1 showed thickened Achilles tendon, hypoechoic and cluttered echo, and increased and disordered blood flow signal (Figure 2A). The ultrasound at week 3 (Figure 2B) showed thickened Achilles tendon, hypoechoic and uneven echo, continuous signal of Achilles tendon, and slightly reduced blood flow signal compared with that at week 1. The ultrasound at week 6 (Figure 2C) showed decreased thickening Achilles tendon, hypoechoic and uneven echo, continuous signal of Achilles tendon, and improved blood flow signal compared with that at week 3. The ultrasound at week 9 (Figure 2D) showed that the anteroposterior diameter of the Achilles tendon was smaller than that at week 6 after surgery, echo was less uniform, and Achilles tendon fiber continuity was good, with a little blood flow in the Achilles tendon by CDFI. The ultrasound at month 3 (Figure 2E) showed significantly reduced thickness of the Achilles tendon (still thicker than the healthy side), enhanced and even echo, and continuous signal of the Achilles tendon without blood flow signal. The ultrasound at month 6 (Figure 2F) showed no changes of thickness, close to normal and uniform echo, continuous and complete signal, and no significant blood flow signal. The ultrasound at month 9 (Figure 2G) revealed that the anteroposterior diameter of the Achilles tendon was smaller than that at month 6 after surgery, echo was less uniform, and Achilles tendon fiber continuity was complete. CDFI showed that the blood flow signal in the Achilles tendon was reduced. The ultrasound at month 12 (Figure 2H) showed smaller anteroposterior diameter of the Achilles tendon than at month 9 after surgery, enhanced echo, intact Achilles tendon fiber continuity, and decreased blood flow signal on CDFI. The ultrasound at month 24 (Figure 2I) showed reduced Achilles tendon thickness (still thicker than the healthy side), normal echo with patchy hyperecho, hypoecho on the back of the Achilles tendon, and no significant blood flow signal.
Figure 2.
Imaging features of Achilles tendon injury on HFCDU after surgery. HFCDU was performed at week 1 (A), week 3 (B), week 6 (C), week 9 (D), month 3 (E), month 6 (F), month 9 (G), month 12 (H), and month 24 (I) after the operation in the left foot of a 31-year-old male. Representative ultrasound images are shown. Arrows indicate the echo and the blood signals.
Treatment evaluation
To evaluate the treatment efficacy, the rehabilitation group was compared with the routine treatment group. One case had a secondary injury due to inappropriate training in the routine treatment group and was treated with another surgery (Figure 3). The overall treatment effects were excellent in 29 cases (69%), satisfactory in 11 cases (26.3%), and poor in 2 cases (4.7%). The combined excellent and satisfactory rate was 95.3% (Table 3). The treatment efficacy in the rehabilitation group was higher than that of the routine treatment group, but the difference was not statistically significant.
Figure 3.
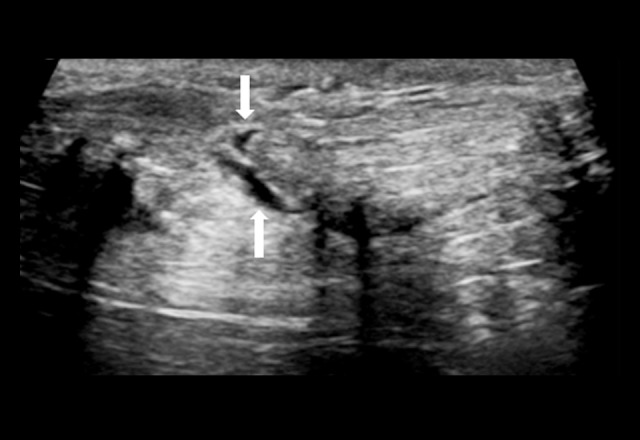
Secondary injury due to excessive exercise. The representative image of the right foot in a 33-year-old male is shown. Arrow refers to the continuously interrupted Achilles tendon fibers caused by the secondary injury and the irregular echo-free cracks.
Table 3.
The 1-year postoperative treatment efficacy between rehabilitation treatment group and routine treatment group.
| Excellent | Satisfactory | Bad | |
|---|---|---|---|
| Rehabilitation treatment group (n=21) | 18 | 3 | 0 |
| Routine treatment group (n=21) | 11 | 8 | 2 |
| P value | 0.0522 | 0.2722 | 0.6480 |
Of the 42 cases of Achilles tendon injury, 30 cases were acute injuries (less than 1 week between injury and operations), and 12 cases were old injury. The recovery of the acute injury was significantly better than that of the chronic injury (P<0.01) (Table 4). As shown in Table 5, the postoperative Achilles tendon recovery rate of the rehabilitation treatment group was significantly higher than that of the conventional treatment group at different time points (P<0.05). The Achilles tendon was obviously swollen after the operation. As shown in Table 6, the average anteroposterior diameter of the injured Achilles tendon was 14.7±3.6 mm and the transverse diameter was 28.2±4.5 mm. The average anteroposterior diameter of the healthy Achilles tendon was 6.2±0.8 mm, and the transverse diameter was 15.3±2.4 mm. Both diameters of the injured Achilles tendon were significantly higher than those of the healthy Achilles tendons (P<0.01).
Table 4.
The 1-year postoperative treatment efficacy between acute injury group and old injury group.
| Excellent | Satisfactory | Bad | |
|---|---|---|---|
| Acute injury group (n=30) | 28 | 2 | 0 |
| Old injury group (n=12) | 1 | 9 | 2 |
| P value | 0.001 | 0.001 | 0.0594 |
Table 5.
The postoperative ultrasound evaluations between rehabilitation treatment group and routine treatment group at different time points.
| Groups | Time | Excellent | Great | Good | Poor |
|---|---|---|---|---|---|
| Rehabilitation treatment group (n=21) | 1 week | 0 | 0 | 0 | 21 |
| 3 weeks | 0 | 0 | 1 | 20 | |
| 6 weeks | 0 | 2 | 7 | 12 | |
| 9 weeks | 2 | 7 | 9 | 3 | |
| 3 months | 9 | 11 | 1 | 0 | |
| 6 months | 17 | 4 | 0 | 0 | |
| 1 year | 20 | 1 | 0 | 0 | |
| Routine treatment group (n=21) | 1 week | 0 | 0 | 0 | 21 |
| 3 weeks | 0 | 0 | 0 | 21 | |
| 6 weeks | 0 | 1 | 5 | 15 | |
| 9 weeks | 1 | 3 | 11 | 6 | |
| 3 months | 5 | 13 | 3 | 0 | |
| 6 months | 9 | 10 | 1 | 0 | |
| 1 year | 17 | 4 | 0 | 0 |
Table 6.
Comparison of the anteroposterior diameter and the transverse diameter between the injured and the healthy Achilles tendon.
| The injured Achilles tendon (mm) | The healthy Achilles tendon (mm) | T value | P value | |
|---|---|---|---|---|
| The anteroposterior diameter | 14.7±3.6 | 6.2±0.8 | 26.26136 | 0.0001 |
| The transverse diameter | 28.2±4.5 | 15.3±2.4 | 31.82657 | 0.0001 |
Discussion
Achilles tendon injury is one of the most common types of ankle tendon injury, with increasing incidences in recent years [5,6]. This injury has various complications and is not easy to repair and heal due to the anatomical and physiological characteristics of the Achilles tendon and its surrounding tissues [7,8]. Therefore, early diagnosis and treatment are essential for its prognosis. Consistent with previous reports [9,10], our results showed that the sensitivity, specificity, and accuracy of HFCDU in the diagnosis of Achilles tendon injury were 98% (49/50), 78% (14/18), and 93% (63/68), respectively.
Of the 15 cases with normal ultrasound features, 1 case had a mild tear. The patient had the history of tendon paratyphoid inflammation, which manifested as a hypoechoic halo around the Achilles tendon and led to the misdiagnosis. Of the 8 cases of laceration, 1 case was focal Achilles tendonitis and tendon tear, showing as obviously enlarged Achilles tendon with focal hypoecho, blurred fiber texture, and no significant fiber loss. The echo was not obvious in the sites of tear, possibly due to the longer duration. Of the 25 cases of partial tear, 1 case had plantar tendon rupture with periapical hemorrhage; it showed liquid echo around the tendon and torn muscle fibers. Surgery showed the muscle fibers were ruptured plantar tendon, and the blood fell around the tendon, leading to hemorrhage. One case was acute Achilles tendonitis, presenting as focal swelling and reduced echo, similar to Achilles tendon tear. Of the 20 cases of complete rupture, 1 case was a partial tear due to its large tear scope, little tendon attachment, and interference of surrounding tissues.
In this study, the site of the Achilles tendon tear was 2–6 cm above the calcaneal attachment point, depending on its blood supply and biomechanical characteristics. The blood supply is rich at both ends of the Achilles tendon in adults. However, the number and diameter of blood vessels is less in the middle section; therefore, the poor blood supply leads to more injuries.
In this study, the ultrasound-guided treatment was 95.3% satisfactory or above in 42 cases of partial or complete rupture. Kainberger et al. [11] suggested ultrasound examination before the treatment selection, especially for those who choose not to have surgeries; otherwise, patients with a large gap between ruptured ends are at risk of being missed. The preoperative ultrasound examination can determine the types and extent of Achilles tendon injuries, locate the ends, and measure the gap size, helping physicians to decide on the surgical approach and reduce the scope of surgery [12].
In this study, in the routine treatment group, 1 case had a secondary injury due to excessive exercise, indicating the importance of a physician-guided rehabilitation program, including muscle strength, mobility, flexibility, and stability training [13].
Timely diagnosis is essential for subsequent treatment and better prognosis. Many old injuries result from failed conservative treatment, misdiagnosis, or improper handling. Of these, misdiagnosis is the most frequent, with a reported rate of 20–30% in the USA [14] and 66.7% in China. The misdiagnosis is due to 1) severe swelling or 2) mistakenly believed loss of plantar function and negative Thompson sign due to scar formation. Qiguang Zhang et al. [15] reported that un-sutured Achilles tendon rupture leads to triceps degeneration and tendon contracture after 1 week. Badalihan et al. [16] have shown the prognosis is better in patients with a rupture within 1 week than in those with longer duration. During a 5-year follow-up, the average plantar flexion of the ruptured side was 91% that of the healthy side in patients who received surgery within 1 week, while it was 74% in those who received surgery after 1 week, which is consistent with our study. Early detection and early treatment of Achilles tendon injury are of great importance [17].
Acute injury and chronic injury are distinct on ultrasound. The acute injury shows clear edges with great tendon sliding, whereas the chronic injury shows dull ends, extensive adhesion, and scar formation of subcutaneous fat, Achilles tendon, and surrounding tissues. The scar formation may be related with necrosis, hemorrhage, and exudation of the Achilles tendon and its surrounding tissues [16].
The time of Achilles tendon rehabilitation depends on the healing time, and usually requires about 6 weeks. Excise starting at 6 weeks may be late for minor injuries but early for severe injuries. We tried to identify the most suitable exercise time by ultrasound. The disordered echo and blood flow of injured sites at week 1 indicates severe inflammation or stapled stump. The swelling, increased echo, and decreased blood flow indicates the healing and reduced inflammation at week 3. The decreased tendon size and continuous fiber echo at week 6 indicates the recovery and warrants ankle joint flexion and extension training. Early training (before 6 weeks) may lead to secondary injury, as was found in our study. The tendon diameter was still increased at month 3; however, the functions improved. Thus, patients may retain quality of life. No differences were detected between month 3 and month 6. Calcification showed at the end of month 24. In conclusion, the continuity of tendon fiber and low blood flow signal on ultrasound allows weight-bearing exercise. The degree of exercise may increase as the blood flow disappears. It also shows the guidance of ultrasound on subsequent functional exercise.
The diameters of postoperative Achilles tendon increased, which is consistent with Bleakney’s study [18]. The largest diameter was 4 times the size of the health side in our study. The Achilles tendon thickness decreased over time with uniformity, less blood flow, and lower adhesion. These results were better in the rehabilitation group than in the routine treatment group. The increased tendon diameter, changed tendon shape, and hyperecho are associated with postoperative proliferation. The unclear tendon edges were related to its surrounding tissues. The decreased echo intensity, atypical fiber-like echo, focal hypoechoic areas, and fiber changes may be associated with hyperplasia, focal degeneration (including fat-like degeneration), and necrosis of small blood vessels in the Achilles tendon.
Our study is limited by its small sample size and short follow-up time. Further studies with larger sample sizes and longer follow-up times are warranted.
Conclusions
In conclusion, ultrasound has important clinical value in the diagnosis and treatment of Achilles tendon injury. Ultrasound can show the type and extent of Achilles tendon injury, and guide subsequent treatments. The intraoperative ultrasound guidance can reduce the injury and postoperative adhesion. Early postoperative monitoring is important in further exercise.
Footnotes
Source of support: Departmental sources
Conflict of interest
None.
References
- 1.Wong J, Barrass V, Maffulli N, et al. Quantitative review of operative and non-oprative management of Achilles tendon rupture. Am J Sports Med. 2002;30:565–75. doi: 10.1177/03635465020300041701. [DOI] [PubMed] [Google Scholar]
- 2.Yinger K, Mandelbaum BR, Almekinders LC, et al. Achilles rupture in the athlete. Current science and treatment. Clin Podiatr Med Surg. 2002;19:231–50. doi: 10.1016/s0891-8422(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 3.Khoury V, Cardinal E, Bureau NJ. Musculoskeletal sonography: Adynamic tool for usual and unusual disorders. Am J Roentgenol. 2007;188:63–73. doi: 10.2214/AJR.06.0579. [DOI] [PubMed] [Google Scholar]
- 4.Kuwade GT. Classification of tendon Achillis rupture with consideration of surgical repair techniques. J Foot Surg. 1990;29:361–65. [PubMed] [Google Scholar]
- 5.Popovic N, Lemaire R. Diagnosis and treatment of acute ruptures of the Achilles tendon Current concepts review. Acta Orthop Belg. 1999;65:458–71. [PubMed] [Google Scholar]
- 6.Martinelli B. Percutaneous repair of the Achilles tendon in athletes. Bull Hosp Joint Dis. 2000;59:149–52. [PubMed] [Google Scholar]
- 7.Lo IK, Kinkley A, Nonweiler B, et al. Operative versus nonopetative treatment of acute Achilles tendon ruptures a quantitative review. Clin J Sport Med. 1997;7:207–11. doi: 10.1097/00042752-199707000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Esenyel CZ, Tekin C, Cakar M, et al. Surgical treatment of the neglected achilles tendon rupture with Hyalonect. J Am Podiatr Med Assoc. 2014;104:434–43. doi: 10.7547/0003-0538-104.5.434. [DOI] [PubMed] [Google Scholar]
- 9.Khoury V, Cardinal E, Bureau NJ. Musculoskeletal sonography: Adynamic tool for usual and unusual disorders. Am J Roentgenol. 2007;188:63–73. doi: 10.2214/AJR.06.0579. [DOI] [PubMed] [Google Scholar]
- 10.Bleakney RR, Tallon C, Wong JK, et al. Long-term ultrasonographic features of the Achilles tendon after rupture. Clin J Sport Med. 2002;12:273–78. doi: 10.1097/00042752-200209000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Kainberger FM, Engel A, Barton P, et al. Injury of the Achilles tendon: Diagnosis with sonography. Am J Roentgenol. 1990;155:1031–36. doi: 10.2214/ajr.155.5.2120931. [DOI] [PubMed] [Google Scholar]
- 12.Maquirriain J. Achilles tendon rupture: avoiding tendon lengthening during surgical repair and rehabilitation. Yale J Biol Med. 2011;84:289–300. [PMC free article] [PubMed] [Google Scholar]
- 13.Donaldson PR. Surgical versus nonsurgical treatment of acute Achilles tendon rupture. Clin J Sport Med. 2012;22:169–70. doi: 10.1097/JSM.0b013e31824c2b2c. [DOI] [PubMed] [Google Scholar]
- 14.Maffull N. The clinical diagnosis of subcutaneoust ear of the Achilles tendon a prospective study in 174 patients. Am J Med. 1998;26:266–70. doi: 10.1177/03635465980260021801. [DOI] [PubMed] [Google Scholar]
- 15.Zhang QG, Yu HX. [Repair of 12 cases of old Achilles tendon rupture with fibular long tendon displacement]. Zhong Guo Xiu Fu Chong Jian Wai Ke Za Zhi. 2002;16:365. [in Chinese] [Google Scholar]
- 16.Badalihan A, Aihemaiti A, Shawutali N, et al. Outcome of a one-stage tensile stress surgical technique and early postoperative rehabilitation in the treatment of neglected Achilles tendon rupture. J Foot Ankle Surg. 2015;54:153–59. doi: 10.1053/j.jfas.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Tay D, Lin HA, Tan BS, et al. Chronic Achilles tendon rupture treated with two turndown flaps and flexor halluces longus augmentation-two-year clinical outcome. Ann Acad Med Singapore. 2010;39:58–60. [PubMed] [Google Scholar]
- 18.Bleakney R, Tallon C, Wong JK, et al. Long-term ultrasonographic features of the Achilles tendon after rupture. Clin J Sport Med. 2002;12:273–78. doi: 10.1097/00042752-200209000-00003. [DOI] [PubMed] [Google Scholar]