Abstract
Purpose:
Conduct of cancer clinical trials requires coordination and cooperation among research and clinic teams. Diffusion of and confusion about responsibility may occur if team members’ perceptions of roles and objectives do not align. These factors are critical to the success of cancer centers but are poorly studied.
Methods:
We developed a survey adapting components of the Adapted Team Climate Inventory, Measure of Team Identification, and Measure of In-Group Bias. Surveys were administered to research and clinic staff at a National Cancer Institute–designated comprehensive cancer center. Data were analyzed using descriptive statistics, t tests, and analyses of variance.
Results:
Responses were received from 105 staff (clinic, n = 55; research, n = 50; 61% response rate). Compared with clinic staff, research staff identified more strongly with their own group (P < .01) but less strongly with the overall cancer center (P = .02). Both clinic staff and research staff viewed their own group’s goals as clearer than those of the other group (P < .01) and felt that members of their groups interacted and shared information within (P < .01) and across (P < .01) groups more than the other group did. Research staff perceived daily outcomes as more important than did clinic staff (P = .05), specifically research-related outcomes (P = .07).
Conclusion:
Although there are many similarities between clinic and research teams, we also identified key differences, including perceptions of goal clarity and sharing, understanding and alignment with cancer center goals, and importance of outcomes. Future studies should examine how variation in perceptions and group dynamics between clinic and research teams may impact function and processes of cancer care.
INTRODUCTION
Cancer clinical trials address important clinical questions, lead to therapeutic advances, provide patients with access to promising treatments, and are intended to deliver the highest level of cancer care available.1,2 Although the intricacies of study design, regulatory approval, and activation have received considerable attention, complexities do not end once patients initiate study therapy and procedures. Clinical trials must address an increasing number of directives to assess safety and the growing drive to maximize scientific yield.3,4 At the same time, standard oncology clinical care has intensified as a result of the growing number of available therapies, demands to see more patients in clinic and infusion facilities, and increasing electronic documentation and communication requirements.5,6 Resulting functional silos have been identified as a challenge to effective coordination of tasks,7-10 but how they specifically affect clinical research operations remains unclear.
Careful and continuous coordination between institutional clinic teams and research teams is needed to optimize patient safety and experience on trial protocols and to generate high-quality clinical data.11 These teams must divide tasks, maintain open lines of communication, and respond to unforeseen developments. Because clinical research procedures are constantly in flux—with new trials opening, older trials closing, and ongoing trials undergoing modifications to study design and procedures—clinic and research personnel must maintain high levels of flexibility, adaptation, and cooperation.
Meeting these goals requires establishment of multiteam systems. Multiteam systems are defined as two or more teams that interface directly and interdependently in response to environmental contingencies toward the accomplishment of collective goals.12,13 For cancer clinical trials, multiteam systems face a number of challenges. Misalignment of goals and lack of communication may arise because the research team focuses on implementation of study protocols, whereas the clinic team focuses on daily care routines. Diffusion of and confusion about responsibility may occur if perceptions of roles and objectives, and coordination of individual tasks in this broader context, do not align. Team members who fail to recognize they are part of this larger multiteam system may engage in rivalries that hinder cooperation and cohesion. Team members who believe key tasks are unimportant or not their responsibility may leave tasks unaddressed to the detriment of shared goals of high-quality cancer care.
Research on multiteam systems has previously demonstrated how perceptions can impact behaviors and impair such coordination and collaboration.12,14,15 Generally, studies applying a social identity perspective have focused on perception of important characteristics of a team’s own group (ie, in-group) and a corresponding other group (ie, out-group). In this approach, memberships in social groups or categories are integral to self-conception. They also determine how people perceive, interpret, and respond to their social situation. When group memberships are made salient, perception and behavior become group based rather than personalized or individuated.16 That is, when people define and evaluate themselves in terms of a self-inclusive social category or in-group, they accentuate similarities among their members but accentuate differences between their members and members of other groups. Moreover, they favor tasks, roles, and responsibilities associated with the in-group over those associated with the out-group to achieve and reinforce a positive social identity. Group involvement and identification also evoke an inclination to render explicit between-group comparisons that make social identity salient to daily life.17 Theoretical accounts of intergroup relations argue that status and power asymmetries between groups impact both the extent of in-group identification and the form of group behavior displayed.18,19 For instance, subjective beliefs about social structure determine whether group members use individual or collective strategies to achieve psychological or actual status improvement.11,15,20,21
Although these dynamics are well described in the team science literature and have been demonstrated in numerous settings, including corporate cultures and professional sports,14,16 there is scant information on their application to health care, particularly to the conduct of clinical trials. Therefore, we adapted validated instruments from the team science field22-24 for use in surveys of clinic staff and clinical research personnel at a National Cancer Institute–designated comprehensive cancer center. Our primary goal was to describe how members of the research team and clinic team perceive their own group (the in-group), the opposite group (the out-group), and the overall cancer center.
METHODS
Study Setting and Sample
The Harold C. Simmons Comprehensive Cancer Center is a freestanding clinical, research, and educational facility within The University of Texas Southwestern Medical Center. Clinic staff are organized into hematology-oncology, radiation oncology, surgical oncology, and gynecologic oncology clinics. Hematology-oncology clinic staff are further categorized as outpatient clinic or infusion staff. The Simmons Clinical Research Office, which is organized by disease site, includes clinical research coordinators and managers; protocol and regulatory team staff; administrative, compliance, and financial support staff; and administrative managers.
Survey Development
This study was approved by The University of Texas Southwestern Institutional Review Board (STU 052016-107). Survey items were designed to assess the following five domains: group identity; perceived objectives and goals; perceived information sharing and interaction frequency; perceived group homogeneity; and perceived contributions to outcomes. Survey questions were taken from previous empirical research on social identity theory and adapted to the current setting. Using items from the Adapted Team Climate Inventory,16,18 the Measure of Team Identification,17 and the Measure of In-Group Bias,19 we assessed participants’ identification with their specific in-group (clinic or research team) and the Simmons Cancer Center as their common in-group; participants’ perceptions of goals and objectives and the extent to which they believed that those objectives are understood by members of their in-group and out-group; and participants’ perceived information sharing and interaction frequency within their in-group and the out-group. To explore in-group homogeneity and favoritism effects, items related to perceived heterogeneity and an overt and subtle measure of in-group and out-group performance were included. A detailed explanation of survey content and listing of survey items is provided in the Data Supplement.
We developed two versions (clinic team and research team) of the questionnaire, which differed only in the referent group label within survey items. Unless indicated otherwise, all items were measured using a 7-point Likert scale with the following labels: agree strongly (7 points), agree (6 points), somewhat agree (5 points), undecided/I don’t know (4 points), disagree somewhat (3 points), disagree (2 points), and disagree strongly (1 point). Thus, higher scores indicate higher agreement with a statement.
Survey Administration and Data Collection
One author (S.G.) administered the survey over a 2-week period in July and August 2016. We distributed surveys to all eligible staff in the cancer center (N = 171) on the basis of human resources records of categorical designations (ie, clinical, nonclinical) for relevant employment positions. For most research staff, surveys were distributed and completed during regularly scheduled team meetings. For clinic staff, surveys were generally completed and returned individually. Survey responses were entered into a Microsoft Excel spreadsheet (Microsoft, Redmond, WA). Data accuracy was cross-checked with survey documents by two investigators (S.G. and D.E.G.).
Statistical Analysis
The principal measures of group identification and member perceptions included several items. As in previous studies,16-19 before aggregating items assumed to measure the same construct, we first determined Cronbach’s α as a measure of internal consistency. Second, we computed a composite score for each participant by averaging answers across items measuring the same construct. Third, we inspected descriptive statistics such as the mean and standard deviations (SDs) of scales across all participants and separately for research and clinic teams. Finally, to test for systematic differences between members of the clinic and research teams in perceptions of their in-group, the out-group, and the cancer center as their common in-group, we conducted t tests and analyses of variance.
RESULTS
In total, 105 staff members participated in the study (research, n = 55; clinic, n = 50). The response rates were 87% among research staff and 46% among clinical staff, with an overall response rate of 61%. Mean age was 38 years (SD, 11 years), and 80% of participants were women. On average, participants had 10.8 years of professional experience (SD, 8.8 years) and had been in their current position for 3.3 years (SD, 4.1 years). Although the lower bound for minimum overall professional experience differed between clinic and research groups (2.0 v 12.0 months, respectively), we found no significant differences for any of these characteristics. Cronbach’s α for all scales used in the study was > .7, indicating acceptable measure reliability.
Group Identity
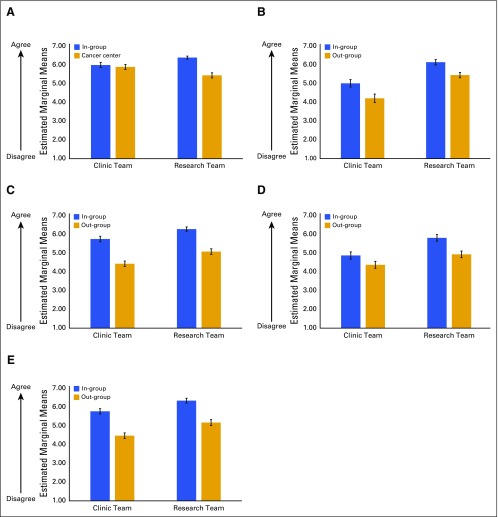
Group identity was measured for participants’ own team (in-group) and for the cancer center using absolute measures of centrality and satisfaction and measures of relative solidarity. The main variables are listed in Table 1. Both the research team and the clinic team indicated that they identify with their in-group as well as with the cancer center. However, there were substantial differences in how strongly members identified with their teams. As shown in Figure 1A, there were no substantial differences in how members of the clinic team identified with their in-group and with the cancer center, whereas members of the research team identified more strongly with their own team than with the cancer center. Members of the research team identified more strongly with their own group than did members of the clinic team but identified less strongly with the overall cancer center. Measures of relative group solidarity revealed that members of the research team and the clinic team expressed more solidarity with their in-group than with the out-group, as well as more solidarity with their own group than with the cancer center.
Table 1.
Main Survey Variables
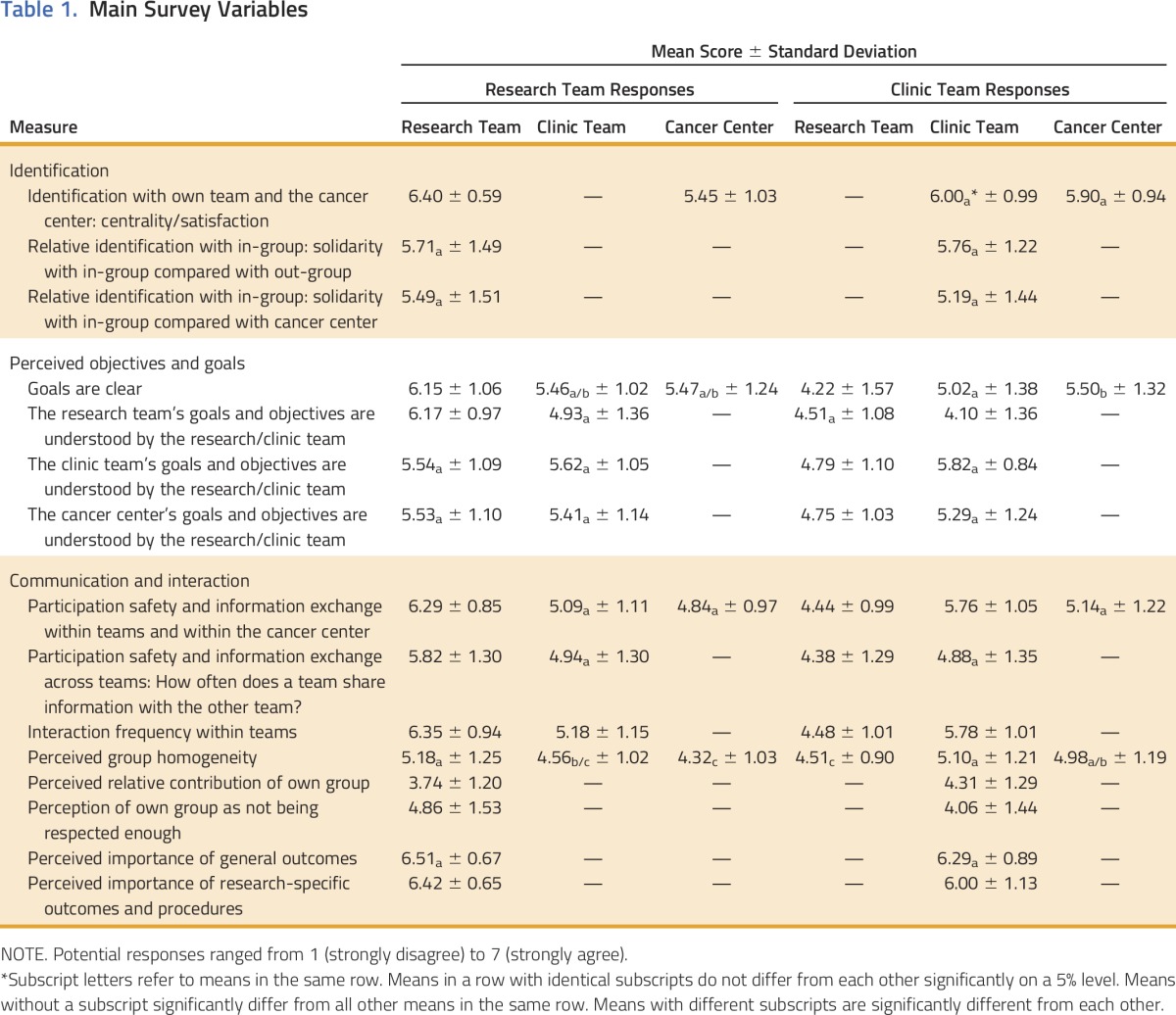
Fig 1.
Graphical representation of clinic team and research team perceptions. (A) Identification with own group relative to the cancer center. The research team identified more strongly with itself than with the cancer center (P < .05). Compared with the clinic team, the research team identified more strongly with itself (P < .01) and less strongly with the cancer center (P = .02). (B) Clarity of in-group and out-group goals. Both the clinic team and the research team perceived their goals to be more clear than the other team’s goals (P < .01). Compared with the clinic team, the research team perceived both teams’ goals to be more clear (P < .01). (C) Within-group information sharing. Both the clinic team and the research team perceived that they share information within their group more than the other group does (P < .01). Compared with the clinic team, the research team perceived both teams to have more within-group information sharing (P < .01). (D) Information sharing with other group. Both teams thought that their team shared more information with the respective out-group than vice versa. (E) Extent of within-group interaction. Both the clinic team and the research team perceived that they interact within their group more than the other group does (P < .01). Compared with the clinic team, the research team perceived both teams to have more within-group interaction (P < .05).
Objectives and Goals
Both teams perceived that the goals of their own group were clearer than the goals of the out-group (Fig 1B). Research team members thought that their team’s goals were clearer overall than did clinic team members. Both teams thought that cancer center goals were less clear than their own team’s goals. Research team and clinic team members perceived that they themselves better understood their team’s goals than did members of the out-group.
The research team indicated that both teams understood the goals of the cancer center to a similar extent. However, the clinic team indicated that the cancer center goals were less well understood by the research team than by the clinic team.
Information Sharing and Interaction Frequency
In general, perceptions of information sharing and interaction frequency mirrored those of objectives and goals. Both teams perceived more information exchange among members of their own group than among members of the out-group (Fig 1C). Both teams felt that there was more information exchange within their own group than with the cancer center. Both teams thought that their team shared more information with the respective out-group than vice versa (Table 1; Fig 1D) and that members of their own group interacted more frequently with each other than do members of the other group (Fig 1E).
Group Homogeneity
Both groups displayed an in-group homogeneity effect; that is, members perceived their own group to be more homogenous than the out-group.
Contributions to Outcomes
Neither group thought that they contributed substantially more or that their work was more important than the other group. Both groups agreed that the specified general clinic routines and research-specific outcomes were important (mean scores > 6 on the 7-point scale). Although members of the research and clinic teams did not differ in the perceived importance of general outcomes, the research team tended to evaluate research-specific outcomes as more important than did clinic team members. The research team also indicated that members of their group were not respected enough compared with members of the clinic team.
DISCUSSION
The issue of teams in cancer care has emerged as a major focus for clinicians and researchers alike.20,21 Simultaneous yet frequently conflicting pressures of complex and urgent medical decisions, coordination between multidisciplinary clinical services, and expectations to save time and cut costs render oncology practice a setting where team functions and interactions are critical. This is particularly apparent in the evaluation, enrollment, and treatment of patients on cancer clinical trials, which impose numerous additional expectations and guidelines onto an already stressful environment.11 How clinic teams and research teams perceive themselves, each other, their work setting, and their roles represent critical but understudied considerations.
We used a social identity approach to provide a theoretical framework and measurements to describe, analyze, and explicate challenges between teams. Although there were many similarities between the clinic and research teams, we also identified key differences. Compared with the clinic team, members of the research team identified more strongly with their own group and less strongly with the cancer center. Although both groups felt their goals were clearer than those of the other group or of the cancer center, these differences in perceptions were stronger among the research team. Clinic team members perceived that the goals of the cancer center were less understood by the research team than by themselves. Although both teams perceived their group to be more homogeneous than the other, the research team indicated that it received less respect than the clinic team.
Perceived group homogeneity measures the extent to which members of a group are believed to be similar to each other. Usually, groups display an out-group homogeneity effect; that is, members who identify with their group tend to perceive out-groups as more homogeneous than their own group, their in-group. We observed the reverse pattern, which is more commonly seen when group identity is under threat (eg, when a minority group perceives merging with the majority will come at the loss of what made the minority distinct).
What underlies the perceived challenges and threats between clinic and research teams revealed by our study? As previously observed,11 most members of the clinic and research teams report that they predominantly interact with members of their own team. Some research team members have considerable time during the work week when they are not directly involved in patient care or located in the clinic setting. Although this less stressful and less fractured environment may strengthen team bonds, it may also lead to a sense of isolation from the overall cancer center as a common organization. Furthermore, at our institution, research staff are divided clearly into small groups according to disease focus. These groups share common office space and work longitudinally over time with a specific group of providers. By contrast, the clinic team is not divided into such small units, and individual clinic staff may work with many providers caring for patients with a diverse array of cancer types.
In principle, participation in an overall parent organization would presuppose that a multiteam system would emerge organically (ie, clinical and research teams recognize they are both in something together). However, our findings suggest that multiteam systems cannot be presumed to evolve or persist without explicit cultivation. Indeed, the current study suggests that individuals tend toward the local (the specific in-group) at the expense of both the out-group and the larger parent group (in this case, the cancer center). In systems literature, this resembles a long-standing tension between core and periphery (eg, headquarters v regional offices).25
Research in other professional areas has revealed that members with strong social identities display a host of behaviors in situations when group membership is made salient, in particular when group identities are threatened. Those behaviors include differences in mutual evaluations and individual support as well as in communication behaviors. In extreme cases, they can also fuel intergroup conflict.19,22 Although no generalized effects of in-group favoritism were observed in the current study, on the basis of prior research, it seems possible that our observed in-group/out-group effects may limit cooperation and collaboration.
As a first step, our study focused on differences in staff members’ perceptions of group identifications, goals, and communication practices. The identified differences in clinic team and research team perceptions may provide one approach to explain challenges and lack of coordination that have been observed among cancer center team members.11 As with other multiteam settings, cancer center organizational and team leaders will need to work actively to countermand those dynamics.26 Staff onboarding processes, training, and coaching will need to explicitly identify and promote collective membership in the multiteam system.27-29 Cross-training activities and cooperative team-building exercises could be leveraged, as could stronger identification with the overall cancer center.30 Systems of reward and recognition that support collaboration and cooperation between clinic and research team members could be implemented.31,32 Evidence-based interventions from organizational sciences should be tested and adapted.33,34
The key limitation of the current study was the single-center setting. Clinic and research team employees at other cancer centers may be organized and function differently, producing different perceptions and intergroup dynamics. However, tensions identified in the present analysis are likely not only applicable to other institutions but also may be generalizable to other medical fields outside of cancer. Indeed, suboptimal relations between clinic and research teams have been reported in multiple settings, leading to job dissatisfaction, high turnover, and burnout.26,35,36 Although the overall response rate was high (even for an internal survey), the research team response rate was much higher than for the clinic team. This difference could reflect the different settings in which the survey was administered (group setting for research, individual setting for clinic) or the research team’s greater inclination to participate in research (ie, survey completion). How these different response rates influence our findings is not clear. One might imagine that those clinic team members who completed the survey represented a particularly motivated subpopulation. That motivation could result from strong feelings about their group, the other group, the cancer center, or any permutation of these entities. Those strong feelings could tend toward either the positive or the negative. Finally, through the current study, one cannot determine the extent to which in-group and out-group perceptions are fundamental to care coordination, a question that requires additional investigation.
In an era of value-based cancer care reform, such as the Medicare Access and CHIP Reauthorization Act of 2015, Merit-Based Incentive Payment System, and the oncology care model,37,38 integration of clinical research with clinical care staff roles and processes through multiteam systems is critical. Such integrated care team models hinge on members’ perceptions as members of broader multiteam systems.39-41 The current study provides early insight into these perceptions. As a next step, future studies should examine how such variation in perceptions and group dynamics between clinic and research teams may impact function and processes of high-quality care delivery for patients with cancer.
ACKNOWLEDGMENT
This study was derived from participation in the National Cancer Institute–American Society of Clinical Oncology Teams in Cancer Care Delivery Project. Supported in part by National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases Short-Term Institutional Research Training Grant No. 5 T35 DK 66141-10 (to S.G.); The University of Texas Southwestern Center for Patient-Centered Outcomes Research Grant No. AHRQ 1R24HS022418-01 (to S.J.C.L.); a National Cancer Institute Midcareer Investigator Award in Patient-Oriented Research (No. K24CA201543-01; to D.E.G.); The University of Texas Southwestern National Cancer Institute National Clinical Trials Network Lead Academic Site Grant No. 5U10CA180870-02 (to D.E.G.); and the Harold C. Simmons Comprehensive Cancer Center, supported in part by a National Cancer Institute Cancer Center Support Grant No. 1P30 CA142543-03. We thank Dru Gray for assistance with manuscript preparation, and Helen Mayo, MLS, from The University of Texas Southwestern Medical Library, for assistance with literature searches.
AUTHOR CONTRIBUTIONS
Conception and design: Torsten Reimer, Simon J. Craddock Lee, David E. Gerber
Administrative support: Simon J. Craddock Lee, David E. Gerber
Provision of study materials or patients: Simon J. Craddock Lee
Collection and assembly of data: Sandra Garcia, Mary Gill, Tobi Duncan, Erin L. Williams
Data analysis and interpretation: Torsten Reimer, Simon J. Craddock Lee, David E. Gerber
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Cancer Center Clinic and Research Team Perceptions of Identity and Interactions
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jop/site/ifc/journal-policies.html.
Torsten Reimer
No relationship to disclose
Simon J. Craddock Lee
No relationship to disclose
Sandra Garcia
No relationship to disclose
Mary Gill
No relationship to disclose
Tobi Duncan
Speakers' Bureau: Merck
Erin L. Williams
No relationship to disclose
David E. Gerber
Stock or Other Ownership: Gilead Sciences
Consulting or Advisory Role: Samsung Bioepis, Bristol-Myers Squibb
Speakers' Bureau: Bristol-Myers Squibb
Research Funding: Immunogen (Inst), ArQule (Inst), ImClone Systems (Inst), BerGenBio (Inst), Karyopharm Therapeutics (Inst)
Patents, Royalties, Other Intellectual Property: Royalties from Oxford University Press from two books; royalties from Decision Support in Medicine from the Clinical Decision Support–Oncology online program
Travel, Accommodations, Expenses: Eli Lilly, ArQule, Bristol-Myers Squibb
REFERENCES
- 1.Lemieux J, Goodwin PJ, Pritchard KI, et al. : Identification of cancer care and protocol characteristics associated with recruitment in breast cancer clinical trials. J Clin Oncol 26:4458-4465, 2008 [DOI] [PubMed] [Google Scholar]
- 2.Filion M, Forget G, Brochu O, et al. : Eligibility criteria in randomized phase II and III adjuvant and neoadjuvant breast cancer trials: Not a significant barrier to enrollment. Clin Trials 9:652-659, 2012 [DOI] [PubMed] [Google Scholar]
- 3.Ledford H: Translational research: 4 ways to fix the clinical trial. Nature 477:526-528, 2011 [DOI] [PubMed] [Google Scholar]
- 4.Gerber DE, Lakoduk AM, Priddy LL, et al. : Temporal trends and predictors for cancer clinical trial availability for medically underserved populations. Oncologist 20:674-682, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hill RG, Jr, Sears LM, Melanson SW: 4000 clicks: A productivity analysis of electronic medical records in a community hospital ED. Am J Emerg Med 31:1591-1594, 2013 [DOI] [PubMed] [Google Scholar]
- 6.Laccetti AL, Chen B, Cai J, et al. : Increase in cancer center staff effort related to electronic patient portal use. J Oncol Pract 12:e981-e990, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Advisory Board: Build the high-value cancer care team. https://www.advisory.com/research/oncology-roundtable/studies/2017/build-the-high-value-cancer-care-team. [Google Scholar]
- 8.Holtrop JS, Potworowski G, Fitzpatrick L, et al. : Understanding effective care management implementation in primary care: A macrocognition perspective analysis. Implement Sci 10:122, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gittell JH, Beswick J, Goldmann D, et al. : Teamwork methods for accountable care: Relational coordination and TeamSTEPPS. Health Care Manage Rev 40:116-125, 2015 [DOI] [PubMed] [Google Scholar]
- 10.Chen LM, Ayanian JZ: Care continuity and care coordination: What counts? JAMA Intern Med 174:749-750, 2014 [DOI] [PubMed] [Google Scholar]
- 11.Gerber DE, Reimer T, Williams EL, et al. : Resolving rivalries and realigning goals: Challenges of clinical and research multiteam systems. J Oncol Pract 12:1020-1028, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mathieu JE, Marks MA, Zaccaro SJ: Multi-team systems, in Anderson N, Ones DS, Sinangil HK, et al (eds): Organizational Psychology: Volume 2. Handbook of Industrial, Work and Organizational Psychology. London, United Kingdom, Sage, 2001, pp 289-313. [Google Scholar]
- 13.Marks MA, DeChurch LA, Mathieu JE, et al. : Teamwork in multiteam systems. J Appl Psychol 90:964-971, 2005 [DOI] [PubMed] [Google Scholar]
- 14.Salas E, Cooke NJ, Rosen MA: On teams, teamwork, and team performance: Discoveries and developments. Hum Factors 50:540-547, 2008 [DOI] [PubMed] [Google Scholar]
- 15. Reimer T, Russell T, Roland C. Groups and teams in organizations, in Scott C, Lewis L (eds): International Encyclopedia of Organizational Communication. Hoboken, NJ, Wiley-Blackwell, 2017, pp. 1-23. [Google Scholar]
- 16.Anderson NR, West MA: Measuring climate for work group innovation: Development and validation of the team climate inventory. J Organ Behav 19:235-258, 1998 [Google Scholar]
- 17. doi: 10.1037/0022-3514.95.1.144. Leach CW, Zomeren M, Zebel S, et al:Group-level self-definition and self-investment: A hierarchical (multicomponent) model of in-group identification. J Pers Soc Psychol 95:144-165, 2008. [DOI] [PubMed] [Google Scholar]
- 18.Valentine MA, Nembhard IM, Edmondson AC: Measuring teamwork in health care settings: A review of survey instruments. Med Care 53:e16-e30, 2015 [DOI] [PubMed] [Google Scholar]
- 19. Gaertner SL, Dovidio JF: Reducing Intergroup Bias: The Common Ingroup Identity Model. Abingdon, United Kingdom, Psychology Press, 2014. [Google Scholar]
- 20.Taplin SH, Weaver S, Salas E, et al. : Reviewing cancer care team effectiveness. J Oncol Pract 11:239-246, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taplin SH, Weaver S, Chollette V, et al. : Teams and teamwork during a cancer diagnosis: Interdependency within and between teams. J Oncol Pract 11:231-238, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tajfel H, Turner J: An integrative theory of intergroup conflict, in Austin WG, Whorchel S (eds): The Social Psychology of Intergroup Relations. Monterey, CA, Brooks/Cole, 1979, pp 33-47. [Google Scholar]
- 23.Tajfel H: Social psychology of intergroup relations. Annu Rev Psychol 33:1-39, 1982 [Google Scholar]
- 24. Bourhis R, Turner J, Gagnon A: Interdependence, social identity, and discrimination, in Spears R, Oakes PJ, Ellemers N, et al (eds): The Social Psychology of Stereotyping and Group Life. Oxford, United Kingdom, Blackwell, 1997, pp 273-295. [Google Scholar]
- 25.Pennings J: Commentary: Recreating and extending buyer-supplier links following international expansion. Adv Strat Manage 10:73-79, 1994 [Google Scholar]
- 26.Matsumoto K, Nagamura F, Ogami Y, et al. : Difficulties of nursing staff involved in phase 1 oncology trials in Japan. Cancer Nurs 34:369-375, 2011 [DOI] [PubMed] [Google Scholar]
- 27.Neily J, Mills PD, Lee P, et al. : Medical team training and coaching in the Veterans Health Administration; assessment and impact on the first 32 facilities in the programme. Qual Saf Health Care 19:360-364, 2010 [DOI] [PubMed] [Google Scholar]
- 28.Neily J, Mills PD, Young-Xu Y, et al. : Association between implementation of a medical team training program and surgical mortality. JAMA 304:1693-1700, 2010 [DOI] [PubMed] [Google Scholar]
- 29.Greenspan S, Nace D, Perera S, et al. : Lessons learned from an osteoporosis clinical trial in frail long-term care residents. Clin Trials 9:247-256, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bunnell CA, Gross AH, Weingart SN, et al. : High performance teamwork training and systems redesign in outpatient oncology. BMJ Qual Saf 22:405-413, 2013 [DOI] [PubMed] [Google Scholar]
- 31.Kemp MG, Keithley JK, Morreale B: Coordinating clinical research: A collaborative approach for perioperative nurses. AORN J 53:104-109, 1991 [DOI] [PubMed] [Google Scholar]
- 32.Hange D, Björkelund C, Svenningsson I, et al. : Experiences of staff members participating in primary care research activities: A qualitative study. Int J Gen Med 8:143-148, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Irwin MM, Bergman RM, Richards R: The experience of implementing evidence-based practice change: A qualitative analysis. Clin J Oncol Nurs 17:544-549, 2013 [DOI] [PubMed] [Google Scholar]
- 34.Fishbach A, Henderson MD, Koo M: Pursuing goals with others: Group identification and motivation resulting from things done versus things left undone. J Exp Psychol Gen 140:520-534, 2011 [DOI] [PubMed] [Google Scholar]
- 35.Gwede CK, Johnsson DJ, Roberts C, et al. : Burnout in clinical research coordinators in the United States. Oncol Nurs Forum 32:1123-1130, 2005 [DOI] [PubMed] [Google Scholar]
- 36.Jackson M, Berman N, Huber M, et al. : Research staff turnover and participant adherence in the Women’s Health Initiative. Control Clin Trials 24:422-435, 2003 [DOI] [PubMed] [Google Scholar]
- 37. CMS oncology care model names NCCN guidelines as high-quality care and evidence-based recommendations. J Natl Compr Canc Netw 13:xx, 2015. [PubMed] [Google Scholar]
- 38.Clough JD, Kamal AH: Oncology care model: Short- and long-term considerations in the context of broader payment reform. J Oncol Pract 11:319-321, 2015 [DOI] [PubMed] [Google Scholar]
- 39.Parsons SK, Fineberg IC, Lin M, et al. : Promoting high-quality cancer care and equity through disciplinary diversity in team composition. J Oncol Pract 12:1141-1147, 2016 [DOI] [PubMed] [Google Scholar]
- 40.Tirodkar MA, Acciavatti N, Roth LM, et al. : Lessons from early implementation of a patient-centered care model in oncology. J Oncol Pract 11:456-461, 2015 [DOI] [PubMed] [Google Scholar]
- 41. Tschan F, NK, Hunziker S, et al: Decisive action vs. joint deliberation: Different medical tasks imply different coordination requirements, in Duffy V (ed): Advances in Human Factors and Ergonomics in Healthcare. Boca Raton, FL, Taylor & Francis, 2011, pp 191-200. [Google Scholar]