Introduction
Motor paresis is a known but rare complication of herpes zoster, estimated to occur between 0% and 6% of all cases.1 The pathogenesis of motor involvement is poorly understood but has been reported occurring with virus reactivation in nerves of the head, trunk, and extremities.1 In addition, visceral motor paresis manifesting as urinary or bowel dysfunction has also been described.1 Here we report a case of a 27-year-old man who presented with a primary complaint of difficulty voiding, which was eventually found to be caused by sacral herpes zoster.
Report
A 27-year-old man presented to the emergency department for an acute allergy manifesting as urticaria to ciprofloxacin. The patient reported visiting an urgent care clinic earlier that day for a 3-day history of difficulty with urinary voiding but no other complaints. He received the antibiotic for a suspected urinary tract infection based solely on symptoms. No urinalysis or blood work was performed. After stabilization for the allergic reaction with oral diphenhydramine and prednisone, the patient was able to spontaneously pass a small amount of urine, after which he reported no urge. However, postvoid pelvic ultrasound scan found a highly distended bladder, and Foley catheterization relieved another 780 mL of urine.
Renal ultrasound scan and genital and prostatic examination findings were all unremarkable. Urinalysis and blood work were also both negative for infection or signs of kidney dysfunction. The patient noted a small erythematous but nonvesicular rash confined to the upper left buttock, roughly 2 cm in diameter, which he claimed to have noticed that morning. However, given the presence of similarly appearing, diffuse allergic urticaria covering much of the patient's back, it was not independently evaluated. After 3 additional hours of observation, he was discharged after a spontaneous, near-complete void confirmed with pelvic ultrasound scan.
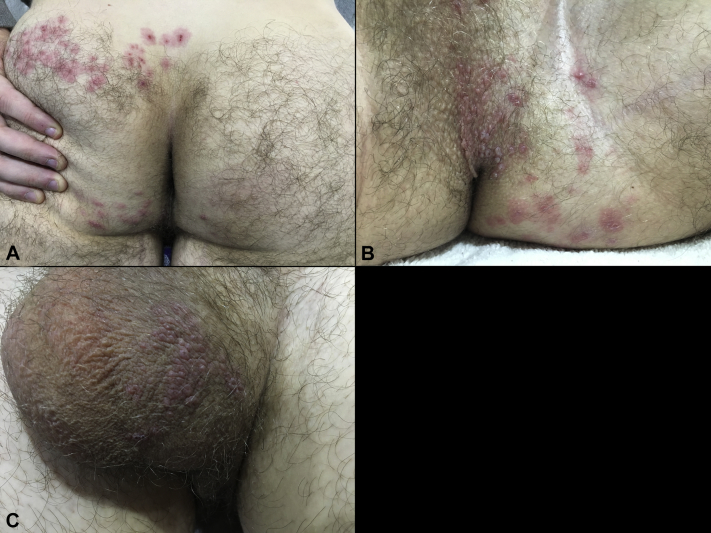
Two days later, the patient was seen in the dermatology department for significant expansion of the previously described rash and newly associated intermittent burning pain. New vesicular eruptions surrounding the original rash still confined to the upper left buttock were observed (Fig 1, A). In addition, similar eruptions were found in the left perineal region (Fig 1, B) and left posterior scrotum (Fig 1, C). He also noted no improvement in spontaneous voiding. History confirmed childhood varicella infection with no known history of genital herpes simplex. These findings were suggestive of varicella zoster virus reactivation with a rare association of voiding dysfunction. The patient was prescribed a 7-day course of oral valacyclovir (1 g, 3 times daily) for the zoster, and tamsulosin (0.4 mg daily) to aid in voiding. He was instructed to return immediately should the rash worsen or flare again.
Fig 1.
Dermatologic examination found a unilateral vesicular rash distributed within the S2 to S4 dermatomes on the left buttocks (A), perineum (B), and posterior scrotum (C) that did not arise as pictured until the fifth morning after onset of urinary dysfunction. The rash resolved without complication in 3 weeks after a 7-day course of valacyclovir.
The patient reported near immediate improvement in the ability to urinate the following day. Complete resolution of the rash occurred within 3 weeks without complication. Serology testing was performed at follow-up to rule out the possibility of herpes simplex virus. At 3 months postresolution, test results were negative for both herpes simplex virus 1 and herpes simplex virus 2 IgG (<0.2 units) with elevated varicella zoster virus IgG titers (>8 units). To date, he also reports no similar subsequent flares.
Discussion
After expansion of the rash, herpes zoster within the S2 to S4 dermatomes with likely pudendal nerve involvement extending to the scrotum became clinically evident. Sacral reactivation is uncommon, accounting for an estimated 4% to 8% of all zoster cases.2 The prevalence of voiding dysfunction associated with such cases is unknown, but one retrospective study found greater than 28% of sacral zoster cases at one institution having some form of visceral motor symptoms.3 This finding could suggest relative underdiagnosis of zoster-induced motor complications, as paresis within most other dermatomes is more likely to produce subclinical symptoms.
Unique to this case is the significant voiding dysfunction experienced before more obvious and typical signs of virus reactivation. Most other reported cases note the appearance of the unilateral vesicular rash preceding or concurrent with symptoms of voiding dysfunction.2, 4, 5, 6, 7 In addition, as with zoster generally, most published cases of associated urinary retention have been observed in the elderly.4, 5, 6, 7, 8 At least one other report notes a similar occurrence in a 25-year-old man, although this patient also suffered from Scrub typhus with other complications requiring hospitalization.2 The man described here was otherwise healthy with no signs of immunocompromise and no other systemic symptoms.
The dermatomal distribution observed shares sacral nerve roots with both parasympathetic and visceral afferent fibers within the micturition pathway.7 This finding could explain both the patient's difficulty voiding and his apparent lack of urge despite a significantly distended bladder. Alpha-1 blockers such as tamsulosin do not seem to be the standard of care for such cases, perhaps because of lack of study, with most other reports favoring regular catheterization.3, 4, 5, 6, 7 Although primarily used for action on the prostate, additional relaxing effects at the internal urethral sphincter could indicate α-1 blockers in similar cases in which sacral motor paresis may cause weakened detrusor contractions. This patient responded well to the treatment and did not require subsequent catheterization. At least one other report also notes similar success.8
Nearly all reports of zoster-induced urinary retention note return of spontaneous bladder function albeit over varying lengths of time, ranging from a few days to as long as 8 weeks.4, 8 This finding could reflect differences in severity, age, and underlying health of those affected. It is unclear whether early antiviral therapy can mitigate the length of urinary retention. Given the relative paucity of cases, such comparisons may be difficult to evaluate. The patient described here reported no continued difficulty urinating after his 1-week course of medication.
Although a more complete workup by the urgent care physician might have helped avoid the adverse drug reaction, the patient's subsequent emergency department visit also did not bring him closer to a definitive diagnosis. It was only after later eruption of the unilateral vesicular rash that the underlying cause of the patient's symptoms became clear. These findings suggest that in the setting of acute urinary retention without any other clear diagnostic signs, sacral zoster may be an important consideration, even in the absence of the classic shingles rash.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Chernev I., Dado D. Segmental zoster abdominal paresis (zoster pseudohernia): a review of the literature. PM R. 2013;5(9):786–790. doi: 10.1016/j.pmrj.2013.05.013. [DOI] [PubMed] [Google Scholar]
- 2.Hur J. Sacral herpes zoster associated with voiding dysfunction in a young patient with scrub typhus. Infect Chemother. 2015;47(2):133–136. doi: 10.3947/ic.2015.47.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen P.H., Hsueh H.F., Hong C.Z. Herpes zoster–associated voiding dysfunction: a retrospective study and literature review. Arch Phys Med Rehabil. 2002;83(11):1624–1628. doi: 10.1053/apmr.2002.34602. [DOI] [PubMed] [Google Scholar]
- 4.Acheson J., Mudd D. Acute urinary retention attributable to sacral herpes zoster. Emerg Med J. 2004;21(6):752–753. doi: 10.1136/emj.2003.009928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Addison B., Harvey M. Herpes zoster-induced acute urinary retention. Emerg Med Australas. 2013;25(3):279–281. doi: 10.1111/1742-6723.12079. [DOI] [PubMed] [Google Scholar]
- 6.Erol B., Avci A., Eken C., Ozgok Y. Urinary retention, erectile dysfunction and meningitis due to sacral herpes zoster: a case report and review of the literature. Urol Int. 2009;82(2):238–241. doi: 10.1159/000200807. [DOI] [PubMed] [Google Scholar]
- 7.Julia J.J., Cholhan H.J. Herpes zoster-associated acute urinary retention: a case report. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(1):103–104. doi: 10.1007/s00192-006-0066-1. [DOI] [PubMed] [Google Scholar]
- 8.Jakubovicz D., Solway E., Orth P. Herpes zoster Unusual cause of acute urinary retention and constipation. Can Fam Physician. 2013;59(3):e146–e147. [PMC free article] [PubMed] [Google Scholar]