Description
A 41-year-old man with a history of crystal methamphetamine and alcohol abuse had progressive fever, nausea, headache, gait difficulties and seizures over 4 weeks while living in California and Mexico. He was diagnosed with meningitis, treated with antibacterials and discharged to a rehabilitation facility. One month later, he had recurrent symptoms with weakness of both arms and legs. Neuroimaging revealed extensive basilar pachymeningitis, leptomeningitis, hydrocephalus (figure 1A), cervical epidural enhancement (figure 1B) and a non-enhancing central cervical intramedullary lesion spanning C1 through C6 (figure 1C). He was started on fluconazole 800 mg daily due to his travel history, although a serum antibody test was negative by double immunodiffusion (<1:1). A ventriculoperitoneal shunt was placed for hydrocephalus and he was discharged but remained quadriplegic. Two weeks later, he developed confusion and was found to have bilateral subcortical strokes on MRI with evidence of arteritis on MR angiogram (figure 1D). He was then transferred to our hospital and amphotericin was added. Testing for HIV, tuberculosis and immunosuppression was negative. He developed worsening hydrocephalus (figure 1E) and died after interventions were withdrawn. Cerebrospinal fluid culture (figure 1F) and coccidioides IgG antibody by ELISA of 3.1 ng/mL later confirmed the diagnosis of coccidioidomycosis
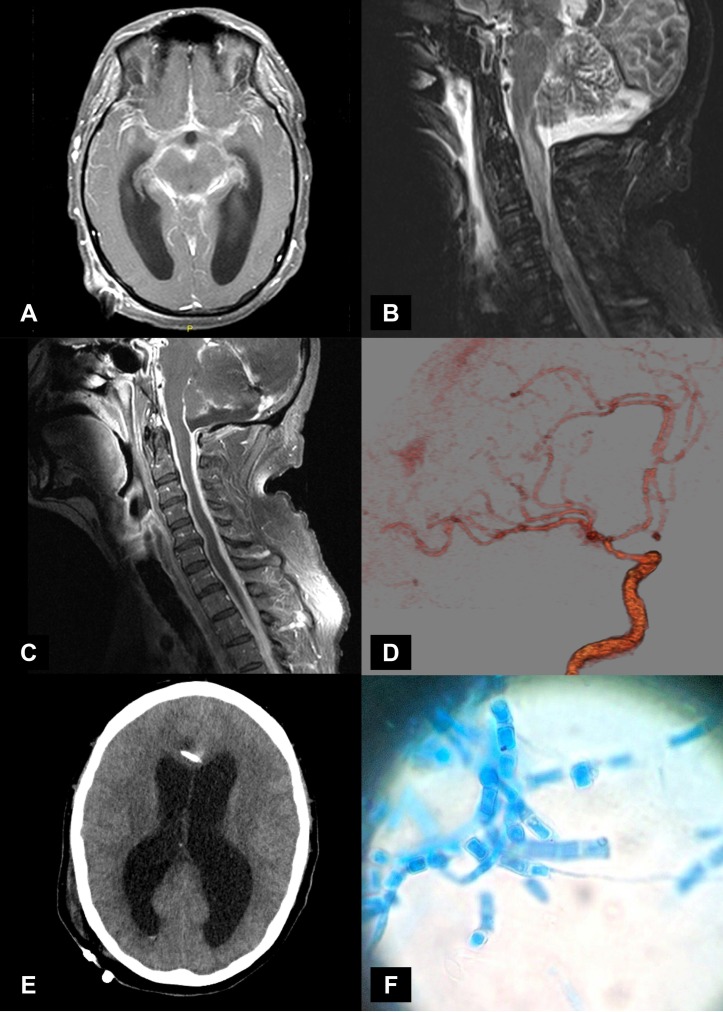
Figure 1.
(A) MRI of brain with gadolinium, axial view showing enhancement consistent with extensive basilar pachymeningitis, and leptomeningitis. Also seen is hydrocephalus. (B) MRI of cervical spine, T2 -weighted short-tau inversion recovery sequence, sagittal view, with a central intramedullary lesion spanning from C1 through C6 of the cervical spinal cord. (C) MRI of cervical spine, T1 sagittal view with gadolinium shows extensive epidural enhancement. No enhancement of the intramedullary lesion is seen. (D) MRA of head, a reconstruction of the left anterior circulation shows a beading pattern consistent with arteritis. (E) CT of head without contrast, an axial view showing worsening hydrocephalus. (F) Cerebrospinal fluid culture showing thin, hyaline, septate hyphae and barrel-shaped arthroconidia (lactophenol cotton blue stain) consistent with coccidioides.
We present a case of an intramedullary spinal cord lesion with quadriplegia from coccidioides infection in an immunocompetent host. Disseminated coccidioidomycosis is seen in only 1%–5% of infected patients.1 2 Recognising the complication of spinal cord intramedullary involvement is important as delayed diagnosis and treatment can lead to poor outcomes.3
Learning points.
Even in an immunocompetent host, intramedullary spinal cord involvement can be a manifestation of disseminated coccidioidomycosis and accompany the more recognisable presentation of coccidioidal meningitis.
Delays in the diagnosis and treatment of coccidioidal meningitis are not uncommon, but as seen in this case can lead to further neurological complications such as hydrocephalus and spinal cord involvement.
Footnotes
Contributors: JMN and TK contributed to the conception, design, drafting and revisions of the article; acquisition, analysis and interpretation of the data; final approval of the article and the agreement to be accountable for the accuracy and integrity of its content. RN contributed to the critical revisions to the article; acquisition, analysis and interpretation of the data; final approval of the article and the agreement to be accountable for the accuracy and integrity of its content.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Tan LA, Kasliwal MK, Nag S, et al. Rapidly progressive quadriparesis heralding disseminated coccidioidomycosis in an immunocompetent patient. J Clin Neurosci 2014;21:1049–51. 10.1016/j.jocn.2013.07.040 [DOI] [PubMed] [Google Scholar]
- 2.Bajema KL, Dalesandro MF, Fredricks DN, et al. Disseminated coccidioidomycosis presenting with intramedullary spinal cord abscesses: Management challenges. Med Mycol Case Rep 2017;15:1–4. 10.1016/j.mmcr.2016.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lammering JC, Iv M, Gupta N, et al. Imaging spectrum of CNS coccidioidomycosis: prevalence and significance of concurrent brain and spinal disease. AJR Am J Roentgenol 2013;200:1334–46. 10.2214/AJR.12.9264 [DOI] [PubMed] [Google Scholar]