To the Editor
Patients evaluated in the emergency department (ED) with symptoms suggestive of acute coronary syndrome (ACS) may experience significant psychological stress. [1–2] In addition to ED factors such as patient volume [3] and hallway care [4], patients’ retrospectively reported feelings of fear and vulnerability during ED evaluation for a life threatening illness (i.e. threat perception) has also been found to be associated with increased posttraumatic symptoms (PSS) at follow-up. [5,6] A recent meta-analysis found 12% of ACS patients subsequently screen positive for PTSD, and that elevated PSS after ACS are associated with increased risk for recurrent cardiac events, medication nonadherence and mortality. [7,8] While clinicians may be reassured, after evaluation, that risk for a serious cardiac event or mortality is low in some patients, for many of these patients the subjective fear of a potentially life threatening illness may still be present, regardless of actual diagnosis. To date, no study has assessed the frequency or intensity of threat perceptions in patients evaluated for ACS during the evaluation period, nor compared threat perceptions across those who ultimately are found to have an actual ACS event versus patients evaluated and discharged with non-ACS events. The goal of our study was to evaluate the frequency of threat perception in a cohort of ED patients evaluated for potential ACS and to compare threat perception severity between patients found to have ACS versus patients found not to have an ACS event after hospitalization.
This study was conducted as part of an ongoing observational cohort study of patients presenting to the ED for evaluation of suspected ACS, the REactions to Acute Care and Hospitalization (REACH). 1000 patients were enrolled at a single site urban academic medical center. English and Spanish speaking patients were eligible if they had a provisional diagnosis of “probable ACS” by the treating ED physician. Exclusion criteria included ST elevations on electrocardiogram, psychiatric intervention, or unavailable for 1-year followup.
In the ED, participants’ perceptions of life threat and personal vulnerability in response to the suspected ACS event were assessed using 12 item scale of threat perception by Ozer et al. [9] Responses were made on a 4-point Likert scale ranging from “not at all” to “extremely”; responses to these items had good internal consistency (Cronbach’s α=.79). Hospital discharge diagnosis was determined by review of the medical record by a committee of 2 cardiologists and 1 emergency physician.
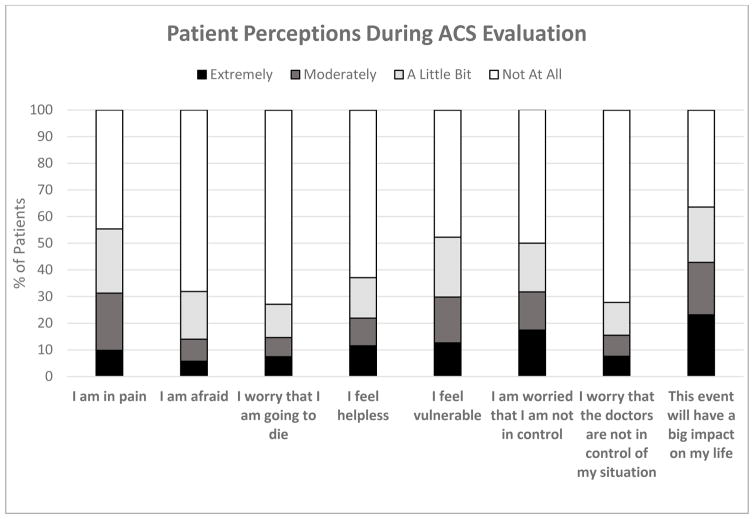
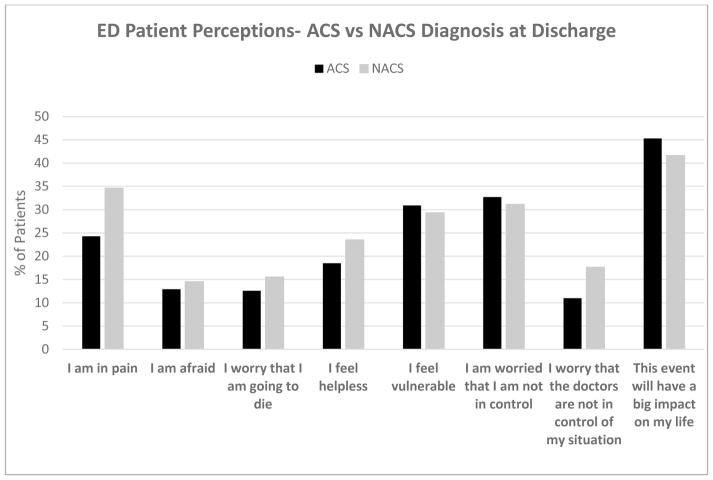
Characteristics for the 1000 individuals are presented in Table 1. Of the 1,000 enrolled participants, the frequency of threat perception scores of 3 (moderately) or 4 (extremely) for individual items are shown in Figure 1. ED threat perception scores for the ACS versus non-ACS groups are shown in Figure 2. ED threat perception scores did not significantly differ between ACS and non-ACS diagnosed patients, except for “I am in pain” (t= 3.856, p <0.001) and “I worry that the doctors are not in control of my situation” (t=3.058, p<0.002). In both cases, non-ACS patients had higher average ED threat perception scores compared to ACS patients.
Table 1.
Patient Characteristics n=1000
| Mean | Std. Deviation | Minimum | Maximum | |
|---|---|---|---|---|
| Age at enrollment** | 60.8 | 13.154 | 22 | 100 |
| Male Sex | 54% | |||
| Hispanic Ethnicity | 57% | |||
| Confirmed ACS | 37% |
Figure 1.
Patient threat perceptions reported at interview during ACS evaluation in the ED.
Figure 2.
Comparison of ED threat perceptions (score 3 or 4) between ACS and non-ACS diagnosed patients.
We found the presence of elevated levels of threat perception in patients evaluated for ACS, both in individuals determined to have actual ACS events, as well as participants not found to have ACS. Elevated threat perception levels have been found to be associated with increased risk for development of PTSD. The presence of similar levels of threat perception in both groups of ACS and non-ACS patients in our study highlights the importance of addressing the subjective fear and stress that patients may experience while in the ED. While clinicians may be reassured, after evaluation, that the risk for acute ACS event is low, for many patients the subjective fear of potentially suffering a life threatening illness may result in the development of negative psychological outcomes irrespective of actual diagnosis. Our work underscores the importance of addressing these psychological factors during medical evaluation and treatment.
This was a single-site study limited to ED patients presenting with ACS symptoms, so findings may not be generalizable to different patient populations. Future work using alternative stress assessment strategies such as autonomic monitoring may build on our work to yield additional insight into PTSD risk development.
The evaluation of potentially life threatening illnesses such as ACS is extremely common in many EDs. This is the first study to uncover the psychological state of patients during evaluation for ACS, and the degree to which the experience impacts patients may be surprising. Future work elaborating on the subjective patient experience while undergoing evaluation in the ED may help improve patients’ experience and guide the development of risk stratification strategies and interventions to optimize medical care as well as reduce the development of negative psychological outcomes for patients cared for in the acute setting.
Acknowledgments
Grant: This work was supported by grants HL117832, HL123368, and HL128310 from NIH/NHLBI.
Footnotes
Meetings: To be presented at the Society for Academic Emergency Medicine Annual Conference Orlando, Fl May 22, 2017 (submitted for oral presentation)
References
- 1.Gander ML, von Kanel R. Myocardial infarction and posttraumatic stress disorder: frequency, outcome, and atherosclerotic mechanisms. Eur J Cardiovasc Prev Rehabil. 2006;13:165–172. doi: 10.1097/01.hjr.0000214606.60995.46. [DOI] [PubMed] [Google Scholar]
- 2.Wiedemar L, Schmid JP, Müller J. Prevalence and predictors of posttraumatic stress disorder in patients with acute myocardial infarction. Heart Lung. 2008;37(2):113–121. doi: 10.1016/j.hrtlng.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 3.Edmondson D, Shimbo D, Ye S, Wyer P, Davidson KW. The association of emergency department crowding during treatment for acute coronary syndrome with subsequent posttraumatic stress disorder symptoms. JAMA internal medicine. 2013;173(6):472–475. doi: 10.1001/jamainternmed.2013.2536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang BP, Carter E, Suh E, Kronish I, Edmondson D. Patient Treatment in Emergency Department Hallways and Patient Perception of Clinician-Patient Communication. American Journal of Emergency Medicine. 2016;34(6):1163–4. doi: 10.1016/j.ajem.2016.02.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sumner JA, Kronish IM, Pietrzak RH, Shimbo D, Shaffer JA, Parsons FE, et al. Dimensional structure and correlates of posttraumatic stress symptoms following suspected acute coronary syndrome. Journal of affective disorders. 2015;186:178–185. doi: 10.1016/j.jad.2015.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang BP, Sumner JA, Haerizadeh M, Carter E, Edmondson D. Perceived clinician-patient communication in the emergency department and subsequent post-traumatic stress symptoms in patients evaluated for acute coronary syndrome. Emergency Medicine Journal. 2016;33(9):626–31. doi: 10.1136/emermed-2015-205473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Edmondson D, Rieckmann N, Shaffer JA, Schwartz JE, Burg MM, Davidson KW, et al. Posttraumatic stress due to an acute coronary syndrome increases risk of 42-month major adverse cardiac events and all-cause mortality. Journal of psychiatric research. 2011;45(12):1621–1626. doi: 10.1016/j.jpsychires.2011.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kronish IM, Ye S. Adherence to cardiovascular medications: lessons learned and future directions. Progress in cardiovascular diseases. 2013;55(6):590–600. doi: 10.1016/j.pcad.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ozer E, Best JS, Weiss DS, et al. Predictors of post-traumatic stress disorder in adults: a meta-analysis. Psychol Bull. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]